Abstract
Background
The Information-Motivation-Behavioral Skills (IMB) model often guides sexual risk reduction programs even though no studies have examined covariation in the theory’s constructs in a dynamic fashion with longitudinal data.
Purpose
Using new developments in latent growth modeling, we explore how changes in information, motivation, and behavioral skills over 9 months relate to changes in condom use among STD clinic patients.
Methods
Participants (N = 1281, 50% female, 66% African American) completed measures of IMB constructs at three time points. We used parallel process latent growth modeling to examine associations among intercepts and slopes of IMB constructs.
Results
Initial levels of motivation, behavioral skills, and condom use were all positively associated, with behavioral skills partially mediating associations between motivation and condom use. Changes over time in behavioral skills positively related to changes in condom use.
Conclusions
Results support the key role of behavioral skills in sexual risk reduction, suggesting these skills should be targeted in HIV prevention interventions.
Keywords: Condoms, HIV, IMB, Sexual risk behavior, STD
Sexually transmitted diseases (STDs) are highly prevalent, with nearly 19 million new infections per year in the USA [1, 2]. HIV rates also remain high, with over 56,300 new infections a year [3], 84% of which result from sexual contact [4]. Patients at STD clinics are more likely than those from community samples to acquire multiple STDs [5] and to be infected with HIV [6]. Correct and consistent condom use provides one of the most effective strategies for preventing the spread of STDs, including HIV [7–9], making determining the predictors of condom use among at-risk populations a priority.
Health behavior theories, such as the Information-Motivation-Behavioral Skills (IMB) model [10], identify precursors of condom use. The IMB model theorizes that information, motivation, and behavioral skills are fundamental determinants of HIV-preventive behaviors. Information involves facts about the targeted behavior (e.g., condom use, HIV transmission). Motivation to reduce risk may include attitudes toward prevention, social norms, and intentions to practice preventive behaviors such as condom use. Finally, behavioral skills involve individuals’ objective and perceived abilities to perform various behaviors involved in sexual risk reduction, such as using condoms with sexual partners. The IMB model posits that sexual health information and motivation to reduce risk lead to the development of the behavioral skills needed to reduce sexual risk behavior. These behavioral skills then contribute directly to HIV-preventive behavior and also partially mediate associations between information and motivation and behavior itself.
Support for the IMB model comes from research with a variety of populations. Multiple studies confirm the hypothesized associations between motivation, behavioral skills, and risk behavior (for reviews, see [11, 12]). However, the theory’s predictions about the role of information have had less consistent support, with studies finding positive, negative, and null associations between information and behavioral skills and behavior [12]. Even with these inconsistencies, the model’s constructs usually account for one third to one half of the variance in condom use [12].
In addition to cross-sectional studies, several longitudinal studies have provided evidence to support the IMB model [10, 13–22]. Although these studies demonstrate the usefulness of the IMB model in intervention design and the potential for its constructs to predict behavior, to our knowledge, no studies have made use of multiple assessments to examine covariation in the theory’s constructs, which is essential to the complete testing of the model. Because of this, we know little about how changes over time in information, motivation, and behavioral skills relate to changes in sexual risk behavior.
Therefore, for this study, we used parallel process latent growth modeling (LGM) to examine changes over time in information, motivation, behavioral skills, and condom use as well as the covariation among these constructs. Parallel process LGM, also known as associative LGM, allows for the examination of correlations between developmental parameters (intercepts and slopes) for multiple constructs [23]. By examining associations between these developmental parameters, multivariate LGMs clarify how changes in one variable relate to changes in other variables. In this case, we examined how changes in information, motivation, and behavioral skills related to changes in condom use. To do so, we used three assessments (3, 6, and 12 months post-intervention) from a large sample of STD clinic patients to test four hypotheses. First, we hypothesized that initial levels of information and motivation would positively predict initial levels of behavioral skills and condom use. Second, we predicted that initial levels of behavioral skills would positively predict initial levels of condom use. Third, we hypothesized that changes over time in information and motivation would positively predict changes over time in behavioral skills and condom use. Finally, we predicted that changes over time in behavioral skills would positively predict changes over time in condom use.
Method
Study Overview
We used three waves of data from a randomized clinical trial (RCT) evaluating interventions to reduce sexual risk among patients attending an STD clinic [24, 25]. For this report, we used only post-intervention assessments because we were interested in the associations between changes in IMB constructs independent of nonlinear, intervention-related change.
Participants and Procedures
Participants were 1,281 clinic patients (50% female; 66% African American; Mage = 29.6 years). Patients met with a research assistant (RA) to be screened and to receive details about the study. To be eligible for the RCT, patients needed to report: (a) that they were age 18 or older; (b) sexual risk behavior (e.g., multiple sexual partners, inconsistent condom use) in the past 3 months; and (c) a willingness to be tested for HIV. Patients were excluded if they were: (a) infected with HIV; (b) impaired (i.e., substance use, mental illness); (c) receiving inpatient substance abuse treatment; or (d) planning to move out of the area within the next year.
