Abstract
Background:
Nicotine dependence is associated with considerable morbidity and mortality. Two predominant classification systems, the Diagnostic and Statistical Manual (DSM-IV) and Fagerström Test for Nicotine Dependence (FTND), have been used to measure liability to nicotine dependence, yet few studies have attempted to simultaneously examine both sets of criteria.
Methods:
Using a sample of 624 regular smoking individuals who are offspring of Vietnam Era Twin fathers ascertained for an offspring of twin study, we applied latent class analysis to the 7 DSM-IV and the 6 FTND criteria to classify individuals by their nicotine dependence symptom profiles. Post-hoc across-class comparisons were conducted using a variety of smoking-related variables and aspects of psychopathology. Whether a single class identified offspring at high genetic and environmental vulnerability was also investigated.
Results:
The cross-diagnosis kappa was .30. A 4-class solution fit these data best. The classes included a low DSM-low FTND class and a high DSM-high FTND class; a moderate DSM-moderate FTND class, which was distinguished by moderate levels of smoking and intermediate levels of comorbid psychopathology; and a light smoking–moderate FTND class consisting primarily of lighter smokers with a more recent onset of regular smoking. High genetic and environmental vulnerability to nicotine dependence was noted in all classes with no statistically significant across-class differences.
Conclusions:
In general, the DSM-IV and FTND criteria performed similarly to define a continuum of risk for nicotine dependence. The emerging class of light smokers should be further investigated to assess whether they transition to another class or remain as such.
Introduction
Nicotine dependence is strongly correlated with persistent smoking, the leading contributor to preventable death in the United States (Centers for Disease Control, 2002). While the public health implications of nicotine dependence are clear (Mackay, Eriksen, & Shafey, 2006), the measurement of liability to nicotine dependence is actively debated (Hughes, 2006). Several diagnostic tools for the measurement of nicotine dependence exist—the most widely used are the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991) and the Diagnostic and Statistical Manual (DSM-IV; American Psychiatric Association, 1994) criteria for nicotine dependence.
The FTND consists of six items assessing aspects of smoking during the period of heaviest smoking, such as smoking when ill or smoking in places where it is prohibited. Two FTND items, time to first cigarette and cigarettes per day (CPD), comprise a subscale known as the Heaviness of Smoking Index (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989). The FTND was adapted from the Fagerström Tolerance Questionnaire (Fagerström, 1978) and has been shown to correlate highly with biochemical dependence. A score of 4 (from a scale ranging from 0 to 10) or greater on the FTND is considered to be indicative of nicotine dependence.
Nicotine dependence is assessed using seven criteria in the DSM (version IV)—these criteria are generically applied across all drug classes (e.g., alcohol, cannabis) with some smoking-related specificity as needed (e.g., chain smoking as an indicator of spending a great deal of time using the substance). The DSM-IV definition of nicotine dependence requires the endorsement of three or more of seven criteria clustering within a 12-month period.
A conceptual challenge in the measurement of nicotine dependence is that FTND and DSM-IV nicotine dependence do not overlap to a significant extent—individuals with DSM-IV nicotine dependence do not uniformly meet criteria for FTND-based nicotine dependence or vice versa (Hughes et al., 2004). In the general population (Brook, Koppel, & Pahl, 2009; Hughes et al., 2004) and in enriched/clinic samples (Moolchan et al., 2002; Strong, Brown, Ramsey, & Myers, 2003), this low concordance is reflected by kappas of .3 and lower. Furthermore, studies show that DSM-based assessments of nicotine dependence more frequently correlate with psychopathology, such as major depression (Breslau & Johnson, 2000), while the FTND is more closely related to tobacco liking (Moolchan, Aung, & Henningfield, 2003; Strong et al., 2003).
Despite the limited overlap across these two popular assessments, few studies have attempted to simultaneously analyze DSM-IV and FTND criteria to examine whether they characterize smokers in a similar or different manner. As noted, individuals with DSM-IV nicotine dependence do not systematically meet criteria for FTND-based nicotine dependence (and vice versa). By examining both sets of criteria simultaneously we can better understand endorsement of criteria across these two constructs. Importantly, this can demonstrate the synergy across the two assessments in providing comprehensive information on how common and specific aspects of the two assessments work in tandem to produce vulnerability to nicotine dependence. Thus, the goals of this study are (a) to utilize self-reported DSM-IV and FTND criteria to classify individuals using latent class analysis; (b) to examine sociodemographic, smoking-related, and other psychiatric correlates of each class; and (c) to contrast the latent classes in terms of latent genetic and environmental vulnerability.
Materials and Methods
Sample
Data for this study come from 624 adolescent/young adult offspring of Vietnam Era Twins who were regular cigarette smokers. Fathers were members of the Vietnam Era Twin Registry (VETR; Eisen, True, Goldberg, Henderson, & Robinette, 1987; Goldberg, True, Eisen, Henderson, & Robinette, 1987; Henderson et al., 1990), which is a national registry of male like–sex twin pairs in which both cotwins served in the military during the Vietnam Era (1965–1975). Construction of the registry and method of determining zygosity have been previously reported (Eisen et al., 1987). In 1987, twins were first surveyed about their general health including number of offspring fathered by them. In 1992, twins were interviewed by telephone with the Diagnostic Interview Schedule (Robins, Helzer, Cottler, & Goldring, 1988). In 2001 and 2004, respectively, data collection was initiated for two offspring of twins (OOT) studies, which aimed to examine outcomes in the children of VETR twin fathers who (a) were concordant or discordant for alcohol dependence (AD, Project 1) or (b) were concordant or discordant for illicit drug dependence (DD, Project 2), along with (c) unaffected control twin pairs. Both OOT projects used an adaptation of the Semi-Structured Assessment for the Genetics of Alcoholism (Bucholz et al., 1994) to collect data from mothers and offspring. For both projects, biological or custodial mothers (e.g., step mothers) were eligible to participate if twins provided permission to contact them. Offspring were eligible to participate if the VETR twin father and biological and/or custodial mothers gave permission to contact them (In Project 2, permission was granted by the VETR twin father). Parents provided written consent for their minor-aged offspring to be interviewed. Due to the nature of data collection, there was some overlap of participants across the two studies—for these participants, the more recently conducted Project 2 data were used.
