Abstract
Background:
Alopecia areata (AA) shows several well-defined dermoscopic features which may help in confirming diagnosis in AA.
Aims:
We carried out a study to examine the dermoscopic features of AA and develop a protocol for diagnosis of AA by dermoscopy.
Materials and Methods:
Dermoscopy was performed in 66 patients with AA. Hanse HVS-500NP dermoscope (magnification of ×32 and ×140) was used.
Results:
The mean age of the patients (46 males and 20 females) was 26.85 years. The mean age of onset was 25.15 years. The mean duration of alopecia was 10.3 months. Most common AA in our study was patchy type (57/66, 87.7%). Single patch was seen in 24 patients and multiple patches in 33 patients. Diffuse AA was seen in five patients. Ophiasis and alopecia universalis were seen in two patients each. Nail changes were fine pitting (4), ridging (2), thinning of nail plate (2). Twenty nail dystrophy, distal onycholysis, striate leukonychia and coarse pitting were seen in one patient each. Intralesional triamcinolone acetonide was the most common therapy offered. Others were oral betamethasone minipulse therapy, dexamethasone pulse, minoxidil, anthralin and corticosteroids. The most common dermoscopic finding was yellow dots seen in 54 patients (81.8%), followed by black dots (44 patients, 66.6%), broken hairs (36 patients, 55.4%), short vellus hair (27 patients, 40.9%) and tapering hairs (8 patients, 12.1%).
Conclusions:
The most common dermoscopic finding of AA in our study was yellow dots, followed by black dots, broken hairs, short vellus hair and tapering hairs. Dermoscopic findings were not affected by the type of AA or the severity of the disease.
Keywords: Alopecia areata, black dots, dermoscopy, tapering hair, yellow dots
Introduction
Alopecia areata (AA) is a common, nonscarring, autoimmune, chronic, inflammatory disease involving hair follicles, characterized by hair loss on the scalp and/or body.[1] Clinically, the disease manifests as patchy alopecia, diffuse alopecia, reticulate alopecia, ophiasis, ophiasis inversus, alopecia totalis (loss of all the scalp hairs), or alopecia universalis (loss of hair all over the body).[1,2] Nail changes (diffuse fine pitting, longitudinal ridging, thin and brittle fingernails and toenails, and trachyonychia) may be seen in 3–30% of patients.[3]
In general, clinical diagnosis of AA is made based on typical pattern of hair loss, which can be supported by the presence of characteristic exclamation mark hair in microscopy. However, in some cases, the clinical diagnosis may not be straightforward, and in such cases, invasive (punch biopsy) techniques are often required, which are frequently not well accepted by patients, especially children.[4] Acute diffuse AA, also known as alopecia areata incognita, presents like acute telogen effluvium causing great diagnostic difficulty.[5,6]
Dermoscopy is a non-invasive procedure which was initially used to assess pigmented lesions. Recent studies have shown that dermoscopy can be a useful tool for the clinical diagnosis of AA by the presence of cadaverized hairs (black dots), exclamation mark hairs (tapering hairs), broken hairs, yellow dots and clustered short vellus hairs in the hair loss areas.[5]
We carried out a study to examine the dermoscopic features of AA and develop a protocol for diagnosis of AA by dermoscopy.
Materials and Methods
Dermoscopic analysis of AA was carried out in 66 patients. Diagnosis of AA was clinically established and ambiguous cases were confirmed by scalp biopsy. In all patients, the clinical diagnosis was made by standard clinical observation, positive trichograms, positive pull test carried out in the involved areas, and past family history.
Hanse HVS-500NP dermoscope (magnification of ×32 and ×140) was used. Oil was used as the immersion fluid. Ethanol (70%) was not used because it reduces the number and size of yellow dots which are considered to be most significant dermoscopic finding of AA occurring in all stages of the disease.[6,7]
Grading of AA was done using the following scale
Scalp hair loss: S0, no hair loss; S1, <25% hair loss; S2, 26–50% hair loss; S3, 51–75% hair loss; S4, 76–99% hair loss; S5, 100% hair loss. Body hair loss: B0, no body hair loss; B1, some body hair loss; B2, 100% body (excluding scalp) hair loss. Nail involvement: N0, no nail involvement; N1, some nail involvement.
Data collected were tabulated in Microsoft Excel Spread Sheet and computer-based analysis was performed using SPSS-13 (Chicago, IL, USA).