Eligible patients who agreed to participate provided written consent and completed an audio computer-assisted self-interview (ACASI) on a laptop computer. After completing the ACASI, participants received STD testing and treatment, as well as one of two brief, clinic-based sexual risk reduction interventions. All participants were reimbursed US$20 for their time. Participants were contacted at 3, 6, and 12 months post-intervention. At each occasion, they completed an ACASI and were reimbursed US$30. The protocol was approved by Institutional Review Boards of the participating institutions, and to protect participant privacy, a Federal Certificate of Confidentiality was obtained. Details regarding the RCT are available elsewhere [24, 25].
Measures
Surveys at each time point (3, 6, and 12 months) assessed the three major IMB constructs (information, motivation, and behavioral skills) as well as sexual behavior. Participants provided demographic and background information at the baseline and 3-month data collection points. All questions have been used in previous research [26–28].
HIV/STD Information
Information was assessed using the 18 items of the Brief HIV Knowledge Questionnaire (HIVKQ-18) [29]. Items assess knowledge about sexual and nonsexual transmission of HIV, condom use, and signs and symptoms of HIV (e.g., “can a woman get HIV if she has anal sex with a man?”). Participants could respond to the statements by choosing “yes,” “no,” or “I don’t know.” Correct responses were coded as 1 and incorrect or uncertain responses were coded as 0. At each time point, items were summed to create an HIV knowledge score, with higher scores indicating greater knowledge (α1 = .79, α2 = .80, α3 = .83).
Motivation
Motivation was assessed using measures of condom attitudes and condom use intentions. Condom attitudes were assessed using five items (e.g., “Sex with a condom can still be pleasurable”) adapted from published scales [30, 31]. Response choices were on a six-point scale ranging from “strongly disagree” [1] to “strongly agree” [6]. Items were averaged to create a condom attitudes score (α1 = .71, α2 = .70, α3 = .71) with higher scores indicating more positive attitudes toward condoms. Condom intentions were assessed using one item in response to a scenario: “I would refuse to have sex if we didn’t use a condom.” Participants rated their intentions using a four-point scale ranging from “definitely no” [1] to “definitely yes” [4]. Higher scores indicate greater intentions to use condoms.
Behavioral Skills
Behavioral skills were measured using seven items (e.g., “I refused to have sex with my partner unless a condom was used”) from the Condom Influence Strategy Questionnaire (CISQ) [32]. Response choices were on a five-point scale ranging from “never” [1] to “almost always” [5]. Items were averaged to create a total score (α1 = .89, α2 = .90, α3 = .91) with higher scores indicating the use of more skills. Previous research found community members who used a condom the last time they had sex reported higher CISQ scores [33].
Condom Use
Condom use (past 3 months) was assessed by asking participants how often they had: (a) vaginal sex with a condom; (b) vaginal sex without a condom; (c) anal sex with a condom; and (d) anal sex without a condom. Participants were asked these questions separately for steady and non-steady partners. Responses were used to determine the proportion of protected sexual events in past 3 months (number of times vaginal and anal sex occurred with a condom divided by the total number of vaginal and anal sexual events).
Demographic and Background Variables
At study enrollment, patients reported basic demographics (e.g., gender, age, ethnicity) and were tested for STDs; a dummy variable indicated whether they tested positive (0 = no, 1 = yes). Twenty-three percent of participants tested positive for an STD at baseline. At baseline, participants also reported the number of times in their lifetime they had engaged in sex in order to get money, drugs, food, or a place to stay; at the 3-month follow-up, they also reported the number of times they had done so in the past 3 months. These two reports were combined and recoded to indicate whether each participant had ever engaged in sex for money (0 = no, 1 = yes); 24% of participants had done so.
Data Management and Analysis
All variables were examined for univariate and multivariate outliers by inspecting box plots and examining the Mahalanobis distance statistic (δ2). Univariate outliers were recoded to a value three standard deviations from the mean [34]. Six multivariate outliers were identified and removed from the sample. We scaled measures equivalently on a 0–3-point scale for the parallel process model in line with recommendations [35], but report intercepts and slopes in terms of the original scales to increase interpretability.
Models were tested using LGM in Mplus [36]. Because many variables had non-normal distributions, the MLR estimator [37] was used. This expectation-maximization based estimator provides a robust χ2 test and correct standard errors under non-normality [38] and is a robust full information maximum likelihood estimator. We first tested LGMs independently for each construct of the IMB model, assuring acceptable fit and examining the means and variances of the intercepts and slopes. Consistent with published guidelines [38], parameters were fixed to represent linear growth over time for all constructs, and error variances were constrained to be equal across time. The individual LGMs were then combined in a parallel process (or associative) LGM [23, 39]. Associative LGMs include multiple individual LGMs (with random intercepts and slopes for each variable), as well as associations between the intercepts and slopes for different variables. When testing an associative LGM, we are interested in the relationships between initial levels of and changes in different variables. Finally, demographic variables were added to the parallel process model to assure that they did not modify associations between constructs.
Model fit was assessed using the comparative fit index (CFI) [40]; the Tucker–Lewis index (TLI) [41]; the standardized root mean square residual (SRMR) [42]; and the misfit measure known as the root-mean-square error of approximation (RMSEA) [43]. Good fit is indicated by CFI and TLI values greater than .95, SRMR values less than .08, and RMSEA values less than .05 [34, 43]. Because models were fit with the MLR estimator, the χ2values reported are Satorra–Bentler scaled (mean-adjusted) χ2values.
