Abstract
Background
Antireflux surgery (ARS) for gastroesophageal reflux disease (GERD) is one of the most frequently performed major operations in children. Many studies have described the results of ARS in children, however, with a wide difference in outcome. This study aims to systematically review the efficacy of pediatric ARS and its effects on gastroesophageal function, as measured by gastroesophageal function tests. This is the first systematic review comprising only prospective, longitudinal studies, minimizing the risk of bias.
Methods
Three electronic databases (Medline, Embase, and the Cochrane Library) were searched for prospective studies reporting on ARS in children with GERD.
Results
In total, 17 eligible studies were identified, reporting on a total of 1,280 children. The median success rate after ARS was 86% (57–100%). The success rate in neurologically impaired children was worse in one study, but similar in another study compared to normally developed children. Different surgical techniques (total versus partial fundoplication, or laparoscopic versus open approach) showed similar reflux recurrence rates. However, less postoperative dysphagia was observed after partial fundoplication and laparoscopic ARS was associated with less pain medication and a shorter hospital stay. Complications of ARS varied from minimal postoperative complications to severe dysphagia and gas bloating. The reflux index (RI), obtained by 24-h pH monitoring (n = 8) decreased after ARS. Manometry, as done in three studies, showed no increase in lower esophageal sphincter pressure after ARS. Gastric emptying (n = 3) was reported either unchanged or accelerated after ARS. No studies reported on barium swallow x-ray, endoscopy, or multichannel intraluminal impedance monitoring before and after ARS.
Conclusion
ARS in children shows a good overall success rate (median 86%) in terms of complete relief of symptoms. Efficacy of ARS in neurologically impaired children may be similar to normally developed children. The outcome of ARS does not seem to be influenced by different surgical techniques, although postoperative dysphagia may occur less after partial fundoplication. However, these conclusions are bound by the lack of high-quality prospective studies on pediatric ARS. Similar studies on the effects of pediatric ARS on gastroesophageal function are also very limited. We recommend consistent use of standardized assessment tests to clarify the effects of ARS on gastroesophageal function and to identify possible risk factors for failure of ARS in children.
Keywords: Gastroesophageal reflux, Antireflux surgery, Fundoplication, Children
Introduction
Gastroeophageal reflux disease (GERD) is a frequently encountered condition, affecting 7–20% of the pediatric population.1–3 Most symptomatic children respond well to medical treatment.3 However, when medical treatment fails and reflux symptoms persist, antireflux surgery (ARS) may be considered.4 ARS is one of the most frequently performed major operations in children, and over the last decades, numerous studies have been published on this subject. The efficacy of ARS and the relationship between ARS and gastroesophageal (GE) function in children is difficult to deduce from these publications, since most studies are underpowered, retrospective, and have heterogeneous study designs, as well as a heterogeneous pediatric patient population.
Therefore, in order to provide the best evidence on the efficacy of pediatric ARS, this article aims to systematically review all prospective, longitudinal studies, and randomized controlled trials (RCTs). In addition, this review aims to study the effects of ARS on GE function in children, as measured by pre- and postoperative assessment tests.
Material and Methods
Study Selection
Using predefined search terms, PubMed (from 1960), Embase (from 1980), and the Cochrane library (issue 11, 2010) were systematically searched for all articles published until November 10, 2010. For PubMed, the following search terms were used: (fundoplication[Title/Abstract] OR nissen[Title/Abstract] OR thal[Title/Abstract] OR toupet[Title/Abstract] OR boerema[Title/Abstract] OR antireflux surgery[Title/Abstract]) AND (child[Title/Abstract] OR children[Title/Abstract] OR infant[Title/Abstract] OR infants[Title/Abstract] OR pediatric[Title/Abstract] OR pediatrics[Title/Abstract] OR pediatric[Title/Abstract] OR pediatrics[Title/Abstract]). The same search strategy was used in EMBASE (replacing “[TIAB]” by “:ti,ab”). In addition, the Cochrane library was manually searched.
Assessment of Study Eligibility
Inclusion Criteria
Each article was independently assessed for eligibility using the following criteria: study population—infants and children (0–18 years), who underwent ARS; type of intervention—open or laparoscopic Nissen, Thal, or Toupet fundoplication; study design—only prospective study format; study results—operative results reported using symptom questionnaires, or clearly defined reflux symptoms, or GE function tests, both before and after ARS.
