Abstract
Purpose
Fatigue, depression, and sleep disturbance are common adverse effects of cancer treatment and frequently co-occur. However, the possibility that inflammatory processes may underlie this constellation of symptoms has not been examined.
Patients and Methods
Women (N = 103) who had recently finished primary treatment (ie, surgery, radiation, chemotherapy) for early-stage breast cancer completed self-report scales and provided blood samples for determination of plasma levels of inflammatory markers: soluble tumor necrosis factor (TNF) receptor II (sTNF-RII), interleukin-1 receptor antagonist, and C-reactive protein.
Results
Symptoms were elevated at the end of treatment; greater than 60% of participants reported clinically significant problems with fatigue and sleep, and 25% reported elevated depressive symptoms. Women treated with chemotherapy endorsed higher levels of all symptoms and also had higher plasma levels of sTNF-RII than women who did not receive chemotherapy (all P < .05). Fatigue was positively associated with sTNF-RII, particularly in the chemotherapy-treated group (P < .05). Depressive symptoms and sleep problems were correlated with fatigue but not with inflammatory markers.
Conclusion
This study confirms high rates of behavioral symptoms in breast cancer survivors, particularly those treated with chemotherapy, and indicates a role for TNF-α signaling as a contributor to postchemotherapy fatigue. Results also suggest that fatigue, sleep disturbance, and depression may stem from distinct biologic processes in post-treatment survivors, with inflammatory signaling contributing relatively specifically to fatigue.
INTRODUCTION
Behavioral symptoms are among the most common adverse effects of cancer diagnosis and treatment and include fatigue, depression, and sleep disturbance.1 The prevalence of fatigue and depression have been carefully studied in patients with and survivors of breast cancer, and research suggests that approximately one third of survivors report significant symptoms of fatigue2–4 and that 20% to 30% report elevated depressive symptoms.5 An emerging literature on sleep disturbance also suggests a high prevalence of sleep disturbance in patients with cancer; 40% to 50% of survivors of breast cancer report problems with sleep.6,7 Each of these symptoms is associated with substantial impairment in quality of life and may also have relevance for disease-related outcomes,8 which motivates calls to include behavioral symptoms as a sixth vital sign.9
The mechanisms underlying behavioral symptoms in cancer survivors have not been determined. Symptoms of fatigue, depression, and sleep disturbance frequently co-occur in cancer populations,2,10 leading to speculation about common underlying mechanisms. In particular, there is growing interest in the possibility that these symptoms may be driven by activation of the proinflammatory cytokine network.9,11 Basic research on neural-immune signaling has demonstrated that proinflammatory cytokines signal the CNS to trigger a constellation of behavioral changes that include fatigue, sleep disturbance, and depressive-like symptoms in animal models.12 Consistent with this research, administration or induction of proinflammatory cytokines in healthy humans is associated with increases in depressed mood, fatigue, and sleep problems,13–15 and inflammation is common among noncancer populations that have depression or sleep disorders.16,17 In research about patients with cancer, there is growing literature that links inflammation and fatigue during18–21 and after22–26 cancer treatment, although little is known about mechanisms underlying fatigue immediately after treatment completion, a time when fatigue levels are typically at their peak.27 There has been minimal examination of inflammatory correlates of depressive symptoms or sleep disturbance in cancer populations, and no studies have comprehensively examined fatigue, depression, and sleep and their association with inflammatory markers in patients with cancer to assess potential common underlying pathways. In addition, the role of cancer treatments as potential inducers of inflammation and behavioral symptoms has not been carefully assessed. Chemotherapy is of particular interest, because it has been associated with acute increases in inflammatory markers18,28–30 and fatigue,4,31,32 which may persist long into survivorship.3,33,34 Determining the mechanisms underlying these common, disabling adverse effects of cancer treatment is critical for the development of targeted interventions for prevention and treatment.
The goals of the current study were as follows: to characterize the prevalence and comorbidity of fatigue, depressive symptoms, and sleep disturbance in a sample of women with early-stage breast cancer who had recently completed treatment with surgery, radiation and/or chemotherapy; to determine the contribution of treatment-related factors to behavioral symptoms and inflammation in the aftermath of cancer treatment, focusing on chemotherapy; and to test the hypothesis that inflammatory processes would contribute to these symptoms.
