Abstract
This study investigated the ability of a theoretically driven, psychosocial prevention program implemented through childbirth education programs to enhance the coparental relationship, parental mental health, the parent–child relationship, and infant emotional and physiological regulation. A sample of 169 heterosexual, adult couples who were expecting their 1st child was randomized to intervention and control conditions. The intervention families participated in Family Foundations, a series of 8 classes, delivered before and after birth, that was designed as a universal prevention program (i.e., it was applicable to all couples, not just those at high risk). Intent-to-treat analyses indicated significant program effects on coparental support, maternal depression and anxiety, distress in the parent–child relationship, and several indicators of infant regulation. Intervention effects were not moderated by income, but greater positive impact of the program was found for lower educated parents and for families with a father who reported higher levels of insecure attachment in close relationships. These findings support the view that coparenting is a potentially malleable intervention target that may influence family relationships as well as parent and child well-being.
Keywords: coparenting, prevention, parenting, infancy
Theory and research suggest that coparenting—that is, how parents coordinate their parenting, support or undermine each other, and manage conflict regarding child rearing—is a central aspect of family life (McHale, Kuersten-Hogan, Lauretti, & Rasmussen, 2000; Minuchin, Rosman, & Baker, 1978; Van Egeren, 2004). A number of studies have demonstrated the influence of the coparenting relationship measured across childhood—from infancy through adolescence—on measures of parenting, parent–child relations, and child social–emotional adjustment and behavioral problems (Feinberg, Kan, & Hetherington, 2007; Schoppe, Mangelsdorf, & Frosch, 2001). Thus, coparenting is a potential leverage point for enhancement of family functioning and child outcomes.
Despite this emerging recognition of the coparenting relationship, there is as yet no published evidence regarding the ability of psychosocial intervention to effect positive change in coparenting (Feinberg, 2002). In this article, we present the first results of a randomized trial of Family Foundations (FF), a universal prevention program that was developed to enhance coparenting quality among cohabiting and/or married couples who were expecting a first child. FF is a series of eight interactive, psychoeducational, skills-based classes designed for expectant couples who are cohabiting or married. The program is delivered through the universal, nonstigmatizing framework of childbirth education departments of local hospitals. This article is poised to shed light on whether positive coparenting can be enhanced through a universal, group-format program and whether such a program would also enhance parental mental health and parenting.
Coparenting and Parent and Child Outcomes During the Transition to Parenthood
Our focus on enhancing coparenting during the transition to parenthood is based on a view of coparenting as a potentially malleable causal mechanism. Research has indicated that the coparenting relationship is more strongly related to parenting and child outcomes than is the general couple or marital relationship (Abidin & Brunner, 1995; Bearss & Eyberg, 1998; Frosch, Mangelsdorf, & McHale, 2000). This research supports Margolin’s view that coparenting represents a risk mechanism, whereas general marital conflict or marital quality may represent a risk indicator (Margolin, Gordis, & John, 2001). This view is also supported by evidence of coparenting as a mediator of the relationship between the couple relationship and parenting, both cross sectionally and longitudinally (e.g., Gonzales, Pitts, Hill, & Roosa, 2000). When developing prevention programs, it is obviously more effective to target the risk mechanism rather than a factor that may be a marker of risk but is not a causal influence on outcomes.
There are several important dimensions of coparenting, including division of labor and joint management of family dynamics (Feinberg, 2003). We have focused on the dimensions of coparental support and undermining, because research has indicated that these dynamics are linked to parenting and child outcomes (Abidin & Brunner, 1995; Belsky, Putnam, & Crnic, 1996; Feinberg, Neiderhiser, Reiss, & Hetherington, 2005; Floyd & Zmich, 1991). Conceptually, coparental support includes affirming the other parent’s competence as a parent, acknowledging and respecting the other parent’s contributions, and upholding his or her parenting decisions and authority (Belsky, Wood-worth, & Crnic, 1996; McHale, 1995; Weissman & Cohen, 1985). The negative counterpart of coparental support is expressed through undermining the other parent through criticism, disparagement, and blame.
Qualitative interviews with new parents (Feinberg, 2002) drew our attention to an additional, potentially significant aspect of coparenting: sharing the joys of parenthood. This dimension of coparenting, which we term parenting-based closeness, is related to but distinct from coparental support. Whereas coparental support relates to respecting and upholding the other parent’s decisions, parenting-based closeness derives from shared celebration of the child’s development, working together as a team, and witnessing one’s partner develop as a parent.
Despite the potential for increased closeness, the transition to parenthood is fraught with risk for a large number of couples (Belsky & Pensky, 1988). Relationship shifts during the postpartum period include dramatically increased conflict, changes in the division of labor and extrafamilial roles, and reduced couple companionship and sex (Cowan & Cowan, 1995). These changes undermine the adjustment and well-being of new parents, with subsequent effects on parenting quality and child adjustment. Derived from our theoretical model of coparenting (Feinberg, 2003) during the transition period (Feinberg, 2002), one goal of FF is to buffer parental adjustment from these strains by enhancing positive support and coordination in the coparenting relationship.
As an indicator of parental adjustment, postpartum depression is relevant for all parents but particularly for mothers (Walther, 1997) and has negative repercussions for parent–child interaction and child development (Field, 2000). Evidence suggests that coparental support—or, as measured in some prior work, general emotional support from the father—is linked to lower maternal depression (Crnic & Greenberg, 1987; O’Hara & Swain, 1996). Less well researched but also problematic is elevated parental anxiety (e.g., Ross & McLean, 2006). Maternal anxiety during pregnancy seems to have negative effects on fetal development and has been linked to children’s later cognitive, behavioral, and emotional problems (O’Connor et al., 2005). Maternal anxiety after birth has been linked to disrupted parenting, parent–child relations, and child behavior (e.g., Kaitz & Maytal, 2005). Although there is limited research on risk factors for maternal anxiety, there is evidence that lack of social support is linked to maternal anxiety as well (Glazier, Elgar, Goel, & Holzapfel, 2004). Thus, we hypothesized that the FF program would reduce parental depression and anxiety.
Our conceptual model (Feinberg, 2003) also led us to expect that enhanced coparental support and, subsequently, enhanced parental adjustment would facilitate more positive parent–child interaction. Coparental support regarding one’s competence as a parent (Tice, 1992) was hypothesized to affect parenting and the parent–child relationship through parental self-efficacy (or confidence), which has been proposed as the final common pathway to addressing disruptions in caregiver sensitivity (Teti, O’Connell, & Reiner, 1996). On the basis of this reasoning, we hypothesized that FF would have a beneficial impact on parent interactions with the child.
