Abstract
Purpose
To examine separate mediational models linking a) menarcheal status or b) pubertal timing to internalizing and externalizing problems through competence.
Method
Cross-sectional analyses of 262 adolescent girls (11–17 years; M=14.93, SD=2.17) enrolled in a longitudinal study examining the association of psychological functioning and smoking with reproductive and bone health. Measures of menarcheal status (pre/post), pubertal timing (early, on-time, or late), internalizing and externalizing behavior, and perceived competence (parent and adolescent report) were obtained. Structural Equation Modeling was used for analyses.
Results
Perceived competence was found to fully mediate the association between menarcheal status and parent report of internalizing and externalizing problems. For adolescent report, there was a full mediation effect for internalizing problems but a partial mediation effect for externalizing problems. Being menarcheal was related to lower competence which was related to higher internalizing and externalizing problems. Models including pubertal timing were not significant.
Conclusions
Perceived competence is important in understanding the associations between menarcheal status and internalizing and externalizing problems. Interventions targeting competence, particularly in post-menarcheal girls, may reduce or prevent problem behaviors.
Keywords: puberty, menarche, competence, internalizing, externalizing
Early pubertal timing is linked with an increase in internalizing and externalizing problems [1–2] while menarcheal status has received less attention. Postmenarcheal girls report more depressive symptoms than premenarcheal girls [3–4], however there are few studies that examined menarche and externalizing problems. Although the extant evidence supports both pubertal timing and menarche as important events that are associated with internalizing and externalizing symptoms, there is little knowledge of the mechanisms explaining these associations. One explanation is the developmental readiness hypothesis. Prior to the pubertal transition, certain adaptive and coping skills must be acquired for an individual to effectively transition from childhood to adolescence. Early maturers have less time to acquire, assimilate, and strengthen these coping skills leading to developmental asynchrony between physical, cognitive, and social maturity that increases risk for psychopathology [5]. Although the majority of the literature on pubertal timing effects finds indirect support for the developmental readiness hypothesis [1, 6–7], none have tested the specific variables that may function as mediators between puberty and symptoms of psychopathology.
One construct that may reflect both cognitive and social maturity/immaturity is competence. In general, competence refers to a pattern of effective adaptation in the environment. Narrowly, it is described in relation to specific domains of achievement such as academics (i.e., school), social (i.e., peer engagement), or physical competence (i.e., physical activities) [8]. Perceived competence is based on an individual’s perception of their competence in different domains, which may affect how they adapt and cope with developmental changes [9]. In the present study we operationalized competence by including competence in academics (parent only), social, and physical domains from the parent and adolescent perspectives. Competence is linked to menarcheal status, depression, and antisocial behavior [10–13], however it has not been tested as a mediator between pubertal development and symptoms of psychopathology.
In order to understand the risks for psychopathology, it is important to evaluate both adaptive and maladaptive developmental trajectories. High competence across multiple domains indicates a normative trajectory in regards to age-salient developmental tasks. Low competence may be associated with symptoms of psychopathology and signify unhealthy adaptation [14]. During pubertal development there are increasing physical, social, and academic demands. If an adolescent is unable to manage these challenges, mood or behavior problems may emerge.
Evidence suggests there are changes in self-perception and competence with the onset of puberty or the attainment of menarche[10, 15]. Most studies have focused on timing of puberty and the association with self-esteem. Although competence is thought to be one component of self-esteem, competence is a more specific construct addressing how an individual is perceived or perceives themselves in various domains [15]. Several studies found postmenarcheal girls at risk for low perceived physical competence [13], and lower scores on physical appearance and athletic competence [10]. No studies have compared how menarcheal status and pubertal timing may differentially relate to competence.
Competence may not only be affected by puberty but may also affect the development of psychopathology. There is more perturbation in self-concept around the time of puberty for females and they may be more likely to feel they have failed to meet their ideal self-concept compared to males [10]. Therefore, females may be at higher risk for disturbances in self-perception and competence along with associated psychopathology. Evidence links competence with both depressive symptoms and antisocial behavior. Studies have found that low academic competence in 1st grade predicted depressive symptoms in 7th grade [16] and similarly, low social competence was associated with higher depressive symptoms [17]. Less literature has focused on competence and externalizing behavior, but studies also find low competence a risk for behavior problems. For example, social competence at age 13 was related to antisocial behavior at age 15 [12] and low academic competence was also associated with antisocial behavior [18].
Competence has been shown to be related to menarcheal status, depression, and antisocial behavior [10–12]. However, no studies have examined competence as a mediator between puberty and symptoms of psychopathology. In addition, there is limited comparison of pubertal timing and menarcheal status in relation to these other variables. Both are crucial to understanding the escalation of internalizing and externalizing problems as status and timing of menarche have different meanings. Status refers to the developmental stage regardless of age, whereas timing refers to attainment of a specific stage at an earlier (or later) age than most peers. Some studies find that the relationship with symptoms of psychopathology[1, 7] are similar for pubertal status and timing while others find that status is more relevant to depressive affect [19]. Therefore, the aims were to examine separate mediational models linking a) menarcheal status or b) pubertal timing to internalizing and externalizing problems via perceived competence.