Experienced staff from the Institute for Survey Research at Temple University conducted data collection. Interviewers were blind to the substance use history of twin father respondents and gave equal effort to recruitment of all respondents. All participants gave verbal consent prior to being interviewed, as approved by the institutional review boards at the participating institutions. Descriptions of survey contents, response rates, and predictors of nonresponse have been previously published (Duncan et al., 2008; Jacob et al., 2003; Scherrer et al., 2004). A total of 1,919 offspring aged 12–32 years completed the interviews. Of these, 32.5% (N = 624, aged 14–31 years) reported regular smoking (self-report of having smoked 21 or more cigarettes over the lifetime and smoking 3 or more times per week for a minimum of three weeks).
Measures
Latent class analyses (LCA) were conducted on the seven DSM-IV nicotine dependence criteria (tolerance, withdrawal, larger/longer, persistent desire/inability to quit/cut back, great deal of time spent, give up activities, and continued use despite physical/psychological problems) and on the six FTND criteria (time to first cigarette, CPD, smoking where prohibited, hate to give up first cigarette of the day, smoking when ill in bed, and smoking more within the first hour of waking). FTND criteria were specifically assessed for the period when the respondent was “smoking the most,” while DSM-IV criteria were assessed across the lifetime. With the exception of time to first cigarette and CPD, all other criteria were coded dichotomously. In the FTND, time to first cigarette is coded as 0 = after 60 min, 1 = 31–60 min, 2 = 6–30 min, and 3 = within 5 min of waking, while CPD is coded as 0 = 10 or less, 1 = 11–19, 2 = 20–25, and 3 = 26 or more. As LCA can accommodate categorical measures and they increase our ability to disentangle classes of individuals, we retained these two measures in their ordinal form. However, for illustrative purposes, only the highest category is depicted in some instances.
Note that our definition of DSM-IV tolerance does include elements of CPD—however, our definition of tolerance was broader (including items on smoking a lot more in order to get what you wanted out of smoking or smoking 20 or more CPD during lifetime). Hence, both tolerance and CPD were included in analyses, although all participants who did not report tolerance were also missing for CPD ≥2.
Correlates
Several sociodemographic and psychiatric measures were used along with measures related to smoking to examine differences between the classes identified in the LCA. These measures are described in Table 2.
Table 2.
Multinomial Odds Ratios and Mean Differences Showing the Association Between Sociodemographic, Psychiatric, and Smoking-Related Measures Across Classes of Individuals (using the low DSM-low FTND class as the reference class) Identified Using DSM-IV and FTND Criteria for Nicotine Dependence
| High DSM-high FTND (N = 177) | Moderate DSM-moderate FTND (N = 167) | Lighter smokers–moderate FTND (N = 117) |
|
| Sociodemographics | |||
| Age < 22 years | 0.72 (0.46–1.11) | 0.67 (0.43–1.05) | 1.11 (0.68–1.80) |
| Male | 2.20 (1.42–3.41)*a | 2.50 (1.61–3.91)*a | 2.63 (1.61–4.30)*a |
| Caucasian | 1.28 (0.64–2.57) | 1.15 (0.57–2.33) | 1.40 (0.62–3.20) |
| Smoking-related outcomes | |||
| Onset of smoking prior to 13 years | 3.45 (2.06–5.80)*a | 1.88 (1.10–3.22)*b | 2.14 (1.20–3.82)*a,b |
| DSM-IV symptom count (0–7) (across-class difference)c | 6.15 (5.76–6.54)* | 2.59 (2.19–2.98)* | 2.84 (2.40–3.27)* |
| DSM-IV nicotine dependence | 23.01 (11.01–48.15)* | 13.78 (6.58–28.88)* | 3.80 (1.67–8.64)* |
| FTND symptom count (0–11) (across-class difference)c | 3.13 (2.84–3.42)* | 2.12 (1.83–2.42)*a | 1.14 (0.81–1.46)*a |
| Current smoking (including smoking a cigarette in the past month) | 2.66 (0.98–7.23) | 1.60 (0.68–3.76) | 1.32 (0.54–3.27) |
| Years since onset of regular smoking (across-class difference)c | 2.36 (1.38–3.37)*a | 1.40 (0.41–2.40)*a | 0.14 (−0.95–1.23) |
| Maximum cigarettes smoked in 24 hr (across-class difference)c | 21.91 (18.53–25.30)*a | 20.14 (16.71–23.58)*a | 4.81 (1.03– 8.59)* |
| Strong urge or craving after stopping or cutting down smoking | 1.81 (1.58–2.07)* | 1.36 (1.20–1.55)*a | 1.38 (1.20–1.59)*a |
| Respondent report of current peer smoking | 2.45 (1.80–3.32)*a | 1.90 (1.42–2.56)*a | 1.26 (0.92–1.71) |
| Other psychopathology | |||
| Conduct disorder (self-report) | 4.77 (2.79–8.17)* | 1.80 (1.02–3.19)*a | 2.17 (1.19–3.95)*a |
| ADHD problems (via maternal report) | 2.16 (1.16–4.02)*a | 1.34 (0.70–2.59) | 2.18 (1.12–4.25)*a |
| DSM-IV alcohol abuse/dependence | 1.85 (1.51–2.27)*a | 1.63 (1.32–2.00)*a | 1.18 (0.93–1.47) |
| DSM-IV marijuana abuse/dependence | 1.63 (1.26–2.11)* | 1.28 (0.98–1.69) | 1.11 (0.83–1.51) |
| Major depressive disorder | 1.21 (1.08–1.36)*a | 1.14 (1.01–1.28)*a | 0.98 (0.85–1.13) |
| Generalized anxiety disorder | 1.88 (0.94–3.76) | 0.77 (0.33–1.76) | 0.61 (0.22–1.67) |
| Panic disorder | 1.81 (1.24–2.59)* | 1.13 (0.75–1.71) | 1.12 (0.71–1.77) |
Note. a,b odds ratios with the same alphabetical superscript could be equated to each other (across the columns/classes only). DSM-IV = Diagnostic and Statistical Manual; FTND = Fagerstrom Test for Nicotine Dependence.
*Statistically significant at p < .05.
Tested using analysis of variance.
OOT Study Design
The original studies selected cases on the basis of the twin father’s alcohol or DD status. According to this design, offspring were designated to be at:
High genetic and high environmental risk if the father of the offspring had AD or DD.