Finally, we hypothesized that FF—through its effects on positive coparenting and subsequent improvements in parental adjustment and parent–child relations—would affect indices of infant well-being. For example, increased coparental support may translate into a less stressful family environment for the infant, with potentially positive effects on stress-related physiological systems. Given the rapid development in emotional and physiological regulation during infancy, we examined three indicators of infant regulation that might be disrupted by stress in family relationships: regular sleep patterns, calming when distressed, and sustained attention. We selected these three indicators for several reasons, among them, evidence that these domains may be important in feed-forward loops with later child development and family relations. For example, infant sleep dysregulation may have negative effects on both children’s and parents’ well-being (Sepa, Frodi, & Ludvigsson, 2004). Parents who feel unable to soothe their child may develop a low sense of parental self-efficacy, with negative implications for parent–infant relations (Papousek & von Hofacker, 1998; Stifter & Bono, 1998). Additionally, the infant’s deployment of attention (e.g., through distraction) may represent an early emotional regulatory mechanism that is a foundation of more complex regulatory strategies (Rothbart, Posner, & Kieras, 2006).
Strategy: Timing and Context
The transition to parenthood is an opportune moment for prevention, because of expectant and new parents’ particular openness to change (Duvall, 1977; Feinberg, 2002), but few prevention programs that focus on the interparental relationship at this period have been rigorously assessed with a substantial sample. A seminal project in this area, the Becoming a Family project, consisted of a 6-month program based largely on a discussion and support group model. Although results demonstrated that intervention during the transition period can have positive effects (Cowan & Cowan, 1992), the number of sessions (25), small group size (four couples in each group), and group leader expertise (the leaders were the Cowans and their graduate students) were not feasible elements for widespread dissemination.
The development of FF built on the efficacy trial of the Cowans and colleagues in order to allow us to examine whether fewer sessions, greater group size, and less trained group leaders could have a beneficial impact on coparenting and on family and child well-being. To promote a universal, nonstigmatizing framework, we collaborated with childbirth education departments at local hospitals to develop and deliver the program. In contrast to some programs recently sponsored by the federal Healthy Marriage Initiative, FF did not focus on the couple or marital relationship per se but rather on how parents could work together effectively (see the Method section for more details). The content of the sessions was directly related to our conceptual theory of coparenting (Feinberg, 2003) and to the risks that emerge during the transition period (Feinberg, 2002). The program focuses on helping couples become aware of areas of coparental disagreement before parenthood and on managing disagreements through productive communication, problem solving, and conflict management techniques. The program material prepares parents for the strains of the transition period by noting that many new parents experience a high level of stress and strain (see review in Sanders, Nicholson, & Floyd, 1997). By providing information on other couples’ experiences of parenthood, enhancing communication skills, and facilitating discussion of partner expectations for each other, we aimed to minimize the strains of the transition, increase coparental support, and decrease coparental undermining.
The Current Study
In this article, we assess whether the FF program had positive effects on the short-term outcomes identified above: coparenting, parental depression and anxiety, distress in the parent–infant relationship, and infant regulatory competence (sleep, attention duration, soothability). All analyses included parent age and education as covariates, because these factors have been linked to parenting and the couple relationship in previous work. To control for potential response bias (Morsbach & Prinz, 2006) related to the demand characteristics of participation in the intervention condition, all analyses also controlled for parent social desirability.
It has frequently been observed that most premarital programs and relationship enhancement programs have been developed with and tested on middle-class, well-educated couples (Ooms & Wilson, 2004). Although the current sample is, on average, well educated and middle class, there is a wide range of income and education in the sample that allows for an exploration of moderation of program effects. Finally, some have critiqued relationship education programs as benefiting those who are already interested in and comfortable with relationship issues (i.e., the rich get richer). To assess the validity of this critique, we assessed whether parents with a low level of insecurity in romantic relationships, which is linked to couple relationship quality, derived relatively greater positive benefit from the program.
Method
Participants
Participants were 169 heterosexual couples who, at the time of recruitment, were expecting their first child and were living together (regardless of marital status). All participants were at least 18 years of age. The couples resided in rural areas, towns, and small cities. Eighty-two percent of couples were married, and the majority of participants (91% of mothers and 90% of fathers) were non-Hispanic White. The remaining participants were African American, Asian, Hispanic, or other ethnicity. Median annual family income was $65,000 (SD = $34,372), with a range of $2,500 to $162,500. Average educational attainment was 15.06 years for mothers (SD = 1.82) and 14.51 years for fathers (SD = 2.19), with a range of ninth grade to beyond college; 14.4% of mothers and 29.3% of fathers did not complete any postsecondary school education. Mean ages were 28.33 years (SD = 4.93) for mothers and 29.76 years (SD = 5.58) for fathers. Although the sample is not representative of U.S. families, it is generally representative of the racial and economic background of families from the regions where the data were collected. Data from 4 couples were not utilized in analyses because of developmental difficulties, death of one of the parents, or congenital medical problems for the baby.
Procedure
Couples were primarily (81%) recruited from childbirth education programs at two hospitals located in small cities. All other couples were recruited from doctors’ offices or health centers (8%), by newspaper ads or flyers (7%), by word of mouth (3%), or by unknown means (including radio advertisement; 1%). Couples recruited from childbirth education programs were sent a letter and then contacted by phone. Couples recruited through health centers returned a postcard, and all other couples called the program office if they were interested in participation. Of eligible couples contacted by phone, 23% agreed to participate; reasons for not participating were a lack of time, inability to attend evening sessions, and a perceived lack of need. Couples in both conditions participated concurrently in standard childbirth education classes.
Pretest data were collected during home interviews when mothers were pregnant (average weeks of gestation = 22.9, SD = 5.3). Human subject protections were reviewed, and consent forms were signed. Couples were paid an honorarium for their participation. Mothers and fathers worked separately on questionnaires regarding their relationship experiences, individual qualities and attitudes, and individual well-being. Additionally, interviewers collected two 12-min videotaped interactions of each couple (not included in the current analyses).
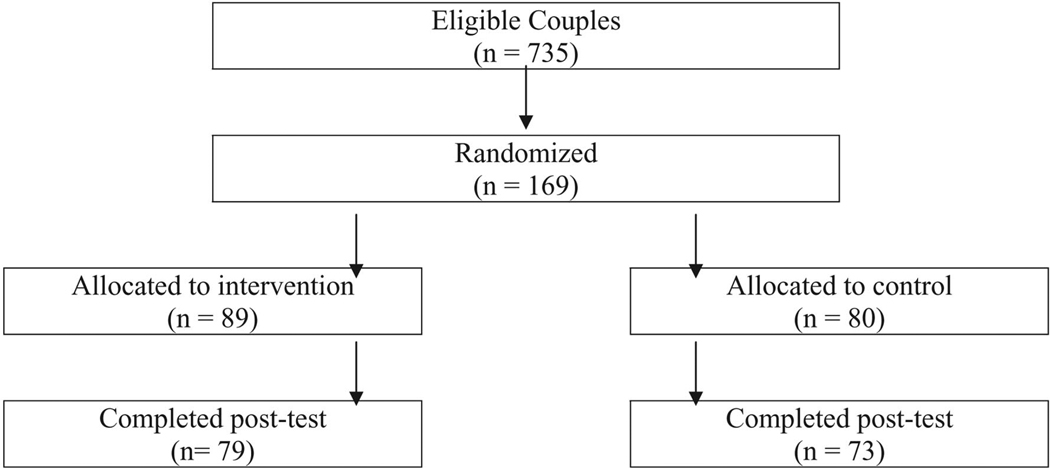
After pretest, couples were randomly assigned to intervention (n = 89) or to no-treatment control conditions (n = 80; see Figure 1). Randomization yielded equivalent groups, as analyses indicated no significant differences between intervention couples and control group couples on a wide range of pretest variables, including age, income, education, marital status, weeks of gestation, mental health, and relationship quality. The couples in the no-treatment control group were mailed a brochure about selecting quality child care; intervention couples received the FF program (consisting of four prenatal and four postnatal sessions). FF was manualized, with didactic material, exercises, and behavioral rehearsal included in the curriculum for each session.