Results
Missing Data
Of the 1,483 participants at baseline, 1,082 (73%) provided data at 3 months, 1,101 (74%) provided data at 6 months, and 1,044 (70%) provided data at 12 months. For the current analyses, data were available from 1,281 participants who completed at least one follow-up (50% female; 66% African American; Mage = 29.6 years). As compared to participants originally enrolled in the study who did not provide follow-up data (Table 1), participants who completed at least one follow-up assessment were more likely to be older, female, African American, unemployed, low-income, and previously treated for STDs. Of the 1,281 participants included in the current analyses, 844 (66%) provided data at all three time points. Results of analyses including only those participants with complete data were not substantively different from those including the full sample of 1,281; therefore, we report results from the full sample.
Table 1.
Comparisons of participants retained and lost to follow-up
| Retained (n = 1281) % or M (SD) |
Lost (n = 202) % or M (SD) |
df | χ2 or t | |
|---|---|---|---|---|
| Female | 50% | 24% | 1 | 46.07*** |
| Latino | 8% | 12% | 1 | 2.98 |
| White | 22% | 39% | 1 | 27.99*** |
| Black | 66% | 48% | 1 | 27.03*** |
| Age | 29.59 (9.90) | 26.58 (7.37) | 1481 | −4.15*** |
| Unemployed | 53% | 42% | 1 | 8.74** |
| Education ≤ high school | 62% | 60% | 1 | .26 |
| Income ≤ $15,000 | 58% | 45% | 1 | 12.05*** |
| Non-heterosexual | 13% | 8% | 1 | 3.50 |
| Ever treated for STD | 79% | 60% | 1 | 34.87*** |
| Positive for STD (baseline) | 23% | 21% | 1 | .64 |
p < .01,
p < .001
Single-Construct LGMs
Descriptive statistics for all measures are reported in Table 2. Prior to fitting a parallel process model, we first fit LGMs independently for information, motivation, behavioral skills, and condom use.
Table 2.
Summary statistics for information, motivation, behavioral skills, and condom use by time of assessment
| Range | Time 1 (3 months) M (SD) | Time 2 (6 months) M (SD) | Time 3 (12 months) M (SD) | |
|---|---|---|---|---|
| Information | 0–18 | 14.88 (3.08) | 14.89 (3.11) | 14.82 (3.35) |
| Motivation: Attitudes | 1–6 | 4.62 (.91) | 4.62 (.92) | 4.61 (.92) |
| Motivation: Intentions | 1–4 | 3.38 (.91) | 3.32 (.94) | 3.33 (.91) |
| Behavioral skills | 1–5 | 2.67 (1.20) | 2.60 (1.23) | 2.53 (1.23) |
| Condom use (proportion) | 0–1 | .50 (.40) | .47 (.40) | .45 (.41) |
Information
The LGM for information fit the data well, χ2(3, N = 1230) = .30, p = .96, CFI = 1.00, TLI = 1.00, RMSEA = .00, SRMR = .02. Knowledge scores at 6 and 12 months were highly correlated; therefore, a correlation between the two was included in the model to improve fit. This model showed that the intercept for information was significantly different from 0, Mi = 2.48, CI.95 = 2.46, 2.51, p < .001; however, the slope for information did not differ from 0, Ms = −.001, CI.95 = −.01, .009, p = .78. At the group level, participants answered an average of 14.87 (out of 18) sexual health questions correctly; no change in their performance was observed over time. There was significant variance in the slope of information, Ds = .004, CI.95 = .000, .008, p < .05, but not in the intercept, Di = .001, CI.95 = −.02, .02, p = .89, indicating that there were individual differences in the change in knowledge across time, but no significant variation among participants in their initial levels of knowledge. Therefore, the variance of the information intercept was constrained to 0 in future models, meaning associations between this intercept and other model constructs could not be examined.
Motivation
Because motivation was modeled at each time point as a latent construct represented by attitudes and intentions, we fit a curve-of-factors LGM [23, 44]. This involved a two-step process: first, a latent construct of motivation was estimated at each time point, and then a growth curve was fit to these three latent constructs. The curve-of-factors LGM assumes factor invariance over each assessment, meaning the latent construct at each time point is represented by the same indicators with equal weighting of indicators over time [45]. Intercepts and residual variances of the indicators were constrained to be equal across time, and the same indicators were allowed to correlate across time [38, 46]. The curve-of-factors model for motivation fit the data well, χ2(10, N = 1274) = 4.65, p = .91, CFI = 1.00, TLI = 1.01, RMSEA = .00, SRMR = .02.
This model showed that that the intercept for motivation differed significantly from zero, Mi = 2.16, CI.95 = 2.13, 2.19, p < .001; however, the slope for motivation did not differ from zero, Ms = .002, CI.95 = −.01, .01, p = .74. These findings indicate that participants expressed strong motivation initially (2.16 out of 3), and there was no change in motivation over time. There was significant variance in the intercept of motivation, Di = .10, CI.95 = .07, .13, p < .001, but not in the slope, Ds = −.001, CI.95 = −.004, .003, p = .63, indicating that there were individual differences in initial levels of motivation, but no variation in the change in motivation across time. Therefore, the variance of the motivation slope was constrained to 0 in future models, meaning associations between this slope and other model constructs could not be examined.