Results
Age, gender, occupation and marital status
There were 46 males and 20 female patients. The male: female ratio was 2.3:1. The mean age of the patients was 26.85 years (SD: 9.394) with a range of 7–45 years. There were only eight children (below 14 years of age). There were 17 students, 14 laborers, 12 housewives, 4 clerks, 3 masons, 2 each of stationary shop owners, drivers and 12 others (1 patient each of attendant, cook, driver, farmer, mill worker, peon, tea vendor, milk vendor, mechanic, painter, medical transcripter, hotel worker). Out of 66 patents, 40 were married, whereas 26 were single.
Age of onset and duration of alopecia areata
The mean age of onset was 25.15 years (SD: 9.581). The mean duration of alopecia was 10.3 months (SD: 19.8) with a range of 1 week to 8 years. Prolonged disease duration was noted in both patients with universal type (duration of 5 and 8 years) and one patient with diffuse type (duration of 8 years) of AA.
Clinical types of alopecia areata
Most common type of AA in our study was patchy type (57/66, 87.7%) – single patch was seen in 24 patients (males: 19, females: 5) and multiple patches in 33 patients (males: 22, females: 11). Diffuse AA was seen in five patients (males: 2, females: 3) (6.3%). Ophiasis (males: 2, females: 0) and alopecia universalis (males: 1, females: 1) were seen in two patients each (3.1%). There was no statistically significant difference in age and age of onset among patients with different types of AA.
Sites
In patchy alopecia, 47 had scalp involvement (one each also had moustache and eyebrow involvement), and 9 had beard region involvement only. In the scalp, most common sites involved were occipital (28 patients) and parietal regions (24 patients). Other sites involved were vertex (21 patients), temporal (17 patients) and frontal (8 patients).
Grading of alopecia areata
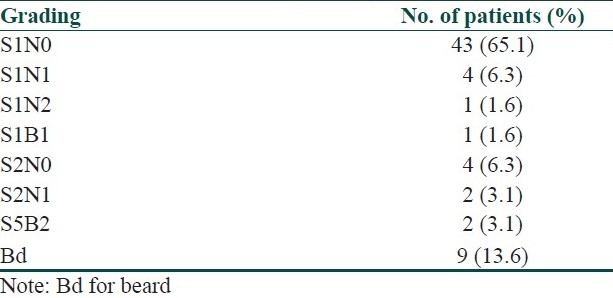
Grading of AA in our study is shown in Table 1.
Table 1.
Grading of alopecia areata
Nail changes
Fine pitting was seen in four patients; whereas ridging and thinning of nail plate were seen in two patients each. Twenty nail dystrophy, distal onycholysis, striate leukonychia and coarse pitting were seen in one patient each.
Associated systemic diseases
Autoimmune urticaria (alopecia universalis), diabetes mellitus (patchy localized AA), psoriasis vulgaris (patchy multiple AA), acanthosis nigricans (patchy multiple AA), vitiligo vulgaris (patchy multiple AA), and essential hypertension (diffuse type AA) were seen in one patient each.
Treatment and response
Intralesional triamcinolone acetonide was used for treatment in 49 patients. Oral betamethasone minipulse therapy was given in 10 patients. Dexamethasone (32 mg) pulse therapy was used in three patients. Minoxidil (2%) was tried in one patient after failure with 1 year of oral minipulse therapy. One patient was treated with topical anthralin and corticosteroids, whereas one patient was treated with only topical anthralin. Out of 34 patients who were assessed for response to treatment, good response to treatment was seen in 28 patients. Four patients showed minimal response, whereas two patients showed poor response to treatment.