PATIENTS AND METHODS
Participants and Procedures
Participants for this study were drawn from a larger study of cognitive functioning after cancer treatment conducted at the University of California, Los Angeles. Eligibility criteria for the parent trial were as follows: diagnosed with stages 0 to IIIA breast cancer; completed primary cancer treatment (ie, surgery, radiation therapy, and/or chemotherapy) within the past 3 months and not yet started endocrine therapy; age 21 to 65 years; no neurologic or immune-related medical conditions (eg, autoimmune disease); and nonsmoker.
Participants for the parent study were identified primarily through tumor registry rapid case ascertainment from hospitals where collaborating physicians practiced as well as through direct referral from surgical and medical oncology practices. Patients received a brochure describing the study and were asked to contact the research office if they were interesting in participating. A phone screen was conducted to determine eligibility, after which participants were scheduled for an in-person appointment at the University of California, Los Angeles, where they provided blood samples, completed self-report questionnaires, were weighed and measured for determination of body mass index (BMI), and underwent comprehensive neuropsychologic testing. Assessments were conducted in the morning (before 11 am) after an overnight fast. The current report focuses on self-report and immune data from 103 women who completed the baseline assessment and who had no confounding medical conditions. The research was approved by the University of California, Los Angeles, institutional review board, and informed consent was obtained from all participants.
Behavioral Measures
Demographic and clinical information were determined from self-report questionnaires. Fatigue was assessed by using the Fatigue Symptom Inventory (FSI), a valid and reliable, 14-item measure specifically designed to assess fatigue in cancer populations.35–37 Items that assessed average fatigue, most fatigue, and least fatigue in the past week were averaged to obtain a measure of fatigue severity.36 Depressive symptoms were assessed by using the Beck Depression Inventory-II (BDI-II), a 21-item measure that assesses cognitive, affective, and vegetative symptoms of depression during the prior 2 weeks with excellent reliability and validity.38 The Pittsburgh Sleep Quality Index (PSQI) was used to assess subjective sleep quality and disturbances over the prior month. This 19-item questionnaire has high internal consistency, test-retest reliability, and diagnostic validity with polysomnography.39
Inflammatory Markers
Blood samples for circulating inflammatory markers were collected by venipuncture into EDTA tubes, placed on ice, centrifuged for acquisition of plasma, and stored at −80°C for subsequent batch testing. We focused on three inflammatory markers that have been associated with cancer-related fatigue in previous research: interleukin-1 (IL-1) receptor antagonist (IL-1ra), soluble tumor necrosis factor (TNF) receptor type II (sTNF-RII), and C-reactive protein (CRP).20,22–25 Plasma levels of IL-1ra and sTNF-RII were determined by enzyme-linked immunosorbent assay (R&D Systems, Minneapolis, MN) according to the manufacturer's protocols, with a lower limit of detection of 31 and 234 pg/mL for IL-1ra and sTNF-RII, respectively. CRP levels were determined by a high-sensitivity enzyme-linked immunosorbent assay (Immundiagnostik; ALPCO Immunoassays, Salem, NH) according to the manufacturer's protocol but with an extended standard curve to a lower limit of detection of 0.2 mg/L. All samples were run in duplicate, and assays were repeated on two separate assay days for sTNF-RII and IL-1ra; intra-assay and interassay mean levels were used in all analyses. The intra- and interassay precision of all tests were less than or equal to 10%.
Statistical Analyses
t tests were used to compare demographic and clinical characteristics of women treated with chemotherapy versus not, and correlations were used to examine associations among behavioral symptoms. Chemotherapy effects on symptoms and inflammatory markers were tested by one-way analysis of covariance (ANCOVA), and predictors of behavioral symptoms were examined with ANCOVA and multiple regression analyses. Given the small numbers of women treated with chemotherapy alone, the chemotherapy group included women treated with and without radiation therapy. Hence, all multivariate analyses controlled for exposure to radiation therapy as well as age and time since treatment completion, given potential effects of these variables on fatigue2,27; analyses with inflammatory markers as the outcome also controlled for BMI.40 Because their distributions were clearly non-normal and highly skewed, all inflammatory marker measures were transformed before analyses by using a natural log transformation. Analyses of depression were conducted by using all items from the BDI-II (total score) and with items that assessed energy/fatigue and sleep quality removed to minimize overlap with these symptoms.
RESULTS
Demographic characteristics of study participants are listed in Table 1. Women treated with chemotherapy were younger at diagnosis (49.6 v 52.8 years; t(101) = 1.99; P = .05) and a longer time had elapsed since their cancer diagnoses (8.3 v 5.1 months; t(100) = −9.58; P < .001), consistent with a longer duration of treatment in this group. In addition, the time between treatment completion and the study visit was somewhat shorter for women treated with chemotherapy (26.8 v 36.5 days; t(87) = 1.82; P = .07).
