Abstract
Background
The US Preventive Services Task Force and the American Academy of Pediatrics recommend that physicians screen patients for obesity and practice counseling interventions to achieve modest (4%–8%) weight loss. Despite this, physicians frequently do not document obesity and/or counsel on weight loss. Our goal was to develop an innovative, easily disseminated workshop to improve resident physicians' skills and confidence in weight-loss counseling.
Methods
We developed a tailored 3-hour interactive Obesity Counseling Workshop. The approach incorporates principles of motivational interviewing, a set of listening and counseling skills designed to enhance patient centeredness and promote behavior change. Adult learning theory served as the foundation for program delivery. The half-day session is administered monthly to internal medicine and pediatric residents on outpatient rotations.
Key Results
To date 77 residents (44 internal medicine and 33 pediatric) have completed the workshop, with approximately even distribution of postgraduate year (PGY)–1, PGY-2, and PGY-3 level residents. Forty-two were women and less than half planned to pursue a primary care–oriented career. Residents completed a 10-item workshop evaluation, with each category scoring an average of 3.5 or greater on a 4-point Likert scale. Residents reported the workshop was well organized and addressed an important topic; they enjoyed the role-playing with observation and feedback.
Conclusions
Residents welcomed the opportunity to participate in an interactive workshop focused on obesity counseling and behavior change, and particularly liked putting new skills into practice with role-playing and receiving real-time feedback. Future analyses will determine the workshop's effect on knowledge, skills, and self-efficacy.
Background
Obesity places an increased burden on America's health care system, and primary care physicians are challenged with preventing and managing this epidemic. Currently, 32% of adults in the United States and 16% of children and adolescents are obese, defined by a body mass index of 30 or greater in adults and a body mass index at or above the 95th percentile for age in children and adolescents.1,2 While obesity rates have increased during the past few decades, so too have the rates of related chronic diseases. Despite this increase, there appears to be a decrease in physician diagnosis of obesity and in weight-loss recommendations.3
Physicians cite multiple barriers to obesity counseling, including a lack of training in behavior counseling, low confidence, and patient noncompliance.4 In 1 study, only 30% of primary care physicians reported being trained well in obesity management.5 At the resident level, a study found that only 26% of internal medicine residents felt well trained to counsel patients regarding obesity.6 The need for training programs that improve residents' counseling skills is concurrent with a growing focus on patient centeredness and interpersonal skills, now designated core competencies for resident education by the Accreditation Council for Graduate Medical Education (ACGME).7
To address this need, we developed and implemented an Obesity Counseling Workshop for pediatric and internal medicine residents, which incorporates key principles of motivational interviewing (MI). Motivational interviewing is a counseling technique designed to enhance patient centeredness, and it is being applied to various types of behavior-change counseling, including obesity-related behaviors.8,9 Unlike traditional patient education, MI does not rely on physicians to provide often untailored advice to their patients.10 It also explores a patient's intrinsic motivation in a directive way shown to be effective in eliciting and sustaining behavior change.11 Using MI as a framework, our goal was to create an innovative, easily disseminated Obesity Counseling Workshop to improve residents' interpersonal and lifestyle counseling skills.
Methods
Program Development
Our workshop builds on a prior educational intervention developed by Davis and colleagues9 at the Albert Einstein College of Medicine, which taught counseling techniques based on the 5 As (Assess, Advise, Agree, Assist, Arrange) and motivational interviewing to 80 internal medicine and family medicine residents. By adding regional obesity statistics, we adapted the content to be more specific for Alabama, currently ranked second in the country for obesity rates among adults.12 We also expanded the content related to MI, emphasizing patient control and exploring patients' ambivalence about change. During the program development phase, the investigators received training from experts in the field of MI13 and participated in a series of web-based seminars offered through the Institute for Motivation and Change (http://www.miinstitute.com/). By becoming proficient in MI, our team was able to adapt the workshop to incorporate key principles of MI into an interactive approach.
Program delivery was based on tenets of adult learning theory, which holds that adults will commit to learning when the goals and objectives are considered realistic, relevant, and pertinent to their personal and professional needs, and that they need activities that allow them to practice new skills and receive constructive feedback.14 We accomplished this by incorporating several opportunities for residents to practice what they learned in a safe environment through role-playing with peers and to practice with standardized patient interviews, while receiving both affirmative and constructive feedback.
To develop the content of our workshop, we formed an interdisciplinary steering committee at the outset of the project. The committee included psychologist and physician experts in obesity research and treatment, and residency program directors. The committee provided feedback on the didactic and interactive portions of the workshop. The resultant workshop was piloted with 6 pediatric and adult endocrinology faculty members and fellows and a health services researcher, and was further refined based on their feedback.