Dermoscopic features
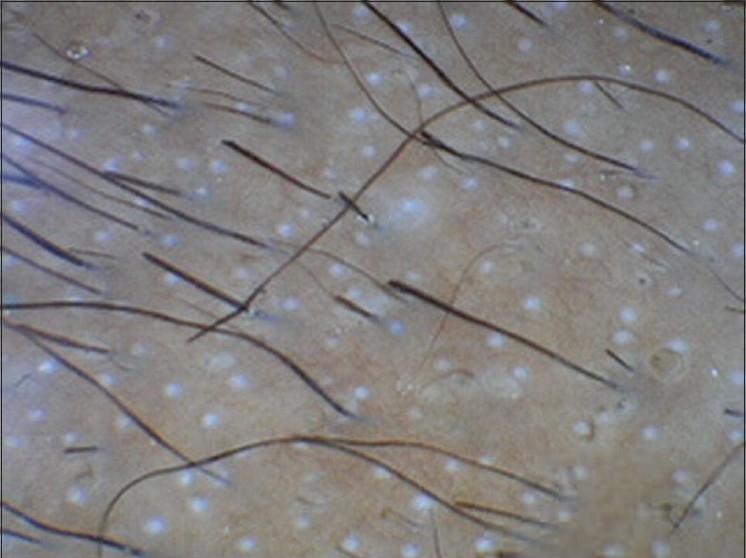
Out of 66 patients, the most common dermoscopic finding was yellow dots seen in 54 patients (81.8%), followed by black dots (44 patients, 66.6%), broken hairs (36 patients, 55.4%), short vellus hair (27 patients, 40.9%) and tapering hairs (8 patients, 12.1%) [Table 2, Figures 1–5]. Short vellus hairs with increased proximal diameter and pigmentation were seen in 17 out of 27 patients. Analysis of variance (ANOVA) test done to examine any statistically significant difference in the mean age of the patients, age of onset, mean duration of alopecia and extent of involvement between those patients showing a certain dermoscopic feature and those not showing it, revealed negative results in all groups, except in the case of duration of AA among patients showing broken hairs. The mean duration of disease in patients showing broken hairs in dermoscopy was 5.31 months and that in those not showing broken hairs was 16.33 months, and this difference was statistically significant (P = 0.023). No dermoscopic feature was significantly more common in any clinical type of AA (Chi-square test). By Spearman rank-order correlation test, no statistically significant positive or negative correlation was found between the severity of the disease and any one of the dermoscopic features. Other findings were red loops and beading of hair shaft (pseudomonilethrix) seen in two patients each.
Table 2.
Dermoscopic findings in alopecia areata
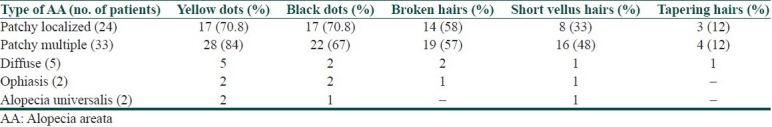
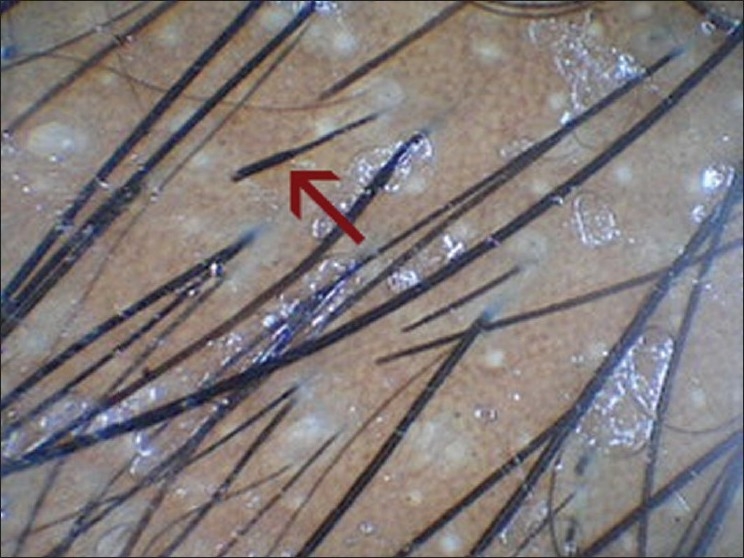
Figure 1.

Yellow dots
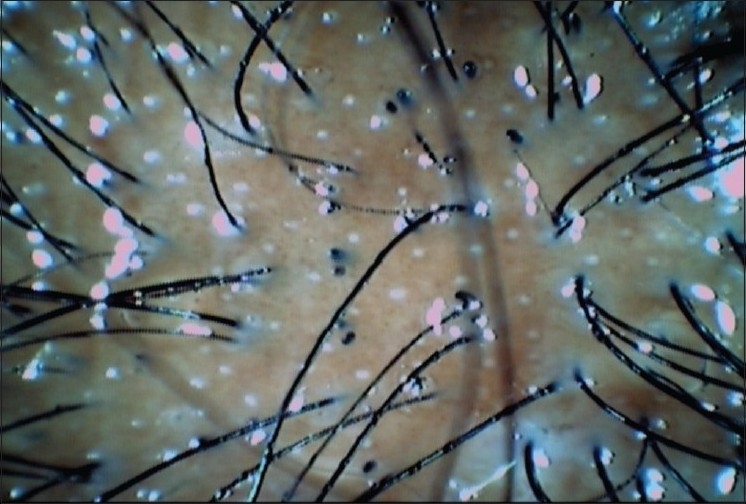
Figure 5.