Table 1.
Demographic and Clinical Characteristics of Study Participants
| Characteristic | Patients |
|
|---|---|---|
| No. | % | |
| Age, years | ||
| Mean | 51.2 | |
| Range | 32-66 | |
| Ethnicity | ||
| White | 89 | 86 |
| Other | 14 | 14 |
| Married/committed relationship* | 81 | 79 |
| Education status | ||
| High school graduate/some college | 20 | 19 |
| College graduate | 53 | 52 |
| Graduate degree | 30 | 29 |
| Yearly income, $* | ||
| ≤ 60,000 | 10 | 10 |
| 60,000-100,000 | 25 | 25 |
| ≥ 100,000 | 65 | 65 |
| Cancer treatment | ||
| No chemotherapy | 53 | 52 |
| Surgery only | 14 | |
| Surgery + radiation | 39 | |
| Chemotherapy | 50 | 48 |
| Surgery + chemotherapy | 9 | |
| Surgery + radiation + chemotherapy | 41 | |
| Time since diagnosis, months | ||
| Mean | 6.7 | |
| Range | 1.7-12.5 | |
| Time since treatment, days | ||
| Mean | 31.8 | |
| Range | 1-112 | |
Numbers were based on available data.
Prevalence of Behavioral Symptoms
Symptoms of fatigue, sleep disturbance, and depression were elevated at the end of primary treatment. The average fatigue severity score was 3.85, and 64% of the sample scored greater than the clinically significant cutoff of 3.36 The average score on the PSQI was 8.02; 65% percent scored greater than the clinically significant cutoff of 5, and 46% scored greater than the alternative cutoff of 8 that was suggested for patients with chronic illness, including cancer.41 The average score on the BDI-II was 9.15, and 25% percent of women scored greater than the clinically significant cutoff of 14.38
Fatigue was significantly correlated with depressive symptoms for total BDI-II (r = 0.54; P < .001) and for BDI-II without energy/fatigue or sleep items (r = 0.43; P < .001); fatigue was also significantly correlated with sleep disturbance (r = 0.34; P = .001). Depressive symptom severity and sleep disturbance were also correlated on the total BDI-II (r = 0.55; P < .001) and on the BDI-II without energy/fatigue or sleep items (r = 0.52; P < .001).
Effects of Chemotherapy on Behavioral Symptoms and Inflammatory Markers
Analyses were first conducted to determine the effect of chemotherapy exposure on behavioral symptoms and inflammatory markers. In analyses controlling for age, time since treatment completion, and radiation therapy, chemotherapy was associated with significantly higher levels of all behavioral symptoms (all P < .02; Table 2). None of the covariates were significantly associated with behavioral symptoms.
Table 2.
Differences in Behavioral and Inflammatory Outcomes by Chemotherapy Status
| Characteristic | Chemotherapy |
No Chemotherapy |
P | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Fatigue by FSI | 4.52 | 2.27 | 3.24 | 1.98 | .003 |
| Sleep disturbance by PSQI | 8.98 | 3.62 | 7.19 | 4.02 | .01 |
| Depressive symptoms by BDI-II | 11.10 | 6.55 | 7.34 | 7.58 | .019 |
| Soluble TNF receptor II, pg/mL | 2454 | 717 | 2152 | 623 | .003 |
| IL-1 receptor antagonist, pg/mL | 231 | 163 | 331 | 399 | .61 |
| C-reactive protein, mg/L | 2.09 | 3.21 | 3.27 | 5.26 | .89 |
NOTE. Unadjusted means are reported. P values are from analysis of covariance controlling for age, time since treatment completion, and radiation therapy; analyses for inflammatory outcomes also controlled for BMI.
Abbreviations: BDI-II, Beck Depression Inventory-II; BMI, body mass index; FSI, Fatigue Symptom Inventory; IL, interleukin; PSQI, Pittsburgh Sleep Quality Index; SD, standard deviation; TNF, tumor necrosis factor.
Chemotherapy was also associated with higher levels of sTNF-RII, controlling for age, time since treatment completion, radiation therapy, and BMI (Table 2). Older age and higher BMI were also significant predictors of higher sTNF-RII in these analyses (all P < .05). There was no significant association between chemotherapy exposure and plasma concentrations of IL-1ra or CRP (Table 2).