Figure 1.
Study participation.
Instead of focusing on the parents’ romantic or marital relationship (as in the federal government’s Healthy Marriage Initiative), FF focuses on emotional self-management, conflict management, problem solving, communication, and mutual support strategies that foster positive joint parenting of an infant. These topics are introduced and applied to issues such as dividing labor, facilitating emotional security, and providing stimulation. Each group consisted of 6–10 couples, and sessions were led by a male–female team. Group leaders received 3 days of training, and ongoing observation of sessions facilitated regular supervision discussions. Observer ratings indicated that the program was implemented as planned, with an average of 95% of the curriculum content delivered.
The average number of sessions attended by each couple in the intervention group was 5.50 for mothers and 5.38 for fathers. Most couples (66% of mothers and 63% of fathers) attended 5 or more sessions. Twelve percent of mothers and 12% of fathers attended 1 or 2 sessions, and 3% of mothers and 5% of fathers attended no sessions. Seventy percent of intervention group couples attended at least 1 of the 4 postnatal sessions. Couples attended sessions together; only in a few cases did a parent attend a session when the partner was unavailable (e.g., because of work schedule or postpartum recovery).
Posttest data collection occurred after the intervention couples had completed the postnatal classes, when babies were about 6 months old (average child age = 6.5 months, SD = 1.6). At posttest, couples filled out written questionnaires and mailed them back to the research office. There was minimal sample attrition from Wave 1 to Wave 2: 92% of mothers and 90% of fathers participated at Wave 2. Both parents in 149 couples and mothers only in 3 couples participated. The Wave 2 participants and nonparticipants were not significantly different on a number of pretest variables; however, the nonparticipants were more likely to be unmarried and to have lower levels of education (p < .05). There was no evidence of differential attrition by condition: The rates of participation at Wave 2 were similar (91% of control couples and 89% of intervention couples), and there were no differences in the association of pretest variables with continued participation across conditions.
Measures
Coparenting
Mothers and fathers reported on multiple dimensions of the coparenting relationship at Wave 2 with a measure, developed for this study, that was based in part on adaptation of prior measures (Abidin & Brunner, 1995; Frank, Olmstead, Wagner, & Laub, 1991; Margolin, 1992; McHale, 1997). Scale development was based on a combination of theoretically based conceptualization, exploratory factor analysis, and reliability analysis. All items utilized 7-point Likert response scales. We utilized three scales to assess the key dimensions of the coparenting relationship: Coparental Support, Parenting-Based Closeness, and Coparental Undermining. Each scale comprised 5 items. Sample items of each of the three scales are as follows: Coparental Support, “My partner supports my parenting decisions”; Parenting-Based Closeness, “I feel close to my partner when I see him or her play with our child”; and Coparental Undermining, “My partner sometimes makes jokes or sarcastic comments about the way I am as a parent.” Cronbach’s alphas ranged from .80 to .83 for mothers and from .66 to .80 for fathers. Descriptive statistics for all measures are in Table 1, and correlations are in Table 2.
Table 1.
Means and Standard Deviations for Study Variables
| Intervention families |
Control families |
|||||||
|---|---|---|---|---|---|---|---|---|
| Mother report |
Father report |
Mother report |
Father report |
|||||
| Variable | M | SD | M | SD | M | SD | M | SD |
| Pretest measure | ||||||||
| Social desirability | 17.41 | 5.17 | 17.68 | 4.56 | 18.63 | 5.12 | 18.20 | 4.85 |
| Attachment insecurity | 2.37 | 0.70 | 2.22 | 0.54 | 2.23 | 0.60 | 2.35 | 0.54 |
| Depressive symptoms | 0.42 | 0.47 | 0.25 | 0.33 | 0.43 | 0.43 | 0.25 | 0.27 |
| Anxiety | 7.08 | 3.40 | 5.31 | 3.39 | 6.94 | 4.24 | 6.05 | 3.70 |
| Posttest measure | ||||||||
| Depressive symptoms | 0.33 | 0.35 | 0.21 | 0.29 | 0.41 | 0.45 | 0.19 | 0.27 |
| Anxiety | 6.48 | 4.44 | 4.43 | 3.71 | 6.59 | 4.48 | 5.22 | 4.00 |
| Coparental support | 4.94 | 0.89 | 5.11 | 0.70 | 4.64 | 1.23 | 4.82 | 0.78 |
| Coparental undermining | 0.53 | 0.89 | 0.73 | 0.92 | 0.49 | 0.60 | 0.63 | 0.71 |
| Parenting-based closeness | 4.81 | 1.15 | 5.02 | 0.94 | 4.75 | 1.09 | 4.67 | 0.98 |
| Parent-child dysf. Interaction | 1.31 | 0.41 | 1.44 | 0.45 | 1.41 | 0.50 | 1.70 | 0.58 |
| Duration of orienting | 4.34 | 1.09 | 4.15 | 1.08 | 4.16 | 0.99 | 3.89 | 0.95 |
| Infant soothability | 5.16 | 0.81 | 4.95 | 0.89 | 5.20 | 0.87 | 4.64 | 1.04 |
| Child sleep habits | 2.95 | 0.66 | — | — | 2.78 | 0.73 | — | — |
Note. Dashes indicate that only mothers completed these measures. Dysf. = dysfunctional.
Table 2.