High genetic and low environmental risk if the father of the offspring was unaffected, but his identical cotwin (who shares 100% of his genes identical-by-descent) had a diagnosis of AD or DD.
Intermediate genetic and low environmental risk if the father of the offspring was unaffected, but his fraternal cotwin (who shares 50% of his genes identical-by-descent) had a diagnosis of AD or DD.
Low genetic and low environmental risk, where irrespective of zygosity, both the father and his cotwin are unaffected.
From the baseline interviews, coded using DSM-III-R (American Psychiatric Association, 1987) criteria, a diagnosis of nicotine dependence (ND) was made for the father and his cotwin. While the study was not ascertained for nicotine dependence risk, based on the nicotine dependence diagnoses in the father and uncle, a comparable nicotine four-group variable was also created and used. Thus, if the biological father (irrespective of whether he was part of the AD or DD project) met criteria for DSM-III-R ND, then the offspring was classified to be at high genetic and high environmental risk. Likewise, if the father was unaffected but the MZ (Monozygotic, identical) uncle met criteria for DSM-III-R ND, then the offspring was classified to be at high genetic and low environmental risk and so on.
Latent Class Analyses
Latent class analysis (McCutcheon, 1987), a form of nonparametric cluster analysis, can be used to identify classes of individuals with similar phenotypic profiles. LCA utilizes responses to categorical data to empirically assign class membership to individuals. Individuals are assigned to the most likely class, and results are characterized by (a) the prevalence of each class and (b) the probability that an individual in a certain class will endorse a certain item (“conditional probability”). The modeling strategy assumes conditional independence (i.e., no additional covariation across items except that attributable to the latent classes); however, methods for relaxing this assumption exist. We used MPlus (version 5.1; L. K. Muthen & Muthen, 2007) to conduct LCA (under the assumption of conditional independence) in the 624 regular smokers. As some of the offspring were related, the robust maximum likelihood estimator was used to adjust standard errors. Selection of the number of latent classes that optimally described our data was done using the Bayesian information criterion (BIC; Raftery, 1995) along with entropy. BIC was preferred over other fit indices as it is particularly suited to LCA (B. O. Muthén & Muthén, 2000). Resulting assignments to latent classes were extracted and analyzed, post-hoc, in SAS (SAS Institute, 1999) and STATA (Stata Corp, 2003). As we were interested in examining the extent to which offspring at high genetic and/or high environmental risk (due to the OOT design) were represented in each class, the LCA were not adjusted for study design.
Characterizing Individuals in Classes
Multinomial logistic regression in STATA, with a robust variance estimator, was used to examine the association between latent class membership and sociodemographic, psychiatric, and other smoking-related measures. The class representing least risk was used as the reference class, and a Wald chi-square comparison was conducted to examine differences across the remaining classes. SAS was used to process data and to compute frequencies. To avoid any confounding effects of the study design (described above), all multinomial logistic models were adjusted for dummy variables representing the study design, with separate variables representing drug- and alcohol-related risk.
Characterizing Genetic and Environmental Risk Across Classes
A four-group variable representing genetic and environmental risk attributable to a paternal history of nicotine dependence was examined to identify whether members of any class showed an over-representation of high genetic and/or environmental risk.
Results
Simply cross-tabulating a DSM-IV diagnosis of nicotine dependence (three or more criteria clustering in a 12-month period) with an FTND (four or more symptoms) diagnosis resulted in a correlation of .50 (κ = .30).
Latent Class Analysis
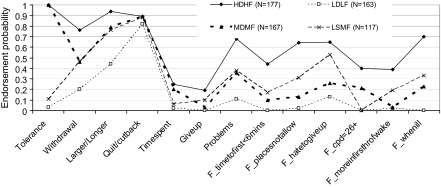
Using the BIC fit indices, a four-class solution fit these data well (Akaike’s information criterion [AIC] = 9729.1, BIC = 10044.1, and Entropy = .80). The three-class (AIC = 9846.2, BIC = 10081.3, and Entropy = .81) and five-class solution (AIC = 9679.3, BIC = 10074.06, and Entropy = .80) did not fit as well as the four-class solution. Figure 1 illustrates the pattern of endorsement probabilities and prevalence of each of the four classes.
Figure 1.
Endorsement probabilities of DSM-IV and FTND criteria in 624 regular smokers. HDHF = high DSM-high FTND; MDMF = moderate DSM-moderate FTND; LDLF = low DSM-low FTND; and LSMF = lighter smokers–moderate FTND (or low tolerance–moderate FTND). Note that for ordinal measures of time to first cigarette and cigarettes per day, the endorsement probability for the highest threshold is shown.
High DSM-High FTND
This class included 28% of the participants (N = 177), all of whom reported high endorsement probabilities for both DSM-IV and FTND criteria.
Low DSM-Low FTND
This class included 26% of the participants (N = 163). This class was distinguished by very high endorsement of the DSM-IV criteria of quit/cut back but fairly low endorsement likelihood across all other DSM-IV and FTND criteria.
Moderate DSM-Moderate FTND
This class (27% of participants, N = 167) is distinguished by moderate to high endorsement probability of the DSM-IV criteria of tolerance, larger/longer and time spent, and moderate endorsement probability of the FTND criteria. Individuals in this class are most likely to endorse smoking 11–25 CPD. These individuals are, therefore, likely to be moderate smokers with tolerance to nicotine and dependence problems indexed more distinctly by DSM-IV criteria.
Light Smokers–Moderate FTND
This class included 19% of the regular smokers (N = 117) and was distinguished by a very low endorsement probability for tolerance and moderate endorsement probabilities for the FTND criteria (smoking where not allowed, hate to give up first cigarette, smoking more within the first hour of waking, and smoking when ill in bed) as well as for the DSM-IV criteria of withdrawal, larger/longer, and quit/cut back. Individuals in this class tended to be more likely to endorse smoking within 6–60 min of waking but were less likely to be heavy smokers as indexed by higher endorsement of CPD = 1 (i.e., 11–19 CPD). Hence, for ease of interpretation, we label this group as lighter smokers with moderate FTND (LSMF).