Association Between Inflammatory Markers and Behavioral Symptoms
Analyses next were conducted to investigate the association between inflammatory markers and fatigue, depression, and sleep disturbance. As predicted, sTNF-RII was associated with higher levels of fatigue, controlling for age, time since treatment, and radiation therapy (P = .025). To additionally probe this association, we examined levels of sTNF-RII in women who scored in the clinically significant range of the FSI (FSI severity > 3) and found significant elevations in sTNF-RII in this group when analysis controlled for confounders (unadjusted mean of sTNF-RII in fatigued women = 2,400 pg/mL v 2127 pg/mL in nonfatigued women; P = .036). However, fatigue was not associated with IL-1ra or CRP (both P > .9), nor were these inflammatory markers elevated in women who had clinically significant fatigue. Neither depression nor sleep disturbance was associated with any of the inflammatory markers (all P for BDI-II > .15; all P for PSQI > .80). Similar findings were observed in analyses in which fatigue and sleep items were deleted from the BDI-II and in analyses that compared data of women who scored in the clinical range of the BDI-II or the PSQI.
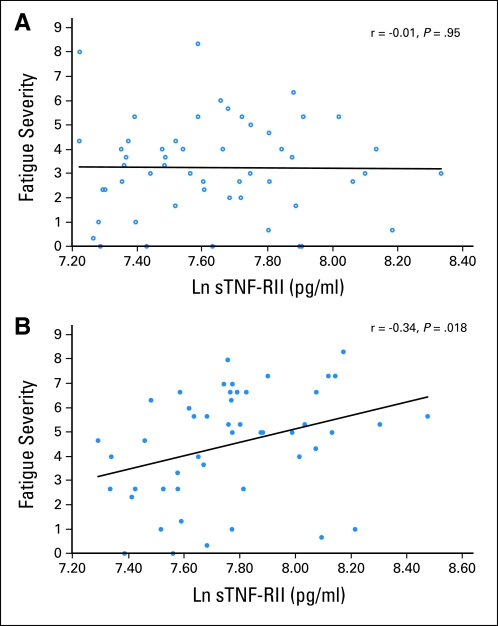
Given effects of chemotherapy on fatigue and sTNF-RII, we examined the association between fatigue and sTNF-RII within the chemotherapy- and no chemotherapy-treated groups separately. Fatigue was associated with significant elevations in sTNF-RII in the chemotherapy-treated group, controlling for confounders (P = .03). However, there was no association between fatigue and sTNF-RII in patients not receiving chemotherapy (P > .70). Simple correlations between fatigue and sTNF-RII in the chemotherapy versus no-chemotherapy groups are shown in Figure 1. Of note, there was no evidence for an association between depressive symptoms or sleep disturbance and the inflammatory markers in either group.
Fig 1.
Correlation between fatigue severity and natural log (LN) –transformed soluble tumor necrosis factor receptor II (sTNF-RII) in (A) no chemotherapy and (B) chemotherapy-treated groups.
DISCUSSION
This study confirms high levels of fatigue, depressive symptoms, and sleep disturbance in patients with breast cancer who have recently completed primary treatment, particularly among those treated with chemotherapy. Scores for all three symptoms were much greater than levels seen in comparison samples of healthy women,36,42,43 which highlights the importance of these behavioral disturbances in the immediate post-treatment period. However, despite strong correlations among symptoms, we found no evidence for a common inflammatory mechanism driving symptom expression. Instead, the only symptom associated with the inflammatory markers assessed was fatigue, which was correlated specifically with elevations in sTNF-RII. These findings are consistent with previous research linking sTNF-RII and fatigue in longer-term survivors of breast cancer,22 and they extend those results to demonstrate an association between TNF and fatigue in the immediate post-treatment period. Exposure to chemotherapy was also associated with elevations in sTNF-RII, and the strongest association between sTNF-RII and fatigue was seen in chemotherapy-treated patients.
In contrast with fatigue, neither depressive symptoms nor sleep disturbance was associated with sTNF-RII or other circulating markers of inflammation. A recent meta-analysis showed a reliable association between inflammatory markers (including CRP and IL-1ra) and self-reported depressive symptoms, although this effect was small, and studies in patients with cancer are extremely limited.16 In addition, few studies have differentiated between affective and vegetative symptoms of depression, which may have distinct biologic correlates. For example, among patients with ovarian cancer, plasma and ascites levels of IL-6 were correlated with vegetative symptoms of depression, including fatigue, but not with affective symptoms (eg, sadness).44 Among patients undergoing interferon alfa therapy for malignant melanoma, fatigue and other vegetative symptoms emerged earlier than depressed mood and were less responsive to paroxetine treatment,45 which was similar to findings in other cancer populations.46 In our previous research in patients with breast cancer, general depressive symptoms were not associated with markers of inflammation, including sTNF-RII, IL-1ra, and CRP.20,22 These findings suggest that fatigue and depression, though closely related, may have distinct biologic underpinnings, and that fatigue may be more closely tied to inflammatory processes in the context of breast cancer.