Correlations Between Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Ed | .59** | .47** | − .05 | − .32** | − .26** | − .41** | − .14† | − .22** | .28** | .22** | − .13 | − .08 | .03 | − .08 | .15† |
| 2. Age | .33** | .81** | .05 | − .08 | − .10 | − .32** | − .02 | − .14† | .22** | .11 | − .15† | .01 | − .05 | − .03 | .06 |
| 3. SD | .07 | − .003 | .05 | − .22** | − .22** | − .14† | − .34** | − .17* | .17* | .07 | − .14† | − .14† | .12 | .03 | − .12 |
| 4. Att In | − .27** | − .09 | − .29** | .16† | .53** | .38** | .52** | .43** | − .26** | − .19* | .28** | .10 | − .09 | − .10 | .05 |
| 5. Dep1 | − .21* | − .11 | − .13 | .34** | .09 | .49** | .54** | .47** | − .21** | − .06 | .23** | .06 | − .06 | − .12 | − .09 |
| 6. Dep2 | − .05 | − .08 | − .10 | .18† | .37** | .14† | .43** | .67** | − .43** | − .45** | .38** | .31** | .08 | − .15† | − .21** |
| 7. Anx1 | − .26** | − .13 | − .19* | .39** | .55** | .29** | .10 | .62** | − .24** | − .17* | .16† | .11 | − .15† | −24** | − .04 |
| 8. Anx2 | − .12 | .02 | − .16† | .25** | .54** | .57** | .66** | .08 | − .42** | − .42** | .21* | .25** | − .01 | − .14† | − .09 |
| 9. Supp | .12 | .07 | .13 | − .31** | − .23** | − .18* | − .30** | − .28** | .33** | .66** | − .49** | − .21** | .05 | .12 | .14† |
| 10. Close | .27** | − .04 | .09 | − .25** | − .14† | − .14† | − .19* | − .15† | .63** | .49** | − .42** | − .34** | − .01 | .16† | .21* |
| 11. Under | − .23** | − .10 | − .22** | .15 | .25** | .33** | .26** | .36** | − .51** | − .42** | .32** | .22 | .01 | − .10 | − .13 |
| 12. DI | − .24** | − .04 | − .13 | .30** | .26** | .15† | .30** | .30** | − .52** | − .49** | .35** | .001 | − .14† | − .28* | − .08 |
| 13. DO | − .06 | − .02 | − .04 | − .09 | .04 | .10 | .02 | .02 | .09 | .01 | .02 | −.11 | .44** | .32** | .03 |
| 14. Sooth | .04 | .09 | .05 | − .10 | − .05 | − .07 | − .17* | − .07 | .22** | .18* | − .02 | − .20* | .04 | .21* | − .02 |
| 15. SH | .11 | − .06 | − .05 | .03 | .05 | − .02 | − .07 | − .11 | .17* | .12 | − .14† | − .14† | .10 | − .01 | — |
Note. Correlations are above the diagonal for mothers and below the diagonal for fathers. Mother-father correlations are shown in boldface along the diagonal. Ed = education; SD = social desirability; Att In = attachment insecurity; Dep1 = pretest depressive symptoms; Dep2 = posttest depressive symptoms; Anx1 = pretest anxiety; Anx2 = posttest anxiety; Supp = coparental support; Close = parenting-based closeness; Under = coparental undermining; DI = parent-child dysfunctional interaction; DO = duration of orienting; Sooth = infant soothability; SH = child sleep habits. Sleep habits are from mother reports only.
p< .10.
p < .05.
p <.01.
Parental mental health
Depressive symptoms were measured at both waves with a subset of 7 items from the Center for Epidemiological Studies Depression Scale (Howe, Levy, & Caplan, 1999; Radloff, 1977). Items referred to symptoms experienced during the past week (e.g., “How often did you feel sad?”) and were answered on a 4-point frequency scale. Cronbach’s alphas were .84 for mothers and .66 for fathers. Anxiety was measured at both waves with the 20-item short form of the Taylor Manifest Anxiety Scale, which measures chronic anxiety (Bendig, 1956; Taylor, 1953). Items (e.g., “I am a high-strung person”) followed a dichotomous yes/no format. Cronbach’s alphas were .85 for mothers and .78 for fathers.
Parent–Child dysfunctional interaction
Due to limited funding, our research design did not include observational data at posttest. Instead, we assessed parent report of distress in the parent–child relationship, a construct associated with observed parenting and later child problems (Reitman, Currier, & Stickle, 2002). The 6-item Dysfunctional Interaction scale from the Parental Stress Index (Abidin, 1997; Reitman, Currier, & Stickle, 2002) assesses distress in the parent–child relationship (e.g., “My child smiles at me much less than I expected”). Cronbach’s alphas were .79 for mothers and .77 for fathers.
Infant regulation
We assessed duration of orienting and infant soothability at Wave 2 with the corresponding subscales of the Infant Behavior Questionnaire (Gartstein & Rothbart, 2003). Duration of orienting included 10 items (e.g., “How often during the last week did your baby play with one toy/object for 5–10 minutes?”); alphas were .84 for mothers and for fathers. Soothability included 9 items (e.g., “When your baby was upset, how often were you able to comfort him/her by rocking?”); alphas were .81 for mothers and .86 for fathers. Child sleep habits were measured at Wave 2 with 8 items that assessed the ability of the baby to put itself to sleep, regularity of sleeping, and night waking (Seifer, Sameroff, Dickstein, & Hayden, 1996). Only mothers completed this measure. Cronbach’s alpha was .75.
Control and moderator variables
We utilized age, education, and social desirability as control variables. Education was measured by total years of education. Participants completed a 33-item Social Desirability scale at Wave 1 (e.g., “I am always courteous, even to people who are disagreeable”; Crowne & Marlow, 1964). Alphas were .75 for mothers and .69 for fathers. Education and attachment insecurity were utilized as moderators. Attachment insecurity in close relationships was measured at Wave 1 with a 20-item subscale of the Relationships Scale Questionnaire (Griffin & Bartholomew, 1994). On a 5-point scale, participants rated the extent to which 20 statements described their characteristic style in close relationships. Alphas were .80 for mothers and .79 for fathers.
Analyses
All tests of the effect of the program were conducted as intent-to-treat analyses; data from all parents who completed the posttest were included, regardless of level of program participation. Condition was coded 0 for control and 1 for intervention. For child temperament, researchers have debated the advantages and disadvantages of utilizing separate versus aggregated parent ratings. We utilized aggregated ratings but explored separate parent ratings where effects were not significant.
To provide consistency across all outcome variables reported on by mothers and fathers, we conducted analyses as multivariate, multilevel regression models (SAS Proc Mixed) with mothers’ and fathers’ scores as two dependent measures (thereby accounting for within-family dependency); this approach yielded separate estimates for mothers and for fathers. For outcomes reported on by only one parent or when mother and father reports were combined into a single measure, analyses were conducted with a general linear model regression approach (SAS Proc GLM). For depression and anxiety, the intervention effect was represented by the interaction of condition with wave (pretest = 0, post-test = 1) for each parent. The same control variables were utilized in all models: parent age, education, and social desirability. We also examined whether parent education or attachment insecurity moderated the impact of the program.