Table 1 shows the prevalence of individual criteria for and diagnosis of DSM-IV– and FTND-based nicotine dependence across the four classes. These post-hoc comparisons revealed that members of the low DSM-low FTND (LDLF) class had uniformly the lowest prevalence of DSM-IV and FTND criteria with only 5.5% meeting criteria for a DSM-IV diagnosis and none meeting criteria for FTND-based nicotine dependence. In contrast, 57.1% and 100% of those in the high DSM-high FTND (HDHF) class met criteria for nicotine dependence via DSM-IV and FTND criteria, respectively. Interesting differences across the remaining two classes (moderate DSM-moderate FTND [MDMF] and LSMF) are underscored by the prevalence of criteria and diagnoses in Table 1. For instance, while approximately equal numbers of individuals in the MDMF class met criteria for an ND diagnosis using DSM-IV and/or FTND (44%–46%), the prevalence of FTND-based ND (51%) exceeded DSM-IV ND (18%) in the LSMF class. While DSM-IV ND was more common in the MDMF versus LSMF class, the prevalence of FTND-based ND could be equated across these two classes. Also, all members of the MDMF class but only 4% of those in the MDMF class reported tolerance. In contrast, 10% of the members in the LSMF class reported giving up activities to smoke, while only 3% of those in the MDMF class reported it. Variations in FTND criterion endorsement across these classes were also pronounced with members of the LSMF class, overall, endorsing significantly more FTND items than those in the MDMF class (e.g., 23% of LSMF members endorsed smoking within the first hour of waking, while only 1.8% of MDMF members endorsed this item). Despite the higher preponderance of FTND items endorsed in the LSMF class, the smokers in this group smoked considerably fewer cigarettes (i.e., no one endorsed 20 or more CPD).
Table 1.
Prevalence of Individual Criteria and Diagnosis of Nicotine Dependence From the DSM-IV and the FTND in 624 Regular Smokers
| High DSM-high FTND (N = 177) | Moderate DSM-moderate FTND (N = 167) | Lighter smokers–moderate FTND (N = 117) | Low DSM-low FTND (N = 163) | |
| DSM-IV ND diagnosis | 57.1 | 44.3 | 18.0 | 5.5 |
| Tolerance | 100 | 100 | 4.3 | 0.6 |
| Withdrawal | 76.3 | 45.5 | 47.9 | 19.6 |
| Larger/longer | 94.4 | 78.9 | 76.1 | 43.6 |
| Persistent desire or inability to quit/cut back | 88.1 | 81.6 | 89.2 | 88.0 |
| Time spent | 24.3 | 19.8 | 6.8 | 1.8 |
| Give up | 19.2 | 3.0 | 10.3 | 0.00 |
| Problems | 69.5 | 34.7 | 38.5 | 11.1 |
| Range of DSM-IV criteria | 2–7 | 1–6 | 0–5 | 0–4 |
| FTND of four or more | 100 | 46.1 | 51.3 | 0 |
| Time to first = 1 (>60 min) | 1.1 | 37.7 | 14.5 | 75.5 |
| Time to first = 1 (31–60 min) | 13.6 | 27.0 | 36.8 | 16.0 |
| Time to first = 2 (6–30 min) | 40.7 | 25.8 | 31.6 | 8.6 |
| Time to first = 3 (within 5 min) | 44.6 | 9.6 | 17.1 | 0.0 |
| Smoke where prohibited | 67.2 | 10.2 | 33.3 | 1.2 |
| Hate to give up first cigarette of day | 65.3 | 25.3 | 56.4 | 12.3 |
| CPD = 0 (<11 cigarettes) | 5.1 | 16.8 | 42.7 | 76.7 |
| CPD = 1 (11–19 cigarettes) | 16.4 | 21.0 | 57.3 | 23.3 |
| CPD = 2 (20–25 cigarettes) | 37.9 | 43.7 | 0.00 | 0.00 |
| CPD = 3 (26 or more cigarettes) | 40.7 | 18.6 | 0.00 | 0.00 |
| Smoke more in first hour of waking | 39.0 | 1.8 | 23.1 | 1.2 |
| Smoked when ill in bed | 71.8 | 21.6 | 33.3 | 0.00 |
| Range of FTND criteria | 4–10 | 0–7 | 1–8 | 0–3 |
Note. CPD = cigarettes per day; DSM-IV = Diagnostic and Statistical Manual; FTND = Fagerstrom Test for Nicotine Dependence.
To further characterize these classes, the association between a host of other smoking-related, other psychiatric, and sociodemographic measures were examined. As shown in Table 2, age at interview was not associated with class membership, and while being male was associated with not being in the LDLF, it did not distinguish between members in the three other classes. For the other smoking-related measures, the HDHF class showed the greatest aggregation of current smokers with the highest number of DSM-IV and FTND criteria. These smokers were also most likely to report craving. However, their maximum number of cigarettes smoked and peer smoking did not differ from those reported by members of MDMF class.
A majority of the psychiatric covariates were more commonly reported by those in the HDHF and the MDMF class relative to members of the LDLF and the LSMF classes, with rates of psychopathology being more pronounced in the HDHF group. Only conduct disorder and Attention-Deficit Hyperactivity Disorder (ADHD) problems were associated with membership in the LSMF class. Additionally, compared with those in the HDHF and the MDMF classes, those in the LSMF class were more likely to be recent regular smokers. Those in the LSMF class, as well as those in the LDLF class, had begun smoking regularly, on average, about 5.5 years ago compared with those in the HDHF and MDMF class who had become regular smokers 6–8 years prior to the interview.
We also examined whether those who were at varying levels of genetic (high, intermediate, and low) and environmental (high, low) risk, due to a paternal history of nicotine dependence, were over-represented in any one of these classes. As shown in Table 3, no one class showed a statistically significant over-representation of those at high genetic or high environmental risk for nicotine dependence. A majority of the sample, irrespective of class membership, could be classified as individuals at high genetic and high environmental risk for nicotine dependence. This may be attributed to this sample being restricted to regular smokers alone (i.e., the effect of parental history on the earlier stage of regular smoking was partialled out).
Table 3.
Percentage of Individuals in Each Latent Class That Are at Varying Degrees of Genetic and Environmental Risk Attributable to the Biological Father or His Cotwin’s DSM-III-R Nicotine Dependence Status
| High DSM-high FTND (N = 177) | Moderate DSM-moderate FTND (N = 167) | Lighter smokers–moderate FTND (N = 117) | Low DSM-low FTND (N = 163) | |
| High G, high E | 53.1 | 52.2 | 59.9 | 58.1 |
| High G, low E | 9.0 | 9.8 | 7.2 | 2.6 |
| Intermediate G, low E | 11.9 | 8.0 | 7.2 | 12.8 |
| Low G, low E | 26.0 | 30.0 | 25.7 | 26.5 |
Note. No statistical differences noted. FTND = Fagerstrom Test for Nicotine Dependence.