Behavioral Skills
The LGM for behavioral skills fit the data well, χ2 (3, N = 1275) = 4.15, p = .25, CFI = 1.00, TLI = 1.00, RMSEA = .02, SRMR = .03. The intercept (Mi = 1.24, CI.95 = 1.19, 1.29, p < .001) and slope (Ms = −.04, CI.95 = −.05, −.02, p < .001) for behavioral skills differed significantly from zero. These findings indicate that participants had low-to-moderate behavioral skills initially (average score of 1.24 out of 3), and there was a decrease in these skills over time. Additionally, there was significant variance in both the intercept (Di = .50, CI.95 = .44, .55, p < .001) and the slope of behavioral skills (Ds = .014, CI.95 = .002, .03, p < .05), indicating that there were individual differences in initial levels of behavioral skills as well as in the change in behavioral skills across time.
Condom Use
The LGM for condom use fit the data well, χ2 (3, N = 1275) = 4.09, p = .25, CFI = 1.00, TLI = 1.00, RMSEA = .02, SRMR = .02. This model showed that that the intercept and slope for condom use both differed significantly from 0, Mi = 1.48, CI.95 = 1.41, 1.54, p < .001, and Ms = −.05, CI.95 = −.08, −.02, p < .001, respectively. These findings indicate that, at the group level, on average, participants were using condoms 49% of the time, and there was a decrease in the percentage of condom use over time (i.e., a 2% decrease every 3 months). Additionally, significant variance in both the intercept and the slope of condom use was found, Di = .74, CI.95 = .63, .84, p < .001, and Ds = .05, CI.95 = .02, .07, p < .001, indicating that there were individual differences in the percentage of condom use initially as well as in the change in this percentage over time.
Parallel Process Latent Growth Model
Based on the acceptable model fits for the individual constructs, we proceeded to fit one model including all constructs and the associations among them. Because we found no significant variance in the intercept of information or the slope of motivation, we could not investigate associations between these parameters and other intercepts and slopes. We modeled paths between intercepts and slopes based on the IMB model (Fig. 1); that is, we included direct paths from information, motivation, and skills to condom use, as well as indirect paths from information and motivation to condom use through skills. The intercept of each construct predicted both the intercepts and slopes of the downstream constructs, except that the information intercept did not predict any constructs. In addition, the slope of each construct predicted downstream slopes, except that the motivation slope did not predict any constructs. We looked at paths from intercepts to slopes (but not from slopes to intercepts) because we expected initial status to influence later trajectories (but not the reverse). We also modeled correlations between (a) the intercept of motivation and the slope of knowledge, (b) the intercept and slope of behavioral skills, and (c) the intercept and slope of condom use. Information and motivation have been found to be correlated in past studies (e.g., [21, 38, 47]); additionally, we anticipated that initial levels of constructs might relate to their later trajectories. All paths and correlations were included in the model initially but then constrained to 0 if t < 1 for parsimony. We allowed correlations between the residuals of measurements taken at the same time point (3, 6, and 12 months) [46]. We report standardized coefficients as well as bootstrapped 95% confidence intervals based on 5,000 iterations. We discuss only those results where the confidence interval indicated significance.
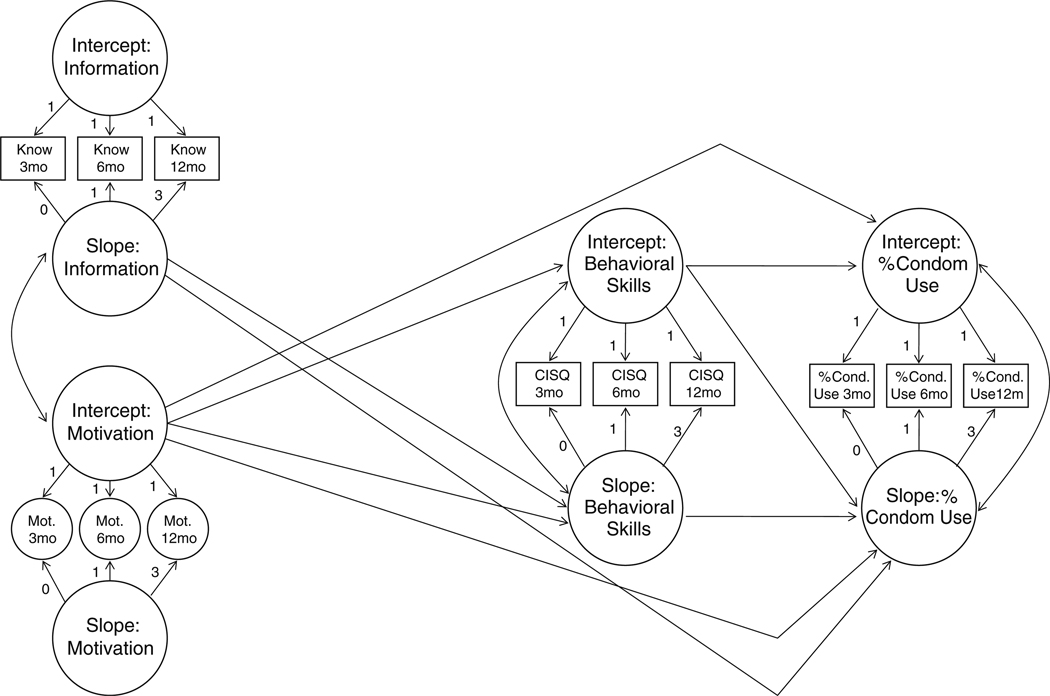
Fig. 1.