Methods
Participants
Participants included girls enrolled in a longitudinal study on the effects of smoking and mood on bone and reproductive health (N = 262) [20]. Girls were primarily Caucasian (62.8%) or African American (32.8%). The remaining 5.3% were mixed-race or other race/ethnicities which were combined with the African American girls to create a non-Caucasian group. Enrollment was by age cohort (11, 13, 15, and 17 years; M=14.93, SD=2.17) and smoking behavior. Participants were recruited from an urban teen clinic and the surrounding community. Exclusion criteria: 1) pregnancy or breast feeding within 6 months, 2) primary or secondary amenorrhea, 3) body mass index < the 1st percentile or weight > 300 pounds, 4) medication/medical disorder influencing bone health, and 5) psychological disabilities impairing comprehension or compliance with the protocol (e.g., schizophrenia). Institutional Review Board approval was obtained. Consent and assent were obtained from the parent and adolescent, respectively.
Procedures
Study visits were conducted at a children’s hospital. A physical exam and menstrual history interview were completed by a clinician researcher, followed by psychological questionnaires. Parents completed questionnaires in a separate room.
Measures
Menarcheal Status
The clinician researcher asked the girl whether she ever had a period, “yes” was categorized as “menarcheal” (n = 209) and “no” was categorized as “premenarcheal” (n = 53).
Pubertal Timing
The girl’s report of age at menarche (years, months) was obtained via clinician interview. Prompts were provided to increase accuracy [21]. Early, on-time, and late timing groups were created based on the sample distribution of age at menarche within Caucasian (range 9.17–16.08yrs) and non-Caucasian (range 7.42–15.08) groups in this study. Girls 1 SD or more below the mean (within their racial group), and those 1 SD or more above the mean were coded as early and late-timing, respectively. Remaining girls were coded as on-time [1]. For the Caucasian group the cut-offs for early and late groups were 11.52 and 13.74 years, respectively. For the non-Caucasian group the cut-offs were 10.67 and 13.34 years, respectively.
Perceived Competence
Parent report
Parent report of their child’s competence was measured with the social, activities, and school competence scales of the Child Behavior Checklist (CBCL).
Adolescent report
The activities and social competence scales from the Youth Self Report (YSR) were used. There is no school competence scale for the YSR.
Both the CBCL and YSR ask questions related to sports, organizations, hobbies, jobs, and school performance. Scores are converted to T scores (M=50, SD=10). The Cronbach’s alphas on the social and activities competence scales in the current sample ranged from .58 to .88 which are similar to other studies [22].
Internalizing problems
Parent report
The anxious/depressed (12 items) and withdrawn/depressed (8 items) subscales from the CBCL were used to measure internalizing problems. Parents answer on a three-point scale (0=none, 1=some, 2=a lot) for their child’s behavior in the past 6 months. The Cronbach’s alphas for the anxious/depressed and withdrawn/depressed scales were .81 and .77, respectively.
Adolescent report
The anxious/depressed and withdrawn/depressed scales from the YSR were used as well as the Children’s Depression Inventory (CDI) and the State Trait Anxiety Inventory (STAI and STAIC). The two scales from the YSR have similar items to the parent scales. The YSR sample alphas were .80 and .67.
The CDI is a 27-item, self-report measure that has been used extensively with children and adolescents. Composite T-scores were used. The CDI correlates strongly with other measures of depressive symptoms [23]. The Cronbach’s alpha was .89.
Trait anxiety was determined by the State-Trait Anxiety Inventory (STAI) [24] for those age 12 and above, or the child version for the 11 year-old girls (STAIC) [25]. The Cronbach’s alpha for trait anxiety (20 items) was .88 and .93 for the STAIC and STAI, respectively.
Externalizing Problems
Parent report
The rule-breaking and aggressive behavior subscales of the CBCL were used along with the oppositional defiant symptom count of the Diagnostic Interview Schedule for Children (DISC) [26]. The rule-breaking scale consists of 17 items and the reliability was .84. The aggressive behavior scale contains 18 items and the reliability was .90. T-scores were used.
The DISC is a computerized structured diagnostic interview to assess mental health symptoms and diagnoses. The total symptom count for oppositional defiant disorder (ODD) was used. Scores ranged from 0–12 with a higher score representing more symptomotology.
Adolescent report
Similar to parent report on the CBCL, the youth version on the rule-breaking scale has 15 items and the aggressive behavior scale has 17 items. Reliabilities for rule breaking and aggressive behavior scales were .80 and .83, respectively. The ODD symptom count from the DISC contains items that overlap with the parent report with scores ranging from 0–11.