Discussion
We sought to examine whether DSM-IV and FTND criteria of nicotine dependence could be used to identify subgroups of individuals with distinct patterns of endorsement of these criteria and consequent variations in risk for nicotine dependence and other comorbid psychopathology.
LCA results can shed light on two underlying patterns of data. Either underlying all nicotine dependence criteria is a common unifying dimension (e.g., smoking quantity) or sets of criteria are etiologically distinct and oblique to each other resulting in subtypes of individuals. In the first instance, where endorsement of a set of criteria largely indexes a severity continuum, plotting the endorsement probabilities (as done in Figure 1) would result in a series of lines that are largely parallel to each other but have varying positions (i.e., index severity) along the y-axis. On the other hand, if distinct subtypes are identified, these lines would be expected to intersect, such that one class of individuals would be characterized by high endorsement probability on a series of criteria, while another class would show low endorsement probabilities for those criteria with a corresponding increase in endorsement probability for another set of criteria. In our sample of regular smokers, four groups of individuals were identified—those with low endorsement of all criteria, those with high endorsement of all criteria, those with intermediate endorsement of FTND and DSM-IV, with particularly high levels of tolerance, and a class of individuals with intermediate endorsement of FTND criteria but only modest endorsement of DSM-IV–based dependence criteria. Thus, while our findings primarily reflect a severity continuum (high endorsement vs. low endorsement of all criteria—in Figure 1, the lines denoting the HDHF, MDMF, and LDLF classes are nearly parallel), there is possible and suggestive support for a subgroup (LSMF class) of smokers. This latter grouping is demonstrated by the intersection of endorsement probabilities for the DSM-IV tolerance criterion across the MDMF and LSMF classes (with a corresponding reversal of endorsement probabilities for some of the FTND criteria across these classes (e.g., higher endorsement of hate to give up first cigarette in the LSMF class).
The MDMF class may be viewed as an intermediate risk class, and while the LSMF class appears to index similar vulnerability to the MDMF class, it is distinguished by a contrasting low endorsement of tolerance and a corresponding high endorsement of smoking less than 20 CPD. Furthermore, examination of the psychiatric covariates that aggregate with the classes highlights two key observations. First, compared with those in the LDLF class, those in the LSMF class are more likely to be male, initiate smoking prior to age 13, report greater DSM-IV and FTND symptoms, report craving, and meet criteria for a lifetime history of DSM-IV conduct disorder and ADHD problems. Thus, while these individuals are lighter smokers, they demonstrate increased vulnerability to some psychopathology. Second, despite this increased risk, relative to those in the HDHF and MDMF class, the individuals in the LSMF class report the same levels of, if not significantly less, psychopathology. For instance, while membership in LSMF class is associated with a 2.2-fold increased likelihood of conduct disorder, membership in the MDMF class is associated with a statistically comparable 1.8-fold increased risk. Furthermore, rates of neither AD nor major depressive disorder appear to be elevated in the LSMF class, while those in the MDMF class are 1.1–1.6 times more likely to meet criteria for a lifetime history of these disorders.
In addition to the marked difference in endorsement of tolerance, the apparent distinction between the MDMF and LSMF class is largely attributable to levels of smoking and recency of becoming a regular smoker. Fifty-seven percent of those in the LSMF class reported smoking 11–19 CPD (with the remainder smoking less than 11 CPD), while an overwhelming 62% of those in the MDMF (also 79% of those in the HDHF class) report smoking more than 19 CPD. Additionally, individuals in the LSMF group were more recent regular smokers, perhaps indicating that they were in the early stages of their smoking trajectories. This variation in smoking may also have contributed to the extreme discordance (0% vs. 100%) in endorsement of DSM-IV tolerance, which incorporates elements of CPD.
However, this raises the question of whether nicotine dependence and its correlated impediment of successful smoking cessation is even a concern in lighter smokers. Our results show that despite lower CPDs, nearly half the individuals in the LSMF class reported withdrawal or withdrawal relief, which is a key predictor of failed cessation (Madden et al., 1997; Rubinstein, Benowitz, Auerback, & Moscicki, 2008, 2009; Xian et al., 2005). Several studies have demonstrated that light smoking, even less than 10 CPD, can be associated with diminished autonomy over smoking, persistent smoking, and nicotine dependence (Coggins, Murrelle, Carchman, & Heidbreder, 2009). Furthermore, studies have found light smoking (defined variously; Husten, 2009) to be somewhat unstable with the social context of smoking (e.g., peers), as well as cooccurring alcohol use and psychopathology, contributing to escalation of smoking quantity and frequency in lighter smokers (Hukkinen, Kaprio, Broms, Koskenvuo, & Korhonen, 2009; Levy, Biener, & Rigotti, 2009; White, Bray, Fleming, & Catalano, 2009). Furthermore, all groups reported persistent desire and repeated unsuccessful attempts to cut back or quite smoking—in fact, this criterion failed to provide any discriminative utility across classes. Therefore, measurement of nicotine dependence in light smokers is necessary for research and practice.
A related and growing concern is that rates of daily light smoking (as well as light and intermittent smoking/LITS) have increased, particularly, in the United States. Some argue that the surge in lighter smoking patterns is attributable to greater social sanctions and prohibitions imposed on smoking (Shiffman, 2009). In our data as well, the FTND criteria of smoking where prohibited along with giving up important activities were considerably elevated in the LSMF class, even though these individuals smoked 19 or fewer CPD. With increasing denormalization of smoking, lighter smokers may continue to grow in numbers, making their characterization a priority.
The LSMF group requires further study. While they appear unique to this sample, none of the covariates tested were successful in distinguishing these individuals from other groups. It is possible that these individuals will eventually transition to the MDMF or HDHF class, and longitudinal data will be extremely informative in confirming whether this is the case. In contrast, as the individuals in this group smoke less than those in the MDMF group, longitudinal data can also be used to determine whether this group will experience successful smoking cessation, making this group a prime target for treatment and interventions. This will be examined in subsequent studies. However, the current data failed to successfully distinguish this group from the others based on post-hoc covariate analyses. Given the methodological caveats discussed below, we cannot be certain that this group is of substantive relevance until further characterized.