Theoretical model tested, including (a) paths from intercepts to intercepts and slopes and (b) paths from slopes to slopes based on the IMB model. Know knowledge score, Mot latent construct representing condom attitudes and intentions, CISQ Condom Influence Strategy Questionnaire score, 3mo 3-month data collection, 6mo 6-month data collection, 12mo 12-month data collection. The time scores for the slope growth factor are fixed at 0, 1, and 3 to define a linear growth model with time points of 3, 6, and 12 months
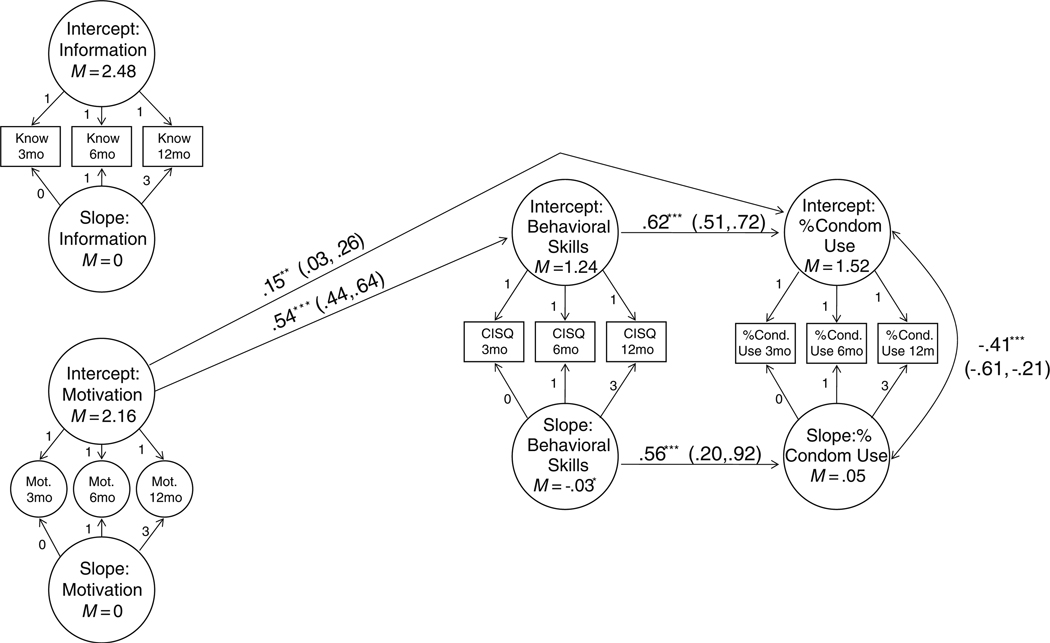
The parallel process model (Fig. 2) fit the data well, χ2 (77, N = 1275) = 157.97, p < .001, CFI =.98, TLI=.98, RMSEA = .03, SRMR = .04. Associations between intercepts were consistent with hypotheses. The intercept of motivation positively predicted the intercept of behavioral skills, β = .54, CI.95 = .44, .64, p < .001, indicating that those with higher levels of motivation initially also had more behavioral skills initially. Additionally, the intercept of motivation positively predicted the intercept of condom use, β = .15, CI.95 = .03, .26, p < .01, indicating that those with higher levels of motivation initially had a higher proportion of condom use initially. The intercept of behavioral skills also positively predicted the intercept of condom use, β = .62, CI.95 = .51, .72, p < .001, indicating that those with more behavioral skills initially used condoms more initially. There was an indirect effect of the intercept of motivation on the intercept of condom use, β = .33, CI.95 = .26, .41, p < .001, indicating that initial behavioral skills partially mediated the association between initial motivation and initial condom use, in line with the IMB model.
Fig. 2.
Parallel process latent growth model including all IMB model constructs. Nonsignificant paths are not shown. The time scores for the slope growth factor are fixed at 0, 1, and 3 to define a linear growth model with time points of 3, 6, and 12 months. χ2(77, N = 1275) = 157.97, p < .001; CFI = .98, TLI = .98, RMSEA = .03, SRMR = .04. ***p < .001 **p < .01
In terms of slopes, the slope of behavioral skills positively predicted the slope of condom use, β = .56, CI.95 = .20, .92, p < .001, indicating that those who decreased their behavioral skills more over time also decreased their percentage of condom use more over time. There was also a negative association between the intercept and slope of condom use, β = −.41, CI.95 = −.61, −.21, p < .001, indicating that those who had a lower percentage of condom use initially decreased the percentage less over time.1 The parallel process model explained 29% of the variance (p < .001) in the intercept of behavioral skills, 4% (p = .29) of the variance in the slope of behavioral skills, 50% of the variance (p < .001) in the intercept of condom use, and 37% of the variance (p < .05) in the slope of condom use.
