Abstract
Background
In 2007, Weill Cornell Medical College (WCMC) began annually to send approximately 30 residents in internal medicine and pediatrics to Bugando Medical Center in Mwanza, Tanzania, where they were supervised and mentored by 2 full-time WCMC faculty physicians.
Objective
To describe the components of the WCMC global health elective and to evaluate the experiences of the participants.
Methods
Subjects were WCMC residents in internal medicine and pediatrics from the graduating classes of 2007–2009. Electronic surveys were sent to all participants (n = 57) and to a group of nonparticipants (n = 57).
Results
Overall response rate was 58%. The most-selected, primary reasons for participation in the program were an interest in global health and a desire to serve an underprivileged population. Participants rated use of routine laboratory tests in the United States as more overused than did nonparticipants (P = .01). After the elective, 62% of participants reported a reduced use of laboratory and/or radiologic tests. All participants (100%; 39 of 39) reported the elective as having a positive effect on their knowledge of international health and tropical medicine. More than 90% of participants (36 of 39) reported the elective as having a positive effect on their physical examination skills.
Conclusions
Participants of the WCMC global health elective report positive experiences from our multidimensional global health collaboration.
Background
Since its inception in 2007, the Weill Cornell Medical College (WCMC) global health elective has been popular among internal medicine and pediatric residents. We describe the components of the WCMC global health elective and evaluate (1) the experiences of the participants, (2) the determinants for participation, and (3) whether there are differences between residents who did or did not participate in the global health elective.
WCMC Global Health Elective
In 2006, WCMC and New York Presbyterian Hospital established a formal affiliation with the Bugando Medical Center (BMC) and the Weill Bugando University College of Health Sciences in Mwanza, Tanzania.1 The goal of this multidimensional and multidepartmental partnership was to create a mutually beneficial relationship, including the bilateral exchange of faculty, residents, and students between the 2 institutions. Starting January 2007, WCMC began sending approximately 30 residents in internal medicine and pediatrics to BMC each year, along with placing 2 full-time WCMC faculty physicians to teach and supervise training at BMC.
The WCMC global health elective is a 6-week rotation for residents in internal medicine and a 4-week rotation for residents in pediatric medicine. Before departure, residents attend an orientation meeting, receive vaccines, and communicate with prior participating residents and the WCMC faculty physicians at BMC. During the elective, residents attend morning report; participate in rounds on the hospital wards with the BMC physicians, residents, and medical students; and assist in teaching at the host institution. The onsite WCMC faculty physicians are able to provide supervision and mentorship during the elective to maximize the learning experience for the residents. At the end of the elective, residents attend a debriefing with the onsite faculty physicians and complete an evaluation form.
Approximately 20 internal medicine and 10 pediatric, international rotation appointments are available each year for primarily third-year residents. There are 43 residents in internal medicine and 20 residents in pediatrics who participate in the elective per graduating class. Since its inception, there have been more applicants than spots available.
The elective is funded through the support of the Touch Foundation and private grants, which covers the cost of vaccines and visa ($500) and the round-trip airfare ($2000). Participants pay for room and board ($20/d).
Methods
Study Population
The study population was WCMC residents in internal and pediatric medicine from the graduating classes of 2007–2009. Two study groups were identified: residents who had participated in the elective (PAR) and residents who declined to participate in the elective (NON).
Survey Instrument
A survey was adapted with permission from faculty at Duke University, who had used it to look at the effect of the Duke University Internal Medicine Residency International Health Program.2 Modifications of the survey were performed by the authors to fit the WCMC global health elective.
Survey Procedure
All participants of the elective from January 2007 to February 2009 were sent an electronic survey in February 2009 (PAR = 57) including 3 pediatric fellows who participated in the elective. At the same time, an electronic survey was sent to a group of randomly chosen nonparticipants (NON = 57). After 1 month, a reminder e-mail was sent to all nonrespondents. Confidentiality of responses was maintained.
Statistical Analysis
Comparison of results between the PAR and NON group were performed using a χ2 test and multivariate analysis of variance. Level of statistical significance was reduced to P ≤ .01 because of multiple comparisons.
The study was approved by the WCMC Institutional Review Board (protocol 0810010030).
