Abstract
Background
The nationwide decline in pediatric admissions to community hospitals threatens the sustainability of small pediatric residency programs. Little is known about the response of small programs to this challenge.
Objectives
We report on the design and evaluation of an innovative, collaborative model for pediatric inpatient training between an academic community medical center and a children's hospital.
Methods
We describe the operational, academic, and financial features of the model. Outcome measures include patient volume and subspecialty mix, resident and faculty perceptions as reported in an anonymous survey, and Accreditation Council for Graduate Medical Education Residency Review Committee (RRC) review.
Results
In 2003, Albert Einstein Medical Center (Einstein) closed its pediatric inpatient unit and established an independent teaching service at St Christopher's Hospital for Children (St Christopher's) in Philadelphia, Pennsylvania. Under the new model, patient volume and subspecialty mix more than tripled. Einstein residents and faculty identified 5 major strengths: level of responsibility and decision making, caring for medically complex children, quality of teaching, teamwork, and opportunity to participate in academic activities at a children's hospital. St Christopher's leadership reported increased volume, no disruption of their residency program, and no dilution of clinical teaching material. The Einstein program was reaccredited by the RRC in 2006 for 2 years and in 2009 for 4 years.
Conclusion
A collaborative model for inpatient training was successful in maintaining a community hospital–based pediatric residency program. Positive outcomes were documented for the residency program, the parent community hospital, and the collaborating children's hospital.
Background
The nationwide decline in pediatric admissions to community hospitals threatens the sustainability of small pediatric residency programs.1 From 2005 through 2009, 6% to 12% of pediatric programs risked probation annually, and 10 lost accreditation. Low inpatient and subspecialty volume were major contributing factors.2
In contrast, children's hospitals have experienced growing occupancy3 and increasing medical complexity of hospitalized children.4 Community and children's hospitals are facing additional resident duty hour restrictions and considerations for inpatient caps. Thus, pediatric programs of any size are facing challenges to maintain educational quality and financial sustainability.
Relatively little is known about how small pediatric programs respond to the challenge of low inpatient census and low acuity. A common solution is the guest rotator model. This enhances resident inpatient exposure but may decrease resident identity with the home program.5 In the merger model, 2 programs integrate their residencies to varying degrees.6 Challenges described include blurring of program identities, conflicts between cultures, and impact upon prestige.7,8 Programs that merge and create separate tracks also describe inequalities in resident workload, patient exposure, and education.9
A third, less explored, approach is the collaborative model, in which programs maintain their individual identity but align resources. In this article, we report on the creation and evaluation of a collaborative model of pediatric inpatient training between a small pediatric residency program at an academic community medical center and a children's hospital.
Methods
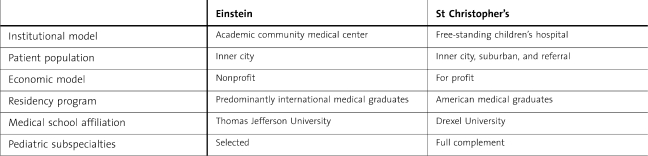
In 2003, a collaborative relationship for inpatient training was established between the Albert Einstein Medical Center (Einstein) and St Christopher's Hospital for Children (St Christopher's) in Philadelphia, Pennsylvania. The characteristics of the institutions are described in the table.
Table.
Characteristics of Albert Einstein Medical Center and St Christopher's Hospital for Children
In 2002, Einstein had explored closing its pediatric inpatient unit owing to declining census and increased demand for adult beds. Einstein′s leadership was committed to maintaining the pediatric residency, and St Christopher's emerged as a potential collaborator owing to its proximity and prior positive history of collaboration through a guest rotator model. At the same time, St Christopher's was seeking to increase admissions and Einstein, with its large primary care network, was viewed as an appealing collaborator.
