Thrombospondins are glycoproteins that associate with the extracellular matrix and have roles in cell signaling and tissue remodeling.
Abstract
Thrombospondins are evolutionarily conserved, calcium-binding glycoproteins that undergo transient or longer-term interactions with other extracellular matrix components. They share properties with other matrix molecules, cytokines, adaptor proteins, and chaperones, modulate the organization of collagen fibrils, and bind and localize an array of growth factors or proteases. At cell surfaces, interactions with an array of receptors activate cell-dependent signaling and phenotypic outcomes. Through these dynamic, pleiotropic, and context-dependent pathways, mammalian thrombospondins contribute to wound healing and angiogenesis, vessel wall biology, connective tissue organization, and synaptogenesis. We overview the domain organization and structure of thrombospondins, key features of their evolution, and their cell biology. We discuss their roles in vivo, associations with human disease, and ongoing translational applications. In many respects, we are only beginning to appreciate the important roles of these proteins in physiology and pathology.
Thrombospondins (TSPs) comprise a conserved family of extracellular, oligomeric, multidomain, calcium-binding glycoproteins. In general, basal metazoa and protostomes encode a single TSP in their genomes and deuterostomes have multiple TSP genes. The TSPs of mammals have many complex tissue-specific roles, including activities in wound healing and angiogenesis, vessel wall biology, connective tissue organization, and synaptogenesis. These activities derive mechanistically from interactions with cell surfaces, growth factors, cytokines, or components of the extracellular matrix (ECM) that collectively regulate many aspects of cell phenotype. Emerging evidence on the functions of TSPs in invertebrates suggests that ancient functions include bridging activities in cell–cell and cell–ECM interactions. Knowledge of TSP domain structures provides a rational basis for understanding their roles in vivo and associations with human disease and is assisting ongoing translational applications.
DOMAIN ARCHITECTURE AND DOMAIN STRUCTURES
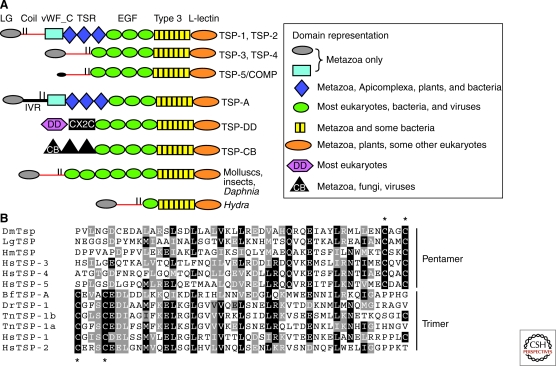
The domain architectures of representative TSP polypeptides are shown in Figure 1A. The invariant carboxy-terminal regions comprise a series of EGF-like domains, thirteen calcium-binding type 3 repeats, and a carboxy-terminal domain structurally homologous to the L-type lectin domain. This domain organization is the hallmark of a TSP and has also been termed the “signature” domain (Adams and Lawler 1993; Carlson et al. 2005). The amino-terminal halves of TSPs are much more varied in domain composition, with the laminin-G like (LG) amino-terminal domain (NTD) being the most widely conserved domain. The discoidin domain or Type 2 chitin-binding domains are present in some TSPs of invertebrates (Fig. 1A). A highly prevalent, although not invariant, feature of TSPs is an α-helical coiled-coil domain located adjacent to the NTD (red line in Fig. 1A) that mediates cotranslational oligomerization via formation of a left-handed super-helix. Vertebrate TSPs assemble either as trimers (subgroup A, comprising TSP-1 and TSP-2) or pentamers (subgroup B, comprising TSP-3, TSP-4, and TSP-5/COMP; TSP-5 is also known as cartilage oligomeric matrix protein [COMP]) (Lawler et al. 1985, 1995; Sottile et al. 1991; Mörgelin et al. 1992; Qabar et al. 1995). Residues important for pentamerization have been identified by mutational studies of the COMP/TSP-5 coiled-coil (Gunasekar et al. 2009). Oligomerization of TSPs is stabilized by intersubunit disulfide bonds formed between cystine residues adjacent to the amino-terminal end of the heptad repeats in trimeric TSPs or the carboxy-terminal end in pentameric TSPs (Fig. 1B) (Prochownik et al. 1989; Sottile et al. 1991; Qabar et al. 1995). Monomeric, dimeric, and pentameric TSPs exist in invertebrates (see also section on Evolution of Thrombospondins).
Figure 1.
Domain architectures of thrombospondins. (A) Schematic diagram of the domain architectures of thrombospondin family members. Key: LG = laminin G-like amino-terminal domain; vWF_C = von Willebrand type C domain; TSR = thrombospondin type 1 domains; EGF = epidermal growth factor-like domains; Type 3 = thrombospondin type 3 repeats; L-lectin = L-type lectin-like domain; DD = discoidin domain; IVR = intervening region; CX2C = Cys-X2-Cys domain; CB = chitin-binding type 2 domain. Horizontal red lines indicate coiled-coil domains. Vertical black lines indicate position of cysteine residues that form intersubunit disulfide bonds. (B) Examples of the coiled-coil oligomerization domain from representative trimeric and pentameric thrombospondins. Asterisks indicate cysteines that form intersubunit disulfide bonds.
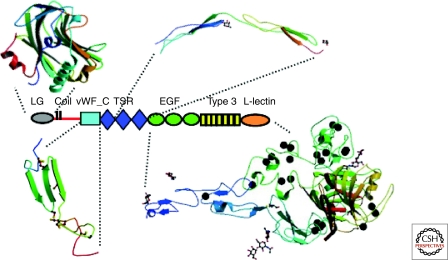
Structures for the major domains of TSPs have been solved by X-ray crystallography. The NTD of TSPs 1–4 folds as a Laminin-G domain (Tan et al. 2006). The structure of the vWF_C domain of TSPs has not been determined but is predicted to conform to the vWF_C domain of collagen IIA (Fig. 2) ([Protein Data Bank—PDB 1U5M] O’Leary et al. 2004). Each thrombospondin type 1 domain (TSR) corresponds to a novel fold composed of three β-strands with alternating orientation, stabilized by three disulfide bonds and cation-π bonds between highly conserved tryptophan residues in the first strand and two arginine residues in the second strand (Tan et al. 2002). This folding pattern brings together sequences from the first and second strands to form a positively charged groove on one surface of the TSR that is thought to represent the binding site for the CD36 receptor (see section Major Binding Partners). Around 90 proteins containing TSR domains are encoded in the human genome. Of those that have been characterized functionally, many are involved in cell–cell and cell–ECM interactions and cell migration (Adams and Tucker 2000). Proteins involved in axon guidance include F-spondin, SCO-spondin, and UNC-5; others include complement factors, proteases, and protease inhibitors (Tucker 2004).
Figure 2.
Structures of the domains of subgroup A thrombospondins. The crystal structures of LG (PDB 2ERF) and the second and third TSRs (PDB 1LSL) of TSP-1, and the carboxy-terminal region/signature domain of TSP-2 (PDB 1YO8) are shown. The vWF_C domain of TSP-1 is modeled on the solution structure of the vWF_C domain of collagen IIA (PDB 1U5M). Each domain is shown in a color gradient from blue at the amino terminus to red at the carboxyl terminus. The black spheres represent calcium ions. Note that the domains are not shown at the same scale.
In TSP-1 and -2, the three TSRs are followed by three epidermal growth factor-like (EGF) domains. TSP-3, -4, and -5/COMP and many TSPs of invertebrates contain larger numbers of EGF-like domains contiguous with the coiled-coil domain (Fig. 1A). Crystal structures have been solved for different portions of the carboxy-terminal regions of TSP-1 ([PDB 1UX6] Kvansakul et al. 2004), TSP-2 ([PDB 1YO8] Carlson et al. 2005) and TSP-5/COMP (Fig. 2) ([PDB 3FBY] Tan et al. 2009). Multiple intramolecular interactions between the EGF-like domains, the type 3 repeats, and the L-type lectin-like domain support the concept that this entire region folds and functions as a single structural unit. The carboxy-terminal region of TSP-2 has been divided into subregions described as a stalk (EGF-like domains 2 and 3), a clasp (EGF-like domain 3), a wire (the type 3 repeats), and the L-type lectin domain (Carlson et al. 2005). The thirteen type 3 repeats form an unusual protein structure in which a series of 26 calcium binding sites (DxDxD/N) are stabilized by disulfide bonds between adjacent repeats, calcium, and interactions with the L-type lectin domain (Kvansakul et al. 2004; Carlson et al. 2005). Removal of calcium leads to disassociation of the type 3 repeats from the L-type lectin domain (Annis et al. 2007). Two classes of type 3 repeat motif, [N] and [C], can be distinguished by their sequence length, the way in which the calcium ions are bound, and their interactions with water molecules (Kvansakul et al. 2004; Carlson et al. 2005; Tan et al. 2009). The importance of the type 3 repeats for the correct folding of the entire carboxy-terminal region is emphasized by the fact most point or single amino acid deletion mutations of human TSP-5/COMP that lead to pseudoachondroplasia (PSACH) or multiple epiphyseal dysplasia (EDM) occur in this region and disrupt protein conformation and calcium binding (see section TSP-5/COMP and PSACH). Coding polymorphisms in the carboxy-terminal regions of TSP-1 or TSP-4, or COMP-equivalent mutations in TSP-2 also affect calcium-binding and protein conformation (Stenina et al. 2003; Carlson et al. 2008a,b) (see section TSP Single Nucleotide Polymorphisms and Disease).
The carboxy-terminal L-type lectin-like domain contains 15 β-strands in two curved antiparallel β-sheets and also binds calcium ions (Kvansakul et al. 2004). All TSPs contain the sequence DDDYAGF in the loop between the β5 and β6 strands and two calcium ions are coordinated by the DDD motif. A third calcium-binding site is in close proximity to the DDDYAGF sequence and, in TSP-1, D956 and D975 coordinates a fourth calcium ion (Kvansakul et al. 2004; Tan et al. 2009).
EVOLUTION OF THROMBOSPONDINS
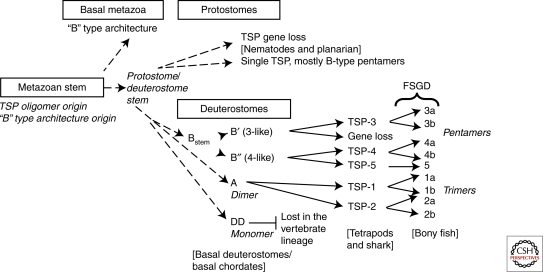
TSPs are exclusive to the metazoa. However, most of their component domains have premetazoan origins (Fig. 1). TSP pentamers apparently arose very early in the metazoa and have been highly conserved. Most protostomes and inferred basal metazoa encode a single TSP with the general domain organization of subgroup B TSPs and with a pentamerizing coiled-coil (Figs. 1 and 3). It appears that gene duplication and domain-shuffling events took place on the deuterostome stem lineage because all modern deuterostomes, urochordates, and cephalochordates encode three to four TSPs per genome. These include two novel forms: the TSP-A domain architecture and TSP-DD, a monomeric form with an amino-terminal discoidin-like domain that was lost from the vertebrate lineage (Figs. 1 and 3). Interestingly, TSP-As of Ciona, sea urchin, and acorn worm have all the major domains of TSP subgroup A yet do not contain a coiled-coil (Fig. 1A). The simplest explanation is that the trimerizing coiled-coils of TSP-1 and TSP-2 evolved separately from the pentamerizing coiled-coils (Bentley and Adams 2010).
Figure 3.
Model for the evolution of thrombospondins within the metazoa. FSGD = fish-specific genome duplication. (Diagram is a development of a figure originally published in Bentley and Adams [2010]. It is reprinted, with permission, from Oxford University Press © 2010.)
TSP evolution in vertebrates involved further gene duplications, likely resulting from the genome-wide duplications that occurred early in the vertebrate lineage, plus subsequent gene losses resulting in a total of five TSP genes in modern tetrapods (Fig. 3 and Table 1). A third genome duplication took place in the ray-finned fish lineage resulting in additional paralogs (Table 1) (McKenzie et al. 2006; Wu et al. 2009). Across both bony fish and tetrapods, orthologous TSP genes display conservation of synteny (Table 1) and Thbs3, Thbs4, and Thbs5/COMP are located in paralogous genomic regions, indicating their evolution as duplicated genes within the vertebrate lineage (Fig. 3). Interestingly, Thbs5/COMP of bony fish encodes a protein that is most closely related in sequence to tetrapod TSP-4 (even though the Thbs5/COMP gene product of both bony fish and tetrapods lacks an LG-NTD) (McKenzie et al. 2006). These data support the model that duplication of a Thbs4-like gene provided the origin for Thbs4 and Thbs5/COMP (Fig. 3). This model implies that TSP-5/COMP protein sequence has diverged faster in tetrapods than in bony fish, and thus might be evolving distinct functions in tetrapods.
Table 1.
Chromosomal locations of thrombospondin genes in representative vertebrates
|
Thbs gene |
Human | Mouse | Chicken | Pufferfish T. nigroviridis |
Zebrafish D. rerio |
|---|---|---|---|---|---|
| Thbs1 | 15q15 | 2 band F | 5 | 1a:14, 1b:10 | 20 |
| Thbs2 | 6q27 | 17 band A3 | 3 | 17 | 2a:13, 2b:12 |
| Thbs3 | 1q21 | 3 band E3 | Unmapped | Not in genome | 3a:16, 3b:19 |
| Thbs4 | 5q23 | 13-52 | Z | 4a:12, 4b:4 | 4aa:5, 4b:21 |
| Thbs5/COMP | 19p13.1 | 8-22 | 28 | 1 | 11b |
The locations of Thbs genes show conservation of synteny across the species (McKenzie et al. 2006).
aD. rerio TSP-4 paralogs were unmapped at time of publication of McKenzie et al. (2006), and in this paper NP_775333 was designated as D. rerio TSP-4a. However, NP_001107896, encoded on Danio chromosome 5, is now known to be adjacent metaxin-3, i.e., to have conservation of synteny with human THBS4. This gene is now designated D. rerio thbs4a.
bLocation according to Zv8 genome assembly.
CELL BIOLOGY OF THROMBOSPONDINS
Expression and Synthesis of TSPs
Data on the tissue expression profiles of TSPs have been collected from adult human or mouse tissues or mouse or chicken embryos; studies of other organisms are more fragmentary (Table 2). TSP-1 and TSP-5/COMP mRNA and protein are regulated by many environmental cues or pathological agents (Table 3). The synthesis of TSP polypeptides involves signal-mediated cotranslational transfer into the lumen of the endoplasmic reticulum (ER). Oligomerization of TSP-1 into trimers occurs through noncovalent association of the coiled-coil domains (Vischer et al. 1985; Prabakaran et al. 1996). Although TSPs are predominantly homooligomers, natural heteropentamers of TSP-4 and TSP-5/COMP subunits occur in tendon (Hecht et al. 1998; Södersten et al. 2006).
Table 2.
Tissue expression patterns of thrombospondins in vertebrates and invertebrates
| TSP | Tissue sites of expression | References |
|---|---|---|
| Mammalian | ||
| TSP-1 | Mouse embryo: */∧widespread, most prominent in heart, lung, intestinal epithelium, skeletal muscle, CNS Adult mouse or human: ∧more restricted, platelet α-granules, activated endothelium, ovary, cornea, lens; in healing wounds of skin, skeletal muscle, or spinal cord; neointima, atherosclerotic plaques |
Murphy-Ullrich and Mosher 1985; Raugi et al. 1987, 1990; O’Shea and Dixit 1988; Watkins et al. 1990; Corless et al. 1992; Iruela-Arispe et al. 1993; Hoffman et al. 1994; Hiscott et al. 1996, 1997; Moller et al. 1996; Roth et al. 1998; Greenaway et al. 2005 |
| TSP-2 | Mouse embryo: ∧cartilage growth zone, ∧skeletal muscle, ∧bone, *kidney, */∧adrenal gland, ∧skin, *brain, *lung, *heart Adult mouse: ∧Adrenal cortex, ∧bone marrow stromal cells. Adult human: *brain |
Laherty et al. 1992; Iruela-Arispe et al. 1993; Kyriakides et al. 1998; Tooney et al. 1998; Adolph 1999; Caceres et al. 2007 |
| TSP-3 | Mouse embryo: */∧CNS, *Meckle’s cartilage, *spinal cord, *lung, *bone, *skeletal muscle, *diaphragm, *intestine Adult mouse or human: *Kidney, *muscle, intestine, *lung, *heart, *tail, *skin, *bone, *skeletal muscle |
Vos et al. 1992; Iruela-Arispe et al. 1993; Lawler et al. 1993; Qabar et al. 1994 |
| TSP-4 | Adult mouse, rat, or human: *Heart, */∧skeletal muscle, *diaphragm, ∧tendon, ∧neuromuscular junction, ∧cerebellum, */∧hippocampus, *cerebral cortex, ∧retina, ∧blood vessels Adult mouse: ∧adventita of arteries, atherosclerotic lesions |
Lawler et al. 1993; Arber and Caroni 1995; Hauser et al. 1995; Chen et al. 2000; Stenina et al. 2003; Caceres et al. 2007; Frovola et al. 2010 |
| TSP-5/ COMP |
Mouse embryo: *skeletal muscle and all cartilaginous tissue Adult mouse or human: ∧articular cartilage, ∧synovium, ∧tendon, ∧skeletal muscle, ∧testis, ∧arteries, ∧eye, ∧heart |
Franzen et al. 1987; DiCesare et al. 1994a,b, 1997; Fang et al. 2000; Kipnes et al. 2000; Riessen et al. 2001; Wilson et al. 2010 |
| Avian TSP-1 TSP-2 TSP-3 TSP-4 |
Gallus gallus embryo: *CNS and floorplate, cartilage *Cartilage growth zone, tendon *CNS, spinal cord, lung, bone *Cornea, early osteogenic tissue |
Tucker 1993; Tucker et al. 1995, 1997 |
| Amphibian TSP-1 TSP-3 TSP-4 |
Xenopus laevis embryos: *Fertilized eggs, in embryo after gastrulation. In tadpole floor plate of neural tube, epidermis, somites, notochord, and alternating rhombomeres *In embryo after gastrulation. In tadpole notochord, floor plate, sensorial layer of the epidermis, and sensory epithelia *In embryo after gastrulation. In tadpole somitic mesoderm and skeletal muscle |
Lawler et al. 1993; Urry et al. 1998 |
| Bony Fish TSP-1 TSP-1a TSP-1b |
Danio rerio early embryos Oreochromis niloticus and Oryzias latipes: *Adult ovary with dynamic expression during the spawning cycle, granulosa cells, skeletal system, brain, intestine, heart, spleen Oreochromis niloticus and Oryzias latipes: *Gonads, theca cells of adult ovary, skeletal system, heart, spleen |
Wu et al. 2009; Zhou et al. 2009 Wu et al. 2009 |
| TSP-2 | Solea senegalensis: *in ovary, 2x up-regulated in atretic ovary relative to vitellogenic/mature ovary | Tingaud-Sequeira et al. 2009, EST accessions FF284909, FF284981 |
| TSP-5/ COMP |
Solea senegalensis: *in ovary, 2x up-regulated on vitellogenesis | |
| Invertebrate Drosophila TSP Prawn TSP-CB |
Embryo: *trunk mesoderm, wing imaginal disc, tendon cells of pharyngeal muscles, */∧myotendinous junction Marsupenaeus japonicus: */∧in cortical rods of vitellogenic and mature oocytes Fennerpenaeus chinensis: *in hemocytes, heart, intestine, stomach and ovary, induced in hepatopancreas on microbial challenge Penaeus monodon: *in ovary Penaeus monodon: *up-regulated in lymphoid organ on Vibrio harveyi infection |
Adams et al. 2003; Chanana et al. 2007; Subramanian et al. 2007 Yamano et al. 2004 Sun et al. 2006 Preechaphol et al. 2007 Pongsomboon et al. 2008 |
*Transcript, ∧protein.