Inflammation is common among individuals with sleep disorders47 and in those with objectively-assessed sleep disturbance.48–51 However, evidence that self-reported sleep problems are associated with circulating markers of inflammation is mixed.52–55 The current findings suggest that elevations in circulating inflammatory markers, specifically sTNF-RII, IL-1ra, and CRP, may not contribute to subjective sleep disturbance at the completion of breast cancer treatment, despite high levels of sleep problems at this time. Instead, other research suggests that affective and cognitive/behavioral factors may contribute to cancer-related insomnia.56 Future studies should probe biologic, affective, and cognitive/behavioral factors that may contribute to fatigue, depression, and sleep problems to identify unique and common mechanisms for these symptoms.
These findings suggest a role for TNF-α in chemotherapy-induced fatigue. Results showed that sTNF-RII, rather than IL-1ra or CRP, was specifically associated with fatigue. The soluble TNF receptor is shed from a cell surface after stimulation of the cell by the proinflammatory cytokine TNF-α and, therefore, serves as a marker for TNF-α activity.57 In animal models, treatment with the chemotherapy agent adriamycin induces elevations in peripheral TNF-α, which then migrates across the blood brain barrier and causes inflammation and oxidative stress in the brain.58 Conversely, pharmacologic blockade of TNF with etanercept led to reduced fatigue in patients with cancer who were undergoing chemotherapy.59 In the current sample, circulating concentrations of sTNF-RII in chemotherapy-treated patients were quite high, comparable to those seen in our previous research with persistently fatigued survivors of breast cancer.22 In contrast, plasma levels of IL-1ra in this sample were much less than levels linked to cancer-related fatigue in our previous research20,22,23 and may have been insufficient to induce behavioral changes. Levels of CRP in this sample were high, comparable to levels associated with fatigue in previous studies.20 It is possible that inflammatory cytokines, although correlated, may have distinct associations with the CNS and physical health. For example, sTNF-RII, but not IL-6, was correlated with stress-induced changes in the CNS,60 and sTNF-RII predicted coronary heart disease independent of CRP.61
Despite growing interest in behavioral adverse effects of cancer treatment and their interrelationships, no previous studies have comprehensively examined fatigue, depressive symptoms, and sleep disturbance and their biologic underpinnings. The current findings suggest that, although these symptoms frequently co-occur in the aftermath of breast cancer treatment, they do not necessarily share a common underlying inflammatory biology at this point in the cancer trajectory. Conclusions are limited by the cross-sectional nature of the data, which particularly limits conclusions about causality; for example, women may have had elevated fatigue and sTNF-RII before treatment. Longitudinal studies are required to additionally probe the associations among these symptoms and the mechanisms that contribute to their onset and persistence over time. In addition, we focused on three biomarkers that serve as proxies for the activity of three key proinflammatory cytokines—IL-1β (IL-1ra), TNF-α (sTNF-RII), and IL-6 (CRP) —and have been correlated with cancer-related fatigue20,22–25 and with depression and sleep disturbance in noncancer populations.18,53,54 However, it is possible that other markers of inflammation not assessed here may contribute to these symptoms. It is also possible that elevated inflammatory markers may be more apparent in women with clinical depression and/or sleep disorders. Moreover, although women were screened for neurologic and immune-related medical conditions, other potential causes of behavioral symptoms, including anemia and thyroid dysfunction, were not assessed.
The present results implicate TNF-α signaling as one mechanism underlying the development of treatment-related fatigue and highlight the need for future studies to define other biologic mechanisms driving the emergence of sleep disturbance and depressive symptoms. Identification of unique and common mechanisms for these common adverse effects of cancer treatment is essential for the development of targeted interventions.
Acknowledgment
We thank Barbara Kahn and Amy Oppenheim, the Los Angeles Surveillance, Epidemiology, and End Results cancer registry, and our participants for their time and dedication to this research.
Footnotes
Supported by National Institutes of Health (NIH) National Cancer Institute Grant No. R01-CA10950 (Cognitive Functioning after Breast Cancer Treatment), the Breast Cancer Research Foundation, and in part by NIH National Institute of Aging Grant No. P30-AG028748 (UCLA Older Americans Independence Center).