The leadership of Einstein and St Christopher's developed 4 goals to guide the collaboration: (1) improve Einstein's pediatric inpatient training; (2) increase St Christopher's admissions and referrals; (3) prevent disruption of St Christopher's residency; and (4) ensure nondiscrimination in patient care. A task force of program leaders met regularly to design the model and evaluate progress.
The Memorandum of Agreement
In 2003, Einstein closed its pediatric inpatient unit and created the Einstein Service at St Christopher's. St Christopher's agreed to bill for hospital services and Einstein, for its physician services. Subspecialty services would be provided by St Christopher's faculty. Einstein would provide resident salary and benefits, but St Christopher's would claim Einstein residents for graduate medical education purposes and reimburse Einstein a fixed amount per rotating resident per year.
Residency Review Committee Approval
In October 2002, Einstein's pediatric residency was reaccredited for 2 years with citations for resident experience in inpatient and subspecialty services. In October 2003, the Residency Review Committee (RRC) approved Einstein's new model and granted a 1-year extension from the original cycle.
The Einstein Service
The Einstein service is an independent clinical and teaching service staffed by Einstein faculty and residents with full access to St Christopher's resources. It is not housed in a specific geographic location; rather patients are assigned to units appropriate for diagnosis. Patients are referred from Einstein's 3 emergency departments and large primary care network. Einstein and St Christopher's services operate in parallel to provide patient care but interface during educational conferences and subspecialty consultations.
Evaluation of the Collaborative Model
We evaluated the inpatient volume, resident and faculty perceptions, and RRC accreditation.
The Inpatient Experience
We analyzed the effect of the collaborative relationship on inpatient admissions and subspecialty exposure. Data sources included inpatient logs (2002–2009) and work sheets (2003–2009). To estimate the rate of subspecialty exposure, defined as a case with a subspecialty principal diagnosis, we sampled 100 consecutive admissions in the first and third quarters of each year (200 patients/year), from 2002 to 2009, for a total of 1600. The years 2002–2003 reflect the old pediatric inpatient unit at Einstein, whereas 2004–2009 reflect the new model.
Resident and Faculty Perceptions
Einstein resident perceptions were obtained through meetings with program leadership and rotation evaluations. In June 2010, we conducted an online anonymous survey of Einstein residents and faculty to assess satisfaction with the inpatient training experience and impressions of how they were perceived by their St Christopher's colleagues. Responses used a 5-point Likert scale and open-ended formats. St Christopher's program leadership provided ongoing feedback regarding their perceptions of the model at task force meetings.
RRC Accreditation
We report on the program's RRC accreditation reviews in 2006 and 2009.
Results
The Einstein Inpatient Experience
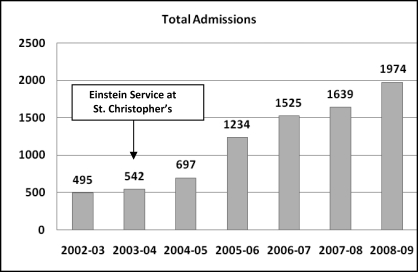
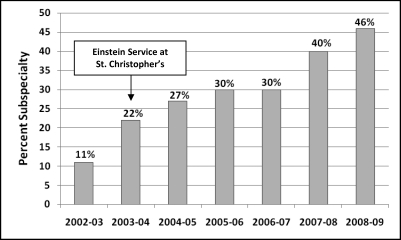
Inpatient admissions and rate of subspecialty exposure more than tripled between 2002–2003 and 2008–2009 in the new collaborative Einstein Service (figures 1 and 2).
Figure 1.
Inpatient Admissions to the Einstein Service at St Christopher's Hospital for Children, 2002–2009
Figure 2.
Percentage Subspecialty Inpatient Admissions to the Einstein Service at St Christopher's Hospital for Children, 2002–2009
Einstein Resident Perceptions
Einstein residents experiencing the transition (2003–2005) perceived the new model as superior with regard to patient volume, diagnostic diversity, and subspecialty access. A critical outcome was preservation of the Einstein program's identity and residents' sense of belonging to their primary institution. Several residents described the experience as the “best of both worlds.” Perceived challenges included the perception of competency by St Christopher's residents, faculty, and staff.