There are some key methodological caveats that should also be considered when viewing these findings. In some instances, such as when there is only partial conditional independence (i.e., sets of observed variables are correlated over and above their relationship via the latent classes), overextraction of classes can occur. In such cases, factor mixture models (where factors are nested within classes and where endorsement probabilities reflect changes in factor loadings and thresholds) have been shown to facilitate superior interpretation of data. Because of this, and also due to the strong observed support for the latent classes reflecting a severity continuum, we conducted an exploratory factor analysis of these data. The three factor solution fit best with the first factor loading well on all the DSM-IV criteria as well as the FTND criteria of difficulty smoking where prohibited and smoking when ill; the second factor loading primarily on the FTND criteria, particularly time to first cigarette, hate to give up first cigarette of the day, and smoking within the first hour of waking; and the third factor showing very high loadings on DSM-IV tolerance (0.997) and the FTND criterion of CPD (0.996), which are key to the LSMF class. Thus, while a factor mixture model may provide an alternate interpretation of these data, a model that accounts for the complexity of both factors and classes is somewhat intractable for this situation (particularly with this sample size, as several complex models failed due to empty cells in the joint distribution). We performed modified LCA using latent class factor analysis (where a single factor is allowed to have varying means across classes) and also partially relaxed the assumption of conditional independence (e.g., a factor with loadings on tolerance and CPD) but neither of these produced any significant improvement in model fit. Additionally, we performed these LCA by dichotomizing the two ordinal FTND measures of time to first cigarette (dichotomized as either <6 min or 6 min and longer) and CPD (dichotomized as 26+ CPD or less)—this eliminated the LSMF class resulting in a severity continuum of LDLF, MDMF, and HDHF that indicates that the identification of the LSMF class is reliant on jointly modeling tolerance with an indicator of light smoking (e.g., CPD ≥ 11 or CPD = 11–19).
Latent mixture models, such as LCA, do not directly address the relative utility and relevance of individual DSM and FTND criteria in the diagnosis of nicotine dependence. From a statistical perspective, approaches such as factor analysis (or item response modeling) are best suited to such interpretations. Several such factor analyses have been conducted. For instance, Saha et al. (2010) found that all DSM-IV nicotine dependence criteria loaded well on an underlying unidimensional construct. In contrast, B. O. Muthen and Asparouhov (2006) have argued that DSM-IV nicotine dependence is best conceptualized as a factor mixture model with three classes (including a zero class) and a single factor nested across the two nonzero classes. For FTND, both one- and two-factor (smoking pattern and morning smoking) solutions have been suggested (Haddock, Lando, Klesges, Talcott, & Renaud, 1999). However, across these studies, tolerance and CPD have been observed to have robustly high factor loadings, suggesting that they are central to the diagnosis of nicotine dependence.
We did not find evidence for increased genetic vulnerability or risk attributable to environmental influences of parental smoking to be over-represented in any class. Two possible explanations exist—first, sample size may have limited our statistical power to distinguish across these groups and second, excluding nonregular smokers may have accounted for a majority of heritable influences and the prominent role of rearing environment. This latter theory is somewhat supported by the increased numbers of members across all four classes in the high genetic (and environment) risk categories (Table 3). Additionally, multiple twin studies (Heath, Martin, Lynskey, Todorov, & Madden, 2002; Kendler et al., 1999; Lessov et al., 2004; Madden, Pedersen, Kaprio, Koskenvuo, & Martin, 2004; Pergadia, Heath, Martin, & Madden, 2006) show that after accounting for the genetic overlap between regular smoking and nicotine dependence (and persistence), most of the variation in liability to dependence/persistence is individual specific (Rose, Broms, Korhonen, Dick, & Kaprio, 2009). These studies also note that while familial environment plays a role in smoking initiation, after accounting for these early stages, there may not be additional specific shared environmental factors that impact dependence alone (Broms, Silventoinen, Madden, Heath, & Kaprio, 2006; Madden et al., 2004; Maes et al., 1999, 2006).
Finally, it is important to note that time to first cigarette played an important role in class membership—those in the MDMF class were more likely to endorse smoking their first cigarette over an hour after waking (37.6%) compared with only 14.5% of those in the LSMF class. Recent studies (Baker et al., 2007; Haberstick et al., 2007; Muscat, Stellman, Caraballo, & Richie, 2009; Niaura, Shadel, Goldstein, Hutchinson, & Abrams, 2001) have begun to focus on the salience of time to first cigarette as a marker of phenotypic and genetic vulnerability to problematic smoking, and our analyses underscore the need for studies focused on this aspect of the FTND.
Some limitations of this study are noteworthy. First, this is an OOT study with a unique sampling design—to what extent these classes would generalize to other populations remains to be seen. However, a considerable strength of this sample is the availability of both DSM-IV– and FTND-based criteria on a large cohort of adolescents and young adults. Second, while the mean age of the sample is 21.4 years, it is likely that some individuals may not be past the period of risk for the emergence of nicotine dependence symptomatology. However, as likelihood of class membership was invariant with age, this sample characteristic did not influence class assignment. Third, despite the considerable wealth of data, some measures (e.g., social context of smoking) were absent. Fourth, some distinctions across classes were attributable to levels of CPD—to what extent individuals can reliably distinguish between smoking 11–19 cigarettes versus smoking 20–25 cigarettes, or more than 25 cigarettes, may have contributed to the results. Fifth, other instruments exist for the assessment of nicotine dependence, such as the Nicotine Dependence Syndrome Scale (Shiffman, Waters, & Hickcox, 2004), the Hooked on Nicotine Checklist (DiFranza & Wellman, 2005; Wellman et al., 2005), and the Wisconsin Inventory of Smoking Dependence Motives (Piper et al., 2004) as well as others. Psychometric comparisons of these scales with the DSM-IV and FTND exist (e.g., Wellman et al., 2006)—however, our interview did not include these assessments.
As we approach the new era of DSM-V, our findings suggest that while measurement and diagnosis of liability to problematic smoking may vary, a combination of assessment instruments, when possible, may afford the most accuracy. In our study, using both DSM-IV and FTND criteria provided a more comprehensive overview of vulnerability to nicotine dependence. While each instrument may capture different aspects of nicotine dependence, our analyses suggest that the DSM-IV and FTND criteria work synergistically and where possible should be used in tandem to provide a finer-grained view of cigarette smoking behavior.