We implemented the 3-hour workshop into the residents' curriculum in pediatrics and internal medicine. In the internal medicine program, it was offered during an outpatient ambulatory block that residents have at least once each year. In pediatrics, it was offered to residents on the ambulatory pediatrics, behavior and development, and endocrinology rotations. Combined, the 3 rotations reached residents from each training level. Institutional Review Board approval was obtained for the entire project and all related protocols.
Participants and Setting
At the beginning of each month, residents scheduled for an outpatient/ambulatory month received an e-mail invitation to a 3-hour Obesity Counseling Workshop. The workshop was also included on outpatient/ambulatory schedules for the month. Workshops were scheduled in the afternoon and most residents were able to attend. Workshops were held from July 2009 to June 2010 and administered once a month separately to each group of residents (pediatric and internal medicine).
Evaluation
As residents arrived, the investigator (A.M.B.) and research assistant (A.A.A.) greeted each individual, spoke with him or her about the risks and benefits of participation, then gave each resident the opportunity to consent or decline participation. Participants were informed that if they declined to participate in the study, they were still welcome to stay for the workshop. After consent was obtained, residents completed a preworkshop questionnaire, including demographic information as well as questions targeting knowledge, attitudes, and self-efficacy about obesity counseling. At the workhop's conclusion, residents completed a postworkshop questionnaire and a workshop evaluation.
Results
Program Description
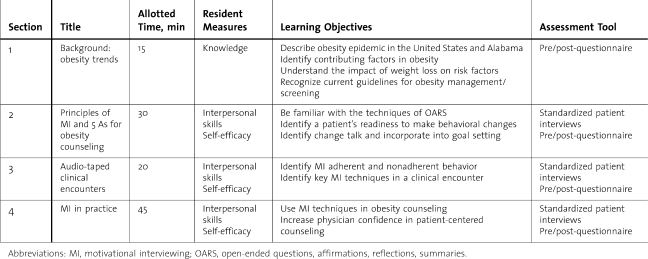
The goal of our workshop was to increase resident physicians' knowledge, self-efficacy, and interpersonal communications skills in the context of obesity counseling (table 1). Section 1 began with a didactic lecture on the national and regional obesity epidemic and its contributing factors. Current obesity guidelines, as outlined by the US Preventive Services Task Force and the American Academy of Pediatrics, and strategies for integration into practice were reviewed. Section 2 focused on the principles of motivational interviewing and communication techniques, with these principles reinforced through videos and interactive exercises aimed at increasing self-efficacy and interpersonal skills. After learning how to incorporate these techniques of MI into a clinical encounter, residents received handouts on community resources and weight-loss counseling tools. Section 3 centered on recognition of MI techniques in 2 audio taped clinical encounters.15 In section 4, residents proceeded to observed role-playing with their peers.
Table 1.
Workshop Outline
Program Evaluation: Resident Satisfaction
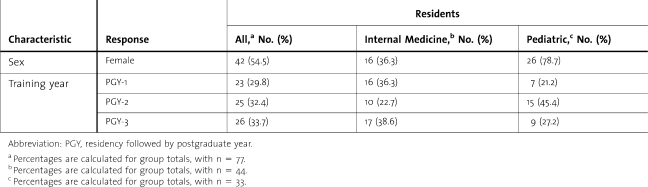
Seventy-seven resident physicians (44 internal medicine, 33 pediatric) participated in the Obesity Counseling Workshop from July 2009 to February 2010 (table 2). Forty-two were women and less than half plan to pursue a primary care–oriented career. Of residents who were able to attend the workshop, only 1 declined participation. Between 3 to 10 residents participated in each workshop. Participants completed a 10-item workshop evaluation, with each category scoring an average of 3.5 or greater on a 4-point Likert scale. The evaluation was adapted from an assessment tool used for internal medicine noon conferences at the University of Alabama at Birmingham. The tool has not been validated. More than 73% (52 of 71) of the residents who completed the evaluation wrote comments. Residents reported the workshop was well organized and addressed an important topic (15 comments). They liked the role-playing with observation and feedback during the workshop (23 comments), audiovisuals, tailored materials, and interactive activities (9 comments). Regarding what could be improved, some residents wanted more detailed notification about the session ahead of time (2 comments) and some wished the session could have been shorter (8 comments).
Table 2.