Exclusion Criteria
Studies were excluded if they did not meet the inclusion criteria or if the outcomes of interest were not reported. Articles in non-English languages were excluded. In case of multiple studies reporting on an overlapping population, only the study with the largest patient population was included.
Outcomes of Interest
Reflux specific symptom questionnaires; clearly defined reflux symptoms; reoperation rate; postoperative dilatations and GE functions tests: 24-h pH monitoring; combined 24-h pH-multichannel intraluminal impedance (pH-MII); manometry; endoscopy; scintigraphy of the stomach (gastric emptying studies) and barium swallow radiography.
In this systematic review, success of pediatric ARS will be defined as complete relief of reflux symptoms.
Data Extraction
The titles and abstracts of all identified studies were reviewed by two independent authors (WS, MH) according to the MOOSE criteria.5 Full publications were obtained for articles that appeared potentially relevant. References in these selected articles were also screened for cross-reference.
The following data were extracted from each selected article: Study design, study population, surgical method, outcome assessment techniques, duration of follow-up, and study outcomes of interest.
Results
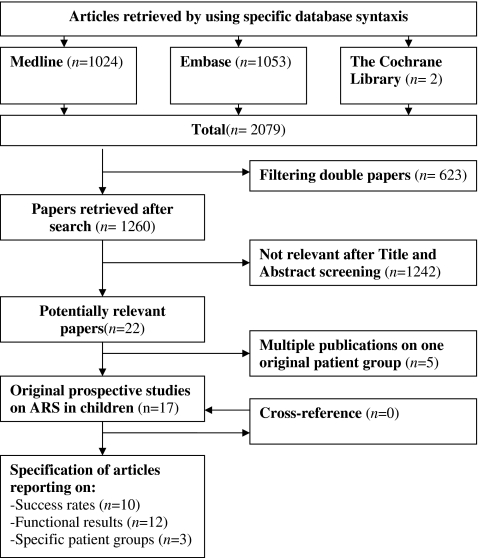
In total, 1,260 articles were identified and screened. Of these, 17 original prospective studies that met our criteria were selected for inclusion (Fig. 1).6–23
Fig. 1.
Flow chart illustrating details of selection of studies on results of anti-reflux surgery in children
Included trials were published between 1995 and 2010 and reported on a total of 1,280 children. Most studies only presented very short-term follow-up; however, a wide range in follow-up duration was present (1–96 months). Age at time of surgical intervention varied widely between the included studies from 0.25 to 20 years (Table 1).
Table 1.
Details on included prospective clinical trials on ARS in children
| Study (year) | Period | Method | n | Follow-up (months) | Patient characteristics | |
|---|---|---|---|---|---|---|
| Comorbidity | Age: mean or range (years) | |||||
| Capito (2008)6 | 1992–2003 | LNF | 127 | 66 | All | 0.25–20 |
| Cheung (2006)7 | 1999–2004 | ONF + G | 9 | 36–60 | Only NI | 8.5 (SD 3.5) |
| LNF + G | 11 | |||||
| Durante (2007)8 | 2003–2004 | ONF ± G | 7 | 3 | Only NI | 0.33–12.25 |
| VGP ± G | 7 | |||||
| Engelmann (2010)9,10 | 2001–2006 | LThF | 76 | 6 | All | 7 (SD 6.1) |
| Estevão-Costa (2010)11 | NR | ONF | 20 | 6–12 | All | NR |
| LNF | 5 | |||||
| Boix–Ochoa | 4 | |||||
| Kawahara (1998)12 | 1996–1997 | NF + Stamm | 7 | 1–3 | All | |
| Kawahara (2000)13 | 1998–1999 | LNF | 12 | 1–2 | All | 0.5–13 |
| Kubiak (2010)14 | 1998–2007 | LNF | 89 | 1.5 | All | 5.2 (SD 4.7) |
| LTouF | 86 | |||||
| Mattioli (2002)15 | 1998–2002 | LNF | 254 | 6–54 | All | 4.8 (0.025–14) |
| LTouF | 5 | |||||
| LThF/LJ | 29/10 | |||||
| Mattioli (2002)16 | 1993–2000 | ONF | 17 | 6 | No NI | 5 (SD 6.3) |
| LNF | 49 | |||||
| Menon (2002)17 | 1993–1999 | LNF | 11 | 12 | No NI | 9–15 |
| LTouF | 1 | |||||
| Mousa (2006)18 | NR | ONF | 6 | 3–7 | All | 0.5–18 |
| LNF | 7 | |||||
| Soyer (2007)19 | 2003–2004 | NF | 13 | 1–3 | All | 6.7 (SD 3.3) |
| Srivastava (2007)20 | 2005–2006 | O + LNF + G | 63 | 1 | Only NI | 1.8 (SD NR) |
| Van der Zee (1999)21 | 1993–1996 | LThF | 53 | 10 | All | NR |
| Weber (1995)22 | 1991–1993 | ONF | 56 | 12–36 | Only NI | 0.5–12 |
| Weber (1999)23 | 1990–1997 | ONF | 102 | 12–96 | No NI | 0.25–16 |
| LTouF | 154 | |||||