Tapering hairs
Figure 2.
Black dots
Figure 3.
Broken hairs
Figure 4.
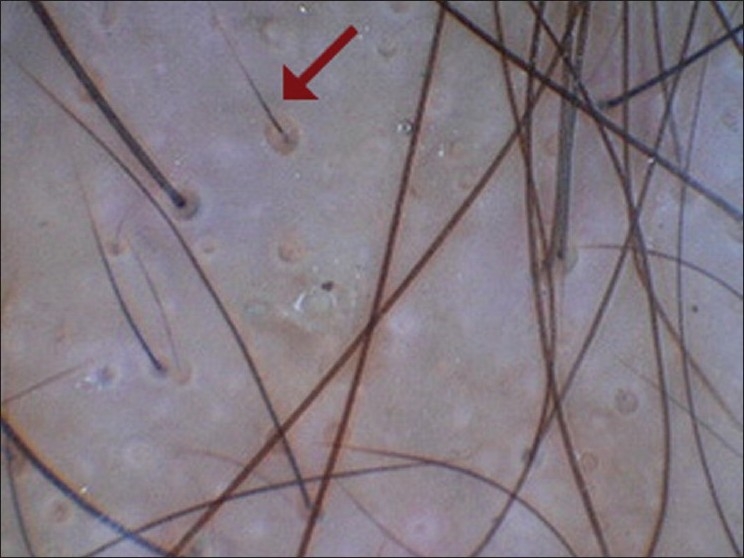
Short vellus hair (with increased proximal diameter and pigmentation)
Discussion
Dermoscopy has recently become a useful diagnostic tool for AA, especially in doubtful cases. Yellow dots, black dots, broken hairs, tapering hairs, and short vellus hairs are considered as characteristic dermoscopic features in AA.[2,8]
Yellow dots, initially proposed by Ross et al., are considered to be the most sensitive dermoscopic feature of AA. These are marked by distinctive array of yellow to yellow-pink, round or polycyclic dots that vary in size and are uniform in color.[6,7] These represent distension of affected follicular infundibulum with keratinous material and sebum.[2] Ross et al.[7] demonstrated yellow dots in 94.8% patients (55 out of 58 patients). Inui et al.,[2] however, noted yellow dots in 63.7% (191 of 300 patients) of AA cases. The incidence of yellow dots in our study was 81.8%. However, yellowish skin color of Asian patients may make it more difficult to perceive yellow color in dermoscopy.[2]
“Tapering hair” (this term is preferred over “exclamation mark hair” because the affected hair is not typical exclamatory mark in shape) is commonly seen in AA.[2] The narrowing of hair shafts toward the follicles is more readily perceived using dermoscopy than by naked eye. Inui et al.,[2] demonstrated tapering hairs in 31.7% (95 out of 300 cases) of alopecia cases. In our study, tapering hairs were seen in 12.1% (8 of 66 patients). Broken hairs, also considered to be similarly produced dystrophic hairs, are clinical markers of the disease activity and severity of AA.[2] Inui et al.,[2] demonstrated broken hairs in 45.7% (137 out of 300 cases) of alopecia cases, which is comparable to our finding (55.4% of cases had broken hairs in our study). Frequency of broken hairs, however, was much higher (95%, 19 out of 20 patients) in another study of “acute diffuse and total alopecia of female scalp”.[5]
Black dots as remnants of exclamation mark hairs or broken hairs provide a sensitive marker for disease activity as well as severity of AA.[2] However, this finding is not readily appreciable in the White population. Inui et al.,[2] demonstrated black dots in 44.3% (133 out of 300 cases) of AA cases. In our study, black dots were seen in 67.7% (44 of 66 patients).