Characteristics of Participants
Discussion
Our project provided a tailored 3-hour interactive Obesity Counseling Workshop to pediatric and internal medicine residents, which was aimed at increasing their knowledge, self-efficacy, and interpersonal communications skills. Overall, the workshop was well received by the residents and most reported that the interactive components were likely to improve their obesity counseling skills. Respondents thought obesity counseling was an essential topic and liked the variety of activities involved in the workshop. Implementing the workshop into each residency curriculum required support from residency directors, faculty involved with outpatient rotations, and chief residents.
Conclusions
By addressing regional and cultural trends in our workshop, as well as incorporating several tenets of MI and adult learning theory, we responded to ACGME requirements with a culturally sensitive and experiential curriculum. Since the workshop focused on effective patient-centered counseling, the skills acquired are transferable to other areas of health promotion that often require behavior change, such as smoking cessation, medication compliance, and substance abuse cessation.
Dissemination of the workshop to other residencies will require leadership from faculty with some working knowledge of basic principles of motivational interviewing. Faculty unfamiliar with MI could be trained through online webinars or by attending conferences held by the Motivational Interviewing Network of Trainers.8 Access to the materials needed for the workshop are available at http://www.uab.edu/gim/education/default.html under the “Patient-Centered Obesity Counseling” link. Once familiar with the materials for the workshop, the time required by a faculty member trained in the basics of MI would be limited to leading the 3-hour workshop.
Future research will include studying the impact of our Obesity Counseling Workshop on residents' knowledge, self-efficacy, counseling, and interpersonal skills. We also plan to measure counseling skills with the audio taped standardized patient interviews before, immediately after, and 4 months after the workshop.
Footnotes
Amy M. Burton, MD, is Faculty Physician, Department of Pediatrics, Division of Endocrinology, UT Southwestern Medical Center; April A. Agne, MPH, is Program Manager, Division of Preventive Medicine, School of Medicine, University of Alabama at Birmingham; Stephanie M. Lehr, MPH, is a student in the School of Public Health, University of Alabama at Birmingham; Nichola J. Davis, MD, is Faculty Physician at the Albert Einstein College of Medicine; Lisa L. Willett, MD, is Faculty Physician in the Division of General Internal Medicine, School of Medicine, University of Alabama at Birmingham; and Andrea L. Cherrington, MD, MPH, is Faculty Physician in the Division of Preventive Medicine, School of Medicine, University of Alabama at Birmingham.
Funding: The project was supported by grants from the University of Alabama Birmingham Health Services Foundation Graduate Education Fund; the Robert Wood Johnson Physician Faculty Scholars' Program; and the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, UAB Diabetes Research and Training Center. The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
This work was made possible by grants from the University of Alabama Birmingham Health Services Foundation Graduate Education Fund; the Robert Wood Johnson Physician Faculty Scholars' Program [047948] (A.L.C.); and the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, UAB Diabetes Research and Training Center [1P60DK079626- 01] (A.L.C.).
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 3.Abid A, Galuska D, Khan LK, Gillespie C, Ford ES, Serdula MK. Are healthcare professionals advising obese patients to lose weight: a trend analysis. MedGenMed. 2005;7(4):10. [PubMed] [Google Scholar]
- 4.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 5.Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7(1):35. doi: 10.1186/1471-2296-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adimoolam V, Charney P. Identification and management of overweight and obesity by internal medicine residents: Christopher B. Ruser, Lisa Sanders et al. J Gen Intern Med. 2006;21(10):1128. doi: 10.1111/j.1525-1497.2006.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ACGME. New program requirements, 2007. http://acgme.org/acWebsite/dutyHours/dh_dutyhoursCommonPR07012007.pdf. Accessed August 31, 2011. [Google Scholar]
- 8.Wagner CC. Ingersoll KS. Beyond behavior: eliciting broader change with motivational interviewing. Journal of Clinical Psychology. 2009;65(11):1180–1194. doi: 10.1002/jclp.20639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis N, Schechter C, Wylie-Rosett J. Effect of resident education and clinic reminders on resident management of obesity. New York City RING Convocation; 2007; New York, NY. [Google Scholar]
- 10.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- 11.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. U.S. obesity trends, 2008. http://www.cdc.gov/obesity/data/trends.html. Accessed August 18, 2010. [Google Scholar]
- 13.Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. The Motivational Interviewing Treatment Integrity (MITI) Code 3. Albuquerque, NM: 2007. [Google Scholar]
- 14.Speck M. Best practice in professional development for sustained educational change. ERS Spectrum. 1996:33–41. [Google Scholar]
- 15.Kenneth Resnicow. BMi2: Brief Motivational Interviewing to Reduce Body Mass Index [DVD] Ann Arbor, MI: 2009. PhD. University of Michigan School of Public Health. [Google Scholar]