Table 3.
Factors that regulate TSP-1, TSP-4, and TSP-5
| Factor | Regulation /cell type | Reference |
|---|---|---|
| Amino acids | Increased TSP-1 in glomerular mesangial cells | Meek et al. 2003 |
| Angiotensin II | Increased TSP-1 synthesis in vascular smooth muscle cells | Scott-Burden et al. 1990 |
| Cardiac overload | Increased TSP-1 and TSP-4 transcripts in left ventricle | Mustonen et al. 2008 |
| Extracellular ATP | Increased TSP-1 production by dendritic cells | Marteau et al. 2005 |
| Glucose | Increased TSP-1 synthesis by mesangial cells and vascular smooth muscle cells | Tada and Isogai 1998; Wang et al. 2004; Raman et al. 2007 |
| Heat shock | TSP-1 in endothelial cells | Ketis et al. 1988 |
| Herpes simplex virus type 1 | Suppression of TSP-1 transcript in endothelial cells | Ziaie et al. 1986 |
| Hypoxia | Increased TSP-1 transcript and protein in endothelial cells | Phelan et al. 1998 |
| Id-1 | Transcriptional repression of TSP-1; modulates angiogenesis | Volpert et al. 2002a |
| KSHV | Transcriptional silencing of TSP-1 by viral microRNAs | Samols et al. 2007 |
| Mechanical cyclic compression | Increased TSP-5/COMP transcript in articular cartilage explants | Giannoni et al. 2003 |
| Nedd4 ubiquitin ligase | Suppression of TSP-1 transcript in MEFs and heart | Fouladkou et al. 2010 |
| PDGF, HS-GAGs | TSP-1 synthesis in vascular smooth muscle cells | Majack et al. 1985 |
| TGFβ1 | Increased TSP-5/COMP synthesis by chondrocytes and synovial fibroblasts | Recklies et al. 1998 |
| Ultraviolet B | Decreased TSP-1 transcript in keratinocytes; increased TSP-1 transcript in dendritic cells | Howell et al. 2004; de la Fuente et al. 2009 |
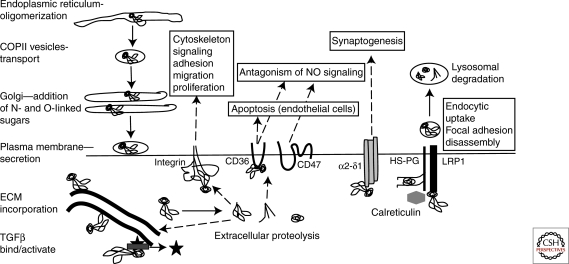
Quality control of TSP-1 polypeptide folding is mediated by ER chaperones (Kuznetsov et al. 1997). BiP, calreticulin, protein disulfide isomerase, ERp72, and grp94 are coretained with TSP-5/COMP in the Golgi of chondrocytes from PSACH patients (see section ROLES OF TSPS IN VIVO), suggesting that these chaperones also participate in its normal quality control (Hecht et al. 2001; Vranka et al. 2001). Trafficking of TSPs from ER to Golgi appears to be by COPII vesicles (Veliceasa et al. 2007). Sec23a-positive vesicles are implicated in trafficking wild-type TSP-5/COMP to the Golgi in chondrocytes (Fig. 4) (Saito et al. 2009).
Figure 4.
Overview of cellular pathways and activities of mammalian TSP-1 (not to scale).
While transiting the secretory pathway, TSP-1 becomes modified by N- and O-linked sugars (Furukawa et al. 1989; Nishimura et al. 1992). The TSRs undergo C-mannosylation of tryptophan residues within the WXXW motifs (Hofsteenge et al. 2001) and are also modified by the unusual disaccaride Glc-Fuc-O-Ser/Thr through the actions of protein O-fucosyl transferase 2 (POFUT2) and β1,3-glucosyltransferase, (β3GLT) (Kozma et al. 2006; Luo et al. 2006; Sato et al. 2006). The biological roles of these modifications of TSRs remain unclear; however, mutations of β3GLT cause a genetic disorder, Peters Plus syndrome (Hess et al. 2008).
Generally, TSPs are secreted from cells by constitutive pathways; an exception is the release of TSP-1 from stored platelet α-granules that are discharged on platelet activation (Blair and Flaumenhaft 2009). In apico-basally polarized cells, TSP-1 secretion is targeted to the basolateral membranes (Prabakaran et al. 1993, 1999; Gath et al. 1997).
Degradation of TSPs
Extracellular. After secretion, TSPs can be incorporated into extracellular matrices in cell culture and in vivo (Raugi et al. 1982; Jaffe et al. 1983; Vischer et al. 1985; DiCesare et al. 1994a; Schlötzer-Schrehardt et al. 2007; Adams et al. 2008). Alternatively, proteolytic fragments can be generated that either have a specific extracellular activity (Lee et al. 2006), or are internalized for full degradation (see below) (Fig. 4). Extracellular proteolysis of TSP-1 by thrombin or plasmin occurs during fibrinolysis and fibrin clot resolution (Lawler and Slayter 1981; Dixit et al. 1984; Bale and Mosher 1986) or during inflammation by elastase (Raugi et al. 1984; Hogg et al. 1993). Cleavage of TSP-1 by ADAMTS-1 releases antiangiogenic fragments (Lee et al. 2006). TSP-5/COMP is a substrate for MMP-19/-20 and ADAMTS-4/-7/-12 (Stracke et al. 2000; Dickinson et al. 2003; Liu et al. 2006a,b) and increased COMP fragments in synovial fluid are correlated with joint damage in rheumatoid arthritis and osteoarthritis (Neidhart et al. 1997).
Intracellular. TSP-1 and TSP-2 are endocytosed for intracellular degradation within lysosomes: the rate depends on the cell type and the expression of cell-surface glycosaminoglycans (McKeown-Longo et al. 1984; Murphy-Ullrich and Mosher 1987a,b; Murphy-Ullrich et al. 1988; Chen et al. 1996a). For TSP-1, endocytosis is mediated by binding of its LG-NTD to a ternary cell-surface complex of LDLR-related protein 1 (LRP1), extracellular calreticulin, and heparan sulphate proteoglycans (Fig. 4) (Godyna et al. 1995; Mikhailenko et al. 1995, 1997; Chen et al. 1996b; Orr et al. 2003; Wang et al. 2004a).
Major Binding Partners
TSPs have many binding partners; the best-validated are listed in Table 4. Integrin-binding by TSPs is important for their activities in cell attachment, spreading, and migration. The best-characterized interaction is that of the single RGD motif of TSP-1 with integrin αvβ3 and, to a lesser extent, with αIIbβ3 (Table 4) (Lawler et al. 1988; Lawler and Hynes 1989). The availability of this RGD motif for integrin-binding is promoted by incomplete calcium ion loading or reduction of disulfide bonds within the type 3 repeats (Sun et al. 1992; Kvansakul et al. 2004). Many cells undergo RGD-independent attachment to calcium-replete TSP-1 or TSP-2 (reviewed in Adams 2004). Many TSPs contain RGD and KGD potential integrin-binding motifs at other locations in the type 3 repeats. Few of these have been tested functionally, however, the RGD motif of TSP-5/COMP is implicated in binding α5β1 and, under reducing conditions, αvβ3 (Chen et al. 2005). The KGD motif of Drosophila TSP is needed for αPS2 integrin-dependent cell adhesion in vitro (Subramanian et al. 2007). TSP-1 and TSP-2 also bind several non-RGD-dependent integrins including α4β1 (Table 4). Binding sites for integrins α3β1 and α6β1 have been mapped to the LG-NTD, yet the physiological significance of these remains uncertain because the identified motifs are not fully surface-exposed in the crystal structure (Krutzsch et al. 1999; Calzada et al. 2003; Tan et al. 2006). However, α3β1 binding may be favored in calcium-depleted TSP-1 (Rodrigues et al. 2001). β1 integrins are also implicated in interactions with the TSRs and EGF-like domains (Calzada et al. 2004b).
Table 4.
Mapped binding partners
| TSP domain | Motif | Binding partner | Reference |
|---|---|---|---|
| LG-NTD | Positive patch involving R29,K32,R42,R77,K80,K81, K106a MKKTRGa E17LTGAARKGSGRRLVKGPDaA159ELDVPaI151DCEKMENAELDVPa | HS-glycosaminoglycansDecorinCalreticulinα4 Integrin Fibrinogen | Lawler et al. 1992; Tan et al. 2006,Merle et al. 1997,Murphy-Ullrich et al. 1993; Goicoechea et al. 2000,Calzada et al. 2004a,Voland et al. 2000 |
| Type 1 repeats | WSXWSeCSVTCGeW420SHWSPWcK412RFKb | HS-glycosaminoglycansCD36TGF-β bindingTGF-β activationb | Guo et al. 1992,Asch et al. 1992,Schulz-Cherry et al. 1995,Ribeiro et al. 1999 |
| Type 3 repeats | RGDa,d | β1 Integrin, β3 integrin | Lawler et al. 1988; Lawler and Hynes 1989; Chen et al. 2005; |
| KGD | PS2 Integrin | Chanana et al. 2007; Subramanian et al. 2007 | |
| L-type lectin domain | GVDFEGTFHVNTVTDDD | Fibrillar collagendCollagen IXdMatrilin-3d | Holden et al. 2001 |
Binding partners of thrombospondins. The interactions listed are those for which the binding site has been mapped within the relevant TSP domain and is surface-exposed in the domain structure, as determined by X-ray crystallography.
aIdentified in TSP-1.
bSpecific to TSP-1.
cPresent in the second type 1 domain of both TSP-1 and TSP-2.
dIdentified for TSP-5/COMP. The DDD motif is also surface-exposed in TSP-1 and TSP-2 and is conserved in most TSPs.
ECM incorporation is a conserved property of TSPs and, through their multivalent structures, TSPs likely function as molecular bridges to facilitate ECM organization. Incorporation of TSP-1 into culture ECM depends on the carboxy-terminal region in trimeric form. This activity is partially inhibited by mutation of the three highly conserved aspartic acid residues that coordinate two calcium ions in the L-lectin domain (see section DOMAIN ARCHITECTURE AND DOMAIN STRUCTURES) (Adams et al. 2008). The DDD motif is also part of a motif in TSP-5/COMP reported to bind collagen IX (Table 4) (Holden et al. 2001). In vitro, TSP-5/COMP acts as a catalyst for collagen fibrillogenesis (Halász et al. 2007; Hansen et al. 2011). Other important interactions are with glycosaminoglycans. Cocrystals of the TSP-1 LG-NTD with heparin oligosaccharides revealed that R29, R42, and R77 form a positively charged patch that binds to sulfate groups on the heparins (Tan et al. 2006, 2008). Molecular docking studies indicate that longer heparins might also interact with other positively charged residues and bridge between LG-NTDs; this might contribute to the high affinity of heparin binding by TSP-1 (San Antonio et al. 1993). R29 and R42 are in a 26 aa segment absent from TSP-3 or TSP-4, thus these TSPs probably engage heparin through other positively charged residues in LG-NTD. TSP-5/COMP has no LG-NTD yet binds with high affinity to chondroitin sulfate and heparin (Chen et al. 2007); this is likely mediated by positively charged patches on the surface of the type 3 repeats and L-lectin domain (Tan et al. 2009). Interactions with other ECM ligands are, as yet, unmapped (Table 5).
Table 5.
Unmapped binding partners
| TSP domain | Binding partner | Reference |
|---|---|---|
| LG-NTD | Link domains of versican and TSG-6 | Kuznetsova et al. 2006 |
| TSR | Collagen V Glycosaminoglycans (low affinity binding) MMP-2, MMP-9 |
Takagi et al. 1993,Bein and Simon 2000 |
| Carboxy-terminal region (EGF to L-lectin domain) | von Willebrand factor multimersbFibrillar collagens (TSP-1, TSP-4, TSP-5) Laminin, fibronectin, matrilin-2 (TSP-4) Fibronectin (TSP-5) Aggrecan (TSP-5) |
Pimanda et al. 2004 DiCesare et al. 2002 Galvin et al. 1987 Rosenburg et al. 1998; Narouz-Ott et al. 2000; Thur et al. 2001; Mann et al. 2004; Chen et al. 2007 |
Binding partners of thrombospondins—domain assigned but unmapped interactions.
HS, heparan sulphate.
aIdentified in TSP-1.
bSpecific to TSP-1.
cPresent in the second type 1 domain of both TSP-1 and TSP-2.
dIdentified for TSP-5/COMP. The DDD motif is also surface-exposed in TSP-1 and TSP-2 and is conserved in most TSPs.
eThese motifs are present in each of the type 1 domains of TSP-1 and TSP-2.
Other interactions of TSPs are with growth factors and proteases. The interaction with TGFβ1 is particularly complex and is specific to TSP subgroup A members. The WSHWSPW motif located in the second TSR of TSP-1 and TSP-2 binds to VLAL motifs present in both TGFβ1 and its latency-associated peptide that together form the small latent complex (SLC) (Schultz-Cherry et al. 1995; Young and Murphy-Ullrich 2004). Binding of SLC may serve to localize inactive TGFβ1 at specific sites within ECM or in proximity to cell surfaces. In addition, TSP-1 specifically activates TGFβ1 by triggering its dissociation from SLC by an interaction of the KRFK motif (located between the first and second TSR) with a LSKL motif proximal to the amino terminus of the latency-associated peptide (Schultz-Cherry et al. 1995; Ribeiro et al. 1999). The TSRs of TSP-1 and TSP-2 also interact with matrix metalloprotease-2 and -9 (MMP-2 or MMP-9) and this inhibits MMP activity (Bein and Simon 2000). TSP-2 also modulates the extracellular levels of MMP-2 because of endocytosis of TSP-2/MMP2 complexes by LRP1 (Yang et al. 2000, 2001).
TSP-1 binds to vascular endothelial cell growth factor (VEGF), a potent proangiogenic factor that is opposed in certain physiological situations or tumors by antiangiogenic activities of TSP-1 and TSP-2 (see section Endothelial Cells and Antiangiogenesis). In the ovary, VEGF binding to TSP-1 results in endocytosis and degradation via LRP1 (Greenaway et al. 2007). In endothelial cells, CD36 and β1 integrin associate in cis with VEGF receptor 2 (VEGFR2) and signaling by VEGFR2 is modulated by the level or activity of TSP-1 (Zhang et al. 2009). Also of interest is the binding of Notch3 and its ligand Jagged1 by TSP-2, which increases ligand-dependent signaling through the Notch pathway. This activity depends on Notch3 extracellular domain and the presence of LRP1 on the ligand-producing cells for the endocytic uptake of cleaved Notch3 extracellular domain (Meng et al. 2010). Complexes of TSP-1 with Notch3 and Jagged1 do not potentiate Notch signaling (Meng et al. 2009).
It is interesting that many binding activities of mammalian TSPs represent either coevolutionary innovations in the deuterostome lineage (for example, TGFβ1 binding by the TSR, or fibrinogen binding by LG-NTD), or neo-functions of ancient molecules such as CD36 or calreticulin. In contrast, binding to glycosaminoglycans, fibrillar collagen, or RGD-dependent integrins represent widely conserved and likely ancestral activities. CD47 is encoded only in amniotes and thus cannot be an evolutionarily ancient ligand of TSP-1 (Bentley and Adams 2010). These findings help us distinguish which interactions might be most appropriate for building synthetic ECM, or as therapeutic targets distinct from ECM organization.
Functions of TSPs at Cellular Level
Fundamental properties attributed to all TSPs examined to date include interactions with ECM components and glycosaminoglycans and support of calcium-dependent cell attachment. Other activities, investigated with regard to particular TSP family members or cell types, include the induction of cell spreading with organization of actin-based protrusions, cell migration, disassembly of focal adhesions, cell-dependent stimulation or inhibition of cell proliferation or apoptosis, stimulation of synaptogenesis by neuronal cells, and antagonism of nitric oxide signaling in vascular cells (reviewed by Adams 2001, 2004; Bornstein et al. 2004; Zhang and Lawler 2007; Isenberg et al. 2009). Here, we summarize the cellular activities of TSPs that underlie their roles in cell–cell and cell–ECM interactions. The biological significance of these activities is discussed in the section ROLES OF TSPS IN VIVO.
Endothelial Cells and Antiangiogenesis
TSP-1 and TSP-2 are specific activators of apoptosis in microvascular endothelial cells (Dawson et al. 1997, 1999). This leads to inhibition of endothelial tubule formation in vitro, and the antiangiogenic activities of TSP-1 and TSP-2 in vivo (see section ROLES OF TSPS IN VIVO). At the molecular level, the TSRs interact with the transmembrane glycoprotein CD36, likely via the positively charged groove of the TSR (Fig. 4) (Asch et al. 1992; Dawson et al. 1997; Jiminez et al. 2000, 2001; Simantov et al. 2005; Yee et al. 2009). Additional motifs within the TSRs, implicated in heparin-binding activity, also contribute to antiangiogenic activity (Iruela-Arispe et al. 1999).