NF Nissen fundoplication (open or laparoscopic unknown), ONF open Nissen fundoplication, LNF laparoscopic Nissen fundoplication, LThF laparoscopic Thal fundoplication, LTouF laparoscopic Toupet fundoplication, LJ Lortat Jacob, VGP vertical gastric placation, G gastrostomy, Stamm Stamm gastrostomy, EA esophageal atresia, NI neurologically impaired, All all patients, SD standard deviation, NR not recorded
Only two RCTs were identified, and only five articles used control groups to verify their results.6,8–10,14,23 Most studies used standardized surgical methods and investigation techniques and reported adequate on lost to follow-up. However, the overall methodological quality was generally poor. All potential threats to validity are summarized in Table 2.
Table 2.
Risk of bias summary
| Study (year) | Capito et al.6 | Cheung et al.7 | Durante et al.8 | Engelmann et al.9,10 | Estevão-Costa et al.11 | Kawahara et al.12 | Kawahara et al.13 | Kubiak et al.14 | Mattioli et al.15 | Mattioli et al.16 | Menon et al.17 | Mousa et al.18 | Soyer et al.19 | Srivastava et al.20 | Van der Zee et al.21 | Weber et al.22 | Weber et al.23 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Randomization | − | − | + | − | − | − | − | + | − | − | − | − | − | − | − | − | − |
| Controlled | + | − | + | + | − | − | − | + | − | − | − | − | − | − | − | − | + |
| Standardization | + | − | + | + | + | + | + | + | − | + | − | + | + | + | + | − | − |
| Adequate report on loss to follow-up | + | NA | NA | + | + | + | + | NA | NA | NA | NA | + | NA | − | + | − | − |
| Potential other source bias | +a | +b,c | +d | − | +e | +c | +b | +f |
NA not applicable (no lost to follow-up)
aNo power calculation, underpowered
bHigh drop-out percentage
cMale/female imbalance
dSignificant baseline imbalance in weight between the two arms
eTime horizon determines method of surgical approach (open vs. laparoscopic)
fPatient assignment based on patient characteristics: Toupet Fundoplication in patients with symptoms or radiological signs of gastroesophageal dysmotility and adolescent patients and Nissen Fundoplication in patients with life-threatening symptoms or esophageal strictures
Success Rate
Overall Success Rate
In 10 out of 17 (59%) studies (Table 3), the success rate of antireflux surgery in eliminating reflux symptoms was reported. Short-term success rates (within 6 months after surgery) were reported in seven of the ten studies and varied from 57–100% (median 86%). Long-term success rates (follow-up period longer than 6 months) were reported in three of the ten studies and varied from 70–96% (median 72%). In one study, the outcome after redo ARS (in 5% of patients) was included, which resulted in a secondary success rate of 99% after long-term follow-up.6 Symptom severity scores were available in only one study,10 showing a significant reduction in symptom severity after laparoscopic anterior partial (Thal) fundoplication.
Table 3.
Success rate (complete resolution of gastroesophageal reflux symptoms) of ARS in children
| Study | Short-term SR (%) (FU < 6 months) | Long-term SR (%) (FU > 6 months) | Long-term SR (%) after second ARS |
|---|---|---|---|
| Capito et al.6 | NR | 72 | 99 |
| Cheung et al.7 | NR | 70 | NR |
| Durante et al.8 | 57 | NR | NR |
| Kawahara et al.12 | 100 | NR | NR |
| Mattioli et al.15 | NR | 96.2 | NR |
| Menon et al.17 | 100 | NR | NR |
| Soyer et al.19 | 86 | NR | NR |
| Van der Zee et al.21 | 75 | NR | NR |
| Weber et al.22 | 79 | NR | NR |
| Weber et al.23 | 93 | NR | NR |
SR Success rate, FU follow-up, NR not recorded
Failure was not defined in most studies. Some studies reported the failure rate only as the need for reoperation. In nine studies,6,7,9,10,15,19–23 a redo percentage was reported, varying from 0–3.8% (median 1%). The indication for redo operation was recurrent reflux in all cases.