Funding
This work was supported by grants from the National Institutes of Health: DA020810, DA18660, DA14363, DA18267, and DA019951 and DA23668 from the National Institute on Drug Abuse, grants AA11667, AA11822, AA007580, and AA11998 from the National Institute on Alcohol Abuse and Alcoholism, and from a Merit Review Grant (TJ) from the Department of Veterans Affairs Medical Research Service. The United States Department of Veterans Affairs has provided financial support for the development and maintenance of the Vietnam Era Twin Registry.
Declaration of Interests
None declared.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorder. 3rd ed.revised. Washington, DC: Author; 1987. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, Kim SY, et al. Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine & Tobacco Research. 2007;9(Suppl. 4):S555–S570. doi: 10.1080/14622200701673480. doi:10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Johnson EO. Predicting smoking cessation and major depression in nicotine-dependent smokers. American Journal of Public Health. 2000;90:1122–1127. doi: 10.2105/ajph.90.7.1122. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446294/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broms U, Silventoinen K, Madden PA, Heath AC, Kaprio J. Genetic architecture of smoking behavior: A study of Finnish adult twins. Twin Research and Human Genetics. 2006;9:64–72. doi: 10.1375/183242706776403046. Retrieved from http://www.atypon-link.com/AAP/doi/pdfplus/10.1375/twin.9.1.64. [DOI] [PubMed] [Google Scholar]
- Brook JS, Koppel J, Pahl K. Predictors of DSM and Fagerstrom-defined nicotine dependence in African American and Puerto Rican young adults. Substance Use and Misuse. 2009;44:809–822. doi: 10.1080/10826080802483985. doi:10.1080/10826080802483985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret RJ, Cloninger RC, Dinwiddie SH, Hesselbrock V, Nurnberger JI, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies. Journal for the Studies on Alcohol and Drugs. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. Retrieved from http://www.jsad.com/jsad/article/A_New_SemiStructured_Psychiatric_Interview_for_Use_in_Genetic_Linkage_Stu/2000.html. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States. Morbidity and Mortality Weekly Report. 2002;51:300–303. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5114a2.htm. [PubMed] [Google Scholar]
- Coggins CR, Murrelle EL, Carchman RA, Heidbreder C. Light and intermittent cigarette smokers: A review (1989–2009) Psychopharmacology (Berlin) 2009;207:343–363. doi: 10.1007/s00213-009-1675-4. doi:10.1007/s00213-009-1675-4. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Wellman RJ. A sensitization-homeostasis model of nicotine craving, withdrawal, and tolerance: Integrating the clinical and basic science literature. Nicotine & Tobacco Research. 2005;7:9–26. doi: 10.1080/14622200412331328538. doi:10.1080/14622200412331328538. [DOI] [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Scherrer JF, Grant JD, Heath AC, Nelson EC, et al. The association between cannabis abuse and dependence and childhood physical and sexual abuse: Evidence from an offspring of twins design. Addiction. 2008;103:990–997. doi: 10.1111/j.1360-0443.2008.02210.x. doi:10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen S, True W, Goldberg J, Henderson W, Robinette CD. The Vietnam Era Twin (VET) Registry: Method of construction. Acta Geneticae Medicae et Gemellologiae (Roma) 1987;36:61–66. doi: 10.1017/s0001566000004591. [DOI] [PubMed] [Google Scholar]
- Fagerstrom KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3:235–246. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- Goldberg J, True W, Eisen S, Henderson W, Robinette CD. The Vietnam Era Twin (VET) Registry: Ascertainment bias. Acta Geneticae Medicae et Gemellologiae (Roma) 1987;36:67–78. doi: 10.1017/s0001566000004608. [DOI] [PubMed] [Google Scholar]
- Haberstick BC, Timberlake D, Ehringer MA, Lessem JM, Hopfer CJ, Smolen A, et al. Genes, time to first cigarette and nicotine dependence in a general population sample of young adults. Addiction. 2007;102:655–665. doi: 10.1111/j.1360-0443.2007.01746.x. doi:10.1111/j.1360-0443.2007.01746.x. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Lando H, Klesges RC, Talcott GW, Renaud EA. A study of the psychometric and predictive properties of the Fagerström Test for Nicotine Dependence in a population of young smokers. Nicotine & Tobacco Research. 1999;1:59–66. doi: 10.1080/14622299050011161. doi:10.1080/14622299050011171. [DOI] [PubMed] [Google Scholar]
- Heath AC, Martin NG, Lynskey MT, Todorov AA, Madden PA. Estimating two-stage models for genetic influences on alcohol, tobacco or drug use initiation and dependence vulnerability in twin and family data. Twin Research and Human Genetics. 2002;5:113–124. doi: 10.1375/1369052022983. Retrieved from http://www.atypon-link.com/AAP/doi/pdfplus/10.1375/twin.5.2.113. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Validity of the Fagerstrom test for nicotine dependence and of the Heaviness of Smoking Index among relatively light smokers. British Journal of Addiction. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Henderson WG, Eisen S, Goldberg J, True WR, Barnes JE, Vitek ME. The Vietnam Era Twin Registry: A resource for medical research. Public Health Reports. 1990;105:368–373. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1580072/?tool=pubmed. [PMC free article] [PubMed] [Google Scholar]
- Hughes JR. Should criteria for drug dependence differ across drugs? Addiction. 2006;101(Suppl. 1):134–141. doi: 10.1111/j.1360-0443.2006.01588.x. doi:10.1111/j.1360-0443.2006.01588.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Oliveto AH, Riggs R, Kenny M, Liguori A, Pillitteri JL, et al. Concordance of different measures of nicotine dependence: Two pilot studies. Addictive Behaviors. 2004;29:1527–1539. doi: 10.1016/j.addbeh.2004.02.031. doi:10.1016/j.addbeh.2004.02.031. [DOI] [PubMed] [Google Scholar]