CD36 is a multifunctional 88kDa glycoprotein with two small cytoplasmic domains at its amino and carboxyl termini. TSP binding involves a short region of the extracellular domain (Asch et al. 1992; Frieda et al. 1995). Inhibition of angiogenesis by TSP-1 depends on residues in the carboxy-terminal cytoplasmic domain (Primo et al. 2005). Ligation of CD36 by TSP-1 or -2 results in intracellular association of Src family kinases, fyn or yes, activation of their kinase activities, and phosphorylation of caspases and JNK leading to apoptosis (Jimenez et al. 2001). Binding of TSP-1 to CD36 also increases expression of death receptors and Fas ligand, thereby sensitizing endothelial cells to apoptosis (Volpert et al. 2002b; Ren et al. 2009). Cell cycle progression and MAP kinase signaling in microvascular endothelial cells are also limited by a nonapoptotic mechanism involving association of the carboxy-terminal region of TSP-2 and VLDL receptor (Oganesian et al. 2008). Antiangiogenesis by TSP-1 and TSP-2 has aroused great interest as a possible therapeutic strategy to block tumor angiogenesis or treat diabetic retinopathy (see sections ROLES OF TSPS IN VIVO and TRANSLATIONAL APPLICATIONS).
Smooth Muscle Cell Migration and Proliferation
TSP-1 is elevated in the neointima of injured arteries or atherosclerotic plaques (Table 2). In cell culture, TSP-1 supports smooth muscle cell (SMC) adhesion, proliferation, and migration (Majack et al. 1986; Yabkowitz et al. 1993; Patel et al. 1997). Under conditions of elevated nitric oxide (NO), the effect of TSP-1 is reversed to inhibit these cell behaviors. This is mediated by TSP-1 binding to CD36 on SMC, resulting in reduced intracellular cyclic GMP (cGMP) levels (Isenberg et al. 2006a, 2007a). Activation of SMC migration by TSP-1 is mediated by αvβ3 and β1 integrins (Lymn et al. 2002; Isenberg et al. 2005) and stimulates assembly of fascin-containing cell protrusions (Anilkumar et al. 2002).
For both smooth muscle cells and endothelial cells, TSP-1 modulates adhesion and promotes motility by antagonizing focal adhesion assembly in response to ECM components such as fibronectin. This activity depends on a motif in the LG-NTD and is mediated by cGMP- and PI 3-kinase-dependent signaling (Murphy-Ullrich et al. 1996; Greenwood et al. 2000). These signals are transduced by a complex of LRP1, cell-surface calreticulin and LG-NTD (Fig. 4) (Orr et al. 2003). Signaling from this complex via Akt also promotes cell survival (Pallero et al. 2008).
Antagonism of Nitric Oxide Signaling
Regulation of NO signaling by TSP-1 in the vasculature affects SMC, endothelial cells and platelets (reviewed by Isenberg et al. 2009). NO is an important regulator of tissue perfusion, platelet function, and vascular tone that is synthesized and released by endothelial cells and enters vascular SMC or platelets by diffusion. In all these cells, the intracellular activity of NO is to bind and activate soluble guanylate cyclase to increase cGMP; this decreases SMC contractility, reduces platelet adhesion and aggregation, and has biphasic effects on endothelial cell proliferation. TSP-1 and TSP-2 inhibit NO-dependent stimulation of proliferation (Isenberg et al. 2005). TSP-1 also counteracts SMC relaxation by NO and increases contractility and the antithrombotic activity of NO on platelets (Isenberg et al. 2006a, 2007b, 2008a). In endothelial cells, the relationship between TSP-1 and NO is complex and triphasic. Low doses of NO are proangiogenic because of suppression of TSP-1 production (Ridnour et al. 2005), and picomolar concentrations of TSP-1 inhibit NO signaling in both endothelial cells and SMC (Isenberg et al. 2005, 2006a). Antagonism of NO signaling by TSP-1 depends on CD36 and the inhibition of myristate uptake by CD36 (Isenberg et al. 2005, 2006a, 2007a). However, in CD36-null cells, NO signaling is inhibited by a mechanism dependent on the immunoglobulin superfamily member CD47 (Isenberg et al. 2006b).
Chondrocytes and Osteoblasts
All five TSPs of mammals are present in cartilage and bone where they have roles in cell–ECM interactions (reviewed by Hankenson et al. 2010). TSP-1 inhibits mineralization by osteoblastic cells or retinal pericytes (Canfield et al. 1996; Ueno et al. 2006), whereas TSP-2 promotes mineralization by preosteoblasts (Alford et al. 2010). TSP-5/COMP produced by chondrocytes is important for the organization of other matrix components; for example, Thbs5–/–: colIIX–/– cultured chondrocytes incorporate less matrilin-3 into their ECM as compared to wild-type chondrocytes (Blumbach et al. 2009) (see also section TSP-5/COMP and PSACH).
Skeletal Muscle
Skeletal myoblasts adhere and migrate on TSP-1 or TSP-2 because of formation of fascin-based protrusions. This response depends on trimeric assembly of the carboxy-terminal region (Anilkumar et al. 2002). Whereas ligation of syndecan-1 by TSP-1 strongly activates F-actin bundling by fascin, the ligation of integrin α5β1 by fibronectin promotes protein kinase C-dependent phosphorylation of fascin, thereby inhibiting its actin-bundling activity (Adams et al. 1999; Anilkumar et al. 2003). Muscle explant cultures have shown multiple roles of TSP-1 in muscle, involving modulation of collagen α1 and α2 secretion that impacts endothelial cell outgrowth and proliferation, and also modulation of SMC migratory capacity (Zhou et al. 2006).
Neuronal Cells
Interactions with neuronal cells are shared properties of mammalian trimeric and pentameric TSPs. Both TSP-1 and TSP-4 support neurite outgrowth (O’Shea et al. 1991; Arber and Caroni 1995); in the case of TSP-4, this may involve interplay with laminin (Dunkle et al. 2007). TSP-1 is also important for developmental neuronal cell migration in the rostral migratory stream. In these cells, TSP-1 binds ApoER2 and VLDLR to induce phosphorylation of the intracellular signaling protein, Dab1 (Blake et al. 2008).
All TSPs secreted by mammalian astrocytes promote assembly of excitatory glutamatergic synapses within the CNS. TSP-induced synapses in culture are ultrastructurally normal and presynaptically active, but lack postsynaptic activity (Christopherson et al. 2005; Eroglu et al. 2009). TSPs do not promote inhibitory GABAergic synaptogenesis (Hughes et al. 2010). Glutamatergic synapatogenic activity is mediated by interaction of the EGF-like domains of TSPs with the vWF_A domain of α2δ-1, a ubiquitously expressed, nonessential subunit of L-type calcium channel that is the target of the drug gabapentin (Eroglu et al. 2009). Synaptogenesis as a result of this interaction is independent of the cytoplasmic domain of α2δ-1; thus, it is likely that additional downstream processes are required for the necessary cytoskeletal and membrane reorganizations, the nature of which remain to be established. In hippocampal neurons, a TSP-1/neuroligin 1 interaction was implicated in promoting synaptogenesis (Xu et al. 2010). Collectively, the data suggest that synaptogenic activity of TSPs is mediated via a multiprotein complex on neuronal cell surfaces (see also article by Barros et al. 2010).
ROLES OF TSPS IN VIVO
Analyses in Drosophila and Mice
Drosophila
Drosophila TSP (D-TSP) is a pentameric, heparin-binding glycoprotein that incorporates into ECM in culture (Adams et al. 2003). In embryos, D-TSP expressed at segmental boundaries is under control of hedgehog signaling in tendon precursor cells, or the transcription factor stripe in differentiated tendon cells (Chanana et al. 2007). D-TSP colocalizes with tiggrin in the ECM at tendon/muscle cell attachment sites. In embryos lacking D-TSP, the longitudinal muscles detach from tendon cells once muscle contractions begin, resulting in lethality. Although tiggrin, PS1, and PS2 integrins are expressed normally by muscle cells in tsp mutant embryos, these proteins do not polarize properly at tendon/muscle cell attachment sites, suggesting that D-TSP is important for organization of the tendon ECM. D-TSP has been identified as a PS2 integrin ligand by both genetic and functional criteria (Chanana et al. 2007; Subramanian et al. 2007). This interaction is regulated by another secreted protein of tendon cells, slowdown. In vitro, slowdown undergoes KGD-modulated association with D-TSP, suggesting that it acts by steric competition (Gilsohn and Volk 2010).
Mice
Phenotypes of mice homozygous for “knockouts” of single TSP genes are summarized in Table 6. All single gene knockouts are viable, as are double Thbs1–/–; Thbs2–/– mice (Agah et al. 2002) and triple Thbs1–/–; Thbs3–/–; Thbs5–/– mice (Posey et al. 2008). Whereas columnar stacking of chondrocytes in growth plates is mildly disrupted in Thbs5–/– mice, the triple Thbs1–/–; Thbs3–/–; Thbs5–/– results in a stronger phenotype (Posey et al. 2008). In relation to the action of astrocyte-secreted TSPs on synaptogenesis (see section Neuronal Cells), formation of synapses in the developing brains of Thbs1–/– or Thbs2–/– mice is indistinguishable from that of wild-type mice. However, Thbs1–/–; Thbs2–/– mice have a 40% decrease in the number of synapses by postnatal day 8 (Christopherson et al. 2005). Thbs1–/–; Thbs2–/– mice recover poorly after experimentally induced stroke, with reduced synaptic recovery and axonal sprouting, indicative of lifelong roles for TSPs in synaptic plasticity (Liauw et al. 2008).
Table 6.
Constitutive and experimentally induced phenotypes of Thbs gene knockout mice
| TSP | Mouse gene knockout phenotype | Reference |
|---|---|---|
| TSP-1 | Decreased embryonic viability Spinal lordosis Pneumonia from 1 month after birth Reduced active TGFβ in lung and pancreas Decreased survival and osteosarcoma incidence in p53-null mice Delayed healing of skin wounds Increased vascular density during retinal development Reduced plasma vWF multimer size Reduced inflammation and proteinurea in experimental glomerulonephritis Increased inflammatory response and granulation tissue in healing myocardial infarcts Reduced platelet vessel wall adherence and thrombus formation on endothelial injury Reduced smooth muscle cell activation and neointima formation after carotid artery ligation Reduced active TGFβ in glomeruli after experimental diabetic nephropathy Increased tissue survival after ischemic injury Decreased age-linked susceptibility to ischemic injury Resistance of soft tissue to radiation injury Increased susceptibility and angiogenic response to experimental inflammatory bowel disease Accelerated atherosclerotic plaque maturation in ApoE–/– mice Increased cardiac and skeletal muscle capillarity and exercise capacity |
Lawler et al. 1998 Crawford et al. 1998 Lawler et al. 2001 Agar et al. 2002 Wang et al. 2003 Pimanda et al. 2004 Hochegger et al. 2004 Frangogiannis et al. 2005 Bonnefoy et al. 2006 Moura et al. 2007 Daniel et al. 2007a Isenberg et al. 2007b Isenberg et al. 2007c Isenberg et al. 2008b Punekar et al. 2008 Moura et al. 2008 Malek et al. 2009 |
| TSP-2 | Fragile skin, lax tendons with enlarged collagen fibrils Twofold increase in bone density Cortical thickening of long bones Increased vascular density Prolonged bleeding time Accelerated healing of skin wounds Increased vascularity of foreign body reaction Altered organization of fibrotic capsule Increased proliferation of osteoblast precursor cells Accelerated skin carcinogenesis with increased tumor angiogenesis Increased inflammation and angiogenesis in delayed-type hypersensitivity reaction Altered bone marrow ultrastructure and megakaryocyte differentiation Increased susceptibility to angiotensin II-induced fatal cardiac rupture Increased osteoblastogenesis and decreased bone resorption after ovariectomy Increased endocortical bone formation in response to mechanical load Increased early phase inflammatory response and MMP-2 activity in experimental glomerulonephritis Altered lamellar morphology of lumbar discs Altered cartilage/bone ratio during bone fracture healing Reduced notch3 target gene expression Increased age-related dilated cardiomyopathy and age-related mortality Inhibition of adipogenesis |
Kyriakides et al. 1998 Kyriakides et al. 1999a Kyriakides et al. 1999b Hankenson et al. 2000 Hawighorst et al. 2001 Lange-Asschenfeldt et al. 2002 Kyriakides et al. 2003 Schroen et al. 2004 Hankenson et al. 2005a Hankenson et al. 2006 Daniel et al. 2007b Gruber et al. 2008 Taylor et al. 2009 Meng et al. 2009 Swinnen et al. 2009 Shitaye et al. 2010 |
| TSP-3 | Transient alteration of biomechanical properties of bone (PN weeks 9–15) Accelerated ossification of the head of the femoral bone |
Hankenson et al. 2005b |
| TSP-4 | No overt phenotype. Thbs4–/–; ApoE–/– mice have reduced development of atherosclerotic lesions and reduced vascular inflammation in lesions | Frolova et al. 2010 |
| TSP-5/COMP | No detectable skeletal phenotype in unchallenged mice Altered growth plate organization |
Svensson et al. 2002 Posey et al. 2008 |
See text for discussion of additional phenotypes in mice that lack multiple TSP family members.
Many other phenotypes of Thbs1–/– and Thbs2–/– null mice (Table 6) stem from the roles of TSP-1 and TSP-2 in inhibiting angiogenesis or suppressing nitric oxide signaling (see section CELL BIOLOGY OF THROMBOSPONDINS). Thbs1–/– mice have increased blood vessel density in cardiac and skeletal muscle, retina, and iris (Table 6) (Cursiefen et al. 2004). In contrast, vascular permeability response to VEGF is significantly diminished in Thbs1–/– mice (Zhang et al. 2009). One antiangiogenic mechanism of TSP-1 is by promoting clearance of VEGF (see section Major Binding Partners), and Thbs1–/– retinal endothelial cells display changes in the distribution of Src family kinases (Wang et al. 2006; Sun et al. 2009). Increased MMP activity in the pericellular space of Thbs1–/– and Thbs2–/– mice affects both cell adhesion and angiogenesis (Rodriguez-Manzaneque et al. 2001; Maclauchlan et al. 2009) In Thbs2–/– mice, increased MMP-2 activity leads to degradation of tissue transglutaminase, decreased integrin activity and weaker collagen fibrils (Agah et al. 2005).
Thbs1–/– and Thbs2–/– mice have opposite phenotypes in wound healing models (Table 6). Because TSP-1 is delivered to wounds by platelets at the time of injury, wounds in Thbs1–/–;Thbs2–/– mice follow the delayed healing pattern of Thbs1–/– mice (Agah et al. 2002). If the survival of the tissue is limited by ischemia, as in experimental models of kidney ischemia/reperfusion injury or the cutaneous flap assay, Thbs1–/– mice recover better than wild-type controls as a result of increased tissue perfusion in the absence of NO signaling suppression (Table 6) (Thakar et al. 2005; Isenberg et al. 2007b). Thbs1–/–-specific phenotypes are caused by decreased levels of activated TGFβ (Miao et al. 2001; see section CELL BIOLOGY OF THROMBOSPONDINS). TSP-1 activates TGFβ in wound healing, immune response, myocardial infarction, renal fibrosis, diabetes, experimental autoimmune uveoretinitis, and tumor progression (Table 6). Inflammatory cell recruitment and fibrosis are decreased during these processes in Thbs1–/– mice. The immune privilege of retinal pigment epithelial cells is maintained by TSP-1-mediated activation of TGFβ (Zamiri et al. 2005). Some disease phenotypes in Thbs2–/– mice are related to aging and indeed Thbs2–/– mice display increased age-related mortality (Table 6). Collectively, these results highlight the complexity of interpreting the diverse phenotypes of TSP-deficient mice: in the absence of TSP-1 or TSP-2 an extensive network of interacting proteins are disrupted with multiple tissue-specific phenotypic consequences.
Roles in Mouse Cancer Models
In general, tumor cells down-regulate TSP-1 expression to promote angiogenesis (Ren et al. 2006). This endpoint is achieved by multiple mechanisms, including: (1) secretion of soluble factors that down-regulate TSP-1 in surrounding fibroblasts (Kalas et al. 2005), (2) loss of TSP-1-dependent inhibition of tumor growth or endothelial cell migration by TGFβ activation (Miao et al. 2001, Motegi et al. 2008), (3) inhibition of VEGF mobilization from the extracellular matrix by MMP-9 (Rodriguez-Manzaneque et al. 2001), (4) down-regulation of circulating endothelial cell progenitors (Shaked at al. 2005), (5) induction of endothelial cell apoptosis (Jimenez et al. 2000), and (6) suppression of melanoma growth by recruitment of M1 macrophages and innate antitumor immunity (Martin-Manso et al. 2008). Megakaryocytes and platelets represent key sources of TSP-1 that regulate bone marrow and tumor angiogenesis (Kopp et al. 2006; Zaslavsky et al. 2010). The tumor-suppressive role of TSP-1 is supported by findings that, in the absence of TSP-1, tumors progress more rapidly in neu/erbB2, APCMin/+, and p53-deficient mouse models (Lawler et al. 2001; Rodriguez-Manzaneque et al. 2001; Gutierrez et al. 2003).
TSP-1 is reported to both inhibit and stimulate metastasis. Inhibitory effects in some cancer models are probably secondary to inhibition of angiogenesis (Weinstat-Saslow et al. 1994; Hawighorst et al. 2001). Because lymphatic vessels have little or no CD36 in vivo, TSP-1 does not inhibit tumor-associated lymphangiogenesis or tumor cell spread to regional lymph nodes (Hawighorst et al. 2001). TSP-1 also reportedly mediates the antimetastatic effect of prosaposin, the precursor form of the lipid hydroxylase activators saposin A-D (Kang et al. 2009). Contrary to these results, TSP-1 promotes metastasis in a transgenic model of breast cancer, likely because of promotion of cell migration (Yee et al. 2009). Migration of invasive breast, melanoma, or thyroid cancer cell lines is also promoted by TSP-1 in vitro (Wang et al. 1996; Albo et al. 1998; Nucera et al. 2010). In several cases, increased migration correlates with elevated activity of extracellular proteases (Albo et al. 1998; Liu et al. 2009). These data further underscore the pleiotropic activities of TSP-1 in cell–ECM interactions and the differential responses of various cell types, resulting in multifaceted effects on tumor progression.