Demographic Controls
We examined four demographic control variables: gender, age, baseline treatment for an STD, and history of exchanging sex for money, adding paths from these covariates to all intercepts and slopes. The full model including these controls fit the data well, χ2 (128, N = 1275) = 229.73, p < .001, CFI = .98, TLI = .98, RMSEA = .03, SRMR = .04. The inclusion of these four control variables in the parallel process model did not significantly modify any of the associations between intercepts and slopes detailed above. As shown in Table 3, higher levels of motivation initially were associated with being female, younger, and having no history of exchanging sex for money. Higher levels of behavioral skills initially were associated with being older and male. There were no significant demographic correlates of slopes. The model including demographic controls explained 22% of the variance (p < .001) in the intercept of motivation, 33% of the variance (p < .001) in the intercept of behavioral skills, 5% of the variance (p = .19) in the slope of behavioral skills, 50% of the variance (p < .001) in the intercept of condom use, and 39% of the variance (p < .05) in the slope of condom use.
Table 3.
Demographic predictors of IMB constructs
| Intercepts | |||
|---|---|---|---|
| Motivation | Behavioral skills | Condom use | |
| Sex | −.36*** (−.44, −.29) | .16*** (.08, .24) | |
| Age | −.21*** (−.29, −.13) | .11** (.03, .19) | |
| STD treatment | |||
| Sex work | −.16*** (−.23, −.09) | ||
Only statistically significant coefficients are shown. There were no significant demographic correlates of slopes. For sex, 0 = female and 1 = male. For STD treatment, 0 = no STD treatment at baseline, 1 = STD treatment at baseline. For sex work, 0 = no history of exchanging sex for money, 1 = history of exchanging sex for money
p < .01,
p < .001
Discussion
The findings from this study, the first to use longitudinal data to examine covariation of IMB model constructs over time, showed that changes in behavioral skills were related to changes in condom use. Associations between changes in these constructs have not previously been examined, and this finding provides strong support for the importance of behavioral skills in predicting safe sex behavior. Additionally, consistent with the IMB model [12], results supported the hypotheses that initial levels of motivation and behavioral skills would be positively associated with initial levels of condom use, and that behavioral skills would partially mediate associations between motivation and condom use.
Although there were clear associations between motivation, behavioral skills, and condom use, information did not play an important role in our parallel process LGM. Models showed no significant variation in initial levels of information, suggestive of a ceiling effect; this prevented us from examining associations between initial information and other constructs. However, we did find significant variance in the slope of information, indicating that participants were increasing or decreasing their knowledge at different rates. However, changes in information over time had no relation to changes in motivation, behavioral skills, or condom use, contrary to the IMB model.
This result replicates previous inconsistencies in associations between information and both behavioral skills [13, 48, 49] and behavior [14–16, 50]. This result, along with other null findings related to the information component of the IMB, suggests that information may not be a key determinant of risk behavior. Although null results might be used to argue for the modification of the IMB model, it is also possible that information’s role in determining risk behavior might vary based on population sub-group. Indeed, studies have shown differences in HIV-related knowledge across samples [51]. Information may play less of a role in determining behavioral skills or behavior when samples are very knowledgeable [12], as they were in this STD clinic sample.
Initial motivation levels were associated with initial behavioral skills and initial condom use, consistent with both the IMB theory and with empiric findings [10, 12–16, 19, 47]. However, in this sample, no changes in motivation occurred over time—the slope of motivation was equal to zero, and there was no variation in this slope across individuals. The motivation construct as measured here (i.e., attitudes and intentions) was quite stable. In order to assess whether changes in motivation relate to changes in other IMB constructs, it is necessary to find a sample where some modification in motivation occurs over time for at least some individuals (e.g., adolescents).
Previous longitudinal and intervention research has identified associations between motivation, behavioral skills, and behavior, with IMB constructs generally accounting for one third to one half of the variance in HIV preventive behaviors such as condom use [12]. These studies have also shown that motivation and behavioral skills at one time point can predict behavior several months to a year later [10, 15, 16, 19, 21]. However, to our knowledge, this study is the first to show that changes in behavioral skills relate to changes in condom use in the way predicted by the IMB model. Indeed, IMB constructs—primarily changes in behavioral skills—accounted for nearly 40% of the variance in change in condom use over time.
This study has important implications for sexual risk reduction interventions. Condom use declined over the 12 months of study follow-up, consistent with previous research finding that intervention effects decay over time [20, 52–55]. Some researchers have suggested that booster sessions, small doses of intervention material designed to prevent relapse, may help to minimize the decay of intervention effects [56, 57], but to date there has been little empiric evidence to guide the development of intervention boosters. Results from this study suggest that including information or motivation components in a booster session may not be an effective use of resources, because there was no deterioration in motivation over time, and because changes over time in information did not predict changes over time in condom use. However, changes over time in behavioral skills were a strong predictor of changes over time in condom use, suggesting that sexual risk reduction boosters should focus specifically on condom skills.
The present study made use of a large, diverse, at-risk sample, and retained more than 70% of participants across multiple data collection points. Nonetheless, one potential limitation is that participants had previously been given a sexual risk reduction intervention. Therefore, changes in IMB constructs over time within this sample might differ from changes over time among those who have not had the benefit of receiving such an intervention. However, it is important to note that 60% of the participants in the current study received only a brief (15 min) clinic-based intervention, with 40% attending a more intensive (4 h) risk reduction workshop [24]. Additionally, we have no reason to suspect that the associations between IMB constructs should be different due to the intervention, although future studies should confirm associations between constructs in other samples. A second limitation of our study is the use of self-report. We minimized this problem by using ACASI, which has been shown to reduce underreporting of sensitive information [58–60].