Short vellus hair is also a diagnostic feature of AA, which can provide useful prognostic information as well (indicates the non-destructive nature of AA). The regrowth of short vellus hairs after treatment can easily be seen in dermoscopy,[5] even when the recovered hairs are hardly visible by naked eye. These are seen as new, thin, and unpigmented hairs within the patch (which may or may not be detectable clinically).[4] Vellus hairs may be straight or thin and twisted which are usually lost in a few weeks.[4] The pigmented skin of Asian patients helps in easy detection of vellus hairs.[2] White dots were considered as sites of targeted follicular destruction, i.e., fibrosis. These are seen in cicatricial alopecia as well as long standing AA.[8]
Some of the dermoscopic features can be used to predict the activity and severity of AA. Tapering hair is considered as a marker of disease activity and known to reflect exacerbation of disease.[2] Inui et al.,[2] reported that black dots, tapering hairs, and broken hairs correlated positively with disease activity. They also noted that black dots and yellow dots correlated positively with the severity of AA. Short vellus hairs correlated negatively with both disease activity and severity. No correlation was found between tapering hair and severity of the disease, which was probably due to the fact that tapering hairs are dystrophic hair produced by the least severely affected follicles of AA.[2] The presence of “vellus” hairs, as well as a sign of the transformation of vellus into terminal hairs (appearing as increased proximal shaft thickness and pigmentation), also indicates a good prognosis.[4] Ross et al.[7] found that occurrence of yellow dots did not depend on AA type and activity. Yellow dots and short vellus hairs appear to be more sensitive marker of diffuse type of AA (also known as alopecia areata incognita).[5] In our study, with one exception (the mean duration of disease in patients showing broken hairs was significantly shorter than those not showing them in dermoscopy), dermoscopic findings were independent of the mean age of the patients, mean duration of alopecia, extent of involvement, type and severity of AA. However, a larger sample size would be desirable to draw significant statistical conclusions.
Thus, these dermoscopic findings will be helpful for management of patients with hair disorders. The yellow dots and short vellus hairs enable AA to be screened from other hair loss disorders. Abundant numbers of the yellow dots seen in AA can differentiate from androgenetic alopecia, female androgenetic alopecia and trichotillomania which can have limited number of yellow dots.[2,5] In addition, black dots, tapering hairs and broken hairs are specific for AA, except for trichotillomania.[2] Single dermoscopic feature may not reliably diagnose AA. Inui et al. found that a combination of cadaverized hairs, exclamation mark hairs, broken hairs and yellow dots could sensitively detect difficult-to-clinically-diagnose types of AA like alopecia areata incognita (black dots resembling cadaverized hairs and broken hairs may be found in tinea capitis and trichotillomania).[5] Inui et al.[2] reported that yellow dots in combination with short vellus hairs provide sensitive clues to the diagnosis of AA, especially diffuse type of AA.
To conclude, the most common dermoscopic finding of AA in our study was yellow dots, followed by black dots, broken hairs, short vellus hair and tapering hairs. Dermoscopic findings were not affected by the type of AA or the severity of the disease.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Wasserman D, Guzman-Sanchez DA, Scott K, McMichael A. Alopecia areata. Int J Dermatol. 2007;46:121–31. doi: 10.1111/j.1365-4632.2007.03193.x. [DOI] [PubMed] [Google Scholar]
- 2.Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: Analysis of 300 cases. Int J Dermatol. 2008;47:688–93. doi: 10.1111/j.1365-4632.2008.03692.x. [DOI] [PubMed] [Google Scholar]
- 3.Papadopoulos AJ, Schwartz RA, Janniger CK. Alopecia areata. Pathogenesis, diagnosis, and therapy. Am J Clin Dermatol. 2000;1:101–5. doi: 10.2165/00128071-200001020-00004. [DOI] [PubMed] [Google Scholar]
- 4.Lacarrubba F, Dall’Oglio F, Rita Nasca M, Micali G. Videodermatoscopy enhances diagnostic capability in some forms of hair loss. Am J Clin Dermatol. 2004;5:205–8. doi: 10.2165/00128071-200405030-00009. [DOI] [PubMed] [Google Scholar]
- 5.Inui S, Nakajima T, Itami S. Significance of dermoscopy in acute diffuse and total alopecia of the female scalp: Review of twenty cases. Dermatology. 2008;217:333–6. doi: 10.1159/000155644. [DOI] [PubMed] [Google Scholar]
- 6.Tosti A, Whiting D, Iorizzo M, Pazzaglia M, Misciali C, Vincenzi C, et al. The role of scalp dermoscopy in the diagnosis of alopecia areata incognita. J Am Acad Dermatol. 2008;59:64–7. doi: 10.1016/j.jaad.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol. 2006;55:799–806. doi: 10.1016/j.jaad.2006.04.058. [DOI] [PubMed] [Google Scholar]
- 8.Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy: A new method for diagnosing hair loss. J Drugs Dermatol. 2008;7:651–4. [PubMed] [Google Scholar]