Covariates
Age, race, socioeconomic status (SES), Tanner breast stage, and mother’s report of ever being anxious/depressed were included as covariates. Tanner breast stage [27] was from a clinician’s assessment. Hollingshead criteria was used to compute SES scores, which ranged from 14–66 (M=37.38, SD=13.63) [28]. A score of 35 equates to working class. Parental depression is correlated with parents’ rating of depression in their children [29] and living with a depressed caregiver increases the child’s risk for internalizing and externalizing problems [30].
Statistical Analysis
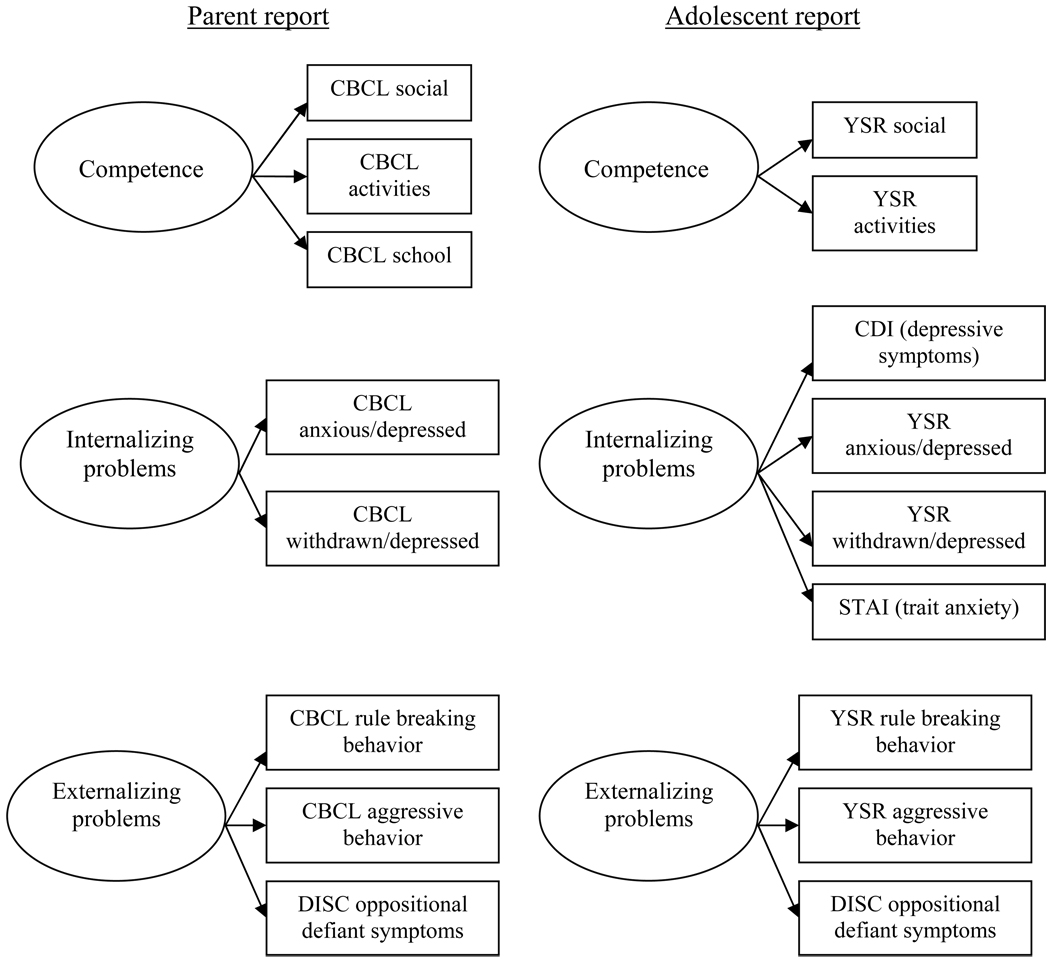
Structural equation modeling was used to examine the aims with Amos 7.0 [31]. Two separate models were tested, one with parent and one with adolescent report. For each reporter, three latent variables were created: competence, internalizing problems, and externalizing problems. The manifest variables composing each latent variable are shown in Figure 1. Covariates for both models included age, race, SES, and mother ever anxious/depressed. For each reporter a mediational model tested the indirect effect of menarcheal status or pubertal timing on internalizing and externalizing behavior through competence Significance of the indirect (mediational) path was computed using Sobel’s test [32].
Figure 1.
Latent variables of competence, internalizing and externalizing problems with manifest variables for parent and adolescent report used in the structural equation models.
Note: CBCL=Child Behavior Checklist; YSR=Youth Self Report; DISC=Diagnostic Interview Schedule for Children; STAI= State Trait Anxiety Inventory; CDI=Children’s Depression Inventory.
Results
Descriptive statistics
Table 1 shows descriptive statistics for the primary study variables by menarcheal status and pubertal timing group. All key variables were normally distributed. An Analysis of Variance (ANOVA) with menarcheal status as the independent variable and age, Tanner breast stage, and SES as the dependent variables revealed significant main effects for all dependent variables (age: F (1, 260) = 222.71, p<.01; Tanner breast: F (1, 260) = 424.17, p<.01; SES: F (1, 259) = 12.23, p<.01). Menarcheal girls were older, had higher Tanner breast stage, and lower SES compared to premenarcheal girls. Additionally menarcheal girls were more likely to be non-Caucasian than premenarcheal girls (OR=3.25; 95% CI=1.55–6.82).