Results
Descriptives
Although our study focused on program impact, we note several interesting features of the descriptive data. First, as shown in Table 1, the levels of depression and anxiety declined from pre- to posttest for both mothers and fathers. Although the physical effects of pregnancy may have elevated the physiologically oriented items related to adjustment, this would not be the case for fathers. It appears that, in this sample at least, the pregnancy period was more disruptive for parental well-being than was the early parenthood period. Moreover, we note that father’s anxiety and depression were lower than mother’s anxiety and depression at both waves and that fathers reported somewhat higher levels of positive and negative coparenting than did mothers. As shown in Table 2, the correlations of most measures across parents were low. Within parent, the correlations between anxiety and depression and among the indices of coparenting were moderate for both mothers and fathers. The correlations between adjustment and coparenting were low to moderate; the stronger ones indicate that concurrent anxiety and depression were negatively linked to coparental support and were positively linked to coparental undermining.
Coparenting
Results of the tests of intervention impact are summarized in Table 3. Intervention status was significant for both mother and father report of coparental support and for father report of parenting-based closeness. (Statistical significance is considered throughout this article as the conventional p < .05.) In all cases, the intervention condition reported more positive coparenting than did the control condition. The variable that represents experimental condition (control vs. intervention) did not have a significant effect on coparental undermining.
Table 3.
Results of Tests of Intervention Impact: Main Effect of Intervention
| Mother report |
Father report |
|||||
|---|---|---|---|---|---|---|
| Dependent measure | B | SE | Effect size | B | SE | Effect size |
| Coparental undermining | .028 | 0.126 | ns | .095 | 0.129 | ns |
| Coparental support | .326* | 0.169 | 0.35 | .280* | 0.123 | 0.54 |
| Parenting-based closeness | .049 | 0.183 | ns | .387* | 0.155 | 0.44 |
| Depressive symptoms | −.195** | 0.065 | 0.56 | .076 | 0.048 | ns |
| Anxiety | −1.218* | 0.569 | 0.38 | .816 | 0.514 | ns |
| Parent-child dysf. interaction | −.137† | 0.075 | 0.34 | − .291* | 0.083 | 0.70 |
| Infant soothability | −.021 | 0.141 | ns | .312* | 0.160 | 0.35 |
| F | df | |||||
| Duration of orienting | 4.33* | 1 | 0.34 | — | — | — |
| Child sleep habits | 2.67† | 1 | ns | — | — | — |
Note. Multilevel models were utilized for variables with both mother and father reports; general linear models were utilized for other variables. Coefficients for depression and anxiety represent Condition × Time interactions; other coefficients are for intervention status predicting posttest measure. Fathers did not report on child sleep habits. Duration of orienting represents aggregate of mother and father reports. Each predictor was examined in a separate model, which included age, education, and social desirability score as covariates. Dysf. = dysfunctional.
p < .10.
p < .05.
p < .01.
Parent Mental Health
Results indicate a significant intervention effect on maternal depression and anxiety: For both outcomes, the interaction term that represented Condition × Time was significant. Follow-up analyses and plots indicated that intervention group mothers had a larger decrease in depression and anxiety than did control group mothers, who had an essentially constant level of depression but reported a decrease in anxiety.
Parent–child Dysfunctional Interaction
Intervention status was a significant predictor (p < .05) of father report of parent–child dysfunctional interaction; intervention status demonstrated a trend (p < .10) toward predicting the mother report. In both cases, intervention parents reported lower levels of dysfunctional interaction than did control parents.
Infant Regulation
Intervention status significantly predicted the mother–father aggregated report of duration of orienting (p < .05) but not infant soothability. We then examined mother and father reports of infant soothability separately: Intervention status significantly predicted father report but not mother report. The sign of the coefficients indicated that intervention group infants had a longer duration of orienting and (by father report) greater soothability. There was evidence of a trend (p < .10) toward intervention impact on child sleep.
Effect Sizes
Effect sizes were calculated for results that were significant or demonstrated a trend and that were based on adjusted group means (i.e., they accounted for the covariates included in the intervention effect models). For coparenting, effect sizes were .35 for mother report and .54 for father report of coparental support, respectively. Father report of coparenting closeness yielded an effect size of .44. The effect size for mother’s depression was .56 and for mother’s anxiety was .38. The largest effect size, .70, was for father report of dysfunctional interaction with the child. The sizes of other significant effects can be found in Table 3.
Moderator Analyses
The tests of moderation examined the interaction term formed by the moderator and the intervention status variable; for depression and anxiety, the test consisted of the three-way interaction of the moderator, intervention status, and time. We used the corresponding mother and father reports of the moderator (e.g., mother’s education, father’s education) to form the appropriate interaction terms for mother and father reports of outcomes. Mother report of the moderator was utilized for outcome variables that were aggregates of mother and father reports.
For education, we examined moderation for each of the 16 outcomes reported in Table 3 as main effects. Parent education significantly moderated the intervention effect on 3 outcomes, each of which was reported by mothers: maternal depression (B = 0.091, p < .01), mother report of coparental support (B = −0.208, p < .05), and child sleep habits (B = −3.908; p < .01). In each case, plots of the results indicated that the intervention effect was greater for mothers with less education than for mothers with more education. We note that for child sleep habits, the main effect of the intervention was not significant; follow-up regression analyses indicated a significant intervention effect for the less educated half of the sample.
For attachment insecurity, we examined whether both maternal and paternal attachment insecurity moderated either maternal or paternal intervention effects. We limited analyses to the program targets of coparental support and undermining, parental depression, and parent–child dysfunctional interaction. Thus, we examined a total of 16 moderation models (4 outcomes × 2 parents × 2 moderators) and found seven significant results. Six of them demonstrated greater intervention effects when the parent had a higher level of insecurity. The one finding that indicated greater intervention effects with lower levels of insecurity may have been due to chance, given that we conducted 16 tests, and will not be interpreted.
We now focus on the six significant findings that indicated greater intervention effects with higher levels of insecurity: The effect of the intervention on maternal depression was moderated by both father’s insecurity (B = −0.225) and mother’s own insecurity (B = −0.241, p < .01). The program effect on mother’s coparental support was moderated by father’s insecurity (B = 0.377, p < .01). (The effect on father’s coparental support showed a trend, p < .10, toward moderation by father’s insecurity.) The program effect on father’s coparental undermining was moderated by father’s insecurity (B = −0.297). Finally, father’s insecurity moderated the effects on both maternal (B = −0.148) and paternal (B = −0.274) dysfunctional interaction with the child.
Finally, we assessed whether session attendance among intervention participants predicted better outcomes. We plan to conduct propensity score analyses after all future waves of data have been collected and here briefly present bivariate results. Attending two or more sessions (vs. attending zero or one session) was associated with significantly higher levels of positive coparenting for all the coparenting variables that demonstrated intervention effects, as well as for father report of parent–child dysfunctional interaction. Additionally, greater attendance showed a trend toward less depression at posttest for mothers.