Success Rate in Selected Patient Groups
Four studies reported solely on neurologically impaired (NI) children undergoing ARS.7,8,20,22 Success rates varied from 57–79% (median 70%). Two studies compared outcome of ARS in NI patients to neurologically normal (NN) children. The first study demonstrated that recurrence of reflux was significantly higher in NI patients than in NN patients (18% vs. 2%, p = 0.01).6 The second study demonstrated a small, but significant difference in favor of NI patients concerning relative postoperative improvement of symptom severity, but no significant differences in 24-h pH monitoring, gastric emptying, or quality of life scores between patient with or without neurological impairment.9,10
In three studies, patients were included who had previously been operated for esophageal atresia, but none reported results for this group separately.14,19,21 No prospective studies have been published showing only results in children with esophageal atresia undergoing antireflux surgery.
Success Rate Depending on Surgical Technique
Recently, an RCT was published comparing complete versus partial fundoplication in children.14 In this study, no significant difference in short-term outcome between laparoscopic Nissen fundoplication and laparoscopic Thal fundoplication was seen. However, a higher rate of severe dysphagia and complications were found after Nissen fundoplication.
A prospective, non-randomized study comparing open Nissen fundoplication to open Toupet fundoplication showed similar recurrence rates.23 In this study, Toupet fundoplication also resulted in less postoperative dysphagia. Furthermore, Toupet fundoplication resulted in lower reoperation rates, shorter time to first feeding, and shorter hospital stay. Patients were, however, assigned to either technique based on preoperative symptoms, gastroesophageal motility, age, and learning curve of the surgeon (Table 2).
Durante et al. randomly allocated patients to either Nissen fundoplication or vertical banded gastroplasty and showed no significant differences between these procedures. However, the number of patients included in this trial was very small (seven patients per group).8
No RCTs comparing laparoscopic to open fundoplication were published. Two prospective studies comparing open with laparoscopic fundoplication were identified, showing similar recurrence rates.7,16 However, patients after laparoscopic ARS required less pain medication (one vs. six doses, p < 0.05), and had a shorter hospital stay (2 vs. 7 days, p < 0.05).
Complications
Complications were not consistently reported. Perioperative complication rates varied widely between 0% and 54%, including esophageal perforation, pneumonia, and wound infections. The highest complication rates were found in studies that only included neurologically impaired patients.22
Nine studies reported on dysphagia, demonstrating postoperative dysphagia in zero to 33% of patients.6,9,12–14,16,17,21,23 However, this rarely lasted after the first few months following surgery. In two studies, balloon dilatation was used to treat postoperative dysphagia.14,17 Only one study reported prolonged dysphagia postoperatively.6 Postoperative dysphagia was more commonly reported after complete fundoplication than after partial fundoplication.23 Postoperative gas bloating was not reported in any of the prospective studies.
Overall mortality during follow-up ranged from 0% to 29%. Surgery-related mortality rate was 0% in eight studies7,8,15,17,19,21–23 and 0.7% in one study.6 In this particular study, the patient died of peritonitis following postoperative detachment of a simultaneously placed gastrostomy.
Pre- and Postoperative Assessment Tests
In most (15/17) studies, 24-h pH monitoring was performed prior to ARS.6–10,12–17,19–23 Postoperative pH monitoring was routinely performed in eight studies.6–10,12,17,19,21 All these studies reported a decrease in incidence and/or severity of reflux after ARS, including a reduction in RI (percentage of time with a pH <4) and the number and duration of reflux episodes. Four of these eight studies actually published the numbers of the RI before and after surgery7,8,12,19 (Table 4). Data on symptom association probability scores were not reported.
Table 4.