Table 1.
Sample Characteristics and Descriptive Statistics for Study Variables by menarcheal status and pubertal timing group
| Menarcheal status | Pubertal Timing group | ||||
|---|---|---|---|---|---|
| Premenarcheal | Menarcheal | Early | On-time | Late | |
| (n=53) | (n=209) | (n=38) | (n=175) | (n=44) | |
| Age (yrs) | 12.01(.85 | 15.68(1.74) | 15.20(2.04) | 14.79(2.16) | 15.67(2.04) |
| Socioeconomic status | 43.06(13.85) | 35.86(13.67) | 37.30(13.12) | 36.71(14.11) | 39.91(11.45) |
| Percent Caucasian | 81% | 57% | 63% | 61% | 66% |
| Percent with mother ever | |||||
| anxious/depressed (Y/N) | 25% | 35% | 37% | 31% | 41% |
| Competence | |||||
| YSR activities | 45.79(8.60) | 42.17(9.96) | 45.16(9.97) | 42.65(9.55) | 42.84(10.19) |
| YSR social | 48.87(8.88) | 46.35(8.77) | 48.32(7.85) | 46.69(9.09) | 46.30(9.06) |
| CBCL activities | 50.30(7.73) | 41.94(10.66) | 42.47(10.22) | 44.02(11.11) | 42.55(9.58) |
| CBCL social | 49.45(9.29) | 44.48(9.12) | 45.09(9.78) | 45.66(9.21) | 44.68(9.78) |
| CBCL school | 49.83(6.17) | 47.47(7.70) | 48.41(7.32) | 47.65(7.36) | 48.26(8.22) |
| Internalizing problems | |||||
| CDI-depressive symptoms | 42.98(8.16) | 47.13(11.23) | 43.89(7.52) | 46.70(11.25) | 47.14(11.58) |
| Trait anxiety | 41.28(11.18) | 47.67(10.11) | 44.95(8.17) | 46.43(10.89) | 48.52(11.23) |
| YSR anxious/depressed | 52.68(4.48) | 54.70(6.54) | 53.13(4.43) | 54.45(6.55) | 55.00(6.44) |
| YSR withdrawn/depressed | 53.43(5.47) | 56.30(6.57) | 55.89(6.75) | 55.77(6.44) | 55.61(6.47) |
| CBCL anxious/depressed | 53.23(4.52) | 54.20(6.38) | 53.00(4.58) | 54.38(6.46) | 53.34(5.35) |
| CBCL withdrawn/depressed | 53.66(5.07) | 55.97(7.29) | 54.89(6.31) | 55.75(7.13) | 55.23(7.10) |
| Externalizing problems | |||||
| YSR rule breaking | 51.23(2.28) | 59.18(7.11) | 57.71(6.92) | 57.59(7.30) | 58.16(7.11) |
| YSR aggressive behavior | 53.70(4.83) | 59.46(7.82) | 57.37(6.34) | 58.57(7.98) | 58.73(7.61) |
| ODD symptoms-adolescent | |||||
| report | 3.83(2.45) | 5.37(2.98) | 4.89(2.91) | 4.97(2.98) | 5.67(2.95) |
| CBCL rule breaking | 52.42(3.52) | 58.95 (8.05) | 58.14(8.02) | 57.52(8.10) | 58.32(6.62) |
| CBCL aggressive behavior | 53.75(5.37) | 56.50(8.45) | 56.43(6.98) | 55.86(8.72) | 56.27(5.71) |
| ODD symptoms-parent report | 6.25(3.21) | 6.50(3.20) | 6.97(3.04) | 6.22(3.35) | 7.30(2.27) |
Note: YSR= Youth Self Report; CBCL=Child Behavior Checklist; CDI=Children's Depression Inventory; ODD=oppositional defiant disorder from the symptom count of the Diagnostic Interview Schedule for Children; T scores were used for CBCL, YSR and CDI;
ANOVA with pubertal timing as the independent variable and age, Tanner breast stage, and SES as the dependent variables revealed significant main effects for age: F (2, 254) =3.24, p<.05 and Tanner breast: F (2, 254) = 5.84, p<.01 but not for SES: F (2, 253) = .98, p=.38. Post hoc tests (Dunnet’s T3) revealed the late maturing group was older than the on-time group but not different from the early group. For Tanner breast stage the early timing group was significantly more mature than the late timing group (Table 1).