Discussion
This randomized controlled trial represents, to our knowledge, the first investigation of whether a brief, universal prevention program is able to enhance parent coordination and mutual support in parenting roles. The selection of coparenting as the primary short-term target was based on a view of the coparenting relationship as a key subset of the overall interparental relationship, which itself has been linked to parenting and child outcomes for 25 years. This initial implementation of the FF program was delivered through an existing and non-stigmatizing institutional niche— childbirth education departments at local hospitals—rather than in a highly controlled university setting.
Main Effects
Results of intent-to-treat analyses on parent reports at posttest indicated that implementation of the program was successful in several important ways. Both intervention mothers and intervention fathers reported better coparental support than did their counterparts in the control condition. Compared with control fathers, intervention fathers reported greater parenting-based closeness with their partner. These results support the view that coparenting can be enhanced through intervention.
Beyond coparenting, the intervention condition demonstrated relatively better maternal mental health. In analyses that controlled for levels of depression and anxiety during pregnancy, we found that intervention mothers had lower levels of depression and anxiety at posttest compared with control mothers. These are important findings for several reasons. First, maternal depression and anxiety have been shown to be related to disrupted parent–child relations and to negative child outcomes (see above). Second, prenatal maternal anxiety affects fetal development (Van der Bergh, Mulder, Mennes, & Glover, 2005). Although we are not able to assess whether the program’s impact on maternal depression and anxiety occurred before the baby’s birth, it is likely there was at least some prenatal effect, because half the classes occurred before birth. Third, because not all psychotropic drugs are safe for pregnant or nursing mothers, there is a need for behavioral preventive approaches.
Although the results for the intervention effect on paternal depression and anxiety were not significant, the direction of the coefficients implies the program may have slightly increased depression and anxiety in fathers. We speculate that the program may have facilitated a balancing of the burden and strain of early parenthood. These increases for fathers do raise a concern about iatrogenic effects; however, the levels of paternal depression and anxiety are much lower than were maternal levels, and the rise in paternal levels was small and nonsignificant.
Results also indicated that intervention parents showed less difficulty in the parent–child relationship. Intervention condition fathers reported significantly lower levels of distress in their relationship with the child than did control fathers, and a trend in the same direction was found for mothers. This construct was measured with a scale that has been linked to observed parenting and later child problems (e.g., Haskett, Ahern, Ward, & Allaire, 2006; Rodriguez & Green, 1997). We also found evidence that the program had an impact on infant regulation. There was a significant intervention effect on parents’ combined rating of the child’s duration of attention and on father report of infant soothability. There was also evidence of a trend that suggested impact on child sleep habits. Although these elements represented secondary program targets, it may be that enhanced family functioning helped foster infant physiological/emotional regulation.
Against these positive results, however, we note that there was no evidence of program impact on coparental undermining. We believe that the lack of impact on this dimension of coparenting is related to a floor effect—that is, low levels of coparental undermining in both the intervention and control groups (see means in Table 1). In our own and others’ experience, explicit hostile–competitiveness between parents of an infant is rare (McHale, Kuersten-Hogan, & Lauretti, 2001), a fact that may be related to the developmental course of coparenting. The infant’s vulnerability and demandingness, coupled with the lack of experience of most fathers in caring for infants, seem to lead many fathers to follow the lead of the mother in providing infant care (McHale, Kuersten-Hogan, & Rao, 2004). The implicit agreement to let mothers lead during infancy may keep levels of coparental hostility low. Coparental undermining emerges as problematic only during the 2nd or 3rd year after birth, when children’s developing physical independence and verbal ability require new parenting behaviors and responses, such as limit setting, disciplining, and educating. We hypothesize that the father’s more active role after infancy combines with parents’ differing child-rearing beliefs to create heightened conflict. Program effects on undermining therefore may not be discernible until after infancy.
The magnitude of the program impact on the constructs examined here was moderate, ranging from .34 to .70. These effects are similar to those obtained by other relationship enhancement programs (relationship satisfaction: d = .3–.4; communication: d = .4–.7), according to a recent meta-analysis (Hawkins, 2007). However, that metaanalysis found nonsignificant effects for relationship enhancement programs that targeted couples at the transition to parenthood (it should be noted that there were only 10 such studies). These data suggest that a focus on coparenting during the transition to parenthood may facilitate positive intervention effects in comparison with those of a focus on the general couple relationship.
Moderation of Effects
An important aspect of testing intervention effects is assessing whether there are particular types of parents or families for whom the intervention was more or less beneficial. We found evidence in several cases that the program had a consistently larger effect for less educated parents. For instance, there was no main effect of intervention status on child sleep habits, but analyses demonstrated the presence of an effect for parents with low levels of education. It may be that more highly educated parents are already aware of the importance of (or strategies for) fostering regular child sleep habits. For maternal depression and mother report of coparental support, there was a main effect for intervention status, but the impact was especially strong for mothers with lower levels of education. These findings allay concerns that the program was best appreciated by more educated parents. Given that low education is a risk factor for marital dissolution, these results suggest that the benefits were greatest for those who needed the program most.
We also found a pattern of moderation of program impact for the pretest measure of parent attachment insecurity in close relationships. In this case, it appears that father’s insecurity is a salient preexisting characteristic that influences which mothers and fathers would benefit most from the program. As for education, the results indicate that those families most at risk because of a high level of father’s attachment insecurity were the ones that benefited most.
The importance of father’s insecurity does not seem to be due to greater overall insecurity among fathers than among mothers (see Table 1). Instead, the explanation may be related to the crucial importance of paternal support for mothers during the enormous physical and emotional strains of pregnancy, birth, and breast-feeding. Although coparenting is a mutual process of negotiation and coordination, we recognize a degree of asymmetry—especially during the transition period—regarding each parent’s needs, responsibilities, and strains. Attachment insecurity would compromise a father’s ability to provide support to a partner for an extended period without receiving a similar level of support in return. Thus, families in which fathers have high levels of insecurity may benefit most from the preparation offered by a program such as FF.
Limitations and Conclusion
There are several limitations to this study. The constructs targeted by the program do show intervention effects, yet we cannot rule out the possibility that generic features of the program—such as attention and time together as a couple—or demand characteristics evoked by program participation were responsible for the changes. This study does not inform us about the active ingredients in the program condition or whether simply spending more time together or participating in a support group without specific content might have similar effects. However, positive relations between session attendance and outcomes support the notion that something about the experience of the program is responsible for the effects. Further study with a comparison group that receives a similar program experience, but with different content, could help elucidate the active ingredients. Moreover, further research could disentangle the role of program content from the mode of delivery (e.g., group format vs. home study materials). Similarly, given the moderate association between the quality of coparenting and the overall couple relationship, we cannot firmly rule out the possibility that the primary effect was on the general couple relationship. A future follow-up wave of data, in which we collect self-report and observational data on both the coparental relationship and the general couple relationship, will allow an investigation of this issue.