Data from Humans
TSP-5/COMP and PSACH
COMP/THBS5 is the causal gene for PSACH ([Online Mendelian Inheritance in Man—OMIM177170] Newton et al. 1994; Briggs et al. 1995; Hecht et al. 1995). Individuals heterozygous for a mutant allele have shortened stature, joint laxity, joint erosion and pain, and early onset osteoarthritis. Subsequent studies have shown that: (1) PSACH mutations occur in multiple locations of the coding sequence of COMP/THBS5, and (2) mutations can also lead to EDM1 (OMIM132400) (Posey and Hecht 2008). Because mutations of collagen IX or matrilin-3 also lead to forms of EDM, the three proteins might work in concert during cartilage ECM assembly.
In PSACH patients and, to a lesser extent, EDM patients, the ER of chondrocytes is dilated with alternating electron-dense and electron-lucent layers that contain collagen II, TSP-5/COMP, collagen IX, matrilin-3, aggrecan, and other ECM proteins (Briggs and Chapman 2002; Merritt et al. 2007). Pulse-chase experiments indicate that many TSP-5/COMP mutants are secreted less rapidly than wild type (Chen et al. 2008). The increased transit time in the ER results in increased interactions between the ECM proteins leading to formation of inclusions and ER stress, chondrocyte death, and premature slowing of bone growth. Some TSP-5/COMP mutations have less severe effects on protein secretion and these may affect extracellular functions of TSP-5/COMP.
Because gene deletion of Thbs5/COMP has minor phenotypic consequences in mice (Table 6), the concept of silencing TSP-5/COMP expression, to reduce the burden of mutant TSP-5/COMP in chondrocytes, is gaining interest as a possible therapeutic strategy. A hammerhead ribozyme against the common D569del mutation significantly reduces mutant TSP-5/COMP mRNA levels in chondrocytes (Alcorn et al. 2009). Reduced TSP-5/COMP levels, ER stress, and intracellular retention of other ECM proteins have been achieved with short hairpin RNA against TSP-5/COMP in cultured cells (Posey et al. 2010).
TSP Single Nucleotide Polymorphisms and Disease
Single nucleotide polymorphisms (SNPs) in TSP-1, -2, and -4 correlate with increased risk of premature myocardial infarction (Topol et al. 2001). However, a recent meta-analysis failed to detect significant correlations (Koch et al. 2008). Nevertheless, biochemical and cellular analyses of the N700S and A387P SNPs of TSP-1 and TSP-4, respectively, have identified effects on calcium binding, protein conformation, and interactions with cells and ECM components of the vessel wall and platelet clot (Stenina et al. 2003, 2005; Narizhneva et al. 2004; Carlson et al. 2008b). It is possible that subtle differences in the patient populations may account for the discrepancies in clinical correlations. For example, the TSP-2 SNP correlates with cases that involved plaque erosion (Burke et al. 2010). Another TSP-2 SNP affects skipping of exon 11 and correlates with lumbar-disc herniation in the Japanese population. Exon 11 encodes the third TSR of TSP-2 and without this TSR, TSP-2 has reduced binding to MMPs (Hirose et al. 2008).
TRANSLATIONAL APPLICATIONS
TSR Domains, Angiogenesis, and Cancer
Therapeutic strategies to exploit the antiangiogenic activity of TSP-1 and -2 have become of great interest (reviewed by Zhang and Lawler 2007). Approaches demonstrating significant efficacy in mouse preclinical models include the delivery of synthetic peptides or recombinant proteins through direct injection, adeno-associated viruses, or cells. A peptide mimetic, ABT-510, based on the second strand of the second TSR, was taken to phase II clinical trials by Abbott Laboratories; however, as a single agent, ABT-510 did not have significant clinical efficacy against metastatic melanoma and renal cell carcinoma (Westphal 2004; Ebbinghaus et al. 2007; Markovic et al. 2007). Recombinant proteins that also include the RFK sequence that activates TGFβ1 (see section Major Binding Partners), have increased antitumor activity in a mouse model (Miao et al. 2001; Yee et al. 2009). Cell-based strategies to deliver intact TSP-1, TSP-2, or the TSRs have been developed and have provided effective inhibition of several experimental cancers (Streit et al. 2002; van Eekelen et al. 2010). ABT-510 improved the uptake and efficacy of cisplatin and paclitaxel in a mouse ovarian cancer model (Campbell et al. 2010), and its activity was increased in combination with troglitazone, which up-regulates CD36 expression on endothelial cells (Huang et al. 2004). The TSRs of TSP-1 also increase the antiangiogenic activity of TRAIL to inhibit colon cancer in a mouse subcutaneous model (Ren et al. 2009). Thus, the TSRs may have important applications in combination cancer therapy. A small molecule mimetic of the FGF-2 binding site of TSP-1 is also in development as a potential inhibitor of angiogenesis (Margosio et al. 2008; Colombo et al. 2010).
TSP-5/COMP Oligomerization Domain
The TSP-5/COMP coiled-coil domain has been used to create engineered pentameric chimeras of bioactive molecules with enhanced stability and improved properties to activate or inhibit specific signaling pathways (Holler et al. 2000; Cho et al. 2004; Wang et al. 2008). Activation of nonphysiological receptors, such as Tie2 receptor by an engineered angiopoietin-2 pentamer, has also been achieved (Kim et al. 2009). The TSP-5/COMP pentamerizing coiled-coil has wide potential for development of high-affinity or stable ligands for clinical or bioengineering applications.
FUTURE DEVELOPMENTS
There are many areas of TSP biology that remain to be explored and translational areas that are expanding. Key questions and developing areas include:
The relationship of structure to function in the TSP carboxy-terminal region, with benefit of the universe of TSP sequences from invertebrates.
The mechanisms and roles of TSPs in collagen fibril organization.
The roles of TSPs in calcium homeostasis.
The cell biology of pentameric TSPs.
The functions of TSPs in invertebrates, especially within the ECMs of Cnidaria and sponges.
The conserved roles of TSPs in the ovary and their relevance to fertilization mechanisms.
The roles of TSPs in excitatory synaptogenesis, and their relevance to learning, memory, and pain perception throughout life.
The mechanisms and potential biological significance of bacterial adhesion to TSPs.
The feasibility and practicality of TSPs/TSP interactions as therapeutic targets, especially in cancer development and metastasis, cardiovascular disease, fibrosis, and ischemia.
The application of engineered TSP moieties in designed molecules or synthetic cellular environments.
ACKNOWLEDGMENTS
We thank Kemin Tan for modeling the vWF_C domain of TSP-1 and Elena Christofidou for assistance with tables and references. Research in J.C.A.’s laboratory is supported by the Wellcome Trust and British Heart Foundation. J.L.’s laboratory is supported by HL049081 and CA130895 from the National Institutes of Health.
REFERENCES
- Adams JC 2001. Thrombospondins: Multifunctional regulators of cell interactions. Annu Rev Cell Dev Biol 17: 25–51 [DOI] [PubMed] [Google Scholar]
- Adams JC 2004. Functions of the conserved thrombospondin carboxy-terminal cassette in cell-extracellular matrix interactions and signaling. Int J Biochem Cell Biol 36: 1102–1114 [DOI] [PubMed] [Google Scholar]
- Adams J, Lawler J 1993. Extracellular matrix: The thrombospondin family. Curr Biol 3: 188–190 [DOI] [PubMed] [Google Scholar]
- Adams JC, Tucker RP 2000. The thrombospondin type 1 repeat (TSR) superfamily: Diverse proteins with related roles in neuronal development. Dev Dyn 218: 280–299 [DOI] [PubMed] [Google Scholar]
- Adams JC, Clelland JD, Collett GD, Matsumura F, Yamashiro S, Zhang L 1999. Cell-matrix adhesions differentially regulate fascin phosphorylation. Mol Biol Cell 10: 4177–4190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams JC, Monk R, Taylor AL, Ozbek S, Fascetti N, Baumgartner S, Engel J 2003. Characterisation of Drosophila thrombospondin defines an early origin of pentameric thrombospondins. J Mol Biol 328: 479–494 [DOI] [PubMed] [Google Scholar]
- Adams JC, Bentley AA, Kvansakul M, Hatherley D, Hohenester E 2008. Extracellular matrix retention of thrombospondin 1 is controlled by its conserved C-terminal region. J Cell Sci 121: 784–795 [DOI] [PubMed] [Google Scholar]
- Adolph KW 1999. Relative abundance of thrombospondin 2 and thrombospondin 3 mRNAs in human tissues. Biochem Biophys Res Commun 258: 792–796 [DOI] [PubMed] [Google Scholar]
- Agah A, Kyriakides TR, Lawler J, Bornstein P 2002. The lack of thrombospondin-1 (TSP1) dictates the course of wound healing in double-TSP1/TSP2-null mice. Am J Pathol 161: 831–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agah A, Kyriakides TR, Bornstein P 2005. Proteolysis of cell-surface tissue transglutaminase by matrix metalloproteinase-2 contributes to the adhesive defect and matrix abnormalities in thrombospondin-2-null fibroblasts and mice. Am J Pathol 167: 81–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albo D, Berger DH, Tuszynski GP 1998. The effect of thrombospondin-1 and TGF-β 1 on pancreatic cancer cell invasion. J Surg Res 76: 86–90 [DOI] [PubMed] [Google Scholar]
- Alcorn JL, Merritt TM, Farach-Carson MC, Wang HH, Hecht JT 2009. Ribozyme-mediated reduction of wild-type and mutant cartilage oligomeric matrix protein (COMP) mRNA and protein. RNA 15: 686–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alford AI, Terkhorn SP, Reddy AB, Hankenson KD 2010. Thrombospondin-2 regulates matrix mineralization in MC3T3-E1 pre-osteoblasts. Bone 46: 464–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anilkumar N, Annis DS, Mosher DF, Adams JC 2002. Trimeric assembly of the C-terminal region of thrombospondin-1 or thrombospondin-2 is necessary for cell spreading and fascin spike organisation. J Cell Sci 115: 2357–2366 [DOI] [PubMed] [Google Scholar]
- Anilkumar N, Parsons M, Monk R, Ng T, Adams JC 2003. Interaction of fascin and protein kinase Cα: A novel intersection in cell adhesion and motility. EMBO J 22: 5390–5402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annis DS, Gunderson KA, Mosher DF 2007. Immunochemical analysis of the structure of the signature domains of thrombospondin-1 and thrombospondin-2 in low calcium concentrations. J Biol Chem 282: 27067–27075 [DOI] [PubMed] [Google Scholar]
- Arber S, Caroni P 1995. Thrombospondin-4, an extracellular matrix protein expressed in the developing and adult nervous system promotes neurite outgrowth. J Cell Biol 131: 1083–1094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asch AS, Silbiger S, Heimer E, Nachman RL 1992. Thrombospondin sequence motif (CSVTCG) is responsible for CD36 binding. Biochem Biophys Res Commun 182: 1208–1217 [DOI] [PubMed] [Google Scholar]
- Bale MD, Mosher DF 1986. Thrombospondin is a substrate for blood coagulation factor XIIIa. Biochemistry 25: 5667–5673 [DOI] [PubMed] [Google Scholar]
- Barros CS, Franco SJ, Müller U 2010. Extracellular matrix: Functions in the nervous system. Cold Spring Harb Perspect Biol 10.1101/cshperspect.a005108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bein K, Simons M 2000. Thrombospondin type 1 repeats interact with matrix metalloproteinase 2. Regulation of metalloproteinase activity. J Biol Chem 275: 32167–32173 [DOI] [PubMed] [Google Scholar]
- Bentley AA, Adams JC 2010. The evolution of thrombospondins and their ligand-binding activities. Mol Biol Evol 27: 2187–2197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair P, Flaumenhaft R 2009. Platelet α-granules: Basic biology and clinical correlates. Blood Rev 23: 177–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake SM, Strasser V, Andrade N, Duit S, Hofbauer R, Schneider WJ, Nimpf J 2008. Thrombospondin-1 binds to ApoER2 and VLDL receptor and functions in postnatal neuronal migration. EMBO J 27: 3069–3080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumbach K, Bastiaansen-Jenniskens YM, DeGroot J, Paulsson M, van Osch GJ, Zaucke F 2009. Combined role of type IX collagen and cartilage oligomeric matrix protein in cartilage matrix assembly: Cartilage oligomeric matrix protein counteracts type IX collagen-induced limitation of cartilage collagen fibril growth in mouse chondrocyte cultures. Arthritis Rheum 60: 3676–3685 [DOI] [PubMed] [Google Scholar]
- Bonnefoy A, Daenens K, Feys HB, De Vos R, Vandervoort P, Vermylen J, Lawler J, Hoylaerts MF 2006. Thrombospondin-1 controls vascular platelet recruitment and thrombus adherence in mice by protecting (sub)endothelial VWF from cleavage by ADAMTS13. Blood 107: 955–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein P, Agah A, Kyriakides TR 2004. The role of thrombospondins 1 and 2 in the regulation of cell-matrix interactions, collagen fibril formation, and the response to injury. Int J Biochem Cell Biol 36: 1115–1125 [DOI] [PubMed] [Google Scholar]
- Briggs MD, Chapman KL 2002. Pseudoachondroplasia and multiple epiphyseal dysplasia: Mutation review, molecular interactions, and genotype to phenotype correlations. Hum Mutat 19: 465–478 [DOI] [PubMed] [Google Scholar]
- Briggs MD, Hoffman SM, King LM, Olsen AS, Mohrenweiser H, Leroy JG, Mortier GR, Rimoin DL, Lachman RS, Gaines ES, et al. 1995. Pseudoachondroplasia and multiple epiphyseal dysplasia due to mutations in the cartilage oligomeric matrix protein gene. Nat Genet 10: 330–336 [DOI] [PubMed] [Google Scholar]
- Burke A, Creighton W, Tavora F, Li L, Fowler D 2010. Decreased frequency of the 3′UTR T>G single nucleotide polymorphism of thrombospondin-2 gene in sudden death due to plaque erosion. Cardiovasc Pathol 19: e45–e49 [DOI] [PubMed] [Google Scholar]
- Cáceres M, Suwyn C, Maddox M, Thomas JW, Preuss TM 2007. Increased cortical expression of two synaptogenic thrombospondins in human brain evolution. Cereb Cortex 17: 2312–2321 [DOI] [PubMed] [Google Scholar]
- Calzada MJ, Sipes JM, Krutzsch HC, Yurchenco PD, Annis DS, Mosher DF, Roberts DD 2003. Recognition of the N-terminal modules of thrombospondin-1 and thrombospondin-2 by a6b1 integrin. J Biol Chem 278: 40679–40687 [DOI] [PubMed] [Google Scholar]
- Calzada MJ, Zhou L, Sipes JM, Zhang J, Krutzsch HC, Iruela-Arispe ML, Annis DS, Mosher DF, Roberts DD 2004a. a4b1 integrin mediates selective endothelial cell responses to thrombospondins 1 and 2 in vitro and modulates angiogenesis in vivo. Circ Res 94: 462–470 [DOI] [PubMed] [Google Scholar]
- Calzada MJ, Annis DS, Zeng B, Marcinkiewicz C, Banas B, Lawler J, Mosher DF, Roberts DD 2004b. Identification of novel β1 integrin binding sites in the type 1 and type 2 repeats of thrombospondin-1. J Biol Chem 279: 41734–41743 [DOI] [PubMed] [Google Scholar]
- Campbell NE, Greenaway J, Henkin J, Moorehead RA, Petrik J 2010. The thrombospondin-1 mimetic ABT-510 increases the uptake and effectiveness of cisplatin and paclitaxel in a mouse model of epithelial ovarian cancer. Neoplasia 12: 275–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canfield AE, Sutton AB, Hoyland JA, Schor AM 1996. Association of thrombospondin-1 with osteogenic differentiation of retinal pericytes in vitro. J Cell Sci 109: 343–353 [DOI] [PubMed] [Google Scholar]
- Carlson CB, Bernstein DA, Annis DS, Misenheimer TM, Hannah BL, Mosher DF, Keck JL 2005. Structure of the calcium-rich signature domain of human thrombospondin-2. Nat Struct Mol Biol 12: 910–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson CB, Gunderson KA, Mosher DF 2008a. Mutations targeting intermodular interfaces or calcium binding destabilize the thrombospondin-2 signature domain. J Biol Chem 283: 27089–27099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson CB, Liu Y, Keck JL, Mosher DF 2008b. Influences of the N700S thrombospondin-1 polymorphism on protein structure and stability. J Biol Chem 283: 20069–20076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanana B, Graf R, Koledachkina T, Pflanz R, Vorbrüggen G 2007. αPS2 integrin-mediated muscle attachment in Drosophila requires the ECM protein thrombospondin. Mech Dev 124: 463–475 [DOI] [PubMed] [Google Scholar]
- Chen H, Strickland DK, Mosher DF 1996a. Metabolism of thrombospondin 2. Binding and degradation by 3t3 cells and glycosaminoglycan-variant Chinese hamster ovary cells. J Biol Chem 271: 15993–15999 [DOI] [PubMed] [Google Scholar]