Studies reporting reflux indices pre- and postoperatively in children
| Study | n | Reflux index preoperatively (%) | Reflux index postoperatively (%) | p |
|---|---|---|---|---|
| Cheung et al.7 | 20 (NI) | 5.7 | 0.15 | 0.009 |
| Durante et al.8 | 7 (Nissen) | 14.8 | 4.3 | 0.002 |
| 7 (VGP) | 25.7 | 12.1 | 0.042 | |
| Kawahara et al.12 | 10 | 15 | 0 | NR |
| Soyer et al.19 | 13 | 24.7 | 0.9 | <0.05 |
NI Neurologically impaired, VGP vertical gastric placation, NR not recorded
Three studies reported manometry data before and after Nissen fundoplication.12,13,19 Although the lower esophageal sphincter (LES) pressure seemed to increase after ARS, this was not statistically significant in any of the studies. In one study, the number of transient LES relaxations had significantly decreased postoperatively from 13 to 7 (p < 0.05).12 ARS did not seem to affect esophageal motor function.13,19
Three studies reported on gastric emptying before and after ARS using scintigraphy. In two studies, ARS had no significant effect on gastric emptying rate.10,18 The third study demonstrated a significant acceleration of the gastric emptying rate after ARS.11
In two studies, a reflux specific symptom severity score was employed, showing significantly improved scores after ARS.9,10,17 In one other study, a quality of life (QoL) questionnaire was performed to evaluate the results of ARS, showing a significant improvement in quality of life after ARS.20
In none of the studies, MII monitoring, endoscopy, or barium swallow radiography was performed before and after ARS.
Discussion
Our systematic review identified more than 1,000 publications after searching the available databases for pediatric ARS. Most of these articles were found to be retrospective studies or case reports. Only 17 prospective, longitudinal studies, using reflux symptom scores and/or GE tests could be identified that described the outcome of ARS in pediatric GERD patients. This indicates that the vast majority of studies on pediatric ARS are of poor quality.
In this systematic review, success was defined as complete relief of reflux symptoms. The median reported success rate after pediatric ARS was 86%, but varied widely (57–100%), due to several reasons. First, in most studies, heterogeneous patient groups and different surgical techniques were included and compiled in one general data pool. Second, although guidelines of the NASPHGAN4 have been published, an actual unanimous definition of therapy-resistant GERD is lacking. This results in a large variety of presumed GERD and non-GERD patients that are included in studies on pediatric ARS.
Our systematic review further shows that the quality of life has been highly underexposed in the evaluation of pediatric ARS, even though validated QoL questionnaires are available for different age groups and development levels.24 In only one study, QoL questionnaires were performed, showing a significant improvement after ARS.20
Several studies have postulated that NI patients are predisposed to a worse outcome after ARS. But in fact, only two studies6,10 actually compared NI patients with NN patients. These two studies reported conflicting results. Capito et al.6 found a significantly higher recurrence rate in NI patients. Engelmann et al.10, however, demonstrated that NI patients showed relatively more improvement than NN patients. Nevertheless, we have to realize that drawing conclusions on the efficacy of ARS in specific groups, such as NI patients or patients after esophageal atresia is challenging, because of a lack of well-designed prospective comparative studies.
Clinical trials comparing laparoscopic to open ARS in pediatric GERD patients have not been published. However, prospective studies in this systematic review have shown that the results of laparoscopic ARS were not different from those of open ARS with regard to reflux symptoms during short-term follow-up. The main benefits of laparoscopic ARS include a shorter hospital stay and a reduced need for pain medication.5,12 Recently, the New Technology Committee of the American Pediatric Surgery Association published a position paper favoring laparoscopic fundoplication. This advice was, however, based on results from case series and retrospective reviews.25
In only three studies, different types of ARS were compared.8,14,23 Two of these studies compared complete versus partial fundoplication demonstrating less postoperative dysphagia in the partial fundoplication group. Reflux control, on the other hand, was comparable in both groups.14,23 Similar results were demonstrated by a recently published systematic review and meta-analysis on RCTs comparing complete posterior (Nissen) with partial posterior (Toupet) fundoplication in adults.26
Finally, we noticed that following ARS, values of 24-h pH monitoring significantly decreased, LES-pressure seemed to increase, and gastric emptying was either unchanged or accelerated. However, no definite conclusions of the effects of ARS on GE function can be drawn, since too few studies have performed standardized GE function tests and the number of patients included in these studies was too small. Only if GE function tests are consistently performed before and after ARS in a sufficient amount of patients, the effects of ARS on GE function may be clarified. Moreover, these tests may then also provide us with the opportunity to identify prognostic factors for failure of ARS.