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Julienne E. Bower, Patricia A. Ganz, Michael R. Irwin, Steve W. Cole
Financial support: Patricia A. Ganz
Administrative support: Patricia A. Ganz
Provision of study materials or patients: Patricia A. Ganz
Collection and assembly of data: Patricia A. Ganz, Lorna Kwan, Elizabeth C. Breen
Data analysis and interpretation: Julienne E. Bower, Michael R. Irwin, Lorna Kwan, Elizabeth C. Breen, Steve W. Cole
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26:768–777. doi: 10.1200/JCO.2007.14.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in breast cancer survivors: Occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 3.Cella D, Davis K, Breitbart W, et al. Cancer-related fatigue: Prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol. 2001;19:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 4.Andrykowski MA, Schmidt JE, Salsman JM, et al. Use of a case definition approach to identify cancer-related fatigue in women undergoing adjuvant therapy for breast cancer. J Clin Oncol. 2005;23:6613–6622. doi: 10.1200/JCO.2005.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;(32):57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 6.Savard J, Simard S, Blanchet J, et al. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583–590. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 7.Bardwell WA, Profant J, Casden DR, et al. The relative importance of specific risk factors for insomnia in women treated for early-stage breast cancer. Psychooncology. 2008;17:9–18. doi: 10.1002/pon.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groenvold M, Petersen MA, Idler E, et al. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat. 2007;105:209–219. doi: 10.1007/s10549-006-9447-x. [DOI] [PubMed] [Google Scholar]
- 9.Miller AH, Ancoli-Israel S, Bower JE, et al. Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol. 2008;26:971–982. doi: 10.1200/JCO.2007.10.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palesh OG, Roscoe JA, Mustian KM, et al. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol. 2010;28:292–298. doi: 10.1200/JCO.2009.22.5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee BN, Dantzer R, Langley KE, et al. A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. Neuroimmunomodulation. 2004;11:279–292. doi: 10.1159/000079408. [DOI] [PubMed] [Google Scholar]
- 12.Dantzer R, O'Connor JC, Freund GG, et al. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reichenberg A, Yirmiya R, Schuld A, et al. Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry. 2001;58:445–452. doi: 10.1001/archpsyc.58.5.445. [DOI] [PubMed] [Google Scholar]
- 14.Späth-Schwalbe E, Hansen K, Schmidt F, et al. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men. J Clin Endocrinol Metab. 1998;83:1573–1579. doi: 10.1210/jcem.83.5.4795. [DOI] [PubMed] [Google Scholar]
- 15.Eisenberger NI, Inagaki TK, Mashal NM, et al. Inflammation and social experience: An inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun. 2010;24:558–563. doi: 10.1016/j.bbi.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 17.Irwin M. Effects of sleep and sleep loss on immunity and cytokines. Brain Behav Immun. 2002;16:503–512. doi: 10.1016/s0889-1591(02)00003-x. [DOI] [PubMed] [Google Scholar]
- 18.Wang XS, Shi Q, Williams LA, et al. Inflammatory cytokines are associated with the development of symptom burden in patients with NSCLC undergoing concurrent chemoradiation therapy. Brain Behav Immun. 2010;24:968–974. doi: 10.1016/j.bbi.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang XS, Shi Q, Williams LA, et al. Serum interleukin-6 predicts the development of multiple symptoms at nadir of allogeneic hematopoietic stem cell transplantation. Cancer. 2008;113:2102–2109. doi: 10.1002/cncr.23820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bower JE, Ganz PA, Tao ML, et al. Inflammatory biomarkers and fatigue during radiation therapy for breast and prostate cancer. Clin Cancer Res. 2009;15:5534–5540. doi: 10.1158/1078-0432.CCR-08-2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mills PJ, Parker B, Dimsdale JE, et al. The relationship between fatigue and quality of life and inflammation during anthracycline-based chemotherapy in breast cancer. Biol Psychol. 2005;69:85–96. doi: 10.1016/j.biopsycho.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Bower JE, Ganz PA, Aziz N, et al. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med. 2002;64:604–611. doi: 10.1097/00006842-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Collado-Hidalgo A, Bower JE, Ganz PA, et al. Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res. 2006;12:2759–2766. doi: 10.1158/1078-0432.CCR-05-2398. [DOI] [PubMed] [Google Scholar]