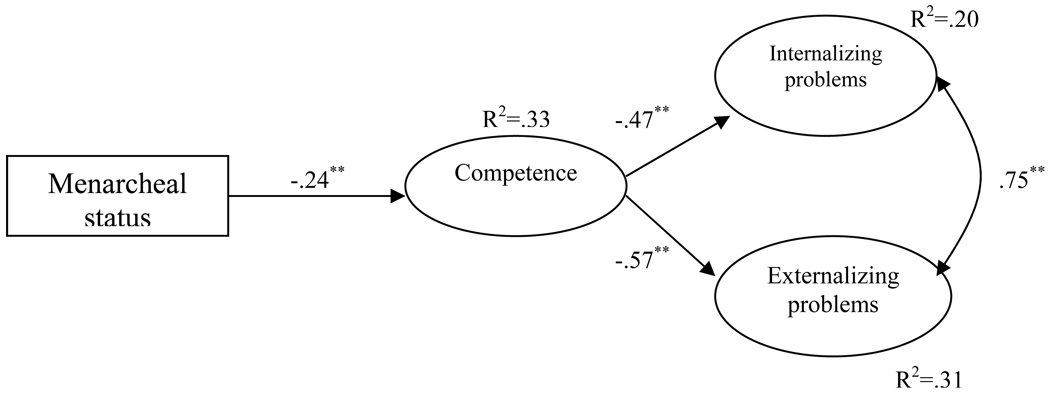
Mediation Models: Menarcheal Status
Parent report
The mediational model with the parent report of competence and behavior problems (Figure 2) fit the data adequately (χ2 =100.18 (29); RMSEA=.09; CFI=.92). There was a significant indirect effect of menarcheal status on internalizing (Sobel’s z = 2.92, p<.01) and externalizing (Sobel’s z = 3.09, p<.01) problems through competence. Being menarcheal was related to lower competence (β = −.24, p<.01) and lower competence was related to higher internalizing (β = −.47, p<.01) and externalizing (β = −.57, p<.01) problems. The model fit did not significantly improve with the addition of direct effects from menarcheal status to internalizing and externalizing problems (χ2Δ= 1.1 (2), ns) indicating that the full mediation model was a better explanation of the data (Figure 2).
Figure 2.
Full mediation model with parent reported competence, internalizing and externalizing problems.
Note: manifest variables and covariates (age, race, SES, mother ever anxious/depressed) are omitted for simplicity of presentation; **p<.01
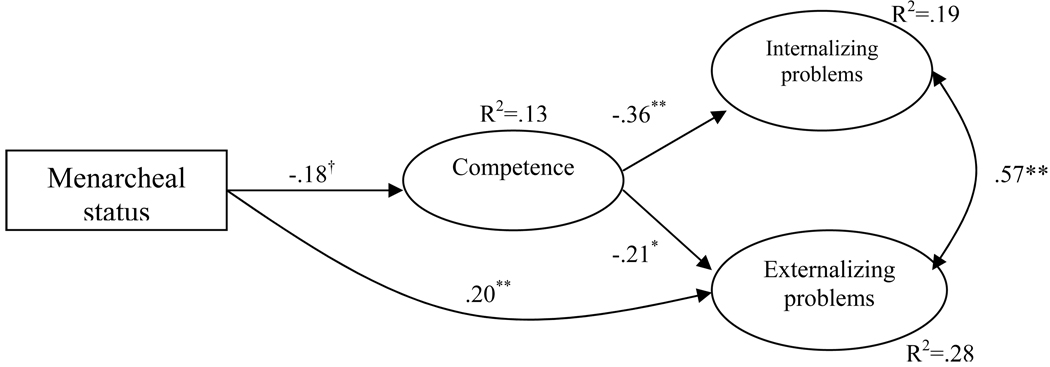
Adolescent report
The mediational model with the adolescent’s report of competence and behavior problems (Figure 3) fit the data adequately (χ2 =155.67 (58); RMSEA=.08; CFI=.92). There was a marginally significant indirect effect of menarcheal status on internalizing problems (Sobel’s z = 1.66, p=.09), however there was not a significant indirect effect for externalizing problems (Sobel’s z = 1.55, p=.12). The inclusion of the path from menarcheal status to externalizing problems significantly improved the model fit (partial mediation). Therefore, the final model included a full mediation effect between menarcheal status and internalizing problems through competence but a partial mediation effect for menarcheal status to externalizing problems (χ2 =148.78 (57); RMSEA=.07; CFI=.93). Similar to the parent report model, being menarcheal was related to lower competence (β = −.18, p=.06) which was related to higher internalizing (β = −.36, p<.01) and externalizing problems (β = −.21, p<.05). In addition, there was a significant main effect of menarcheal status on externalizing problems with the menarcheal girls reporting more externalizing problems (β = −.20, p<.01) (Figure 3).
Figure 3.
Model with full mediation of menarcheal status to internalizing problems and partial mediation of externalizing problems
Note: manifest variables and covariates (age, race, SES, mother ever anxious/depressed) are omitted for simplicity of presentation; †p<.10, *p<.05, **p<.01
Mediation Models: Pubertal Timing Group
Parent report
The mediational model with the parent report of competence and behavior problems fit the data adequately (χ2 =68.49 (29); RMSEA=.07; CFI=.96). However there was no direct effect of pubertal timing on competence. Direct paths from pubertal timing to internalizing and externalizing problems did not improve the model fit (χ2Δ= .003 (2), ns) and the parameter estimates were not significant.