- Chen H, Sottile J, Strickland DK, Mosher DF 1996b. Binding and degradation of thrombospondin-1 mediated through heparan sulphate proteoglycans and low-density-lipoprotein receptor-related protein: Localization of the functional activity to the trimeric N-terminal heparin-binding region of thrombospondin-1. Biochem J 318: 959–963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YW, Zhao P, Borup R, Hoffman EP 2000. Expression profiling in the muscular dystrophies: Identification of novel aspects of molecular pathophysiology. J Cell Biol 151: 1321–1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FH, Thomas AO, Hecht JT, Goldring MB, Lawler J 2005. Cartilage oligomeric matrix protein/thrombospondin 5 supports chondrocyte attachment through interaction with integrins. J Biol Chem 280: 32655–32661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FH, Herndon ME, Patel N, Hecht JT, Tuan RS, Lawler J 2007. Interaction of cartilage oligomeric matrix protein/thrombospondin 5 with aggrecan. J Biol Chem 282: 24591–24598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen TL, Posey KL, Hecht JT, Vertel BM 2008. COMP mutations: Domain-dependent relationship between abnormal chondrocyte trafficking and clinical PSACH and MED phenotypes. J Cell Biochem 103: 778–787 [DOI] [PubMed] [Google Scholar]
- Cho CH, Kammerer RA, Lee HJ, Steinmetz MO, Ryu YS, Lee SH, Yasunaga K, Kim KT, Kim I, Choi HH, et al. 2004. COMP-Ang1: A designed angiopoietin-1 variant with nonleaky angiogenic activity. Proc Natl Acad Sci 101: 5547–5552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopherson KS, Ullian EM, Stokes CC, Mullowney CE, Hell JW, Agah A, Lawler J, Mosher DF, Bornstein P, Barres BA 2005. Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell 120: 421–433 [DOI] [PubMed] [Google Scholar]
- Colombo G, Margosio B, Ragona L, Neves M, Bonifacio S, Annis DS, Stravalaci M, Tomaselli S, Giavazzi R, Rusnati M, et al. 2010. Non-peptidic thrombospondin-1 mimics as fibroblast growth factor-2 inhibitors: An integrated strategy for the development of new antiangiogenic compounds. J Biol Chem 285: 8733–8742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corless CL, Mendoza A, Collins T, Lawler J 1992. Colocalization of thrombospondin and syndecan during murine development. Dev Dyn 193: 346–358 [DOI] [PubMed] [Google Scholar]
- Crawford SE, Stellmach V, Murphy-Ullrich JE, Ribeiro SM, Lawler J, Hynes RO, Boivin GP, Bouck N 1998. Thrombospondin-1 is a major activator of TGF-β1 in vivo. Cell 93: 1159–1170 [DOI] [PubMed] [Google Scholar]
- Cursiefen C, Masli S, Ng TF, Dana MR, Bornstein P, Lawler J, Streilein JW 2004. Roles of thrombospondin-1 and -2 in regulating corneal and iris angiogenesis. Invest Ophthalmol Vis Sci 45: 1117–1124 [DOI] [PubMed] [Google Scholar]
- Daniel C, Schaub K, Amann K, Lawler J, Hugo C 2007a. Thrombospondin-1 is an endogenous activator of TGF-β in experimental diabetic nephropathy in vivo. Diabetes 56: 2982–2989 [DOI] [PubMed] [Google Scholar]
- Daniel C, Amann K, Hohenstein B, Bornstein P, Hugo C 2007b. Thrombospondin 2 functions as an endogenous regulator of angiogenesis and inflammation in experimental glomerulonephritis in mice. J Am Soc Nephrol 18: 788–798 [DOI] [PubMed] [Google Scholar]
- Dawson DW, Pearce SF, Zhong R, Silverstein RL, Frazier WA, Bouck NP 1997. CD36 mediates the in vitro inhibitory effects of thrombospondin-1 on endothelial cells. J Cell Biol 138: 707–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DW, Volpert OV, Pearce SF, Schneider AJ, Silverstein RL, Henkin J, Bouck NP 1999. Three distinct D-amino acid substitutions confer potent antiangiogenic activity on an inactive peptide derived from a thrombospondin-1 type 1 repeat. Mol Pharmacol 55: 332–338 [DOI] [PubMed] [Google Scholar]
- de la Fuente H, Lamana A, Mittelbrunn M, Perez-Gala S, Gonzalez S, García-Diez A, Vega M, Sanchez-Madrid F 2009. Identification of genes responsive to solar simulated UV radiation in human monocyte-derived dendritic cells. PLoS One 4: e6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiCesare PE, Mörgelin M, Mann K, Paulsson M 1994a. Cartilage oligomeric matrix protein and thrombospondin 1. Purification from articular cartilage, electron microscopic structure, and chondrocyte binding. Eur J Biochem 223: 927–937 [DOI] [PubMed] [Google Scholar]
- DiCesare P, Hauser N, Lehman D, Pasumarti S, Paulsson M 1994b. Cartilage oligomeric matrix protein (COMP) is an abundant component of tendon. FEBS Lett 354: 237–240 [DOI] [PubMed] [Google Scholar]
- DiCesare PE, Carlson CS, Stollerman ES, Chen FS, Leslie M, Perris R 1997. Expression of cartilage oligomeric matrix protein by human synovium. FEBS Lett 412: 249–252 [DOI] [PubMed] [Google Scholar]
- DiCesare PE, Chen FS, Moergelin M, Carlson CS, Leslie MP, Perris R, Fang C 2002. Matrix-matrix interaction of cartilage oligomeric matrix protein and fibronectin. Matrix Biol 21: 461–470 [DOI] [PubMed] [Google Scholar]
- Dickinson SC, Vankemmelbeke MN, Buttle DJ, Rosenberg K, Heinegård D, Hollander AP 2003. Cleavage of cartilage oligomeric matrix protein (thrombospondin-5) by matrix metalloproteinases and a disintegrin and metalloproteinase with thrombospondin motifs. Matrix Biol 22: 267–278 [DOI] [PubMed] [Google Scholar]
- Dixit VM, Grant GA, Santoro SA, Frazier WA 1984. Isolation and characterization of a heparin-binding domain from the amino terminus of platelet thrombospondin. J Biol Chem 259: 10100–10105 [PubMed] [Google Scholar]
- Dunkle ET, Zaucke F, Clegg DO 2007. Thrombospondin-4 and matrix three-dimensionality in axon outgrowth and adhesion in the developing retina. Exp Eye Res 84: 707–717 [DOI] [PubMed] [Google Scholar]
- Ebbinghaus S, Hussain M, Tannir N, Gordon M, Desai AA, Knight RA, Humerickhouse RA, Qian J, Gordon GB, Figlin R 2007. Phase 2 study of ABT-510 in patients with previously untreated advanced renal cell carcinoma. Clin Can Res 13: 6689–6695 [DOI] [PubMed] [Google Scholar]
- Eroglu C, Allen NJ, Susman MW, O’Rourke NA, Park CY, Ozkan E, Chakraborty C, Mulinyawe SB, Annis DS, Huberman AD, et al. 2009. Gabapentin receptor α2δ-1 is a neuronal thrombospondin receptor responsible for excitatory CNS synaptogenesis. Cell 139: 380–392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang C, Carlson CS, Leslie MP, Tulli H, Stolerman E, Perris R, Ni L, Di Cesare PE 2000. Molecular cloning, sequencing, and tissue and developmental expression of mouse cartilage oligomeric matrix protein (COMP). J Orthop Res 18: 593–603 [DOI] [PubMed] [Google Scholar]
- Fouladkou F, Lu C, Jiang C, Zhou L, She Y, Walls JR, Kawabe H, Brose N, Henkelman RM, Huang A, et al. 2010. The ubiquitin ligase Nedd4-1 is required for heart development and is a suppressor of thrombospondin-1. J Biol Chem 285: 6770–6780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frangogiannis NG, Ren G, Dewald O, Zymek P, Haudek S, Koerting A, Winkelmann K, Michael LH, Lawler J, Entman ML 2005. Critical role of endogenous thrombospondin-1 in preventing expansion of healing myocardial infarcts. Circulation 111: 2935–2942 [DOI] [PubMed] [Google Scholar]
- Franzen A, Heinegard D, Solursh M 1987. Evidence for sequential appearance of cartilage matrix proteins in developing mouse limbs and in cultures of mouse mesenchymal cells. Differentiation 36: 199–210 [DOI] [PubMed] [Google Scholar]
- Frieda S, Pearce A, Wu J, Silverstein RL 1995. Recombinant GST/CD36 fusion proteins define a thrombospondin binding domain. Evidence for a single calcium-dependent binding site on CD36. J Biol Chem 270: 2981–2986 [DOI] [PubMed] [Google Scholar]
- Frolova EG, Pluskota E, Krukovets I, Burke T, Drumm C, Smith JD, Blech L, Febbraio M, Bornstein P, Plow EF, et al. 2010. Thrombospondin-4 regulates vascular inflammation and atherogenesis. Circ Res 107: 1313–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa K, Roberts DD, Endo T, Kobata A 1989. Structural study of the sugar chains of human platelet thrombospondin. Arch Biochem Biophys 270: 302–312 [DOI] [PubMed] [Google Scholar]
- Galvin NJ, Vance PM, Dixit VM, Fink B, Frazier WA 1987. Interaction of human thrombospondin with types I-V collagen: Direct binding and electron microscopy. J Cell Biol 104: 1413–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gath U, Hakvoort A, Wegener J, Decker S, Galla HJ 1997. Porcine choroid plexus cells in culture: Expression of polarized phenotype, maintenance of barrier properties and apical secretion of CSF-components. Eur J Cell Biol 74: 68–78 [PubMed] [Google Scholar]
- Giannoni P, Siegrist M, Hunziker EB, Wong M 2003. The mechanosensitivity of cartilage oligomeric matrix protein (COMP). Biorheology 40: 101–109 [PubMed] [Google Scholar]
- Gilsohn E, Volk T 2010. Slowdown promotes muscle integrity by modulating integrin-mediated adhesion at the myotendinous junction. Development 137: 785–794 [DOI] [PubMed] [Google Scholar]
- Godyna S, Liau G, Popa I, Stefansson S, Argraves WS 1995. Identification of the low density lipoprotein receptor-related protein (LRP) as an endocytic receptor for thrombospondin-1. J Cell Biol 129: 1403–1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goicoechea S, Orr AW, Pallero MA, Eggleton P, Murphy-Ullrich JE 2000. Thrombospondin mediates focal adhesion disassembly through interactions with cell surface calreticulin. J Biol Chem 275: 36358–36368 [DOI] [PubMed] [Google Scholar]
- Greenaway J, Gentry PA, Feige JJ, LaMarre J, Petrik JJ 2005. Thrombospondin and vascular endothelial growth factor are cyclically expressed in an inverse pattern during bovine ovarian follicle development. Biol Reprod 72: 1071–1078 [DOI] [PubMed] [Google Scholar]
- Greenaway J, Lawler J, Moorehead R, Bornstein P, Lamarre J, Petrik J 2007. Thrombospondin-1 inhibits VEGF levels in the ovary directly by binding and internalization via the low density lipoprotein receptor-related protein-1 (LRP-1). J Cell Physiol 210: 807–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood JA, Theibert AB, Prestwich GD, Murphy-Ullrich JE 2000. Restructuring of focal adhesion plaques by PI 3-kinase. Regulation by PtdIns (3,4,5)-p(3) binding to α-actinin. J Cell Biol 150: 627–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber HE, Bornstein P, Sage EH, Ingram JA, Zinchenko N, Norton HJ, Hanley EN Jr 2008. Disruption of the thrombospondin-2 gene alters the lamellar morphology but does not permit vascularization of the adult mouse lumbar disc. Arthritis Res Ther 10: R96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunasekar SK, Asnani M, Limbad C, Haghpanah JS, Hom W, Barra H, Nanda S, Lu M, Montclare JK 2009. N-terminal aliphatic residues dictate the structure, stability, assembly, and small molecule binding of the coiled-coil region of cartilage oligomeric matrix protein. Biochemistry 48: 8559–8567 [DOI] [PubMed] [Google Scholar]
- Guo NH, Krutzsch HC, Nègre E, Vogel T, Blake DA, Roberts DD 1992. Heparin- and sulfatide-binding peptides from the type I repeats of human thrombospondin promote melanoma cell adhesion. Proc Natl Acad Sci 89: 3040–3044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez LS, Suckow M, Lawler J, Ploplis VA, Castellino FJ 2003. Thrombospondin 1–a regulator of adenoma growth and carcinoma progression in the APCMin/+ mouse model. Carcinogenesis 24: 199–207 [DOI] [PubMed] [Google Scholar]
- Halász K, Kassner A, Mörgelin M, Heinegård D 2007. COMP acts as a catalyst in collagen fibrillogenesis. J Biol Chem 282: 31166–31173 [DOI] [PubMed] [Google Scholar]
- Hankenson KD, Bain SD, Kyriakides TR, Smith EA, Goldstein SA, Bornstein P 2000. Increased marrow-derived osteoprogenitor cells and endosteal bone formation in mice lacking thrombospondin 2. J Bone Miner Res 15: 851–862 [DOI] [PubMed] [Google Scholar]
- Hankenson KD, James IE, Apone S, Stroup GB, Blake SM, Liang X, Lark MW, Bornstein P 2005a. Increased osteoblastogenesis and decreased bone resorption protect against ovariectomy-induced bone loss in thrombospondin-2-null mice. Matrix Biol 24: 362–370 [DOI] [PubMed] [Google Scholar]
- Hankenson KD, Hormuzdi SG, Meganck JA, Bornstein P 2005b. Mice with a disruption of the thrombospondin 3 gene differ in geometric and biomechanical properties of bone and have accelerated development of the femoral head. Mol Cell Biol 25: 5599–5606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankenson KD, Ausk BJ, Bain SD, Bornstein P, Gross TS, Srinivasan S 2006. Mice lacking thrombospondin 2 show an atypical pattern of endocortical and periosteal bone formation in response to mechanical loading. Bone 38: 310–316 [DOI] [PubMed] [Google Scholar]
- Hankenson KD, Sweetwyne MT, Shitaye H, Posey KL 2010. Thrombospondins and novel TSR-containing proteins, R-spondins, regulate bone formation and remodeling. Curr Osteoporos Rep 8: 68–76 [DOI] [PubMed] [Google Scholar]
- Hansen U, Platz N, Becker A, Bruckner P, Paulsson M, Zaucke F 2011. A secreted variant of cartilage oligomeric matrix protein carrying a chondrodysplasia-causing mutation (p.H587R) disrupts collagen fibrillogenesis. Arthritis Rheum 63: 159–167 [DOI] [PubMed] [Google Scholar]
- Hauser N, Paulsson M, Kale AA, DiCesare PE 1995. Tendon extracellular matrix contains pentameric thrombospondin-4 (TSP-4). FEBS Lett 368: 307–310 [DOI] [PubMed] [Google Scholar]
- Hawighorst T, Velasco P, Streit M, Hong YK, Kyriakides TR, Brown LF, Bornstein P, Detmar M 2001. Thrombospondin-2 plays a protective role in multistep carcinogenesis: A novel host anti-tumor defense mechanism. EMBO J 20: 2631–2640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht JT, Nelson LD, Crowder E, Wang Y, Elder FF, Harrison WR, Francomano CA, Prange CK, Lennon GG, Deere M, et al. 1995. Mutations in exon 17B of cartilage oligomeric matrix protein (COMP) cause pseudoachondroplasia. Nat Genet 10: 325–329 [DOI] [PubMed] [Google Scholar]
- Hecht JT, Deere M, Putnam E, Cole W, Vertel B, Chen H, Lawler J 1998. Characterization of cartilage oligomeric matrix protein (COMP) in human normal and pseudoachondroplasia musculoskeletal tissues. Matrix Biol 17: 269–278 [DOI] [PubMed] [Google Scholar]
- Hecht JT, Hayes E, Snuggs M, Decker G, Montufar-Solis D, Doege K, Mwalle F, Poole R, Stevens J, Duke PJ 2001. Calreticulin, PDI, Grp94 and BiP chaperone proteins are associated with retained COMP in pseudoachondroplasia chondrocytes. Matrix Biol 20: 251–262 [DOI] [PubMed] [Google Scholar]
- Hess D, Keusch JJ, Oberstein SA, Hennekam RC, Hofsteenge J 2008. Peters Plus syndrome is a new congenital disorder of glycosylation and involves defective O-glycosylation of thrombospondin type 1 repeats. J Biol Chem 283: 7354–7360 [DOI] [PubMed] [Google Scholar]
- Hirose Y, Chiba K, Karasugi T, Nakajima M, Kawaguchi Y, Mikami Y, Furuichi T, Mio F, Miyake A, Miyamoto T, et al. 2008. A functional polymorphism in THBS2 that affects alternative splicing and MMP binding is associated with lumbar-disc herniation. Am J Hum Genet 82: 1122–1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiscott P, Sorokin L, Schlötzer-Schrehardt U, Blüthner K, Endress K, Mayer U 1996. Expression of thrombospondin 1 by adult lens epithelium. Exp Eye Res 62: 709–712 [DOI] [PubMed] [Google Scholar]
- Hiscott P, Seitz B, Schlötzer-Schrehardt U, Naumann GO 1997. Immunolocalisation of thrombospondin 1 in human, bovine and rabbit cornea. Cell Tissue Res 289: 307–310 [DOI] [PubMed] [Google Scholar]
- Hochegger K, Knight S, Hugo C, Mayer G, Lawler J, Mayadas TN, Rosenkranz AR 2004. Role of thrombospondin-1 in the autologous phase of an accelerated model of anti-glomerular basement membrane glomerulonephritis. Nephron Exp Nephrol 96: e31–e38 [DOI] [PubMed] [Google Scholar]
- Hoffman JR, Dixit VM, O’Shea KS 1994. Expression of thrombospondin in the adult nervous system. J Comp Neurol 340: 126–139 [DOI] [PubMed] [Google Scholar]
- Hofsteenge J, Huwiler KG, Macek B, Hess D, Lawler J, Mosher DF, Peter-Katalinic J 2001. C-mannosylation and O-fucosylation of the thrombospondin type 1 module. J Biol Chem 276: 6485–6498 [DOI] [PubMed] [Google Scholar]
- Hogg PJ, Owensby DA, Mosher DF, Misenheimer TM, Chesterman CN 1993. Thrombospondin is a tight-binding competitive inhibitor of neutrophil elastase. J Biol Chem 268: 7139–7146 [PubMed] [Google Scholar]
- Holden P, Meadows RS, Chapman KL, Grant ME, Kadler KE, Briggs MD 2001. Cartilage oligomeric matrix protein interacts with type IX collagen, and disruptions to these interactions identify a pathogenetic mechanism in a bone dysplasia family. J Biol Chem 276: 6046–6055 [DOI] [PubMed] [Google Scholar]
