Abstract
Purpose
Evaluation of the advantages and limitations of the Taylor Spatial Frame (TSF) with regard to the healing index (HI), distraction–consolidation time (DCT), accuracy of correction complications, and cost of the device.
Methods
Comparison of results with the traditional Ilizarov apparatus and a unilateral Orthofix fixator in a consecutive patient series with 135 bony deformity corrections.
Results
The HI did not differ significantly between all three fixators and was 57 days/cm for all patients. The DCT was significantly shorter for the TSF (148 days) compared to the Ilizarov fixator (204 days) and the Orthofix device (213 days). The accuracy of deformity correction was higher for the TSF than the other devices. The mean values of the measured angles after correction did not differ, but the variance of the results was the lowest. Also, the total rate of complications was considerably lower for the TSF. The Orthofix device showed a high rate of angular deformity during treatment, whereas both ring fixators had a relatively higher number of pin-related problems.
Conclusions
The findings in our patient series suggest the use of the Orthofix apparatus for simple lengthening over short to median distances and the Ilizarov device for the correction of simple bony deformities and pure lengthening over long distances. The TSF allows multiplanar corrections and lengthenings without complex modifications of the device. But, due to the remarkably higher costs, it has not yet been established as our routine device.
Level of evidence
Level IV—case series. Therapeutic Study—Investigating the Results of Treatment.
Keywords: Limb lengthening, Deformity correction, Taylor Spatial Frame, Ilizarov, Orthofix
Introduction
The Taylor Spatial Frame (TSF) is one of the more recent developments for deformity correction by external fixation and is based on a ring and strut concept utilizing the principles of the Stuart Gough or hexapod platform. The device has been in clinical use for more than 10 years and allows multiplanar deformity corrections simultaneously. To date, several studies have been published about its clinical application [1–5], but only a few addressed limb deformity correction [6–8]. Good results have been achieved with the TSF in achieving safe gradual correction, accurate results, and easy handling for both the patient and the surgeon. Only Fadel and Hosny raised concerns, regarding the system as complicated and the original Ilizarov device as easier for their daily clinical practice [1]. However, each type of external fixator exhibits individual mechanical characteristics that may affect osteogenesis and healing [9]. Comparative studies turned out to be an appropriate instrument to elaborate the advantages and limitations of new devices [10–13]. Hence, it was proposed to compare any new method to historical standards [14]. Rödl et al. have shown the presence of different workspaces for the TSF and the Ilizarov device with an increased minimal frame height for the TSF that might limit the indications for the TSF in a theoretical study [15]. To assess and compare the rate of bone formation, the bone distraction–consolidation time (DCT) has been indexed to the amount of lengthening. De Bastiani et al. [16] and Aldegheri [17] termed this the “healing index” (HI). Fischgrund et al. [18] defined the DCT as the interval from osteotomy to bony healing and considered the minimal consolidation time to be the more significant factor for smaller gaps. In addition to the assessment of the amount of healing, the accuracy of deformity correction and the rate of complications are important clinical outcome parameters for the assessment of external devices. But the definition of complications has been a subject of controversy in the limb-length literature [11] and differing definitions of complications have been suggested [11, 19–21].
Due to the lack of standardization, clinical reports of deformity correction vary widely in the published literature, which makes a direct comparison of these studies impossible [12, 22]. Published complication rates such as of the Orthofix device illustrate this problem, varying between 11 [23] and 250% [24]. The present study was conducted in order to compare the clinical results of the TSF with the traditional Ilizarov ring fixator and a unilateral Orthofix device in one institution under the same criteria to evaluate the relative advantages and limitations of the TSF.