Adolescent report
The mediational model with the adolescent’s report of competence and behavior problems fit the data adequately (χ2 =143.79 (58); RMSEA=.07; CFI=.92). Similar to the parent model there was not a significant effect of pubertal timing group on competence. When the partial mediation model was tested there was not a significant improvement in model fit (χ2Δ= .54 (2), ns), nor were there significant effects of pubertal timing on internalizing or externalizing problems.
Discussion
This study examined mediational models linking puberty to internalizing and externalizing problems through perceived competence. Separate models were analyzed for both menarcheal status and pubertal timing, where the former received support for mediation. Specifically, for the model with parental report of competence and behavior problems, competence fully mediated the association between menarcheal status and both internalizing and externalizing problems. Menarcheal girls had lower competence which was related to more internalizing and externalizing problems. Interestingly, for the adolescent’s report, the mediational model differed slightly. There was a full mediation trend for internalizing problems, with menarcheal girls having lower competence which was related to more internalizing problems. However, for externalizing problems in addition to the indirect effect, there was also a significant direct effect of menarcheal status on externalizing problems.
Although the parent and adolescent report models might differ, we cannot directly compare the parameter estimates or model fit. We can only conclude that the models are the best fitting to the respective data. This information still provides an interesting difference in parent versus adolescent reports of competence and symptomotology. For parents, low competence of their children explained the association between menarcheal status and both internalizing and externalizing problems. However for adolescents, low competence only explained part of the association between menarcheal status and externalizing problems. This may be due to the differences in how each reporter views the adolescent’s externalizing behavior. Parents may combine externalizing problems and competence into an amorphous construct of poor competence and acting out behavior, not necessarily distinguishing between them, whereas the adolescent may separate their perceived competence from their behavior. Alternatively, parents who think their child has low competence may be more likely to view behavior problems as more severe. Parents and adolescents have been found to differ in reports of behavior problems, depression, and competence [33]. Another potential reason for the differences in the findings is that there may be differences in the raters’ expectation about normal competence for that age and stage in development.
It is noteworthy that there were associations between menarcheal status and competence as well as behavior problems, but those same associations did not emerge with pubertal timing. This implies that the transition from pre-menarcheal to menarcheal may affect competence and psychopathology whereas the age at which a girl makes this transition is irrelevant. According to the developmental readiness hypothesis the girl who enters menarche earlier should be at higher risk for psychopathology because she is cognitively and socially more immature than a girl who enters menarche at an older age. However, our results do not support this supposition and instead find that there is a disruption in competence and increased symptoms of psychopathology after menarche.
Menarcheal status is a dichotomous variable that does not capture time since menarche. Menarche may be more immediately disruptive with the effects diminishing after time has passed. However, when we examined the gynecologic age of the girls (number of years since menarche) we found no effect on competence or internalizing or externalizing problems. This indicates that simply the attainment of menarche is associated with a lower competence which is related to higher internalizing and externalizing behavior. However, there was limited range in gynecologic age because the oldest participant was 17 years old. If the sample were older, perhaps we would see an effect of gynecologic age. Evidence shows that the effects of puberty do diminish as the adolescent enters young adulthood [34].
The absence of an association between pubertal timing and internalizing and externalizing problems is in opposition to the bulk of the literature that finds early timing to be detrimental for girls [1, 35]. Numerous studies have found that early timing is associated with depression, antisocial behavior, delinquency, and violent behavior [36–37]. The difference between previous findings and ours may be due in part to the wide age range of the sample which covers early, mid, and late adolescence. The incongruence may be tied to the methods used to construct the pubertal timing variable. We used age at menarche whereas other studies have used Tanner stages or the Pubertal Development Scale. Menarche is a relatively late event in the pubertal process and timing of menarche may have different implications than timing of breast development. Additionally, studies that use timing of breast development relative to peers are assessing the impact of an outward sign of pubertal development compared to use of menarche which is a relatively private and socially unrecognized event among adolescents.
There is little research on puberty-associated changes in competence; studies have primarily focused on body image and self-esteem. According to our results the attainment of menarche is associated with low competence as indicated by both parent and adolescent reports. One implication is that menarcheal girls may see themselves as adult-like and subsequently are not able to measure up to adult standards, resulting in decreased perceived competence. Around menarche girls may experience inconvenience, ambivalence, and confusion [38] which may result in lowered self-perceptions of competence. Parents may see their daughter’s attainment of menarche as a marker of womanhood and report them to have lower competence because they have not yet achieved the skills of adulthood. With menarche comes a redefinition of the adolescent’s role in society and expectations about their responsibilities [38]. It is likely both the parent and adolescent are confused by this event which may influence their perceptions of competence and symptoms of psychopathology.