In 2010, 27 of 30 Einstein residents (90%) responded to the survey. Most (81%) felt the model prepared them well to care for sick children, were satisfied/very satisfied with level of responsibility (100%), experience of teamwork (100%), development of clinical judgment skills (88%), and patient volume (81%). Only one-third (38%) were satisfied with patient diversity. Einstein residents felt they were perceived as competent/very competent by St Christopher's residents (85%), faculty (73%), and staff (88%). There were no differences in responses by year of training. Residents identified 5 major strengths: level of responsibility and decision making, caring for medically complex children, quality of teaching, teamwork, and conferences.
Einstein Faculty Perceptions
One hundred percent of the Einstein inpatient faculty (7 of 7) felt the model prepared residents very well for the care of sick children, responsibility, and clinical skills (100%). Most were satisfied with patient volume (72%) and diversity (86%). Most felt the inpatient experience enhanced their own professional development (71%) and felt very respected by St Christopher's faculty and staff (100%).
St Christopher's Leadership Perceptions
St Christopher's leadership rated their experience highly. The collaboration increased inpatient volume and subspecialty referrals in a competitive health care market. They described an overall perception of positive relationships between residents and faculty of both programs and felt interactions during educational conferences were mutually enhancing. Importantly, there was no perception of compromise of teaching experience or dilution of clinical material. As St Christopher's volume grew and their program implemented a resident cap system, the additional trainee workforce provided by the Einstein residents was seen as a positive contribution. Although not quantitatively measured, St Christopher's leadership reported progressive acceptance of Einstein residents and respect for their competency by St Christopher's residents and faculty.
RRC Accreditation
In June 2006, the Einstein program was reaccredited for 2 years. Inpatient volume was considered adequate but “lacking variety and complexity.” In August 2009, the program was reaccredited for 4 years, with noted improvement in inpatient subspecialty exposure.
Discussion
Our collaborative model for pediatric inpatient residency training was successful in maintaining a pediatric residency program in an academic community medical center by developing a defined relationship with a children's hospital. The model is unique in that we created a separate inpatient service at a children's hospital, which further is not centered on a “geographic” unit. Although there may be precedent in graduate medical education for other collaborative models, to our knowledge, this is the first description of such a model for pediatric residency training.
The results show that both collaborators benefited under the model. For Einstein, the academic community medical center, it enhanced inpatient residency training and helped maintain program accreditation. For St Christopher's, the children's hospital, it increased admissions and provided additional trainee workforce.
An initial concern was how to successfully interface 2 distinct residency programs in 1 institution and create success for both.10 Unlike mergers, with their forced integrations of programs, our model was successful as it resulted from the initiative and work of the program leaders, sought an optimal blend of independence and interdependence, and enhanced the service-learning balance for both programs in a time of restricted resident duty hours. Our collaborative model could be replicated in other programs, with the key determinants for success being a prior positive history between the institutions, geographic proximity, and commitment of leadership and faculty. In addition, the model should have the ability to produce early and significant outcomes for both collaborators, in our case residency program accreditation and increased inpatient admissions. These elements have also been described as important tools for designing successful program mergers.11–13
We describe key aspects of our graduate medical education collaboration and the impact on our small pediatrics program. If this model is to be applied to other programs, studies should assess additional outcomes, such as outcomes for similar collaborations in large programs, and the effect of the collaboration on resident and faculty recruitment, quality of patient care, and financial outcomes.