Patients and methods
Between September 1995 and May 2010, 135 elective deformity corrections of the femur (n = 64) and the tibia (n = 71) were performed by external fixation on 80 patients at the first author’s institution. The average age at operation was 16.4 (4.0–69.8) years for all patients and this did not differ between the three devices. Thirty-five corrections were performed for congenital and 100 for acquired deformities. All patients were classified into three groups according to the device used:
Taylor Spatial Frame™ (TSF, Smith and Nephew, Memphis, TN, USA)
Ilizarov Fixator™ (Smith and Nephew, Memphis, TN, USA)
Orthofix® dynamic axial fixator (DAF, Orthofix S.R.L., Bussolengo, Verona, Italy)
Seventeen patients have been treated at two levels (femur and tibia) simultaneously and three patients twice at different points of time. It was suggested in the literature to evaluate the outcome for each segment rather than each patient [12]. Only elective corrections of angular deformities and/or limb lengthenings were included; traumatic cases and nonunions were excluded from this study. All interventions were performed by 11 surgeons. The TSF was only used by three surgeons. When performed by less experienced surgeons, the intervention was always directly supervised by a consultant orthopedic surgeon. The technique has already been published elsewhere [24].
All patients had a standing patella-forward full-length anteroposterior and lateral radiograph of both limbs for the malalignment test and standardized deformity measurements [25]. Patients were administered prophylactic perioperative single-shot antibiotics. Low-energy osteotomy was performed subperiostally with multiple drill holes and an osteotome [16]. The dressing at the pin sites was left in place until postoperative day 5. Showering was then allowed and the patients were instructed to clean the pin sites daily with a liquid disinfectant. A 7-day course of oral antibiotics was instituted if a pin site showed clinical signs of infections. Callotasis was started 1 week after the operation with 1 mm per day and adjusted commensurate with the degree of ossification on the radiographs in the further course. Regular X-ray controls were performed with a maximum interval of 6 weeks. Clinical review was performed weekly during lengthening until consolidation. The device was removed when tricortical consolidation was seen on the anteroposterior and lateral radiographs.
Retrospective radiographic assessment was performed by one independent observer who was not involved in the surgery (K.K.). The evaluated parameters for the assessment of bone formation were DCT (time from corticotomy until the distraction gap was healed) [18] and HI (number of days of external fixation treatment per cm of distraction) [16]. All complications have been documented in the medical records and were reviewed retrospectively. Patients with angulations of more than 5° had fixator manipulation and axial correction or fixator adjustment during the lengthening process if the apparatus did not allow modification for chronic correction. Complications rates were defined to be the number of complications per lengthened segment [11] and were graded independently according to the systems described by Dahl et al. [11], Donnan et al. [20], and Paley [19].
Statistical analysis was performed with the SPSS 17.0 statistical software package (SPSS Inc., Chicago, IL, USA). Analysis was performed for all patients and also for patients with pure lengthenings (>5 mm), patients with axis correction (≤5 mm), and for patients with minor lengthenings (5–50 mm) alone. The Gaussian distribution was tested with the Kolmogorov–Smirnov test. Quantitative variables are described by the mean and standard deviation: mean ± SD. The mean values of the subgroups were compared with Student’s t-test, one-way analysis of variance (ANOVA) (e.g., HI, DCT, angular measures), or the nonparametric Mann–Whitney test and Kruskal–Wallis test (e.g., complications), respectively. Correlations were calculated with Pearson’s or Spearman’s correlation coefficient, depending on the Gaussian distribution. Variables of multiple responses (e.g., for complications) were coded as dichotomies. A 0.05 level of significance was used for all analyses.
The present study was approved by the local ethical committee.
Results
Assessment of the rate of bone formation: healing index
The results are listed in detail in Table 1. The mean lengthening was the lowest for the TSF and differed significantly between the three devices (P = <0.001). In contrast, the distraction time was lower for the TSF than the other two devices, and did not differ significantly between the three devices when corrected for the severity of deformity (minor lengthenings) (P = 0.421). No significant correlation between the HI and the number of complications was detected (r = −0.090, P = 0.372).
Table 1.