This study represents a first effort to use new developments in latent growth modeling to examine associations among constructs of the Information-Motivation-Behavioral Skills model. By showing that changes over time in behavioral skills are positively related to changes over time in condom use, results support the key role of behavioral skills in sexual risk reduction. Additionally, previously-identified associations between initial levels of motivation, behavioral skills, and condom use were again supported, with behavioral skills partially mediating associations between motivation and condom use, supporting the IMB model. Future studies should continue to make use of new statistical developments to test aspects of health behavior theories.
Acknowledgments
Funding This study was supported by grant R01-MH068171 from the Center for Mental Health Research on AIDS, National Institute of Mental Health to Michael P. Carey.
Footnotes
Because Mplus does not allow for the calculation of standardized, bootstrapped confidence intervals for covariances, this confidence interval was calculated by hand using the MLR standardized standard errors.
Conflict of Interest Statement The authors have no conflict of interest to disclose.
References
- 1.Centers for Disease Control and Prevention. 2007 Disease Profile. Atlanta: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 2.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: Incidence and prevalence estimates, 2000. Perspectives on Sexual and Reproductive Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 3.Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV in the United States. Atlanta, GA: 2010. [Google Scholar]
- 5.Leichliter J, Ellen J, Gunn R. STD repeaters: Implications for the individual and STD transmission in a population. In: Aral S, Douglas J, Lipshutz J, editors. Behavioral interventions for prevention and control of sexually transmitted diseases. New York: Springer; 2007. pp. 354–373. [Google Scholar]
- 6.Weinstock H, Sweeney S, Satten GA, Gwinn M. Grp SCHSS: HIV seroincidence and risk factors among patients repeatedly tested for HIV attending sexually transmitted disease clinics in the United States, 1991 to 1996. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998;19:506–512. doi: 10.1097/00042560-199812150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Condoms and STDs: Fact sheet for public health personnel. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2010. [Google Scholar]
- 8.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization. 2004;82:454–461. [PMC free article] [PubMed] [Google Scholar]
- 9.Pinkerton SD, Abramson PR. The Bernoulli-process model of HIV transmission: Applications and implications. In: Holtgrave DR, editor. Handbook of economic evaluation of HIV prevention programs. New York, NY US: Plenum Press; 1998. pp. 13–32. [Google Scholar]
- 10.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 11.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychology. 2006;25:462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 12.Fisher J, Fisher W, Shuper P. The Information–Motivation–Behavioral Skills model of HIV preventive behavior. Emerging theories in health promotion practice and research. 2009:21–63. [Google Scholar]
- 13.Anderson ES, Wagstaff DA, Heckman TG, et al. Information-Motivation-Behavioral Skills (IMB) model: Testing direct and mediated treatment effects on condom use among women in low-income housing. Annals of Behavioral Medicine. 2006;31:70–79. doi: 10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- 14.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13:238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman SC, Picciano JF, Roffman RA. Motivation to reduce HIV risk behaviors in the context of the Information, Motivation and Behavioral Skills (IMB) model of HIV prevention. Journal of Health Psychology. 2008;13:680–689. doi: 10.1177/1359105307082456. [DOI] [PubMed] [Google Scholar]
- 16.Mustanski B, Donenberg G, Emerson E. I can use a condom, I just don’t: The importance of motivation to prevent HIV in adolescent seeking psychiatric care. AIDS and Behavior. 2006;10:753–762. doi: 10.1007/s10461-006-9098-2. [DOI] [PubMed] [Google Scholar]
- 17.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychology. 1996;15:114–123. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- 18.Jaworski BC, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. Journal of Adolescent Health. 2001;29:417–425. doi: 10.1016/s1054-139x(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalichman S, Malow R, Devieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: Test of the information-motivation-behavior skills (IMB) model. Community Mental Health Journal. 2005;41:277–290. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalichman SC, Cain D, Weinhardt L, et al. Experimental components analysis of brief theory-based HIV/AIDS risk-reduction counseling for sexually transmitted infection patients. Health Psychology. 2005;24:198–208. doi: 10.1037/0278-6133.24.2.198. [DOI] [PubMed] [Google Scholar]
- 21.Kalichman SC, Simbayi LC, Cain D, et al. Generalizing a model of health behaviour change and AIDS stigma for use with sexually transmitted infection clinic patients in Cape Town, South Africa. AIDS Care. 2006;18:178–182. doi: 10.1080/09540120500456292. [DOI] [PubMed] [Google Scholar]