In conclusion, ARS in children shows a good overall success rate (median 86%) in terms of complete relief of symptoms. The success rate in NI patients may not be worse compared to NN patients. The outcome of ARS does not seem to be influenced by different surgical techniques, although postoperative dysphagia may occur less after partial fundoplication. The strength of these conclusions is, however, bound by the lack of high-quality prospective studies on pediatric ARS. Similar studies on the effects of pediatric ARS on gastroesophageal function are also very limited. Therefore, future studies should be performed in a well-designed prospective format, either as an RCT comparing different types of ARS, or as a prospective, age- and sex-matched study comparing different patient groups. But, even more crucial is the use of standardized GE function tests to clarify the effects of ARS on GE function and to identify possible risk factors of failure of ARS in children.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Shepherd RW, Wren J, Evans S, Lander M, Ong TH. Gastroesophageal reflux in children. Clinical profile, course and outcome with active therapy in 126 cases. Clin Pediatr (Phila) 1987;26(2):55–60. doi: 10.1177/000992288702600201. [DOI] [PubMed] [Google Scholar]
- 2.Treem WR, Davis PM, Hyams JS. Gastroesophageal reflux in the older child: presentation, response to treatment and long-term follow-up. Clin Pediatr (Phila) 1991;30(7):435–440. doi: 10.1177/000992289103000705. [DOI] [PubMed] [Google Scholar]
- 3.Vandenplas Y. Hiatal hernia and gastro-oesophageal reflux. Management of Digestive and Liver Disorders in Infants and Children, Elsevier Science. 1993. 103–116.
- 4.Vandenplas Y, Rudolph CD, Di LC, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) J Pediatr Gastroenterol Nutr. 2009;49(4):498–547. doi: 10.1097/01.mpg.0000361306.15727.54. [DOI] [PubMed] [Google Scholar]
- 5.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 6.Capito C, Leclair MD, Piloquet H, Plattner V, Heloury Y, Podevin G. Long-term outcome of laparoscopic Nissen-Rossetti fundoplication for neurologically impaired and normal children. Surg Endosc. 2008;22(4):875–880. doi: 10.1007/s00464-007-9603-3. [DOI] [PubMed] [Google Scholar]
- 7.Cheung KM, Tse HW, Tse PWT, Chan KH. Nissen fundoplication and gastrostomy in severely neurologically impaired children with gastroesophageal reflux. Hong Kong Med J. 2006;12(4):282–288. [PubMed] [Google Scholar]
- 8.Durante AP, Schettini ST, Fagundes DJ. Vertical gastric plication versus Nissen fundoplication in the treatment of gastroesophageal reflux in children with cerebral palsy. Sao Paulo Med J. 2007;125(1):15–21. doi: 10.1590/S1516-31802007000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelmann C, Gritsa S, Ure BM. Impact of laparoscopic anterior 270 degrees fundoplication on the quality of life and symptoms profile of neurodevelopmentally delayed versus neurologically unimpaired children and their parents. Surg Endosc. 2010;24(6):1287–1295. doi: 10.1007/s00464-009-0762-2. [DOI] [PubMed] [Google Scholar]
- 10.Engelmann C, Gritsa S, Gratz KF, Ure BM. Laparoscopic anterior hemifundoplication improves key symptoms without impact on GE in children with and children without neurodevelopmental delays. J Pediatr Gastroenterol Nutr. 2010;51(4):437–442. doi: 10.1097/MPG.0b013e3181d1f1c8. [DOI] [PubMed] [Google Scholar]
- 11.Estevâo-Costa J, Fragoso AC, Prata MJ, Campos M, Trindade E, Dias JA et al. Gastric emptying and antireflux surgery. Pediatr Surg Int 2010. [DOI] [PubMed]
- 12.Kawahara H, Imura K, Yagi M, Yoneda A, Soh H, Tazuke Y, et al. Mechanisms underlying the antireflux effect of Nissen fundoplication in children. J Pediatr Surg. 1998;33(11):1618–1622. doi: 10.1016/S0022-3468(98)90593-0. [DOI] [PubMed] [Google Scholar]