We did not assess whether program impact on coparenting mediated impact on other constructs. In future work, we plan to collect follow-up data that will allow us to assess longitudinal mediational questions (for example, whether long-term effects on parenting or child outcomes are explained by program impact on coparenting at posttest). In addition, although the sample had a range of education and income, the majority of participants were well educated and middle class. This feature of the sample is in part a result of the eligibility requirements for the study, which excluded young teen parents and parents who were not cohabiting or married. We do not know if the program would have similar impact with a sample that had different characteristics. For example, the results that suggest moderation by education suggest that program impact may be larger with a sample with lower socioeconomic status; however, we cannot rule out the possibility that the impact would be smaller. We are currently pursuing research with an adapted version of the FF program that would be appropriate for low-income participants who are not living together.
With these limitations in mind, we believe these results suggest that it is possible to foster positive coparenting among first-time parents by utilizing a modest dosage of a universal psychosocial program. Assignment to the FF program condition had a positive impact on maternal depression and anxiety, on father’s (and to some extent mother’s) distress in the relationship with the child, and even on infant regulation. Moreover, a program such as FF may be particularly valuable for families at elevated risk during the transition period—whether because of low parental education or a high level of father’s attachment insecurity. If the results of this experiment are replicated and extended, strong evidence would accumulate in favor of the view that the coparenting relationship plays a central, causal role in guiding the course of family relationships and thus in influencing the well-being of both parents and children.
Acknowledgments
This study was funded by National Institute of Child Health and Development Grant 1 K23 HD042575 and by National Institute of Mental Health Grant R21 MH064125-01 to Mark E. Feinberg, principal investigator. We are grateful to the families who participated in this study. We appreciate the assistance of Karen Newell, Sherry Turchetta, and Carole Brtalik in implementing the program. We thank Jesse Boring, Megan Goslin, Carmen Hamilton, Richard Puddy, Carolyn Ransford, and Samuel Sturgeon for their assistance in conducting this study. George Howe and Mark Greenberg provided thoughtful advice and support.
Contributor Information
Mark E. Feinberg, Prevention Research Center, Pennsylvania State University
Marni L. Kan, Human Development and Family Studies, Pennsylvania State University
References
- Abidin RR. Parenting Stress Index: A measure of the parent–child system. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: A book of resources. Lanham, MD: Scarecrow Press; 1997. pp. 277–291. [Google Scholar]
- Abidin RR, Brunner JF. Development of a Parenting Alliance Inventory. Journal of Clinical Child Psychology. 1995;24(1):31–40. [Google Scholar]
- Bearss KE, Eyberg S. A test of the parenting alliance theory. Early Education & Development. 1998;9(2):179–185. [Google Scholar]
- Belsky J, Pensky E. Marital change across the transition to parenthood. Marriage & Family Review. 1988;12(3–4):133–156. [Google Scholar]
- Belsky J, Putnam S, Crnic K. Coparenting, parenting, and early emotional development. In: McHale JP, Cowan PA, editors. Understanding how family-level dynamics affect children’s development: Studies of two-parent families. New directions for child development, No. 74. San Francisco: Jossey-Bass; 1996. pp. 45–55. [DOI] [PubMed] [Google Scholar]
- Belsky J, Woodworth S, Crnic K. Trouble in the second year: Three questions about family interaction. Child Development. 1996;67:556–578. [PubMed] [Google Scholar]
- Bendig AW. The development of a short form of the Manifest Anxiety Scale. Journal of Consulting Psychology. 1956;20:384. doi: 10.1037/h0045580. [DOI] [PubMed] [Google Scholar]
- Cowan CP, Cowan PA. When partners become parents: The big life change for couples. New York: Basic Books; 1992. [Google Scholar]
- Cowan CP, Cowan PA. Interventions to ease the transition to parenthood: Why they are needed and what they can do. Family Relations: Journal of Applied Family & Child Studies. 1995;44(4):412–423. [Google Scholar]
- Crnic K, Greenberg MT. Maternal stress, social support, and coping: Influences on the early mother–infant relationship. In: Boukydis CFZ, editor. Research on support for parents and infants in the postnatal period. Norwood, NJ: Ablex; 1987. pp. 25–40. [Google Scholar]
- Crowne DP, Marlow D. The approval motive. New York: Wiley; 1964. [Google Scholar]
- Duvall EC. Marriage and family development. Philadelphia: Lippincott; 1977. [Google Scholar]
- Feinberg M. Coparenting and the transition to parenthood: A framework for prevention. Clinical Child & Family Psychology Review. 2002;5:173–195. doi: 10.1023/a:1019695015110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg M. The internal structure and ecological context of coparenting: A framework for research and intervention. Parenting: Science and Practice. 2003;3:95–132. doi: 10.1207/S15327922PAR0302_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg M, Kan ML, Hetherington EM. Longitudinal study of coparenting conflict on adolescent maladjustment. Journal of Marriage and Family. 2007;69:687–702. doi: 10.1111/j.1741-3737.2007.00400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Neiderhiser JM, Reiss D, Hetherington EM. Differential association of family subsystem negativity on siblings’ maladjustment: Using behavior genetic methods to test process theory. Journal of Family Psychology. 2005;19:601–610. doi: 10.1037/0893-3200.19.4.601. [DOI] [PubMed] [Google Scholar]
- Field TM. Infants of depressed mothers. In: Johnson SL, Hayes AM, editors. Stress, coping, and depression. Mahwah, NJ: Erlbaum; 2000. pp. 3–22. [Google Scholar]
- Floyd FJ, Zmich DE. Marriage and parenting partnership: Perceptions and interactions of parents with mentally retarded and typically developing children. Child Development. 1991;62:1434–1448. [PubMed] [Google Scholar]
- Frank SJ, Olmstead CL, Wagner AE, Laub CC. Child illness, the parenting alliance, and parenting stress. Journal of Pediatric Psychology. 1991;16(3):361–371. doi: 10.1093/jpepsy/16.3.361. [DOI] [PubMed] [Google Scholar]
- Frosch CA, Mangelsdorf SC, McHale JL. Marital behavior and the security of preschooler–parent attachment relationships. Journal of Family Psychology. 2000;14:144–161. doi: 10.1037//0893-3200.14.1.144. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behavior & Development. 2003;26(1):64–86. [Google Scholar]
- Glazier RH, Elgar FJ, Goel V, Holzapfel S. Stress, social support and emotional distress in a community sample of pregnant women. Journal of Psychosomatic Obstetrics & Gynecology. 2004;25(3–4):247–255. doi: 10.1080/01674820400024406. [DOI] [PubMed] [Google Scholar]