Results for all three devices in detail (lengthenings: all patients with lengthening >5 mm; minor lengthening: lengthening >5 mm and ≤50 mm)
| TSF | Ilizarov | Orthofix | All patients | P-value | |
|---|---|---|---|---|---|
| Lengthened distance (mm) | |||||
| Lengthenings—femur | 26.5 (5–73) | 21.0 (5–81) | 40.0 (19–120) | 34.5 (5–120) | 0.009 |
| Lengthenings—tibia | 30.0 (6–75) | 40.0 (15–85) | 40.0 (17–100) | 40.0 (6–100) | 0.071 |
| Minor lengthenings | 30.0 (6–50) | 40.0 (12–50) | 32.0 (17–50) | 30.0 (6–50) | 0.122 |
| All patients | 30.0 (5–75) | 40.0 (5–85) | 40.0 (17–120) | 35.0 (5–120) | <0.001 |
| Distraction time (days) | |||||
| Patients—femur | 30.0 (5–216) | 38.0 (31–68) | 53.0 (19–150) | 40.0 (5–216) | 0.011 |
| Patients—tibia | 30.0 (10–84) | 40.0 (10–105) | 50.0 (19–95) | 35.0 (10–105) | 0.027 |
| Minor lengthenings | 30.5 (13–216) | 40.0 (20–76) | 35.0 (19–95) | 35.0 (13–216) | 0.421 |
| All patients | 30.0 (5–216) | 40.0 (10–105) | 52.0 (19–150) | 35.5 (5–216) | <0.001 |
| Healing index (HI; days/cm) | |||||
| Lengthenings—femur | 87.0 (32–266) | 40.0 (23–111) | 54.8 (19–134) | 55.2 (19–266) | 0.233 |
| Lengthenings—tibia | 67.7 (24–245) | 53.9 (23–173) | 66.1 (29–160) | 61.0 (23–245) | 0.651 |
| Minor lengthenings | 69.2 (24–266) | 56.7 (23–173) | 66.1 (41–160) | 67.7 (23–266) | 0.901 |
| All patients | 68.7 (24–266) | 52.9 (23–173) | 55.0 (19–160) | 56.6 (19–266) | 0.297 |
| Healing index (HI; days/cm) | |||||
| HI for ≤14 years old | 46.4 (24–188) | 51.8 (23–107) | 47.6 (29–89) | 47.6 (23–188) | 0.694 |
| HI for >14 years old | 89.4 (36–266) | 68.3 (23–173) | 57.1 (19–160) | 68.2 (19–266) | 0.016 |
| HI for ≤18 years old | 64.3 (24–266) | 51.8 (23–111) | 54.5 (29–160) | 54.0 (23–266) | 0.472 |
| HI for >18 years old | 142.8 (46–245) | 80.5 (41–173) | 56.2 (19–113) | 68.4 (19–245) | 0.009 |
| Distraction–consolidation time (DCT; days) | |||||
| All patients—femur | 146.5 (85–335) | 136.0 (92–363) | 206.0 (31–480) | 181.5 (31–480 | 0.107 |
| All patients—tibia | 148.5 (90–368) | 213.0 (92–385) | 280.0 (152–458) | 190.0 (90–458) | <0.001 |
| Minor lengthenings | 150.5 (87–368) | 213.0 (129–385) | 206.0 (129–385) | 190.0 (87–385) | 0.079 |
| All patients | 148.0 (85–368) | 204.5 (92–385) | 213.5 (31–480) | 188.0 (31–480) | <0.001 |
| Time between removal of the frame and full weight bearing (days)—all patients | |||||
| Median | 42.0 (13–1150) | 50.0 (10–330) | 48.5 (9–550) | 49.0 (9–1150) | 0.920 |
| Results of deformity measurements after correction and removal of the fixator [25]—all axis corrections | |||||
| mLDFA | 88.0 (82–94) | 86.0 (79–93) | 89.0 (82–100) | 87.7 (79–100) | 0.311 |
| mMPTA | 90.0 (84–94) | 90.0 (87–95) | 90.0 (87–92) | 90.0 (84–95) | 0.674 |
| mLDTA | 89.0 (84–93) | 89.7 (87–92) | 87.5 (80–92) | 89.0 (80–93) | 0.843 |
| aPPTA | 81.0 (50–91) | 73.5 (58–90) | 77.5 (66–91) | 78.0 (50–91) | 0.509 |
The Kruskal–Wallis test was used for the calculation of the P-values