Results
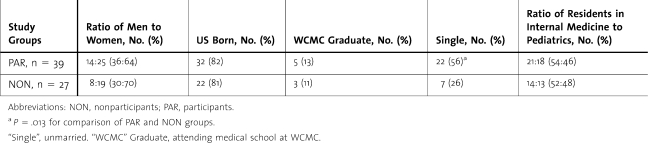
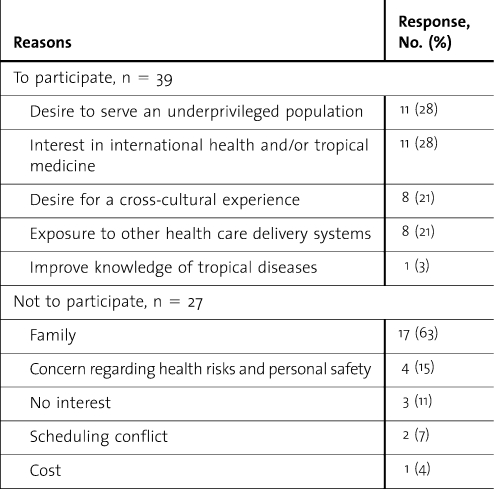
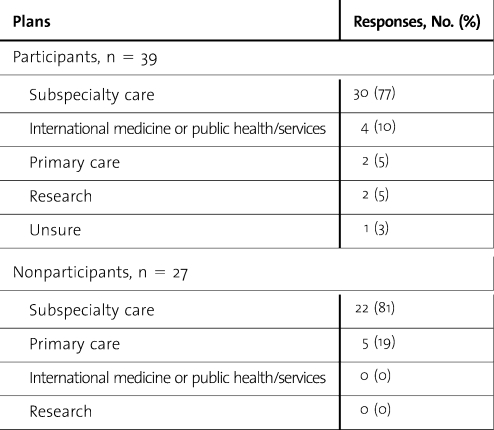
Response rate was 68% (39 of 57) for the PAR group and 47% (27 of 57) for the NON group. Demographic information between the PAR and NON group is summarized in table 1. The most selected, primary reasons for participation and nonparticipation are listed in table 2. Career plans 10 years after completion of residency for residents in both groups are summarized in table 3.
Table 1.
Demographic Information on Study Groups
Table 2.
Selected Primary Reasons to Participate or Not to Participate in the Weill Cornell Medical College Global Health Elective
Table 3.
Participant and Nonparticipant Career Plans 10 Years After Completion of Residency Training
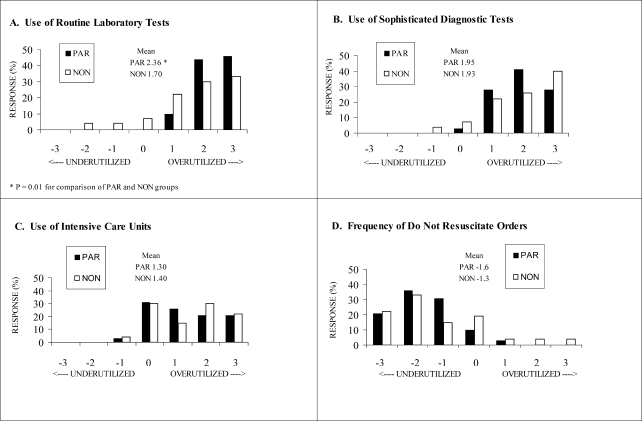
The opinions of residents about general use of health care resources in the United States were collected. Residents were asked whether the use of routine laboratory tests, sophisticated diagnostic tests (ie, cardiac catheterization, computed tomography scans, magnetic resonance imaging scans), and intensive care units and frequency of do not resuscitate orders were appropriately used in the United States (figure). The PAR group rated the use of routine laboratory tests as more overused than did the NON group (100% versus 85%; P = 0.01). Upon returning to the United States, 62% of the residents in the PAR group self-reported a reduced use of laboratory and/or radiologic tests, 28% reported no change, and 10% reported an increased use.
Figure.