There are several limitations of the current study. First, our analyses were cross-sectional and therefore we cannot draw causal inferences regarding mediation. Second, although the literature supports categorical pubertal timing measures based on the sample distribution, creating artificial cut points and unequal cell sizes can reduce the power to detect significant effects. Additionally, we used latent constructs of competence, internalizing and externalizing behavior which may limit the understanding of more specific problems such as depression or aggressive behavior. However, the advantage of latent constructs is that they account for measurement error inherent in just one scale. Lastly, although the CBCL/YSR have been used in other studies to assess perceived competence [39], these measures are not as comprehensive as a direct interview to assess competence and could result in different patterns of associations.
Overall, we find that competence is an important consideration in understanding associations between menarcheal status and internalizing and externalizing problems. Future research should examine longitudinal associations between these variables. There may be reciprocal relationships between competence and internalizing and externalizing problems. Studies have found that across 10 years, low social competence predicted an increase in internalizing problems which was subsequently predicted an increase in externalizing problems [40]. Furthermore, how puberty may affect these reciprocal relationships is unknown. Clinically, our findings provide a potential target for intervention programs to treat internalizing and externalizing disorders by addressing adolescent competence. For example, a post-menarcheal adolescent female with depression might benefit from targeted behavioral therapy to improve competence as a component of treatment. Therefore interventions could target competence, particularly for post-menarcheal adolescents, in order to reduce or prevent symptoms of psychopathology.
Acknowledgments
This work was supported by the National Institute of Drug Abuse (Grant Number R01 DA 16402) to Lorah Dorn, PI.; the National Center for Research Resources (USPHS Grant # UL1RR026314); and National Research Service Award Training Grant 1T32PE10027 from the National Institutes of Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ge X, Brody GH, Conger RD, et al. Pubertal maturation and African American children’ s internalizing and externalizing symptoms. Journal of Youth and Adolescence. 2006;35(4):531–540. [Google Scholar]
- 2.Graber JA, Lewinsohn PM, Seeley JR, et al. Is psychopathology associated with the timing of pubertal development? Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(12):1768–1776. doi: 10.1097/00004583-199712000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Hayward C, Gotlib IH, Schraedley PK, et al. Ethnic differences in the association between pubertal status and symptoms of depression in adolescent girls. Journal of Adolescent Health. 1999;25:143–149. doi: 10.1016/s1054-139x(99)00048-8. [DOI] [PubMed] [Google Scholar]
- 4.Capron C, Therond C, Duyme M. Brief report: effect of menarcheal status and family structure on depressive symptoms and emotional/behavioural problems in young adolescent girls. Journal of Adolescence. 2007 Feb;30(1):175–179. doi: 10.1016/j.adolescence.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Ge X, Natsuaki NM. In search of explanations for early pubertal timing effects on developmental psychopathology. Current Directions in Psychological Science. 2009;18(6):327–331. [Google Scholar]
- 6.Lynne SD, Graber JA, Nichols TR, et al. Links between pubertal timing, peer influences, and externalizing behaviors among urban students followed through middle school. Journal of Adolescent Health. 2007;40(2) doi: 10.1016/j.jadohealth.2006.09.008. 181.e187-181.e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge X, Brody GH, Conger RD, et al. Contextual amplification of pubertal transition effects on deviant peer affiliation and externalizing behavior among African American children. Developmental Psychology. 2002;38(1):42–54. doi: 10.1037//0012-1649.38.1.42. [DOI] [PubMed] [Google Scholar]
- 8.Masten AS, Coatsworth JD, Neemann J, et al. The structure and coherence of competence from childhood through adolescence. Child Dev. 1995 Dec;66(6):1635–1659. [PubMed] [Google Scholar]
- 9.Romer D, Walker EF. Adolescent psychopathology and the developing brain: Integrating brain and prevention science. New York: Oxford University Press; 2007. [Google Scholar]
- 10.O'Dea JA, Abraham S. Association between self-concept and body weight, gender, and pubertal development among male and female adolescents. Adolescence. 1999 Spring;34(133):69–79. [PubMed] [Google Scholar]
- 11.Dallaire DH, Cole DA, Smith TM, et al. Predicting children's depressive symptoms from community and individual risk factors. Journal of Youth and Adolescence. 2008 Aug;37(7):830–846. doi: 10.1007/s10964-008-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sorlie M, Hagen KA, Ogden T. Social competence and antisocial behavior: Continuity and distinctiveness across early adolescence. Journal of Research on Adolescence. 2008 Mar;18(1):121–144. [Google Scholar]
- 13.Craft LL, Pfeiffer KA, Pivarnik JM. Predictors of physical competence in adolescent girls. Journal of Youth and Adolescence. 2003 Dec;32(6):431–438. [Google Scholar]