HI was only calculated for patients with lengthening procedures (>5 mm). Distraction ≤5 mm was used for axis correction in order to avoid impingement of the segments. The mean HI did not differ between the three fixators and was 57 days/cm for all patients (P = 297; range: 19–266). The HI was significantly lower for patients under 14 years of age (48 days/cm, range: 23–188 days, P = 0.297) in comparison to older patients (68 days/cm, range: 19–266 days; t-test: P = 0.016). The HI showed a low negative correlation with the number of complications (r = −0.090, P = 0.372) and a moderate negative correlation with the distracted distance (r = −0.587; P < 0.001), with a high variation of the HI of all three devices for shorter distances and flattening of the curve towards a constant value (see Fig. 1). The HI did not differ between the three devices for the tibia (P = 0.651) and femur (P = 0.233) and acquired or congenital etiology when corrected for the severity of the deformity.
Fig. 1.
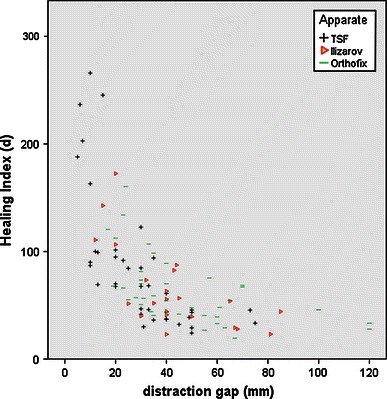
Scattergram of the healing index (HI) versus distracted distance (distraction gap) showing a correlation between the two parameters for all three devices
Assessment of the rate of bone formation: distraction–consolidation time
The DCT was significantly shorter for the TSF than for the other devices. The DCT did not differ between the three devices for minor lengthenings and lengthenings of the femur. The correlation between the DCT and distracted distance was highly significant (r = 0.510, P = <0.001). The DCT did not differ between acquired or congenital etiology when corrected for the severity of the deformity.
Precision of deformity correction
Axis correction was performed in 81 cases; 60 of them were combined with lengthening. The results of deformity measurements before and after correction showed a normal Gaussian distribution for all three devices. The mean values after deformity correction of all patients were within the normal values of a healthy population [25]. But looking at the subgroups in detail revealed singular values slightly outside the standard values. However, the mean measures after correction did not differ significantly between the three devices, but the variance of the results was lower for the TSF than the Ilizarov and Orthofix devices.
Complications
An average of 1.5 complications per osteotomy occurred (see Table 2). The number and rate of complications per patient was significantly lower for the TSF than for the Ilizarov fixator and was the highest for the Orthofix device. Looking at the data in detail revealed that the relative number of angulations during distraction was noticeably higher for the unilateral Orthofix device than for the TSF and the Ilizarov fixator (P = <0.001), whereas pin site problems and a decrease of knee flexion occurred relatively more frequently by the use of circular fixators, although the mean lengthened distance was relatively smaller. This higher rate of minor to moderate complications is also displayed in the three classification systems as published by Dahl et al. [11], Donnan et al. [20], and Paley [19] (see Table 2). The rate of severe complications did differ between all three fixators (see Table 2). The unilateral Orthofix device had significantly more “obstacles” (50.1%), “serious” (71.7%), and “grade III” (45.7%) complications, respectively, than the two circular fixators. There was a significant correlation between the age of the patient at the time of surgery and the number of complications (r = 0.0325, P < 0.001). The number of complications did not differ between femur and the tibia and congenital or acquired etiology.