- Holler N, Kataoka T, Bodmer JL, Romero P, Romero J, Deperthes D, Engel J, Tschopp J, Schneider P 2000. Development of improved soluble inhibitors of FasL and CD40L based on oligomerized receptors. J Immunol Methods 237: 159–173 [DOI] [PubMed] [Google Scholar]
- Howell BG, Wang B, Freed I, Mamelak AJ, Watanabe H, Sauder DN 2004. Microarray analysis of UVB-regulated genes in keratinocytes: downregulation of angiogenesis inhibitor thrombospondin-1. J Dermatol Sci 34: 185–194 [DOI] [PubMed] [Google Scholar]
- Huang H, Campbell SC, Bedford DF, Nelius T, Veliceasa D, Shroff EH, Henkin J, Schneider A, Bouck N, Volpert OV 2004. Peroxisome proliferator-activated receptor γ ligands improve the antitumor efficacy of thrombospondin peptide ABT510. Mol Cancer Res 2: 541–550 [PubMed] [Google Scholar]
- Hughes EG, Elmariah SB, Balice-Gordon RJ 2010. Astrocyte secreted proteins selectively increase hippocampal GABAergic axon length, branching, and synaptogenesis. Mol Cell Neurosci 43: 136–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iruela-Arispe ML, Liska DJ, Sage EH, Bornstein P 1993. Differential expression of thrombospondin 1, 2, and 3 during murine development. Dev Dyn 197: 40–56 [DOI] [PubMed] [Google Scholar]
- Iruela-Arispe ML, Lombardo M, Krutzsch HC, Lawler J, Roberts DD 1999. Inhibition of angiogenesis by thrombospondin-1 is mediated by 2 independent regions within the type 1 repeats. Circulation 100: 1423–1431 [DOI] [PubMed] [Google Scholar]
- Isenberg JS, Ridnour LA, Perruccio EM, Espey MG, Wink DA, Roberts DD 2005. Thrombospondin-1 inhibits endothelial cell responses to nitric oxide in a cGMP-dependent manner. Proc Natl Acad Sci 102: 13141–13146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JS, Wink DA, Roberts DD 2006a. Thrombospondin-1 antagonizes nitric oxide-stimulated vascular smooth muscle cell responses. Cardiovasc Res 71: 785–793 [DOI] [PubMed] [Google Scholar]
- Isenberg JS, Ridnour LA, Dimitry J, Frazier WA, Wink DA, Roberts DD 2006b. CD47 is necessary for inhibition of nitric oxide-stimulated vascular cell responses by thrombospondin-1. J Biol Chem 281: 26069–26080 [DOI] [PubMed] [Google Scholar]
- Isenberg JS, Jia Y, Fukuyama J, Switzer CH, Wink DA, Roberts DD 2007a. Thrombospondin-1 inhibits nitric oxide signaling via CD36 by inhibiting myristic acid uptake. J Biol Chem 282: 15404–15415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JS, Hyodo F, Matsumoto K, Romeo MJ, Abu-Asab M, Tsokos M, Kuppusamy P, Wink DA, Krishna MC, Roberts DD 2007b. Thrombospondin-1 limits ischemic tissue survival by inhibiting nitric oxide-mediated vascular smooth muscle relaxation. Blood 109: 1945–1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JS, Hyodo F, Pappan LK, Abu-Asab M, Tsokos M, Krishna MC, Frazier WA, Roberts DD 2007c. Blocking thrombospondin-1/CD47 signaling alleviates deleterious effects of aging on tissue responses to ischemia. Arterioscler Thromb Vasc Biol 27: 2582–2588 [DOI] [PubMed] [Google Scholar]
- Isenberg JS, Romeo MJ, Yu C, Yu CK, Nghiem K, Monsale J, Rick ME, Wink DA, Frazier WA, Roberts DD 2008a. Thrombospondin-1 stimulates platelet aggregation by blocking the antithrombotic activity of nitric oxide/cGMP signaling. Blood 111: 613–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JS, Maxhimer JB, Hyodo F, Pendrak ML, Ridnour LA, DeGraff WG, Tsokos M, Wink DA, Roberts DD 2008b. Thrombospondin-1 and CD47 limit cell and tissue survival of radiation injury. Am J Pathol 173: 1100–1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg JS, Martin-Manso G, Maxhimer JB, Roberts DD 2009. Regulation of nitric oxide signalling by thrombospondin 1: Implications for anti-angiogenic therapies. Nat Rev Cancer 9: 182–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe EA, Ruggiero JT, Leung LK, Doyle MJ, McKeown-Longo PJ, Mosher DF 1983. Cultured human fibroblasts synthesize and secrete thrombospondin and incorporate it into extracellular matrix. Proc Natl Acad Sci 80: 998–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez B, Volpert OV, Crawford V, Febbraio M, Silverstein R, Bouck N 2000. Signals leading to apoptosis-dependent inhibition of neovascularization by thrombospondin-1. Nat Med 6: 41–48 [DOI] [PubMed] [Google Scholar]
- Jiménez B, Volpert OV, Reiher F, Chang L, Muñoz A, Karin M, Bouck N 2001. c-Jun N-terminal kinase activation is required for the inhibition of neovascularization by thrombospondin-1. Oncogene 20: 3443–3448 [DOI] [PubMed] [Google Scholar]
- Kalas W, Yu JL, Milsom C, Rosenfeld J, Benezra R, Bornstein P, Rak J 2005. Oncogenes and angiogenesis: Down-regulation of thrombospondin-1 in normal fibroblasts exposed to factors from cancer cells harboring mutant ras. Cancer Res 65: 8878–8886 [DOI] [PubMed] [Google Scholar]
- Kang SY, Halvorsen OJ, Gravdal K, Bhattacharya N, Lee JM, Liu NW, Johnston BT, Johnston AB, Haukaas SA, Aamodt K, et al. 2009. Prosaposin inhibits tumor metastasis via paracrine and endocrine stimulation of stromal pp53 and Tsp-1. Proc Natl Acad Sci 106: 12115–12120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketis NV, Lawler J, Hoover RL, Karnovsky MJ 1988. Effects of heat shock on the expression of thrombospondin by endothelial cells in culture. J Cell Biol 106: 893–904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HZ, Jung K, Kim HM, Cheng Y, Koh GY 2009. A designed angiopoietin-2 variant, pentameric COMP-Ang2, strongly activates Tie2 receptor and stimulates angiogenesis. Biochim Biophys Acta 1793: 772–780 [DOI] [PubMed] [Google Scholar]
- Kipnes JR, Xu L, Han F, Rallapalli R, Jimenez S, Hall DJ, Tuan RS, Li Y 2000. Molecular cloning and expression patterns of mouse cartilage oligomeric matrix protein gene. Osteoarthritis Cartilage 8: 236–239 [DOI] [PubMed] [Google Scholar]
- Koch W, Hoppmann P, de Waha A, Schömig A, Kastrati A 2008. Polymorphisms in thrombospondin genes and myocardial infarction: A case-control study and a meta-analysis of available evidence. Hum Mol Genet 17: 1120–1126 [DOI] [PubMed] [Google Scholar]
- Kopp HG, Hooper AT, Broekman MJ, Avecilla ST, Petit I, Luo M, Milde T, Ramos CA, Zhang F, Kopp T, et al. 2006. Thrombospondins deployed by thrombopoietic cells determine angiogenic switch and extent of revascularization. J Clin Invest 116: 3277–3291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozma K, Keusch JJ, Hegemann B, Luther KB, Klein D, Hess D, Haltiwanger RS, Hofsteenge J 2006. Identification and characterization of a β1,3-glucosyltransferase that synthesizes the Glc-β1,3-Fuc disaccharide on thrombospondin type 1 repeats. J Biol Chem 281: 36742–36751 [DOI] [PubMed] [Google Scholar]
- Krutzsch HC, Choe BJ, Sipes JM, Guo N, Roberts DD 1999. Identification of an a(3)b(1) integrin recognition sequence in thrombospondin-1. J Biol Chem 274: 24080–24086 [DOI] [PubMed] [Google Scholar]
- Kuznetsov G, Chen LB, Nigam SK 1997. Multiple molecular chaperones complex with misfolded large oligomeric glycoproteins in the endoplasmic reticulum. J Biol Chem 272: 3057–3063 [DOI] [PubMed] [Google Scholar]
- Kuznetsova SA, Issa P, Perruccio EM, Zeng B, Sipes JM, Ward Y, Seyfried NT, Fielder HL, Day AJ, Wight TN, et al. 2006. Versican-thrombospondin-1 binding in vitro and colocalization in microfibrils induced by inflammation on vascular smooth muscle cells. J Cell Sci 119: 4499–4509 [DOI] [PubMed] [Google Scholar]
- Kvansakul M, Adams JC, Hohenester E 2004. Structure of a thrombospondin C-terminal fragment reveals a novel calcium core in the type 3 repeats. EMBO J 23: 1223–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriakides TR, Zhu YH, Yang Z, Bornstein P 1998a. The distribution of the matricellular protein thrombospondin 2 in tissues of embryonic and adult mice. J Histochem Cytochem 46: 1007–1015 [DOI] [PubMed] [Google Scholar]
- Kyriakides TR, Zhu YH, Smith LT, Bain SD, Yang Z, Lin MT, Danielson KG, Iozzo RV, LaMarca M, McKinney CE, et al. 1998b. Mice that lack thrombospondin 2 display connective tissue abnormalities that are associated with disordered collagen fibrillogenesis, an increased vascular density, and a bleeding diathesis. J Cell Biol 140: 419–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriakides TR, Tam JW, Bornstein P 1999a. Accelerated wound healing in mice with a disruption of the thrombospondin 2 gene. J Invest Dermatol 113: 782–787 [DOI] [PubMed] [Google Scholar]
- Kyriakides TR, Leach KJ, Hoffman AS, Ratner BD, Bornstein P 1999b. Mice that lack the angiogenesis inhibitor, thrombospondin 2, mount an altered foreign body reaction characterized by increased vascularity. Proc Natl Acad Sci 96: 4449–4454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriakides TR, Rojnuckarin P, Reidy MA, Hankenson KD, Papayannopoulou T, Kaushansky K, Bornstein P 2003. Megakaryocytes require thrombospondin-2 for normal platelet formation and function. Blood 101: 3915–3923 [DOI] [PubMed] [Google Scholar]
- Laherty CD, O’Rourke K, Wolf FW, Katz R, Seldin MF, Dixit VM 1992. Characterization of mouse thrombospondin 2 sequence and expression during cell growth and development. J Biol Chem 267: 3274–3281 [PubMed] [Google Scholar]
- Lange-Asschenfeldt B, Weninger W, Velasco P, Kyriakides TR, von Andrian UH, Bornstein P, Detmar M 2002. Increased and prolonged inflammation and angiogenesis in delayed-type hypersensitivity reactions elicited in the skin of thrombospondin-2–deficient mice. Blood 99: 538–545 [DOI] [PubMed] [Google Scholar]
- Lawler J, Hynes RO 1989. An integrin receptor on normal and thrombasthenic platelets that binds thrombospondin. Blood 74: 2022–2027 [PubMed] [Google Scholar]
- Lawler JW, Slayter HS 1981. The release of heparin binding peptides from platelet thrombospondin by proteolytic action of thrombin, plasmin and trypsin. Thromb Res 22: 267–279 [DOI] [PubMed] [Google Scholar]
- Lawler J, Derick LH, Connolly JE, Chen JH, Chao FC 1985. The structure of human platelet thrombospondin. J Biol Chem 260: 3762–3772 [PubMed] [Google Scholar]
- Lawler J, Weinstein R, Hynes RO 1988. Cell attachment to thrombospondin: The role of ARG-GLY-ASP, calcium, and integrin receptors. J Cell Biol 107: 2351–2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler J, Ferro P, Duquette M 1992. Expression and mutagenesis of thrombospondin. Biochemistry 31: 1173–1180 [DOI] [PubMed] [Google Scholar]
- Lawler J, Duquette M, Whittaker CA, Adams JC, McHenry K, DeSimone DW 1993. Identification and characterization of thrombospondin-4, a new member of the thrombospondin gene family. J Cell Biol 120: 1059–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler J, McHenry K, Duquette M, Derick L 1995. Characterization of human thrombospondin-4. J Biol Chem 270: 2809–2814 [DOI] [PubMed] [Google Scholar]
- Lawler J, Sunday M, Thibert V, Duquette M, George EL, Rayburn H, Hynes RO 1998. Thrombospondin-1 is required for normal murine pulmonary homeostasis and its absence causes pneumonia. J Clin Invest 101: 982–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler J, Miao WM, Duquette M, Bouck N, Bronson RT, Hynes RO 2001. Thrombospondin-1 gene expression affects survival and tumor spectrum of p53-deficient mice. Am J Pathol 159: 1949–1956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee NV, Sato M, Annis DS, Loo JA, Wu L, Mosher DF, Iruela-Arispe ML 2006. ADAMTS1 mediates the release of antiangiogenic polypeptides from TSP1 and 2. EMBO J 25: 5270–5283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liauw J, Hoang S, Choi M, Eroglu C, Choi M, Sun GH, Percy M, Wildman-Tobriner B, Bliss T, Guzman RG, et al. 2008. Thrombospondins 1 and 2 are necessary for synaptic plasticity and functional recovery after stroke. J Cereb Blood Flow Metab 28: 1722–1732 [DOI] [PubMed] [Google Scholar]
- Liu CJ, Kong W, Xu K, Luan Y, Ilalov K, Sehgal B, Yu S, Howell RD, Di Cesare PE 2006a. ADAMTS-12 associates with and degrades cartilage oligomeric matrix protein. J Biol Chem 281: 15800–15808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CJ, Kong W, Ilalov K, Yu S, Xu K, Prazak L, Fajardo M, Sehgal B, Di Cesare PE 2006b. ADAMTS-7: A metalloproteinase that directly binds to and degrades cartilage oligomeric matrix protein. FASEB J 20: 988–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu A, Garg P, Yang S, Gong P, Pallero MA, Annis DS, Liu Y, Passaniti A, Mann D, Mosher DF, et al. 2009. Epidermal growth factor-like repeats of thrombospondins activate phospholipase Cγ and increase epithelial cell migration through indirect epidermal growth factor receptor activation. J Biol Chem 284: 6389–6402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Koles K, Vorndam W, Haltiwanger RS, Panin VM 2006. Protein O-fucosyltransferase 2 adds O-fucose to thrombospondin type 1 repeats. J Biol Chem 281: 9393–9399 [DOI] [PubMed] [Google Scholar]
- Lymn JS, Patel MK, Clunn GF, Rao SJ, Gallagher KL, Hughes AD 2002. Thrombospondin-1 differentially induces chemotaxis and DNA synthesis of human venous smooth muscle cells at the receptor-binding level. J Cell Sci 115: 4353–4360 [DOI] [PubMed] [Google Scholar]
- Maclauchlan S, Skokos EA, Agah A, Zeng J, Tian W, Davidson JM, Bornstein P, Kyriakides TR 2009. Enhanced angiogenesis and reduced contraction in thrombospondin-2-null wounds is associated with increased levels of matrix metalloproteinases-2 and -9, and soluble VEGF. J Histochem Cytochem 57: 301–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majack RA, Cook SC, Bornstein P 1985. Platelet-derived growth factor and heparin-like glycosaminoglycans regulate thrombospondin synthesis and deposition in the matrix by smooth muscle cells. J Cell Biol 101: 1059–1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majack RA, Cook SC, Bornstein P 1986. Control of smooth muscle cell growth by components of the extracellular matrix: Autocrine role for thrombospondin. Proc Natl Acad Sci 83: 9050–9054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malek MH, Olfert IM 2009. Global deletion of thrombospondin-1 increases cardiac and skeletal muscle capillarity and exercise capacity in mice. Exp Physiol 94: 749–760 [DOI] [PubMed] [Google Scholar]
- Mann HH, Ozbek S, Engel J, Paulsson M, Wagener R 2004. Interactions between the cartilage oligomeric matrix protein and matrilins. Implications for matrix assembly and the pathogenesis of chondrodysplasias. J Biol Chem 279: 25294–25298 [DOI] [PubMed] [Google Scholar]
- Margosio B, Rusnati M, Bonezzi K, Cordes BL, Annis DS, Urbinati C, Giavazzi R, Presta M, Ribatti D, Mosher DF, et al. 2008. Fibroblast growth factor-2 binding to the thrombospondin-1 type III repeats, a novel antiangiogenic domain. Int J Biochem Cell Bio 40: 700–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markovic SN, Suman VJ, Rao RA, Ingle JN, Kaur JS, Erickson LA, Pitot HC, Croghan GA, McWilliams RR, Merchan J, et al. 2007. A phase II study of ABT-510 (thrombospondin-1 analog) for the treatment of metastatic melanoma. Am J Clin Oncol 30: 303–309 [DOI] [PubMed] [Google Scholar]
- Marteau F, Gonzalez NS, Communi D, Goldman M, Boeynaems JM, Communi D 2005. Thrombospondin-1 and indoleamine 2,3-dioxygenase are major targets of extracellular ATP in human dendritic cells. Blood 106: 3860–3866 [DOI] [PubMed] [Google Scholar]
- Martin-Manso G, Galli S, Ridnour LA, Tsokos M, Wink DA, Roberts DD 2008. Thrombospondin 1 promotes tumor macrophage recruitment and enhances tumor cell cytotoxicity of differentiated U937 cells. Cancer Res 68: 7090–7099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie P, Chadalavada SC, Bohrer J, Adams JC 2006. Phylogenomic analysis of vertebrate thrombospondins reveals fish-specific paralogues, ancestral gene relationships and a tetrapod innovation. BMC Evol Biol 6: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeown-Longo PJ, Hanning R, Mosher DF 1984. Binding and degradation of platelet thrombospondin by cultured fibroblasts. J Cell Biol 98: 22–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meek RL, Cooney SK, Flynn SD, Chouinard RF, Poczatek MH, Murphy-Ullrich JE, Tuttle KR 2003. Amino acids induce indicators of response to injury in glomerular mesangial cells. Am J Physiol Renal Physiol 285: F79–F86 [DOI] [PubMed] [Google Scholar]