Footnotes
Anna M. Carr, MD, is Director of Einstein Inpatient Service at St. Christopher's and Associate Pediatric Residency Program Director, Albert Einstein Medical Center; Matilde Irigoyen, MD, is Chairperson, Department of Pediatrics, Albert Einstein Medical Center; Allan M. Arbeter, MD, is Associate Chair for Research, Department of Pediatrics, Albert Einstein Medical Center; Robert S. Wimmer, MD, is Pediatric Residency Program Director and Associate Chair, Albert Einstein Medical Center; Robert S. McGregor, MD, is Pediatric Residency Program Director and Associate Chair, Department of Pediatrics, St. Christopher's Hospital for Children; Charles R. Reed, MD, is Director of General Pediatrics and Designated Institution Official, St Christophers Hospital for Children; and Daniel V. Schidlow, MD, is Chairperson, Department of Pediatrics, St. Christopher s Hospital for Children.
Funding: The authors report no external funding source.
References
- 1.Sigriest TD, Stucky ER, Szilagy PG, et al. Recent physician-reported trends in the hospitalization of U.S. children. Presented at: 2007 Pediatric Academic Societies Annual Meeting; May 5, 2007 Toronto, Canada. http://www.aap.org/research/abstracts/07abstract14.htm. Accessed June 24, 2010. [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Withdrawn programs/accreditation decisions. http://www.acgme.org/adspublic/. Accessed June 24, 2010. [Google Scholar]
- 3.Sectish TC, Zalneraitis EL, Carraccio C, Behrman RE. The state of pediatrics residency training: a period of transformation of graduate medical education. Pediatrics. 2004;114(3):832–841. doi: 10.1542/peds.2004-0088. [DOI] [PubMed] [Google Scholar]
- 4.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chapman R, Nuovo J. Combined residency training in family practice and other specialties. Fam Med. 1997;29(10):715–718. [PubMed] [Google Scholar]
- 6.Cora-Bramble D, Joseph J, Jain S, Huang ZJ, Gaughan-Chaplain M, Batshaw M. A cross-cultural pediatric residency program merger. Acad Med. 2006;81(12):1108–1114. doi: 10.1097/01.ACM.0000246707.75114.7e. [DOI] [PubMed] [Google Scholar]
- 7.Rider EA, Longmaid HE., III A model for merging residency programmes during health care consolidations: a course for success. Med Educ. 2003;37(9):794–801. doi: 10.1046/j.1365-2923.2003.01599.x. [DOI] [PubMed] [Google Scholar]
- 8.Smith M, Graham P, Holtrop JS, Thomason C, Joyce B. Muddling through a merger: a qualitative study of two combined family practice residencies. Fam Med. 2003;35(7):482–488. [PubMed] [Google Scholar]
- 9.Lovejoy FH, Jr, Nathan DG, Zuckerman BS, Pizzo PA, Fleisher GR, Vinci RJ. The merger of two pediatric residency programs: lessons learned. J Pediatr. 2008;153(6):731–732. doi: 10.1016/j.jpeds.2008.07.036. [DOI] [PubMed] [Google Scholar]
- 10.Tasman A, Riba M. Strategic issues for the successful merger of residency training programs. Hosp Community Psychiatry. 1993;44(10):981–985. doi: 10.1176/ps.44.10.981. [DOI] [PubMed] [Google Scholar]
- 11.Sussman AJ, Otten JR, Goldszer RC, et al. Integration of an academic medical center and a community hospital: the Brigham and Women's/Faulkner hospital experience. Acad Med. 2005;80(3):253–260. doi: 10.1097/00001888-200503000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Cohen JR, Dowling M, Gallagher JS. The trials, tribulations, and relative success of the ongoing clinical merger of two large academic hospital systems. Acad Med. 2001;76(7):675–683. doi: 10.1097/00001888-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Grossman RI, Berne R. Commentary: less is better—lessons from the New York–Mount Sinai merger. Acad Med. 2010;85(12):1817–1818. doi: 10.1097/ACM.0b013e3181f85a4b. [DOI] [PubMed] [Google Scholar]