- 14.Masten AS, Coatsworth JD, Neeman J, et al. The structure and coherence of competence from childhood through adolescence. Child Development. 1995;66(6):1635–1659. [PubMed] [Google Scholar]
- 15.Gullotta TP, Adams GR, Montemayor R. Developing social competency in adolescence. Newbury Park: Sage Publications; 1990. [Google Scholar]
- 16.Herman KC, Lambert SF, Reinke WM, et al. Low academic competence in first grade as a risk factor for depressive cognitions and symptoms in middle school. Journal of Counseling Psychology. 2008 Jul;55(3):400–410. doi: 10.1037/a0012654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kistner JA, David-Ferdon CF, Lopez CM, et al. Ethnic and sex differences in children's depressive symptoms. Journal of Clinical Child and Adolescent Psychology 2007. 2007;36(2):171–181. doi: 10.1080/15374410701274942. [DOI] [PubMed] [Google Scholar]
- 18.Vermeiren R, Bogaerts J, Ruchkin V, et al. Subtypes of self-esteem and self-concept in adolescent violent and property offenders. Journal of Child Psychology and Psychiatry. 2004 Feb;45(2):405–411. doi: 10.1111/j.1469-7610.2004.00231.x. [DOI] [PubMed] [Google Scholar]
- 19.Angold A, Costello EJ, Worthman CM. Puberty and depression: the roles of age, pubertal status and pubertal timing. Psychological Medicine. 1998;28(1):51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- 20.Dorn LD, Susman EJ, Pabst S, et al. Association of depressive symptoms and anxiety with bone mass and density in ever-smoking and never-smoking adolescent girls. Arch Pediatr Adolesc Med. 2008 Dec;162(12):1181–1188. doi: 10.1001/archpedi.162.12.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorn LD, Dahl RE, Woodward HR, et al. Defining the boundaries of early adolescence: a user's guide to assessing pubertal status and pubertal timing in research with adolescents. Applied Developmental Science. 2006;10(1):30–56. [Google Scholar]
- 22.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children Youth and Families; 2001. [Google Scholar]
- 23.Kovacs M. Child Depression Inventory Manual. Toronto: Multi-Health System; 1992. [Google Scholar]
- 24.Spielberger CD, Gorusch RL, Lushene RE. STAI Manual. Palo Alto, CA: Consulting Psychologist Press; 1970. [Google Scholar]
- 25.Spielberger CD. Preliminary manual for the State-Trait Anxiety Inventory for Children (“How I Feel Questionnaire“) Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- 26.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children, version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Marshall WA, Tanner JM. Variations in Patterns of pubertal changes in girls. Archives of Disease in Childhood. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hollingshead AF. Four Factor Index of Social Status: Manual. New Haven, CT: Department of Sociology, Yale University; 1976. [Google Scholar]
- 29.Friedlander S, Weiss DS, Traylor J. Assessing the influence of maternal depression on the validity of the Child Behavior Checklist. Journal of Abnormal Child Psychology. 1986 Mar;14(1):123–133. doi: 10.1007/BF00917228. [DOI] [PubMed] [Google Scholar]
- 30.Lovejoy MC, Graczyk PA, O'Hare E, et al. Maternal depression and parenting behavior: a meta-analytic review. Clinical Psychology Review. 2000 Aug;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 31.Arbuckle JL. Amos 7.0 [Computer software] Spring House, PA: Amos Development Corporation; 2006. Computer software. [Google Scholar]
- 32.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- 33.Hope TL, Adams C, Reynolds L, et al. Parent vs. self report: Contribution toward diagnosis of adolescent psychopathology. Journal of Psychopathology and Behavioral Assessment. 1999;21(4):349–363. [Google Scholar]
- 34.Natsuaki NM, Biehl MC, Ge X. Trajectories of depressed mood from early adolescence to young adulthood: The effects of pubertal timing and adolescent dating. Journal of Research on Adolescence. 2009;19(1):47–74. [Google Scholar]
- 35.Hayward C, Killen JD, Wilson DM, et al. Psychiatric risk associated with early puberty in adolescent girls. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(2):255–262. [PubMed] [Google Scholar]
- 36.Ge X, Kim IJ, Brody GH, et al. It's about timing and change: pubertal transition effects on symptoms of major depression among African American youths. Developmental Psychology. 2003;39(3):430–439. doi: 10.1037/0012-1649.39.3.430. [DOI] [PubMed] [Google Scholar]
- 37.Susman EJ, Dockray S, Schiefelbein VL, et al. Morningness/eveningness, morning-toafternoon cortisol ratio, and antisocial behavior problems during puberty. Developmental Psychology. 2007 Jul;43(4):811–822. doi: 10.1037/0012-1649.43.4.811. [DOI] [PubMed] [Google Scholar]
- 38.Ruble DN, Brooks-Gunn J. The experience of menarche. Child Development. 1982;53(6):1557–1566. [PubMed] [Google Scholar]
- 39.Vaisto T, Aronen ET, Simola P, et al. Psychosocial symptoms and competence among adolescents with inflammatory bowel disease and their peers. Inflammatory Bowel Diseases. 2010;16(1):27–35. doi: 10.1002/ibd.21002. [DOI] [PubMed] [Google Scholar]
- 40.Burt KB, Obradovic J, Long JD, et al. The interplay of social competence and psychopathology over 20 years: testing transactional and cascade models. Child Development. 2008 Mar–Apr;79(2):359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]