Table 2.
Total number and rate of complications (number per osteotomy) of all three devices
| TSF | Ilizarov | Orthofix | All patients | P-value | |
|---|---|---|---|---|---|
| Number osteotomies/number of devices | |||||
| Total number of osteotomies, females | 29/27 | 15/15 | 26/21 | 70/63 | – |
| Total number of osteotomy, males | 25/19 | 20/20 | 20/19 | 65/58 | – |
| Total number of osteotomies | 54/46 | 35/35 | 46/40 | 135/121 | – |
| Number complications/number of devices | |||||
| Total number of complications | 58/46 | 69/35 | 76/40 | 203/121 | – |
| Rate of complications according to Donnan et al. [20] | |||||
| Grade I | 51.9% (range 1–2) | 48.6% (range 1–3) | 41.3% (range 1–3) | 47.4% (range 1–3) | 0.632 |
| Grade II | 31.5% (range 1–2) | 51.4% (range 1–3) | 34.8% (range 1–2) | 37.8% (range 1–3) | 0.118 |
| Grade III | 13.0% (range 1) | 22.9% (range 1–3) | 45.7% (range 1–6) | 26.7% (range 1–6) | <0.001 |
| Grade IV | 14.8% (range 1) | 31.4% (range 1–2) | 19.3% (range 1–3) | 20.7% (range 1–3) | 0.142 |
| Rate of complications according to Dahl et al. [11] | |||||
| Minor (I) | 50.0% (range 1–2) | 51.4% (range 1–3) | 45.7% (range 1–3) | 48.9% (range 1–3) | 0.754 |
| Serious (II) | 46.3% (range 1–2) | 51.4% (range 1–3) | 71.7% (range 1–6) | 56.3% (range 1–6) | <0.001 |
| Severe (III) | 13.0% (range 1) | 11.4% (range 1–2) | 17.4% (range 1–3) | 14.1% (range 1–3) | 0.734 |
| Rate of complications according to Paley [19] | |||||
| Problems (%) | 59.3% (range 1–2) | 60.1% (range 1–5) | 47.8% (range 1–3) | 55.6% (range 1–5) | 0.506 |
| Obstacles (%) | 20.4% (range 1) | 42.8% (range 1–2) | 50.1% (range 1–3) | 36.3% (range 1–3) | 0.003 |
| Major complications (%) | 3.7% (range 1) | 5.7% (range 1) | 8.7% (range 1–2) | 5.9% (range 1–2) | 0.563 |
| Minor complications (%) | 5.6% (range 1) | – | 4.3% (range 1) | 3.7% (range 1) | 0.386 |
| Late complications (%) | 3.7% (range 1) | 14.3% (range 1–2) | 10.9% (range 1) | 8.9% (range 1–2) | 0.184 |
Discussion
Healing index (HI)
Bone healing and the HI vary largely in former studies as they reportedly depend on multiple factors. The HI was shown to be higher for lengthening with simultaneous axial correction [19], to differ with the type of bone [12, 16, 18], level [18] form- [26] and number of osteotomies [9, 18, 19], underlying diagnosis [12], age of the patients [11, 12, 18, 19], and even the type of fixator when using a varying surgical technique [27]. In the present study, patients younger than 14 years of age had a significantly lower HI than older ones. The HI did not, however, differ between the three investigated devices. Fischgrund et al. have shown an exponential increase of the HI when the distraction gap approaches zero and a tendency towards a plateau only for large distances [18]. This indirect correlation was confirmed by Noonan et al. [12] and was also seen in our findings for all three fixators (see Fig. 1). The HI was regarded to be inaccurate except when distances are greater than 8 cm [18] and the DCT is suggested as a better parameter for shorter distances [12, 18].