- 24.Alexander S, Minton O, Andrews P, et al. A comparison of the characteristics of disease-free breast cancer survivors with or without cancer-related fatigue syndrome. Eur J Cancer. 2009;45:384–392. doi: 10.1016/j.ejca.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orre IJ, Murison R, Dahl AA, et al. Levels of circulating interleukin-1 receptor antagonist and C-reactive protein in long-term survivors of testicular cancer with chronic cancer-related fatigue. Brain Behav Immun. 2009;23:868–874. doi: 10.1016/j.bbi.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Reinertsen KV, Cvancarova M, Loge JH, et al. Predictors and course of chronic fatigue in long-term breast cancer survivors. J Cancer Surviv. 2010;4:405–414. doi: 10.1007/s11764-010-0145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobsen PB, Donovan KA, Small BJ, et al. Fatigue after treatment for early stage breast cancer: A controlled comparison. Cancer. 2007;110:1851–1859. doi: 10.1002/cncr.22993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mills PJ, Ancoli-Israel S, Parker B, Natarajan L, et al. Predictors of inflammation in response to anthracycline-based chemotherapy for breast cancer. Brain Behav Immun. 2008;22:98–104. doi: 10.1016/j.bbi.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mills PJ, Parker B, Jones V, et al. The effects of standard anthracycline-based chemotherapy on soluble ICAM-1 and vascular endothelial growth factor levels in breast cancer. Clin Cancer Res. 2004;10:4998–5003. doi: 10.1158/1078-0432.CCR-0734-04. [DOI] [PubMed] [Google Scholar]
- 30.Pusztai L, Mendoza TR, Reuben JM, et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;25:94–102. doi: 10.1016/j.cyto.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Jacobsen PB, Hann DM, Azzarello LM, et al. Fatigue in women receiving adjuvant chemotherapy for breast cancer: Characteristics, course, and correlates. J Pain Symptom Manage. 1999;18:233–242. doi: 10.1016/s0885-3924(99)00082-2. [DOI] [PubMed] [Google Scholar]
- 32.Donovan KA, Jacobsen PB, Andrykowski MA, et al. Course of fatigue in women receiving chemotherapy and/or radiotherapy for early stage breast cancer. J Pain Symptom Manage. 2004;28:373–380. doi: 10.1016/j.jpainsymman.2004.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: A longitudinal investigation. Cancer. 2006;106:751–758. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 34.Broeckel JA, Jacobsen PB, Horton J, et al. Characteristics and correlates of fatigue after adjuvant chemotherapy for breast cancer. J Clin Oncol. 1998;16:1689–1696. doi: 10.1200/JCO.1998.16.5.1689. [DOI] [PubMed] [Google Scholar]
- 35.Hann DM, Jacobsen PB, Azzarello LM, et al. Measurement of fatigue in cancer patients: Development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7:301–310. doi: 10.1023/a:1024929829627. [DOI] [PubMed] [Google Scholar]
- 36.Donovan KA, Jacobsen PB, Small BJ, et al. Identifying clinically meaningful fatigue with the Fatigue Symptom Inventory. J Pain Symptom Manage. 2008;36:480–487. doi: 10.1016/j.jpainsymman.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donovan KA, Jacobsen PB. The Fatigue Symptom Inventory: A systematic review of its psychometric properties. Support Care Cancer. 2010;19:169–185. doi: 10.1007/s00520-010-0989-4. [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Steer RA, Brown GK. BDI-II Manual (ed 2) San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 39.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14:331–338. [PubMed] [Google Scholar]
- 40.O'Connor MF, Bower JE, Cho HJ, et al. To assess, to control, to exclude: Effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun. 2009;23:887–897. doi: 10.1016/j.bbi.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 42.Otte JL, Carpenter JS, Russell KM, et al. Prevalence, severity, and correlates of sleep-wake disturbances in long-term breast cancer survivors. J Pain Symptom Manage. 2010;39:535–547. doi: 10.1016/j.jpainsymman.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wassertheil-Smoller S, Shumaker S, Ockene J, et al. Depression and cardiovascular sequelae in postmenopausal women: The Women's Health Initiative (WHI) Arch Intern Med. 2004;164:289–298. doi: 10.1001/archinte.164.3.289. [DOI] [PubMed] [Google Scholar]