- Gonzales NA, Pitts SC, Hill NE, Roosa MW. A mediational model of the impact of interparental conflict on child adjustment in a multiethnic, low-income sample. Journal of Family Psychology. 2000;14:365–379. doi: 10.1037//0893-3200.14.3.365. [DOI] [PubMed] [Google Scholar]
- Griffin DW, Bartholomew K. Models of the self and other: Fundamental dimensions underlying measures of adult attachment. Journal of Personality and Social Psychology. 1994;67(3):430–445. [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the Parenting Stress Index— Short Form. Journal of Clinical Child and Adolescent Psychology. 2006;35(2):302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Hawkins A. Is marriage and relationship education effective? A comprehensive meta-analysis; Paper presented at the annual conference of the Society for Prevention Research; Washington, DC. 2007. May, [Google Scholar]
- Howe GW, Levy ML, Caplan RD. Job loss and mental health: Models of individual- and couple-level effect. 1999 Submitted for publication. [Google Scholar]
- Kaitz M, Maytal H. Interactions between anxious mothers and their infants: An integration of theory and research findings. Infant Mental Health Journal, Special Issue: Angels in the Nursery. 2005;26(6):570–597. doi: 10.1002/imhj.20069. [DOI] [PubMed] [Google Scholar]
- Margolin G. Co-Parenting Questionnaire. University of Southern California; 1992. Unpublished manuscript. [Google Scholar]
- Margolin G, Gordis EB, John RS. Coparenting: A link between marital conflict and parenting in two-parent families. Journal of Family Psychology. 2001;15(1):3–21. doi: 10.1037//0893-3200.15.1.3. [DOI] [PubMed] [Google Scholar]
- McHale JP. Coparenting and triadic interactions during infancy: The roles of marital distress and child gender. Developmental Psychology. 1995;31:985–996. [Google Scholar]
- McHale JP. Overt and covert coparenting processes in the family. Family Process. 1997;36(2):183–201. doi: 10.1111/j.1545-5300.1997.00183.x. [DOI] [PubMed] [Google Scholar]
- McHale JP, Kuersten-Hogan R, Lauretti A. Evaluating coparenting and family-level dynamics during infancy and early childhood: The Coparenting and Family Rating System. In: Kerig PK, Lindahl KM, editors. Family observational coding systems: Resources for systemic research. Mah-wah, NJ: Erlbaum; 2001. pp. 151–170. [Google Scholar]
- McHale JP, Kuersten-Hogan R, Lauretti A, Rasmussen JL. Parental reports of coparenting and observed coparenting behavior during the toddler period. Journal of Family Psychology. 2000;14(2):220–236. doi: 10.1037//0893-3200.14.2.220. [DOI] [PubMed] [Google Scholar]
- McHale JP, Kuersten-Hogan R, Rao N. Growing points for coparenting theory and research. Journal of Adult Development, Special Issue: Coparenting. 2004;11(3):221–234. doi: 10.1023/B:JADE.0000035629.29960.ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minuchin S, Rosman B, Baker L. Psychosomatic families. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- Morsbach SK, Prinz RJ. Understanding and improving the validity of self-report of parenting. Clinical Child and Family Psychology Review. 2006;9(1):1–21. doi: 10.1007/s10567-006-0001-5. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Ben-Shlomo Y, Heron J, Golding J, Adams D, Glover V. Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biological Psychiatry. 2005;58(3):211–217. doi: 10.1016/j.biopsych.2005.03.032. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Swain AM. Rates and risk of post-partum depression—a meta-analysis. Intternational Review of Psychiatry. 1996;8:37–54. [Google Scholar]
- Ooms T, Wilson P. The challenges of offering relationship and marriage eduation to low-income populations. Family Relations. 2004;53:440–447. [Google Scholar]
- Papousek M, von Hofacker N. Persistent crying in early infancy: A non-trivial condition of risk for the developing mother-infant relationship. Child: Care, Health and Development. 1998;24(5):395–424. doi: 10.1046/j.1365-2214.2002.00091.x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index—Short Form (PSI-SF) in a Head Start population. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Rodriguez CM, Green AJ. Parenting stress and anger expression as predictors of child abuse potential. Child Abuse & Neglect. 1997;21(4):367–377. doi: 10.1016/s0145-2134(96)00177-9. [DOI] [PubMed] [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. Journal of Clinical Psychiatry. 2006;67(8):1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Posner MI, Kieras J. Temperament, attention, and the development of self-regulation. In: McCartney K, Phillips D, editors. Blackwell handbook of early childhood development. Malden, MA: Blackwell; 2006. pp. 338–357. [Google Scholar]
- Sanders MR, Nicholson JM, Floyd FJ. Couples’ relationships and children. In: Halford WK, Markman HJ, editors. Clinical handbook of marriage and couples interventions. Chichester, England: Wiley; 1997. pp. 225–253. [Google Scholar]
- Schoppe SJ, Mangelsdorf SC, Frosch CA. Coparenting, family process, and family structure: Implications for preschoolers’ externalizing behavior problems. Journal of Family Psychology. 2001;15:526–545. doi: 10.1037//0893-3200.15.3.526. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Hayden LC. Parental psychopathology and sleep variation in children. Child and Adolescent Psychiatric Clinics of North America. 1996;5(3):715–727. [Google Scholar]
- Sepa A, Frodi A, Ludvigsson J. Psychosocial correlates of parenting stress, lack of support and lack of confidence/ security. Scandinavian Journal of Psychology. 2004;45(2):169–179. doi: 10.1111/j.1467-9450.2004.00392.x. [DOI] [PubMed] [Google Scholar]
- Stifter CA, Bono MA. The effect of infant colic on maternal self-perceptions and mother-infant attachment. Child: Care, Health and Development. 1998;24(5):339–351. doi: 10.1046/j.1365-2214.2002.00088.x. [DOI] [PubMed] [Google Scholar]
- Taylor JA. A personality scale of manifest anxiety. Journal of Abnormal and Social Psychology. 1953;48:285–290. doi: 10.1037/h0056264. [DOI] [PubMed] [Google Scholar]
- Teti DM, O’Connell MA, Reiner CD. Parenting sensitivity, parental depression and child health: The mediational role of parental self-efficacy. Early Development & Parenting. 1996;5(4):237–250. [Google Scholar]
- Tice DM. Self-concept change and self-presentation: The looking glass self is also a magnifying glass. Journal of Personality and Social Psychology. 1992;63(3):435–451. doi: 10.1037//0022-3514.63.3.435. [DOI] [PubMed] [Google Scholar]
- Van der Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms. A review. Neuroscience & Biobehavioral Reviews. 2005;29(2):237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Van Egeren LA. The development of the coparenting relationship over the transition to parenthood. Infant Mental Health Journal, Special Issue: Amsterdam World Congress: Plenary Papers. 2004;25(5):453–477. [Google Scholar]
- Walther VN. Postpartum depression: A review for perinatal social workers. Social Work in Health Care. 1997;24:99–111. doi: 10.1300/J010v24n03_08. [DOI] [PubMed] [Google Scholar]
- Weissman S, Cohen RS. The parenting alliance and adolescence. Adolescent Psychiatry. 1985;12:24–45. [PubMed] [Google Scholar]