Distraction–consolidation time (DCT)
In our study, the DCT was significantly lower for the TSF than the other two devices. Our findings suggest that DCT for a given distraction gap is lower for the TSF than for the Ilizarov and the highest for the Orthofix device. However, direct comparison of minor lengthening only, as recommended by other authors [25], revealed no significant difference for DCT in our series. Further studies with larger groups of patients have to be conducted in order to confirm this hypothesis finding.
Precision of deformity correction
The majority of deformity corrections with the unilateral Orthofix system in our study had to be readjusted due to an angulation of more than 5° during distraction. But only four cases in the Ilizarov group and none in the TSF group had fixator manipulation for angulation during distraction. However, the prescription of strut adjustments had to be modified for an average of 1.35 times per TSF patient to correct axial deviation during lengthening. Other authors reported angulations of between 9 and 37% for the Orthofix [12, 24, 27] and from 8 to 25% for the Ilizarov device [19]. But comparison of those studies is not possible due to the different definitions of angulation.
In our study, the Orthofix DAF turned out to be less stable than ring fixators, especially for femoral lengthenings, although the ball joint of the fixator was locked in the corrected position and stabilized with bone cement after the axial bony deformity was corrected [10]. Additionally, three pins for each fragment were used [24, 27] and prealignment was performed [19, 28]. Clearly, the Orthofix DAF cannot withstand the soft tissue tension, as other authors have already shown [10].
In contrast to other devices, residual correction with the TSF requires no return to the operating room and, therefore, less morbidity for the patient and little work for the surgeon [3]. However, the mean values of defined angles after deformity correction were comparable for all three devices, but the variance of results was lower for the TSF. In some previous studies using the TSF, the precision of deformity correction was not evaluated [4, 6]. Other authors reported on the accurate results of the deformity correction, but only in a low number of patients [2]. None of these authors did a direct comparison of the TSF with other fixators [1–8].
Complications
Complications and problems are common regardless of the method used [11, 24]. Except for the length gained, the outcome measures are based on the subjective assignment of end points and changing definitions of complications [12]. Tetsworth and Paley likewise reported on a comparatively low rate of complications (36%) but did not include pins site infections, which occurred in almost all of their patients [29]. For such reasons, complication rates in limb length surgery vary considerably between investigators [11]. This clearly shows that comparative studies are necessary in order to elaborate on the advantages and limitations of each device. Dahl et al. have shown comparable complication rates for the Ilizarov and De Bastiani method when corrected for the severity of the deformity [11]. In the present study, the two ring fixators had a tendency but not significantly higher rate of complications according to the three classification systems (see Table 2).
Certain types of complications seemed to be more specific for particular devices. Using a uniform pin care protocol for all three devices in our study, superficial pin infections occurred more frequently in circular fixators than in the unilateral Orthofix. Similar pin infection rates, but with great variation have been reported previously for the circular fixators, whereas remarkably low rates of pin site problems have been reported for the Orthofix device, especially by Italian work groups, obviously only quoting soft tissue abscesses [16, 23], and other authors mentioning only severe infections [12, 22]. Distinct from Paley’s association of pin site problems and their diameter [19], the Orthofix pins did not lead to a higher rate of pin site infections in our study. Other authors have also found equal infection rates between half pins and wires [30].
We observed a higher rate of temporary knee stiffness in both groups of circular fixators, although their mean distracted distance was slightly lower than for the Orthofix patients. The higher number of pin site problems and temporary knee stiffness in the ring fixator groups may be related to the soft tissue penetration of pins and wires at multiple sites in the axial plane, causing pain in flexion and extension. Fractures of K-wires and pins only occurred in the Ilizarov group. Other authors have found high rates of joint stiffness for the Orthofix, but their distracted distance was also remarkably longer [24]. On the other hand, lower stability of the unilateral system was evidently the cause for a higher number of angulations during distraction (see above).