- 44.Lutgendorf SK, Weinrib AZ, Penedo F, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol. 2008;26:4820–4827. doi: 10.1200/JCO.2007.14.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Capuron L, Gumnick JF, Musselman DL, et al. Neurobehavioral effects of interferon-alpha in cancer patients: Phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacology. 2002;26:643–652. doi: 10.1016/S0893-133X(01)00407-9. [DOI] [PubMed] [Google Scholar]
- 46.Morrow GR, Hickok JT, Roscoe JA, et al. Differential effects of paroxetine on fatigue and depression: A randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol. 2003;21:4635–4641. doi: 10.1200/JCO.2003.04.070. [DOI] [PubMed] [Google Scholar]
- 47.Vgontzas AN, Papanicolaou DA, Bixler EO, et al. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: Role of sleep disturbance and obesity. J Clin Endocrinol Metab. 1997;82:1313–1316. doi: 10.1210/jcem.82.5.3950. [DOI] [PubMed] [Google Scholar]
- 48.Mills PJ, von Känel R, Norman D, et al. Inflammation and sleep in healthy individuals. Sleep. 2007;30:729–735. doi: 10.1093/sleep/30.6.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hong S, Mills PJ, Loredo JS, et al. The association between interleukin-6, sleep, and demographic characteristics. Brain Behav Immun. 2005;19:165–172. doi: 10.1016/j.bbi.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 50.von Känel R, Dimsdale JE, Ancoli-Israel S, et al. Poor sleep is associated with higher plasma proinflammatory cytokine interleukin-6 and procoagulant marker fibrin D-dimer in older caregivers of people with Alzheimer's disease. J Am Geriatr Soc. 2006;54:431–437. doi: 10.1111/j.1532-5415.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 51.von Känel R, Ancoli-Israel S, Dimsdale JE, et al. Sleep and biomarkers of atherosclerosis in elderly Alzheimer caregivers and controls. Gerontology. 2010;56:41–50. doi: 10.1159/000264654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McDade TW, Hawkley LC, Cacioppo JT. Psychosocial and behavioral predictors of inflammation in middle-aged and older adults: The Chicago health, aging, and social relations study. Psychosom Med. 2006;68:376–381. doi: 10.1097/01.psy.0000221371.43607.64. [DOI] [PubMed] [Google Scholar]
- 53.Liukkonen T, Räsänen P, Ruokonen A, et al. C-reactive protein levels and sleep disturbances: Observations based on the northern Finland 1966 birth cohort study. Psychosom Med. 2007;69:756–761. doi: 10.1097/PSY.0b013e318157cb96. [DOI] [PubMed] [Google Scholar]
- 54.Suarez EC. Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: Evidence for gender disparity. Brain Behav Immun. 2008;22:960–968. doi: 10.1016/j.bbi.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Friedman EM, Hayney MS, Love GD, et al. Social relationships, sleep quality, and interleukin-6 in aging women. Proc Natl Acad Sci U S A. 2005;102:18757–18762. doi: 10.1073/pnas.0509281102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Savard J, Villa J, Ivers H, et al. Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol. 2009;27:5233–5239. doi: 10.1200/JCO.2008.21.6333. [DOI] [PubMed] [Google Scholar]
- 57.Diez-Ruiz A, Tilz GP, Zangerle R, et al. Soluble receptors for tumour necrosis factor in clinical laboratory diagnosis. Eur J Haematol. 1995;54:1–8. doi: 10.1111/j.1600-0609.1995.tb01618.x. [DOI] [PubMed] [Google Scholar]
- 58.Tangpong J, Cole MP, Sultana R, et al. Adriamycin-induced, TNF-alpha-mediated central nervous system toxicity. Neurobiol Dis. 2006;23:127–139. doi: 10.1016/j.nbd.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 59.Monk JP, Phillips G, Waite R, et al. Assessment of tumor necrosis factor alpha blockade as an intervention to improve tolerability of dose-intensive chemotherapy in cancer patients. J Clin Oncol. 2006;24:1852–1859. doi: 10.1200/JCO.2005.04.2838. [DOI] [PubMed] [Google Scholar]
- 60.Slavich GM, Way BM, Eisenberger NI, et al. Neural sensitivity to social rejection is associated with inflammatory responses to social stress. Proc Natl Acad Sci U S A. 2010;107:14817–14822. doi: 10.1073/pnas.1009164107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shai I, Schulze MB, Manson JE, et al. A prospective study of soluble tumor necrosis factor-alpha receptor II (sTNF-RII) and risk of coronary heart disease among women with type 2 diabetes. Diabetes Care. 2005;28:1376–1382. doi: 10.2337/diacare.28.6.1376. [DOI] [PubMed] [Google Scholar]