- 13.Kawahara H, Imura K, Nakajima K, Yagi M, Kamata S, Okada A. Motor function of the esophagus and the lower esophageal sphincter in children who undergo laparoscopic nissen fundoplication. J Pediatr Surg. 2000;35(11):1666–1671. doi: 10.1053/jpsu.2000.18348. [DOI] [PubMed] [Google Scholar]
- 14.Kubiak R, Andrews J, Grant HW. Laparoscopic nissen fundoplication versus thal fundoplication in children: comparison of short-term outcomes. J Laparoendosc Adv Surg Tech A. 2010;20(7):665–669. doi: 10.1089/lap.2010.0218. [DOI] [PubMed] [Google Scholar]
- 15.Mattioli G, Esposito C, Lima M, Garzi A, Montinaro L, Cobellis G, et al. Italian multicenter survey on laparoscopic treatment of gastro-esophageal reflux disease in children. Surg Endosc. 2002;16(12):1666–1668. doi: 10.1007/s00464-002-9002-8. [DOI] [PubMed] [Google Scholar]
- 16.Mattioli G, Repetto P, Carlini C, Torre M, Pini Prato A, Mazzola C, et al. Laparoscopic vs open approach for the treatment of gastroesophageal reflux in children. Surg Endosc. 2002;16(5):750–752. doi: 10.1007/s00464-001-9040-7. [DOI] [PubMed] [Google Scholar]
- 17.Menon KV, Booth M, Stratford J, Dehn TCB. Laparoscopic fundoplication in mentally normal children with gastroesophageal reflux disease. Dis Esophagus. 2002;15(2):163–166. doi: 10.1046/j.1442-2050.2002.00245.x. [DOI] [PubMed] [Google Scholar]
- 18.Mousa H, Caniano DA, Alhajj M, Gibson L, Di Lorenzo C, Binkowitz L. Effect of Nissen fundoplication on gastric motor and sensory functions. J Pediatr Gastroenterol Nutr. 2006;43(2):185–189. doi: 10.1097/01.mpg.0000228115.14111.24. [DOI] [PubMed] [Google Scholar]
- 19.Soyer T, Karnak I, Tanyel FC, Senocak ME, Ciftci AO. The use of pH monitoring and esophageal manometry in the evaluation of results of surgical therapy for gastroesophageal reflux disease. Eur J Pediatr Surg. 2007;17(3):158–162. doi: 10.1055/s-2007-965393. [DOI] [PubMed] [Google Scholar]
- 20.Srivastava R, Downey EC, Feola P, Samore M, Coburn L, Holubkov R, et al. Quality of life of children with neurological impairment who receive a fundoplication for gastroesophageal reflux disease. J Hosp Med. 2007;2(3):165–173. doi: 10.1002/jhm.167. [DOI] [PubMed] [Google Scholar]
- 21.van der Zee DC, Arends NJ, Bax NM. The value of 24-h pH study in evaluating the results of laparoscopic antireflux surgery in children. Surg Endosc. 1999;13(9):918–921. doi: 10.1007/s004649901134. [DOI] [PubMed] [Google Scholar]
- 22.Weber TR. A prospective analysis of factors influencing outcome after fundoplication. J Pediatr Surg. 1995;30(7):1061–1063. doi: 10.1016/0022-3468(95)90342-9. [DOI] [PubMed] [Google Scholar]
- 23.Weber TR. Toupet fundoplication for gastroesophageal reflux in childhood. Arch Surg. 1999;134(7):717–720. doi: 10.1001/archsurg.134.7.717. [DOI] [PubMed] [Google Scholar]
- 24.Deal L, Gold BD, Gremse DA, Winter HS, Peters SB, Fraga PD, et al. Age-specific questionnaires distinguish GERD symptom frequency and severity in infants and young children: development and initial validation. J Pediatr Gastroenterol Nutr. 2005;41(2):178–185. doi: 10.1097/01.mpg.0000172885.77795.0f. [DOI] [PubMed] [Google Scholar]
- 25.Kane TD, Brown MF, Chen MK. Position paper on laparoscopic antireflux operations in infants and children for gastroesophageal reflux disease. American Pediatric Surgery Association. J Pediatr Surg. 2009;44(5):1034–1040. doi: 10.1016/j.jpedsurg.2009.01.050. [DOI] [PubMed] [Google Scholar]
- 26.Broeders JA, Mauritz FA, Ahmed AU, Draaisma WA, Ruurda JP, Gooszen HG, et al. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2010;97(9):1318–1330. doi: 10.1002/bjs.7174. [DOI] [PubMed] [Google Scholar]