- 22.Malow RM, Stein JA, McMahon RC, et al. Effects of a culturally adapted HIV prevention intervention in Haitian youth. Journal of the Association of Nurses in AIDS Care. 2009;20:110–121. doi: 10.1016/j.jana.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling: concepts, issues, and applications. 2nd Ed. Mahwah, N.J: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 24.Carey MP, Senn TE, Vanable PA, Coury-Doniger P, Urban MA. Brief and intensive behavioral interventions to promote sexual risk reduction among STD clinic patients: results from a randomized controlled trial. AIDS and Behavior. 2010;14:504–517. doi: 10.1007/s10461-009-9587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Evaluating a two-step approach to sexual risk reduction in a publicly-funded STI clinic: Rationale, design, and baseline data from the Health Improvement Project-Rochester (HIP-R) Contemporary Clinical Trials. 2008;29:569–586. doi: 10.1016/j.cct.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carey MP, Maisto SA, Kalichman SC, et al. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carey MP, Braaten LS, Maisto SA, et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: A second randomized clinical trial. Health Psychology. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- 28.Carey MP, Carey KB, Maisto SA, et al. Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: Results from a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2004;72:252–268. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Education and Prevention. 2002;14:172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown IS. Development of a Scale to Measure Attitude toward the Condom as a Method of Birth-Control. Journal of Sex Research. 1984;20:255–263. [Google Scholar]
- 31.Sacco W, Levine B, Reed D, Thompson K. Attitudes about condom use as an AIDS-relevant behavior: Their factor structure and relation to condom use. Psychological Assessment. 1991;3:265–272. [Google Scholar]
- 32.Noar SM, Morokoff PJ, Harlow LL. Condom negotiation in heterosexually active men and women: Development and validation of a condom influence strategy questionnaire. Psychology & Health. 2002;17:711–735. [Google Scholar]
- 33.Noar SM, Morokoff PJ, Harlow LL. Condom influence strategies in a community sample of ethnically diverse men and women. Journal of Applied Social Psychology. 2004;34:1730–1751. [Google Scholar]
- 34.Kline R. Principles and practice of structural equation modeling. The Guilford Press; 2010. [Google Scholar]
- 35.Muthén L, Muthén B. Growth modeling with latent variables using Mplus. 2007 [Google Scholar]
- 36.Muthén LK, Muthén BO. Mplus user’s guide. 6 Ed. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 37.Asparouhov T, Muthen B. Multivariate statistical modeling with survey data. 2005 [Google Scholar]
- 38.Kaplan D. Structural equation modeling: Foundations and extensions. Sage Publications, Inc; 2008. [Google Scholar]
- 39.Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus Web Notes. 2002;4:1–22. [Google Scholar]
- 40.Bentler PM. Comparative Fit Indexes in Structural Models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 41.Tucker LR, Lewis C. Reliability Coefficient for Maximum Likelihood Factor-Analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 42.Jöreskog KG, Sörbom D. Chicago: National Educational Resources; 1981. LISREL V: Analysis of linear structural relationships by the method of maximum likelihood. [Google Scholar]
- 43.Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- 44.McArdle JJ. Dynamic but structural equation modeling of repeated measures data. In: Nesselroade JR, Cattell RB, editors. Handbook of multivariate experimental psychology. 2nd ed. New York, NY US: Plenum Press; 1988. pp. 561–614. [Google Scholar]
- 45.Nesselroade J. Temporal selection and factor invariance in the study of development and change. In: Baltes P, Brim J, OG, editors. Life-span development and behavior. Vol. 5. 1983. pp. 59–87. [Google Scholar]
- 46.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY US: Oxford University Press; 2003. [Google Scholar]
- 47.Donenberg GR, Schwartz RM, Emerson E, et al. Applying a Cognitive-Behavioral Model of HIV Risk to Youths in Psychiatric Care. AIDS Education and Prevention. 2005;17:200–216. doi: 10.1521/aeap.17.4.200.66532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bryan AD, Fisher JD, Fisher WA, Murray DM. Understanding condom use among heroin addicts in methadone maintenance using the information-motivation-behavioral skills model. Substance Use and Misuse. 2000;35:451–471. doi: 10.3109/10826080009147468. [DOI] [PubMed] [Google Scholar]
- 49.Fisher W, Williams S, Fisher J, Malloy T. Understanding AIDS risk behavior among sexually active urban adolescents: An empirical test of the information–motivation–behavioral skills model. AIDS and Behavior. 1999;3:13–23. [Google Scholar]
- 50.Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: testing the information-motivation-behavior skills (IMB) model. Journal of Adolescent Health. 2006;38:18–25. doi: 10.1016/j.jadohealth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 51.Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS and Behavior. 1997;1:61–74. [Google Scholar]
- 52.Ehrhardt AA, Exner TM, Hoffman S, et al. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: short- and long-term results of a randomized clinical trial. AIDS Care. 2002;14:147–161. doi: 10.1080/09540120220104677. [DOI] [PubMed] [Google Scholar]
- 53.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21:177–186. [PubMed] [Google Scholar]
- 54.Jemmott JB, 3 rd, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 55.Kalichman SC, Carey MP, Johnson BT. Prevention of sexually transmitted HIV infection: A meta-analytic review of the behavioral outcome literature. Annals of Behavioral Medicine. 1996;18:6–15. doi: 10.1007/BF02903934. [DOI] [PubMed] [Google Scholar]
- 56.Hennessy M, Bolan G, Hoxworth T, et al. Using growth curves to determine the timing of booster sessions. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:322–342. [Google Scholar]
- 57.Pedlow CT, Carey MP. Developmentally appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Annals of Behavioral Medicine. 2004;27:172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353:1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 59.Newman JC, Jarlais D, Turner CF, et al. The differential effects of face-to-face and computer interview modes. American Journal of Public Health. 2002;92:294–297. doi: 10.2105/ajph.92.2.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine. 2003;26:104–123. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]