Deformity correction is demanding and has a steep learning curve [11]. We also found a slight but insignificantly higher rate of complications for more inexperienced surgeons. Sluga et al. recommended the use of the TSF due to its ease of use and a low complication rate after only five patients treated with this device [4]. Other authors reported on a steep learning curve using the TSF and preferred using the Ilizarov device in their environment [1]. However, the choice of external fixator is generally determined by the experience and preference of the surgeon, the complexity of the problem, and the number of sites that need treatment [9].
The main weakness of the present study is the number of factors that might have biased the results. This is a common finding in most studies dealing with deformity correction by external fixation. However, this study should preferably be understood as expertise gained from a consecutive patient series. This study presents clinical results in the period from September 1995 to May 2010, with 135 deformities of 80 patients. Based on the experiences of our patient series, we redefined the indications at our institution for the devices used in this study:
Our findings suggest the use of the unilateral Orthofix apparatus for simple lengthening over short to median distances due to its simple mounting and better patient compatibility. Further advantages are its low weight and bulk [31] and ability to change from rigid to dynamic fixation via a telescopic body which, thus, promotes callus formation and ossification [10]. There are limitations in the correction of especially residual deformities, which also occur more frequently than in ring fixators.
The Ilizarov device allows corrections in multiple planes and is cheaper than the TSF. Also, gradual corrections of rotational deformities with simultaneous angular deformity correction and lengthening are possible [32], but it is complex, prone to errors [3], and there is a steep learning curve [11, 22]. Secondary deformities like translation may occur especially after derotation, requiring complex trigonometric calculations and frame adjustments, which, in some cases, have to be done while the patients are under anesthesia [32]. We use the Ilizarov device for the correction of simple bony deformities and pure lengthening over long distances, treatment of nonunions, and foot deformities.
In our series, the Taylor Spatial Frame achieved the most accurate results and was the easiest device to handle for the surgeon with the lowest number of complications, despite a relatively higher number of pin site problems and rate of reduced knee motion for ring fixators. In combination with computer software, by adjusting only the strut lengths on a simple frame, it allows multiplanar corrections also of residual deformities without complex modifications of the device. But, due to the remarkably higher costs, it has not yet been established as our routine device
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005;29:125–129. doi: 10.1007/s00264-004-0611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res. 2010;468:1352–1361. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feldman DS, Madan SS, Koval KJ, van Bosse HJ, Bazzi J, Lehman WB. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003;23:387–391. [PubMed] [Google Scholar]
- 4.Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop B. 2003;12:123–128. doi: 10.1097/01.bpb.0000049578.53117.03. [DOI] [PubMed] [Google Scholar]
- 5.Rozbruch SR, Pugsley JS, Fragomen AT, Ilizarov S. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22:88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 6.Blondel B, Launay F, Glard Y, Jacopin S, Jouve JL, Bollini G. Limb lengthening and deformity correction in children using hexapodal external fixation: preliminary results for 36 cases. Orthop Traumatol Surg Res. 2009;95:425–430. doi: 10.1016/j.otsr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Iobst C. Limb lengthening combined with deformity correction in children with the Taylor Spatial Frame. J Pediatr Orthop B. 2010;19:529–534. doi: 10.1097/BPB.0b013e32833dec43. [DOI] [PubMed] [Google Scholar]
- 8.Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 2006;15:387–395. doi: 10.1097/01.bpb.0000228380.27239.8a. [DOI] [PubMed] [Google Scholar]