- Meng H, Zhang X, Hankenson KD, Wang MM 2009. Thrombospondin 2 potentiates notch3/jagged1 signaling. J Biol Chem 284: 7866–7874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng H, Zhang X, Lee SJ, Strickland DK, Lawrence DA, Wang MM 2010. LDL-receptor related protein (LRP1) regulates Thrombospondin-2 (TSP2) enhancement of Notch3 signaling. J Biol Chem 285:23047–23055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merle B, Malaval L, Lawler J, Delmas P, Clezardin P 1997. Decorin inhibits cell attachment to thrombospondin-1 by binding to a KKTR-dependent cell adhesive site present within the N-terminal domain of thrombospondin-1. J Cell Biochem 67: 75–83 [PubMed] [Google Scholar]
- Merritt TM, Bick R, Poindexter BJ, Alcorn JL, Hecht JT 2007. Unique matrix structure in the rough endoplasmic reticulum cisternae of pseudoachondroplasia chondrocytes. Am J Pathol 170: 293–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao WM, Seng WL, Duquette M, Lawler P, Laus C, Lawler J 2001. Thrombospondin-1 type 1 repeat recombinant proteins inhibit tumor growth through transforming growth factor-β-dependent and -independent mechanisms. Cancer Res 61: 7830–7839 [PubMed] [Google Scholar]
- Mikhailenko I, Kounnas MZ, Strickland DK 1995. Low density lipoprotein receptor-related protein/α 2-macroglobulin receptor mediates the cellular internalization and degradation of thrombospondin. A process facilitated by cell-surface proteoglycans. J Biol Chem 270: 9543–9549 [DOI] [PubMed] [Google Scholar]
- Mikhailenko I, Krylov D, Argraves KM, Roberts DD, Liau G, Strickland DK 1997. Cellular internalization and degradation of thrombospondin-1 is mediated by the amino-terminal heparin binding domain (HBD). High affinity interaction of dimeric HBD with the low density lipoprotein receptor-related protein. J Biol Chem 272: 6784–6791 [DOI] [PubMed] [Google Scholar]
- Möller JC, Klein MA, Haas S, Jones LL, Kreutzberg GW, Raivich G 1996. Regulation of thrombospondin in the regenerating mouse facial motor nucleus. Glia 17: 121–132 [DOI] [PubMed] [Google Scholar]
- Mörgelin M, Heinegård D, Engel J, Paulsson M 1992. Electron microscopy of native cartilage oligomeric matrix protein purified from the Swarm rat chondrosarcoma reveals a five-armed structure. J Biol Chem 267: 6137–6141 [PubMed] [Google Scholar]
- Motegi K, Harada K, Ohe G, Jones SJ, Ellis IR, Crouch DH, Schor SL, Schor AM 2008. Differential involvement of TGF-β1 in mediating the motogenic effects of TSP-1 on endothelial cells, fibroblasts and oral tumour cells. Exp Cell Res 314: 2323–2333 [DOI] [PubMed] [Google Scholar]
- Moura R, Tjwa M, Vandervoort P, Cludts K, Hoylaerts MF 2007. Thrombospondin-1 activates medial smooth muscle cells and triggers neointima formation upon mouse carotid artery ligation. Arterioscler Thromb Vasc Biol 27: 2163–2169 [DOI] [PubMed] [Google Scholar]
- Moura R, Tjwa M, Vandervoort P, Van Kerckhoven S, Holvoet P, Hoylaerts MF 2008. Thrombospondin-1 deficiency accelerates atherosclerotic plaque maturation in ApoE–/– mice. Circ Res 103: 1181–1189 [DOI] [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Mosher DF 1985. Localization of thrombospondin in clots formed in situ. Blood 66: 1098–1104 [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Mosher DF 1987a. Interactions of thrombospondin with endothelial cells: Receptor-mediated binding and degradation. J Cell Biol 105: 1603–1611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Mosher DF 1987b. Interactions of thrombospondin with cells in culture: Rapid degradation of both soluble and matrix thrombospondin. Semin Thromb Hemost 13: 343–351 [DOI] [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Westrick LG, Esko JD, Mosher DF 1988. Altered metabolism of thrombospondin by Chinese hamster ovary cells defective in glycosaminoglycan synthesis. J Biol Chem 263: 6400–6406 [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Gurusiddappa S, Frazier WA, Hook M 1993. Heparin-binding peptides from thrombospondins 1 and 2 contain focal adhesion-labilizing activity. J Biol Chem 268: 26784–26789 [PubMed] [Google Scholar]
- Murphy-Ullrich JE, Pallero MA, Boerth N, Greenwood JA, Lincoln TM, Cornwell TL 1996. Cyclic GMP-dependent protein kinase is required for thrombospondin and tenascin mediated focal adhesion disassembly. J Cell Sci 109: 2499–2508 [DOI] [PubMed] [Google Scholar]
- Mustonen E, Aro J, Puhakka J, Ilves M, Soini Y, Leskinen H, Ruskoaho H, Rysä J 2008. Thrombospondin-4 expression is rapidly upregulated by cardiac overload. Biochem Biophys Res Commun 373: 186–191 [DOI] [PubMed] [Google Scholar]
- Narizhneva NV, Byers-Ward VJ, Quinn MJ, Zidar FJ, Plow EF, Topol EJ, Byzova TV 2004. Molecular and functional differences induced in thrombospondin-1 by the single nucleotide polymorphism associated with the risk of premature, familial myocardial infarction. J Biol Chem 279: 21651–21657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narouz-Ott L, Maurer P, Nitsche DP, Smyth N, Paulsson M 2000. Thrombospondin-4 binds specifically to both collagenous and non-collagenous extracellular matrix proteins via its C-terminal domains. J Biol Chem 275: 37110–37117 [DOI] [PubMed] [Google Scholar]
- Neidhart M, Hauser N, Paulsson M, DiCesare PE, Michel BA, Häuselmann HJ 1997. Small fragments of cartilage oligomeric matrix protein in synovial fluid and serum as markers for cartilage degradation. Br J Rheumatol 36: 1151–1160 [DOI] [PubMed] [Google Scholar]
- Newton G, Weremowicz S, Morton CC, Copeland NG, Gilbert DJ, Jenkins NA, Lawler J 1994. Characterization of human and mouse cartilage oligomeric matrix protein. Genomics 24: 435–439 [DOI] [PubMed] [Google Scholar]
- Nishimura H, Yamashita S, Zeng Z, Walz DA, Iwanaga S 1992. Evidence for the existence of O-linked sugar chains consisting of glucose and xylose in bovine thrombospondin. J Biochem 111: 460–464 [DOI] [PubMed] [Google Scholar]
- Nucera C, Porrello A, Antonello ZA, Mekel M, Nehs MA, Giordano TJ, Gerald D, Benjamin LE, Priolo C, Puxeddu E, et al. 2010. B-Raf(V600E) and thrombospondin-1 promote thyroid cancer progression. Proc Natl Acad Sci 107: 10649–10654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oganesian A, Armstrong LC, Migliorini MM, Strickland DK, Bornstein P 2008. Thrombospondins use the VLDL receptor and a nonapoptotic pathway to inhibit cell division in microvascular endothelial cells. Mol Biol Cell 19: 563–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary JM, Hamilton JM, Deane CM, Valeyev NV, Sandell LJ, Downing AK 2004. Solution structure and dynamics of a prototypical chordin-like cysteine-rich repeat (von Willebrand Factor type C module) from collagen IIA. J Biol Chem 279: 53857–53866 [DOI] [PubMed] [Google Scholar]
- Orr AW, Pedraza CE, Pallero MA, Elzie CA, Goicoechea S, Strickland DK, Murphy-Ullrich JE 2003. Low density lipoprotein receptor-related protein is a calreticulin coreceptor that signals focal adhesion disassembly. J Cell Biol 161: 1179–1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea KS, Dixit VM 1988. Unique distribution of the extracellular matrix component thrombospondin in the developing mouse embryo. J Cell Biol 107: 2737–2748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea KS, Liu LH, Dixit VM 1991. Thrombospondin and a 140 kd fragment promote adhesion and neurite outgrowth from embryonic central and peripheral neurons and from PC12 cells. Neuron 7: 231–237 [DOI] [PubMed] [Google Scholar]
- Pallero MA, Elzie CA, Chen J, Mosher DF, Murphy-Ullrich JE 2008. Thrombospondin 1 binding to calreticulin-LRP1 signals resistance to anoikis. FASEB J 22: 3968–3979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MK, Lymn JS, Clunn GF, Hughes AD 1997. Thrombospondin-1 is a potent mitogen and chemoattractant for human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 17: 2107–2114 [DOI] [PubMed] [Google Scholar]
- Phelan MW, Forman LW, Perrine SP, Faller DV 1998. Hypoxia increases thrombospondin-1 transcript and protein in cultured endothelial cells. J Lab Clin Med 132: 519–529 [DOI] [PubMed] [Google Scholar]
- Pimanda JE, Ganderton T, Maekawa A, Yap CL, Lawler J, Kershaw G, Chesterman CN, Hogg PJ 2004. Role of thrombospondin-1 in control of von Willebrand factor multimer size in mice. J Biol Chem 279: 21439–21448 [DOI] [PubMed] [Google Scholar]
- Pongsomboon S, Wongpanya R, Tang S, Chalorsrikul A, Tassanakajon A 2008. Abundantly expressed transcripts in the lymphoid organ of the black tiger shrimp, Penaeus monodon, and their implication in immune function. Fish Shellfish Immunol 25: 485–493 [DOI] [PubMed] [Google Scholar]
- Posey KL, Hecht JT 2008. The role of cartilage oligomeric matrix protein (COMP) in skeletal disease. Curr Drug Targets 9: 869–877 [DOI] [PubMed] [Google Scholar]
- Posey KL, Hankenson K, Veerisetty AC, Bornstein P, Lawler J, Hecht JT 2008. Skeletal abnormalities in mice lacking extracellular matrix proteins, thrombospondin-1, thrombospondin-3, thrombospondin-5, and type IX collagen. Am J Pathol 172: 1664–1674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posey KL, Liu P, Wang HR, Veerisetty AC, Alcorn JL, Hecht JT 2010. RNAi reduces expression and intracellular retention of mutant cartilage oligomeric matrix protein. PLoS One 5: e10302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prabakaran D, Kim P, Kim KR, Arvan P 1993. Polarized secretion of thrombospondin is opposite to thyroglobulin in thyroid epithelial cells. J Biol Chem 268: 9041–9048 [PubMed] [Google Scholar]
- Prabakaran D, Kim PS, Dixit VM, Arvan P 1996. Oligomeric assembly of thrombospondin in the endoplasmic reticulum of thyroid epithelial cells. Eur J Cell Biol 70: 134–141 [PubMed] [Google Scholar]
- Prabakaran D, Ahima RS, Harney JW, Berry MJ, Larsen PR, Arvan P 1999. Polarized targeting of epithelial cell proteins in thyrocytes and MDCK cells. J Cell Sci 112: 1247–1256 [DOI] [PubMed] [Google Scholar]
- Preechaphol R, Leelatanawit R, Sittikankeaw K, Klinbunga S, Khamnamtong B, Puanglarp N, Menasveta P 2007. Expressed sequence tag analysis for identification and characterization of sex-related genes in the giant tiger shrimp Penaeus monodon. J Biochem Mol Biol 40: 501–510 [DOI] [PubMed] [Google Scholar]
- Primo L, Ferrandi C, Roca C, Marchiò S, di Blasio L, Alessio M, Bussolino F 2005. Identification of CD36 molecular features required for its in vitro angiostatic activity. FASEB J 19: 1713–1715 [DOI] [PubMed] [Google Scholar]
- Prochownik EV, O’Rourke K, Dixit VM 1989. Expression and analysis of COOH-terminal deletions of the human thrombospondin molecule. J Cell Biol 109: 843–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punekar S, Zak S, Kalter VG, Dobransky L, Punekar I, Lawler JW, Gutierrez LS 2008. Thrombospondin 1 and its mimetic peptide ABT-510 decrease angiogenesis and inflammation in a murine model of inflammatory bowel disease. Pathobiology 75: 9–21 [DOI] [PubMed] [Google Scholar]
- Qabar AN, Lin Z, Wolf FW, O’Shea KS, Lawler J, Dixit VM 1994. Thrombospondin 3 is a developmentally regulated heparin binding protein. J Biol Chem 269: 1262–1269 [PubMed] [Google Scholar]
- Qabar A, Derick L, Lawler J, Dixit V 1995. Thrombospondin 3 is a pentameric molecule held together by interchain disulfide linkage involving two cysteine residues. J Biol Chem 270: 12725–12729 [DOI] [PubMed] [Google Scholar]
- Raman P, Krukovets I, Marinic TE, Bornstein P, Stenina OI 2007. Glycosylation mediates up-regulation of a potent antiangiogenic and proatherogenic protein, thrombospondin-1, by glucose in vascular smooth muscle cells. J Biol Chem 282: 5704–5714 [DOI] [PubMed] [Google Scholar]
- Raugi GJ, Mumby SM, Abbott-Brown D, Bornstein P 1982. Thrombospondin: synthesis and secretion by cells in culture. J Cell Biol 95: 351–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raugi GJ, Mumby SM, Ready CA, Bornstein P 1984. Location and partial characterization of the heparin-binding fragment of platelet thrombospondin. Thromb Res 36: 165–175 [DOI] [PubMed] [Google Scholar]
- Raugi GJ, Olerud JE, Gown AM 1987. Thrombospondin in early human wound tissue. J Invest Dermatol 89: 551–554 [DOI] [PubMed] [Google Scholar]
- Raugi GJ, Mullen JS, Bark DH, Okada T, Mayberg MR 1990. Thrombospondin deposition in rat carotid artery injury. Am J Pathol 137: 179–185 [PMC free article] [PubMed] [Google Scholar]
- Recklies AD, Baillargeon L, White C 1998. Regulation of cartilage oligomeric matrix protein synthesis in human synovial cells and articular chondrocytes. Arthritis Rheum 41: 997–1006 [DOI] [PubMed] [Google Scholar]
- Ren B, Yee KO, Lawler J, Khosravi-Far R 2006. Regulation of tumor angiogenesis by thrombospondin-1. Biochim Biophys Acta 1765: 178–188 [DOI] [PubMed] [Google Scholar]
- Ren B, Song K, Parangi S, Jin T, Ye M, Humphreys R, Duquette M, Zhang X, Benhaga N, Lawler J, et al. 2009. A double hit to kill tumor and endothelial cells by TRAIL and antiangiogenic 3TSR. Cancer Res 69: 3856–3865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro SM, Poczatek M, Schultz-Cherry S, Villain M, Murphy-Ullrich JE 1999. The activation sequence of thrombospondin-1 interacts with the latency-associated peptide to regulate activation of latent transforming growth factor-β. J Biol Chem 274: 13586–13593 [DOI] [PubMed] [Google Scholar]
- Ridnour LA, Isenberg JS, Espey MG, Thomas DD, Roberts DD, Wink DA 2005. Nitric oxide regulates angiogenesis through a functional switch involving thrombospondin-1. Proc Natl Acad Sci 102: 13147–13152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riessen R, Fenchel M, Chen H, Axel DI, Karsch KR, Lawler J 2001. Cartilage oligomeric matrix protein (thrombospondin-5) is expressed by human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 21: 47–54 [DOI] [PubMed] [Google Scholar]
- Rodrigues RG, Guo N, Zhou L, Sipes JM, Williams SB, Templeton NS, Gralnick HR, Roberts DD 2001. Conformational regulation of the fibronectin binding and α 3β 1 integrin-mediated adhesive activities of thrombospondin-1. J Biol Chem 276: 27913–27922 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Manzaneque JC, Lane TF, Ortega MA, Hynes RO, Lawler J, Iruela-Arispe ML 2001. Thrombospondin-1 suppresses spontaneous tumor growth and inhibits activation of matrix metalloproteinase-9 and mobilization of vascular endothelial growth factor. Proc Natl Acad Sci 98: 12485–12490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg K, Olsson H, Mörgelin M, Heinegård D 1998. Cartilage oligomeric matrix protein shows high affinity zinc-dependent interaction with triple helical collagen. J Biol Chem 273: 20397–20403 [DOI] [PubMed] [Google Scholar]
- Roth JJ, Gahtan V, Brown JL, Gerhard C, Swami VK, Rothman VL, Tulenko TN, Tuszynski GP 1998. Thrombospondin-1 is elevated with both intimal hyperplasia and hypercholesterolemia. J Surg Res 74: 11–16 [DOI] [PubMed] [Google Scholar]
- Saito A, Hino S, Murakami T, Kanemoto S, Kondo S, Saitoh M, Nishimura R, Yoneda T, Furuichi T, Ikegawa S, et al. 2009. Regulation of endoplasmic reticulum stress response by a BBF2H7-mediated Sec23a pathway is essential for chondrogenesis. Nat Cell Biol 11: 1197–1204 [DOI] [PubMed] [Google Scholar]
- Samols MA, Skalsky RL, Maldonado AM, Riva A, Lopez MC, Baker HV, Renne R 2007. Identification of cellular genes targeted by KSHV-encoded microRNAs. PLoS Pathog 3: e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Antonio JD, Slover J, Lawler J, Karnovsky MJ, Lander AD 1993. Specificity in the interactions of extracellular matrix proteins with subpopulations of the glycosaminoglycan heparin. Biochemistry 32: 4746–4755 [DOI] [PubMed] [Google Scholar]
- Sato T, Sato M, Kiyohara K, Sogabe M, Shikanai T, Kikuchi N, Togayachi A, Ishida H, Ito H, Kameyama A, et al. 2006. Molecular cloning and characterization of a novel human β1,3-glucosyltransferase, which is localized at the endoplasmic reticulum and glucosylates O-linked fucosylglycan on thrombospondin type 1 repeat domain. Glycobiology 16: 1194–1206 [DOI] [PubMed] [Google Scholar]
- Schlötzer-Schrehardt U, Dietrich T, Saito K, Sorokin L, Sasaki T, Paulsson M, Kruse FE 2007. Characterization of extracellular matrix components in the limbal epithelial stem cell compartment. Exp Eye Res 85: 845–860 [DOI] [PubMed] [Google Scholar]
- Schroen B, Heymans S, Sharma U, Blankesteijn WM, Pokharel S, Cleutjens JP, Porter JG, Evelo CT, Duisters R, van Leeuwen RE, et al. 2004. Thrombospondin-2 is essential for myocardial matrix integrity: Increased expression identifies failure-prone cardiac hypertrophy. Circ Res 95: 515–522 [DOI] [PubMed] [Google Scholar]