Residents' Opinions Regarding Use of US Health Care Resources
Opinions regarding the use of US health care resources were determined on a 7-point Likert scale (from −3, greatly underused, to 3, greatly overused) for use of (A) routine laboratory tests, (B) sophisticated diagnostic tests, and (C) intensive care units and for the frequency of (D) do not resuscitate orders. Abbreviations: NON, nonparticipants; PAR, participants.
One hundred percent of participants (39 of 39) indicated the WCMC global health elective had some degree of positive effect on their knowledge of international health and/or tropical medicine. More than 90% of participants (36 of 39) indicated some degree of positive effect on their physical examination skills.
One hundred percent of participants (39 of 39) indicated that the WCMC global health elective should continue to be offered to future residents, and 95% of participants (37 of 39) indicated they would return to BMC if given the opportunity.
Discussion
The results of our survey suggest the WCMC global health elective has had a positive effect on participating residents. Consequences of the elective included increased medical knowledge, improved physical examination skills, reduced dependence on laboratory tests, and increased awareness of resource use. These reported benefits on the practice of medicine are consistent with other documented international health experiences.3
The survey also provided strong support for continuation of the WCMC global health elective. Recently, WCMC has started sending residents from the neurology, neurosurgery, ophthalmology, psychiatry, and general surgery programs on the elective. Furthermore, in 2009, WCMC initiated a bilateral exchange with residents and faculty from the host institution to receive training in New York for periods of 6 to 12 weeks. Thus far, 7 BMC residents in internal medicine and 7 junior faculty have received training in New York. The exchange has further strengthened institutional and personal bonds and has enhanced the collaborative program training mission.
A limitation of our study is that we relied solely on self-reported changes in behavior. We have not determined whether these responses reflect actual medical practices or how long those changes continue over time, but that could be the focus of future studies. Also, our survey focused solely on the experiences of the WCMC residents. It would be equally important to survey the effect of the elective from the perspective of the host institution.
Conclusion
Participants of the WCMC global health elective report positive experiences from our multidimensional global health collaboration. With effective partnerships and supportive funding, similar electives may be an effective way for residency programs to teach the Accreditation Council for Graduate Medical Education competencies of medical knowledge, patient care, and systems-based practice.
Footnotes
Duncan K. Hau, MD, is Pediatric Resident at the New York Presbyterian Hospital-Weill Cornell Medical Center; Jennifer I. DiPace, MD, is Assistant Professor of Pediatrics and Director of Pediatric Graduate Medical Education at the New York Presbyterian Hospital–Weill Cornell Medical Center; Robert N. Peck, MD, is Assistant Professor at the Departments of Medicine and Pediatrics, Center for Global Health, Division of Infectious Diseases, Weill Cornell Medical College, and Lecturer at the Weill Bugando University College of Health Sciences, Bugando Medical Center in Mwanza, Tanzania; and Warren D. Johnson Jr, MD, is B. H. Kean Professor of Tropical Medicine and Director at the Center for Global Health, Department of Medicine/Division of Infectious Diseases, Weill Cornell Medical College.
Funding: The authors report no external funding source for this study.
The authors would like to thank Professor Jacob Mtabaji, Principal of Weill Bugando University College of Health Sciences, and Dr Charles Majinge, Hospital Director of the Bugando Medical Center, for the unique training opportunity they provided; and to acknowledge the generous support from the Touch Foundation, Dr Antonio Gotto, Dean of Weill Cornell Medical College, and Joan and Sanford Weill. The authors also thank the Tanzanian residents for their support of the program. Lastly, the authors are grateful to Dr Mary Jo Ward for assistance with survey design and data analysis.
References
- 1.Weill Cornell Medical College Center for Global Health. Weill Cornell Bugando Program, http://weill.cornell.edu/globalhealth/major-initiatives/weill_cornell_program_in_bugando. Accessed January 8, 2009. [Google Scholar]
- 2.Miller WC, Corey GR, Lallinger GJ, Durack DT. International health and internal medicine residency training: the Duke University experience. Am J Med. 1995;99(3):291–297. doi: 10.1016/s0002-9343(99)80162-4. [DOI] [PubMed] [Google Scholar]
- 3.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med. 2009;84(3):320–325. doi: 10.1097/ACM.0b013e3181970a37. [DOI] [PMC free article] [PubMed] [Google Scholar]