- 9.Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–1258. doi: 10.2106/00004623-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Grill F. Correction of complicated extremity deformities by external fixation. Clin Orthop Relat Res. 1989;241:166–176. [PubMed] [Google Scholar]
- 11.Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994;301:10–18. [PubMed] [Google Scholar]
- 12.Noonan KJ, Leyes M, Forriol F, Cañadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80:793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Manner HM, Huebl M, Radler C, Ganger R, Petje G, Grill F. Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop. 2007;1:55–61. doi: 10.1007/s11832-006-0005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanitski DF, Bullard M, Armstrong P, Stanitski CL. Results of femoral lengthening using the Ilizarov technique. J Pediatr Orthop. 1995;15:224–231. doi: 10.1097/01241398-199503000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Rödl R, Leidinger B, Böhm A, Winkelmann W. Correction of deformities with conventional and hexapod frames—comparison of methods. Z Orthop Ihre Grenzgeb. 2003;141:92–98. doi: 10.1055/s-2003-37296. [DOI] [PubMed] [Google Scholar]
- 16.De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis) J Pediatr Orthop. 1987;7:129–134. doi: 10.1097/01241398-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Aldegheri R. Femoral callotasis. J Pediatr Orthop B. 1997;6:42–47. doi: 10.1097/01202412-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop. 1994;301:31–37. [PubMed] [Google Scholar]
- 19.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 20.Donnan LT, Saleh M, Rigby AS. Acute correction of lower limb deformity and simultaneous lengthening with a monolateral fixator. J Bone Joint Surg Br. 2003;85:254–260. doi: 10.1302/0301-620X.85B2.12645. [DOI] [PubMed] [Google Scholar]
- 21.Ilizarov GA. Clinical application of the tension–stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 22.Bonnard C, Favard L, Sollogoub I, Glorion B. Limb lengthening in children using the Ilizarov method. Clin Orthop Relat Res. 1993;293:83–88. [PubMed] [Google Scholar]
- 23.De Bastiani G, Aldegheri R, Renzi Brivio L. The treatment of fractures with a dynamic axial fixator. J Bone Joint Surg Br. 1984;66:538–545. doi: 10.1302/0301-620X.66B4.6746689. [DOI] [PubMed] [Google Scholar]
- 24.Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of the Ilizarov–Taylor Spatial Frame. J Bone Joint Surg Am. 2006;88:156–174. doi: 10.2106/JBJS.F.00745. [DOI] [PubMed] [Google Scholar]
- 25.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 26.Sakurakichi K, Tsuchiya H, Kabata T, Yamashiro T, Watanabe K, Tomita K. Correction of juxtaarticular deformities in children using the Ilizarov apparatus. J Orthop Sci. 2005;10:360–366. doi: 10.1007/s00776-005-0908-6. [DOI] [PubMed] [Google Scholar]
- 27.Aldegheri R. Distraction osteogenesis for lengthening of the tibia in patients who have limb-length discrepancy or short stature. J Bone Joint Surg Am. 1999;81:624–634. doi: 10.2106/00004623-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Leyes M, Noonan KJ, Forriol F, Cañadell J. Statistical analysis of axial deformity during distraction osteogenesis of the tibia. J Pediatr Orthop. 1998;18:190–197. [PubMed] [Google Scholar]
- 29.Tetsworth KD, Paley D. Accuracy of correction of complex lower-extremity deformities by the Ilizarov method. Clin Orthop Relat Res. 1994;301:102–110. [PubMed] [Google Scholar]
- 30.Gordon JE, Kelly-Hahn J, Carpenter CJ, Schoenecker PL. Pin site care during external fixation in children: results of a nihilistic approach. J Pediatr Orthop. 2000;20:163–165. [PubMed] [Google Scholar]
- 31.Tsuchiya H, Uehara K, Abdel-Wanis ME, Sakurakichi K, Kabata T, Tomita K. Deformity correction followed by lengthening with the Ilizarov method. Clin Orthop Relat Res. 2002;402:176–183. doi: 10.1097/00003086-200209000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Shtarker H, Volpin G, Stolero J, Kaushansky A, Samchukov M. Correction of combined angular and rotational deformities by the Ilizarov method. Clin Orthop Relat Res. 2002;402:184–195. doi: 10.1097/00003086-200209000-00017. [DOI] [PubMed] [Google Scholar]