- Schultz-Cherry S, Chen H, Mosher DF, Misenheimer TM, Krutzsch HC, Roberts DD, Murphy-Ullrich JE 1995. Regulation of transforming growth factor-β activation by discrete sequences of thrombospondin 1. J Biol Chem 270: 7304–7310 [DOI] [PubMed] [Google Scholar]
- Scott-Burden T, Hahn AW, Resink TJ, Bühler FR 1990. Modulation of extracellular matrix by angiotensin II: Stimulated glycoconjugate synthesis and growth in vascular smooth muscle cells. J Cardiovasc Pharmacol 16 (Suppl 4): S36–S41 [PubMed] [Google Scholar]
- Shaked Y, Bertolini F, Man S, Rogers MS, Cervi D, Foutz T, Rawn K, Voskas D, Dumont DJ, Ben-David Y, et al. 2005. Genetic heterogeneity of the vasculogenic phenotype parallels angiogenesis; Implications for cellular surrogate marker analysis of antiangiogenesis. Cancer Cell 7: 101–111 [DOI] [PubMed] [Google Scholar]
- Shitaye HS, Terkhorn SP, Combs JA, Hankenson KD 2010. Thrombospondin-2 is an endogenous adipocyte inhibitor. Matrix Biol 29: 549–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simantov R, Febbraio M, Silverstein RL 2005. The antiangiogenic effect of thrombospondin-2 is mediated by CD36 and modulated by histidine-rich glycoprotein. Matrix Biol 24: 27–34 [DOI] [PubMed] [Google Scholar]
- Södersten F, Ekman S, Schmitz M, Paulsson M, Zaucke F 2006. Thrombospondin-4 and cartilage oligomeric matrix protein form heterooligomers in equine tendon. Connect Tissue Res 47: 85–91 [DOI] [PubMed] [Google Scholar]
- Sottile J, Selegue J, Mosher DF 1991. Synthesis of truncated amino-terminal trimers of thrombospondin. Biochemistry 30: 6556–6562 [DOI] [PubMed] [Google Scholar]
- Stenina OI, Desai SY, Krukovets I, Kight K, Janigro D, Topol EJ, Plow EF 2003. Thrombospondin-4 and its variants: Expression and differential effects on endothelial cells. Circulation 108: 1514–1519 [DOI] [PubMed] [Google Scholar]
- Stenina OI, Ustinov V, Krukovets I, Marinic T, Topol EJ, Plow EF 2005. Polymorphisms A387P in thrombospondin-4 and N700S in thrombospondin-1 perturb calcium binding sites. FASEB J 19: 1893–1895 [DOI] [PubMed] [Google Scholar]
- Stracke JO, Fosang AJ, Last K, Mercuri FA, Pendás AM, Llano E, Perris R, Di Cesare PE, Murphy G, Knäuper V 2000. Matrix metalloproteinases 19 and 20 cleave aggrecan and cartilage oligomeric matrix protein (COMP). FEBS Lett 478: 52–56 [DOI] [PubMed] [Google Scholar]
- Streit M, Stephen AE, Hawighorst T, Matsuda K, Lange-Asschenfeldt B, Brown LF, Vacanti JP, Detmar M 2002. Systemic inhibition of tumor growth and angiogenesis by thrombospondin-2 using cell-based antiangiogenic gene therapy. Cancer Res 62: 2004–2012 [PubMed] [Google Scholar]
- Subramanian A, Wayburn B, Bunch T, Volk T 2007. Thrombospondin-mediated adhesion is essential for the formation of the myotendinous junction in Drosophila. Development 134: 1269–1278 [DOI] [PubMed] [Google Scholar]
- Sun X, Skorstengaard K, Mosher DF 1992. Disulfides modulate RGD-inhibitable cell adhesive activity of thrombospondin. J Cell Biol 118: 693–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun YD, Zhao XF, Kang CJ, Wang JX 2006. Molecular cloning and characterization of Fc-TSP from the Chinese shrimp Fennerpenaeus chinensis. Mol Immunol 43: 1202–1210 [DOI] [PubMed] [Google Scholar]
- Sun J, Hopkins BD, Tsujikawa K, Perruzzi C, Adini I, Swerlick R, Bornstein P, Lawler J, Benjamin LE 2009. Thrombospondin-1 modulates VEGF-A-mediated Akt signaling and capillary survival in the developing retina. Am J Physiol Heart Circ Physiol 296: H1344–H1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svensson L, Aszódi A, Heinegård D, Hunziker EB, Reinholt FP, Fässler R, Oldberg A 2002. Cartilage oligomeric matrix protein-deficient mice have normal skeletal development. Mol Cell Biol 22: 4366–4371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinnen M, Vanhoutte D, Van Almen GC, Hamdani N, Schellings MW, D’Hooge J, Van der Velden J, Weaver MS, Sage EH, Bornstein P, et al. 2009. Absence of thrombospondin-2 causes age-related dilated cardiomyopathy. Circulation 120: 1585–1597 [DOI] [PubMed] [Google Scholar]
- Tada H, Isogai S 1998. The fibronectin production is increased by thrombospondin via activation of TGF-β in cultured human mesangial cells. Nephron 79: 38–43 [DOI] [PubMed] [Google Scholar]
- Takagi J, Fujisawa T, Usui T, Aoyama T, Saito Y 1993. A single chain 19-kDa fragment from bovine thrombospondin binds to type V collagen and heparin. J Biol Chem 268: 15544–15549 [PubMed] [Google Scholar]
- Tan K, Duquette M, Liu JH, Zhang R, Joachimiak A, Wang JH, Lawler J 2006. The structures of the thrombospondin-1 N-terminal domain and its complex with a synthetic pentameric heparin. Structure 14: 33–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K, Duquette M, Liu JH, Shanmugasundaram K, Joachimiak A, Gallagher JT, Rigby AC, Wang JH, Lawler J 2008. Heparin-induced cis- and trans-dimerization modes of the thrombospondin-1 N-terminal domain. J Biol Chem 283: 3932–3941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K, Duquette M, Joachimiak A, Lawler J 2009. The crystal structure of the signature domain of cartilage oligomeric matrix protein: Implications for collagen, glycosaminoglycan and integrin binding. FASEB J 23: 2490–2501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K, Duquette M, Liu JH, Dong Y, Zhang R, Joachimiak A, Lawler J, Wang JH 2002. Crystal structure of the TSP-1 type 1 repeats: A novel layered fold and its biological implication. J Cell Biol 159: 373–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DK, Meganck JA, Terkhorn S, Rajani R, Naik A, O’Keefe RJ, Goldstein SA, Hankenson KD 2009. Thrombospondin-2 influences the proportion of cartilage and bone during fracture healing. J Bone Miner Res 24: 1043–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakar CV, Zahedi K, Revelo MP, Wang Z, Burnham CE, Barone S, Bevans S, Lentsch AB, Rabb H, Soleimani M 2005. Identification of thrombospondin 1 (TSP-1) as a novel mediator of cell injury in kidney ischemia. J Clin Invest 115: 3451–3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thur J, Rosenberg K, Nitsche DP, Pihlajamaa T, Ala-Kokko L, Heinegård D, Paulsson M, Maurer P 2001. Mutations in cartilage oligomeric matrix protein causing pseudoachondroplasia and multiple epiphyseal dysplasia affect binding of calcium and collagen I, II, and IX. J Biol Chem 276: 6083–6092 [DOI] [PubMed] [Google Scholar]
- Tingaud-Sequeira A, Chauvigné F, Lozano J, Agulleiro MJ, Asensio E, Cerdà J 2009. New insights into molecular pathways associated with flatfish ovarian development and atresia revealed by transcriptional analysis. BMC Genomics 10: 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tooney PA, Sakai T, Sakai K, Aeschlimann D, Mosher DF 1998. Restricted localization of thrombospondin-2 protein during mouse embryogenesis: A comparison to thrombospondin-1. Matrix Biol 17: 131–143 [DOI] [PubMed] [Google Scholar]
- Topol EJ, McCarthy J, Gabriel S, Moliterno DJ, Rogers WJ, Newby LK, Freedman M, Metivier J, Cannata R, O’Donnell CJ, et al. 2001. Single nucleotide polymorphisms in multiple novel thrombospondin genes may be associated with familial premature myocardial infarction. Circulation 104: 2641–2644 [DOI] [PubMed] [Google Scholar]
- Tucker RP 1993. The in situ localization of tenascin splice variants and thrombospondin 2 mRNA in the avian embryo. Development 117: 347–358 [DOI] [PubMed] [Google Scholar]
- Tucker RP 2004. The thrombospondin type 1 repeat superfamily. Int J Biochem Cell Biol 36: 969–974 [DOI] [PubMed] [Google Scholar]
- Tucker RP, Adams JC, Lawler J 1995. Thrombospondin-4 is expressed by early osteogenic tissues in the chick embryo. Dev Dyn 203: 477–490 [DOI] [PubMed] [Google Scholar]
- Tucker RP, Hagios C, Chiquet-Ehrismann R, Lawler J 1997. In situ localization of thrombospondin-1 and thrombospondin-3 transcripts in the avian embryo. Dev Dyn 208: 326–337 [DOI] [PubMed] [Google Scholar]
- Ueno A, Miwa Y, Miyoshi K, Horiguchi T, Inoue H, Ruspita I, Abe K, Yamashita K, Hayashi E, Noma T 2006. Constitutive expression of thrombospondin 1 in MC3T3-E1 osteoblastic cells inhibits mineralization. J Cell Physiol 209: 322–332 [DOI] [PubMed] [Google Scholar]
- Urry LA, Whittaker CA, Duquette M, Lawler J, DeSimone DW 1998. Thrombospondins in early Xenopus embryos: Dynamic patterns of expression suggest diverse roles in nervous system, notochord, and muscle development. Dev Dyn 211: 390–407 [DOI] [PubMed] [Google Scholar]
- van Eekelen M, Sasportas LS, Kasmieh R, Yip S, Figueiredo JL, Louis DN, Weissleder R, Shah K 2010. Human stem cells expressing novel TSP-1 variant have anti-angiogenic effect on brain tumors. Oncogene 29: 3185–3195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veliceasa D, Ivanovic M, Hoepfner FT, Thumbikat P, Volpert OV, Smith ND 2007. Transient potential receptor channel 4 controls thrombospondin-1 secretion and angiogenesis in renal cell carcinoma. FEBS J 274: 6365–6377 [DOI] [PubMed] [Google Scholar]
- Vischer P, Beeck H, Voss B 1985. Synthesis, intracellular processing and secretion of thrombospondin in human endothelial cells. Eur J Biochem 153: 435–443 [DOI] [PubMed] [Google Scholar]
- Voland C, Serre CM, Delmas P, Clezardin P 2000. Platelet-osteosarcoma cell interaction is mediated through a specific fibrinogen-binding sequence located within the N-terminal domain of thrombospondin 1. J Bone Miner Res 15: 361–368 [DOI] [PubMed] [Google Scholar]
- Volpert OV, Pili R, Sikder HA, Nelius T, Zaichuk T, Morris C, Shiflett CB, Devlin MK, Conant K, Alani RM 2002a. Id1 regulates angiogenesis through transcriptional repression of thrombospondin-1. Cancer Cell 2: 473–483 [DOI] [PubMed] [Google Scholar]
- Volpert OV, Zaichuk T, Zhou W, Reiher F, Ferguson TA, Stuart PM, Amin M, Bouck NP 2002b. Inducer-stimulated Fas targets activated endothelium for destruction by anti-angiogenic thrombospondin-1 and pigment epithelium-derived factor. Nat Med 8: 349–357 [DOI] [PubMed] [Google Scholar]
- Vos HL, Devarayalu S, de Vries Y, Bornstein P 1992. Thrombospondin 3 (Thbs3), a new member of the thrombospondin gene family. J Biol Chem 267: 12192–12196 [PubMed] [Google Scholar]
- Vranka J, Mokashi A, Keene DR, Tufa S, Corson G, Sussman M, Horton WA, Maddox K, Sakai L, Bächinger HP 2001. Selective intracellular retention of extracellular matrix proteins and chaperones associated with pseudoachondroplasia. Matrix Biol 20: 439–450 [DOI] [PubMed] [Google Scholar]
- Wang TN, Qian X, Granick MS, Solomon MP, Rothman VL, Berger DH, Tuszynski GP 1996. Thrombospondin-1 (TSP-1) promotes the invasive properties of human breast cancer. J Surg Res 63: 39–43 [DOI] [PubMed] [Google Scholar]
- Wang S, Wu Z, Sorenson CM, Lawler J, Sheibani N 2003. Thrombospondin-1-deficient mice exhibit increased vascular density during retinal vascular development and are less sensitive to hyperoxia-mediated vessel obliteration. Dev Dyn 228: 630–642 [DOI] [PubMed] [Google Scholar]
- Wang S, Herndon ME, Ranganathan S, Godyna S, Lawler J, Argraves WS, Liau G 2004a. Internalization but not binding of thrombospondin-1 to low density lipoprotein receptor-related protein-1 requires heparan sulfate proteoglycans. J Cell Biochem 91: 766–776 [DOI] [PubMed] [Google Scholar]
- Wang S, Skorczewski J, Feng X, Mei L, Murphy-Ullrich JE 2004b. Glucose up-regulates thrombospondin 1 gene transcription and transforming growth factor-β activity through antagonism of cGMP-dependent protein kinase repression via upstream stimulatory factor 2. J Biol Chem 279: 34311–34322 [DOI] [PubMed] [Google Scholar]
- Wang Y, Wang S, Sheibani N 2006. Enhanced proangiogenic signaling in thrombospondin-1-deficient retinal endothelial cells. Microvasc Res 71: 143–151 [DOI] [PubMed] [Google Scholar]
- Wang J, Feng J, Shi M, Qian L, Chen L, Yu M, Xu R, Shen B, Guo N 2008. De novo design of ErbB2 epitope targeting fusion protein stabilized by coiled coil structure. Mol Immunol 45: 106–116 [DOI] [PubMed] [Google Scholar]
- Watkins SC, Lynch GW, Kane LP, Slayter HS 1990. Thrombospondin expression in traumatized skeletal muscle. Correlation of appearance with post-trauma regeneration. Cell Tissue Res 261: 73–84 [DOI] [PubMed] [Google Scholar]
- Weinstat-Saslow DL, Zabrenetzky VS, VanHoutte K, Frazier WA, Roberts DD, Steeg PS 1994. Transfection of thrombospondin 1 complementary DNA into a human breast carcinoma cell line reduces primary tumor growth, metastatic potential, and angiogenesis. Cancer Res 54: 6504–6511 [PubMed] [Google Scholar]
- Westphal JR 2004. Technology evaluation: ABT-510, Abbott. Curr Opin Mol Ther 6: 451–457 [PubMed] [Google Scholar]
- Wilson R, Diseberg AF, Gordon L, Zivkovic S, Tatarczuch L, Mackie EJ, Gorman JJ, Bateman JF 2010. Comprehensive profiling of cartilage extracellular matrix formation and maturation using sequential extraction and label-free quantitative proteomics. Mol Cell Proteomics 9: 1296–1313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu FR, Zhou LY, Nagahama Y, Wang DS 2009. Duplication and distinct expression patterns of two thrombospondin-1 isoforms in teleost fishes. Gene Expr Patterns 9: 436–443 [DOI] [PubMed] [Google Scholar]
- Xu J, Xiao N, Xia J 2010. Thrombospondin 1 accelerates synaptogenesis in hippocampal neurons through neuroligin 1. Nat Neurosci 13: 22–24 [DOI] [PubMed] [Google Scholar]
- Yabkowitz R, Mansfield PJ, Ryan US, Suchard SJ 1993. Thrombospondin mediates migration and potentiates platelet-derived growth factor-dependent migration of calf pulmonary artery smooth muscle cells. J Cell Physiol 157: 24–32 [DOI] [PubMed] [Google Scholar]
- Yamano K, Qiu GF, Unuma T 2004. Molecular cloning and ovarian expression profiles of thrombospondin, a major component of cortical rods in mature oocytes of penaeid shrimp, Marsupenaeus japonicus. Biol Reprod 70: 1670–1678 [DOI] [PubMed] [Google Scholar]
- Yang Z, Kyriakides TR, Bornstein P 2000. Matricellular proteins as modulators of cell-matrix interactions: Adhesive defect in thrombospondin 2-null fibroblasts is a consequence of increased levels of matrix metalloproteinase-2. Mol Biol Cell 11: 3353–3364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Strickland DK, Bornstein P 2001. Extracellular matrix metalloproteinase 2 levels are regulated by the low density lipoprotein-related scavenger receptor and thrombospondin 2. J Biol Chem 276: 8403–8408 [DOI] [PubMed] [Google Scholar]
- Yee KO, Connolly CM, Duquette M, Kazerounian S, Washington R, Lawler J 2009. The effect of thrombospondin-1 on breast cancer metastasis. Breast Cancer Res Treat 114: 85–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young GD, Murphy-Ullrich JE 2004. The tryptophan-rich motifs of the thrombospondin type 1 repeats bind VLAL motifs in the latent transforming growth factor-β complex. J Biol Chem 279: 47633–47642 [DOI] [PubMed] [Google Scholar]
- Zamiri P, Masli S, Kitaichi N, Taylor AW, Streilein JW 2005. Thrombospondin plays a vital role in the immune privilege of the eye. Ocul Immunol Inflamm 15: 279–294 [DOI] [PubMed] [Google Scholar]
- Zaslavsky A, Baek KH, Lynch RC, Short S, Grillo J, Folkman J, Italiano JE Jr, Ryeom S 2010. Platelet-derived thrombospondin-1 is a critical negative regulator and potential biomarker of angiogenesis. Blood 115: 4605–4613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Lawler J 2007. Thrombospondin-based antiangiogenic therapy. Microvasc Res 74: 90–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Kazerounian S, Duquette M, Perruzzi C, Nagy JA, Dvorak HF, Parangi S, Lawler J 2009. Thrombospondin-1 modulates vascular endothelial growth factor activity at the receptor level. FASEB J 23: 3368–3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L, Isenberg JS, Cao Z, Roberts DD 2006. Type I collagen is a molecular target for inhibition of angiogenesis by endogenous thrombospondin-1. Oncogene 25: 536–545 [DOI] [PubMed] [Google Scholar]
- Zhou J, Feng X, Ban B, Liu J, Wang Z, Xiao W 2009. Elongation factor ELL (Eleven-Nineteen Lysine-rich Leukemia) acts as a transcription factor for direct thrombospondin-1 regulation. J Biol Chem 284: 19142–19152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziaie Z, Friedman HM, Kefalides NA 1986. Suppression of matrix protein synthesis by herpes simplex virus type 1 in human endothelial cells. Coll Relat Res 6: 333–349 [DOI] [PubMed] [Google Scholar]