- Hukkinen M, Kaprio J, Broms U, Koskenvuo M, Korhonen T. Characteristics and consistency of light smoking: Long-term follow-up among Finnish adults. Nicotine & Tobacco Research. 2009;11:797–805. doi: 10.1093/ntr/ntp065. doi:10.1093/ntr/ntp065. [DOI] [PubMed] [Google Scholar]
- Husten CG. How should we define light or intermittent smoking? Does it matter? Nicotine & Tobacco Research. 2009;11:111–121. doi: 10.1093/ntr/ntp010. doi:10.1093/ntr/ntp010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Waterman B, Heath A, True W, Bucholz KK, Haber R, et al. Genetic and environmental effects on offspring alcoholism: New insights using an offspring-of-twins design. Archives of General Psychiatry. 2003;60:1265–1272. doi: 10.1001/archpsyc.60.12.1265. Retrieved from http://archpsyc.ama-assn.org/cgi/content/full/60/12/1265. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Sullivan P, Corey LA, Gardner CO, Prescott CA. A population-based twin study in women of smoking initiation and nicotine dependence. Psychological Medicine. 1999;29:299–308. doi: 10.1017/s0033291798008022. Retrieved from http://journals.cambridge.org/action/displayIssue?decade=1990&jid=PSM&volumeId=29&issueId=02&iid=25922. [DOI] [PubMed] [Google Scholar]
- Lessov CN, Martin NG, Statham DJ, Todorov AA, Slutske WS, Bucholz KK, et al. Defining nicotine dependence for genetic research: Evidence from Australian twins. Psychological Medicine. 2004;34:865–879. doi: 10.1017/s0033291703001582. Retrieved from http://journals.cambridge.org/action/displayIssue?decade=2000&jid=PSM&volumeId=34&issueId=05&iid=232258. [DOI] [PubMed] [Google Scholar]
- Levy DE, Biener L, Rigotti NA. The natural history of light smokers: A population-based cohort study. Nicotine & Tobacco Research. 2009;11:156–163. doi: 10.1093/ntr/ntp011. doi:10.1093/ntr/ntp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackay J, Eriksen M, Shafey O. The tobacco atlas. Switzerland, Geneva: World Health Organization; 2006. [Google Scholar]
- Madden PA, Bucholz KK, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, et al. Nicotine withdrawal in women. Addiction. 1997;92:889–902. doi:10.1111/j.1360-0443.1997.tb02957.x. [PubMed] [Google Scholar]
- Madden PA, Pedersen NL, Kaprio J, Koskenvuo MJ, Martin NG. The epidemiology and genetics of smoking initiation and persistence: Crosscultural comparisons of twin study results. Twin Research. 2004;7:82–97. doi: 10.1375/13690520460741471. Retrieved from http://www.atypon-link.com/AAP/toc/twin/7/1. [DOI] [PubMed] [Google Scholar]
- Maes HH, Neale MC, Kendler KS, Martin NG, Heath AC, Eaves LJ. Genetic and cultural transmission of smoking initiation: An extended twin kinship model. Behavior Genetics. 2006;36:795–808. doi: 10.1007/s10519-006-9085-4. doi:10.1007/s10519-006-9085-4. [DOI] [PubMed] [Google Scholar]
- Maes HH, Woodard CE, Murrelle L, Meyer JM, Silberg JL, Hewitt JK, et al. Tobacco, alcohol and drug use in eight- to sixteen-year-old twins: The Virginia Twin Study of adolescent behavioral development. Journal for the Studies on Alcohol and Drugs. 1999;60:293–305. doi: 10.15288/jsa.1999.60.293. Retrieved from http://www.jsad.com/jsad/article/Tobacco_Alcohol_and_Drug_Use_in_Eight_to_SixteenYearOld_Twins_The_Virg/612.html. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent class analysis. Newbury Park, CA: Sage; 1987. [Google Scholar]
- Moolchan ET, Aung AT, Henningfield JE. Treatment of adolescent tobacco smokers: Issues and opportunities for exposure reduction approaches. Drug and Alcohol Dependence. 2003;70:223–232. doi: 10.1016/s0376-8716(03)00012-7. doi:10.1016/S0376-8716(03)00012-7. [DOI] [PubMed] [Google Scholar]
- Moolchan ET, Radzius A, Epstein DH, Uhl G, Gorelick DA, Cadet JL, et al. The Fagerstrom Test for Nicotine Dependence and the Diagnostic Interview Schedule: Do they diagnose the same smokers? Addictive Behaviors. 2002;27:101–113. doi: 10.1016/s0306-4603(00)00171-4. doi:10.1016/S0306-4603(00)00171-4. [DOI] [PubMed] [Google Scholar]
- Muscat JE, Stellman SD, Caraballo RS, Richie JP., Jr. Time to first cigarette after waking predicts cotinine levels. Cancer Epidemiology, Biomarkers and Prevention. 2009;18:3415–3420. doi: 10.1158/1055-9965.EPI-09-0737. doi:10.1158/1055-9965.EPI-09-0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen BO, Asparouhov T. Item response mixture modeling: Application to tobacco dependence criteria. Addictive Behaviors. 2006;31:1050–1066. doi: 10.1016/j.addbeh.2006.03.026. doi:10.1016/j.addbeh.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Integrating person-centered and variable-centered analysis: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide. 5th ed. Los Angeles, CA: Author; 2007. [Google Scholar]
- Niaura R, Shadel WG, Goldstein MG, Hutchinson KE, Abrams DB. Individual differences in responses to the first cigarette following overnight abstinence in regular smokers. Nicotine & Tobacco Research. 2001;3:37–44. doi: 10.1080/14622200020032088. doi:10.1080/14622200124231. [DOI] [PubMed] [Google Scholar]
- Pergadia ML, Heath AC, Martin NG, Madden PA. Genetic analysis of DSM-IV nicotine withdrawal in adult twins. Psychological Medicine. 2006;36:963–972. doi: 10.1017/S0033291706007495. doi:10.1017/S0033291706007495. [DOI] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) Journal of Consulting and Clinical Psychology. 2004;72:139–154. doi: 10.1037/0022-006X.72.2.139. doi:10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. In: Marsden PV, editor. Sociological methodology. Cambridge, MA: Blackwell; 1995. pp. 111–195. [Google Scholar]
- Robins L, Helzer J, Cottler L, Goldring E. NIMH Diagnostic Interview Schedule Version III Revised (DIS-III-R) St. Louis, MO: Department of Psychiatry, Washington University Medical School; 1988. [Google Scholar]
- Rose RJ, Broms U, Korhonen T, Dick D, Kaprio J. Genetics of smoking behavior. In: Kim Y.-K., editor. Handbook of behavior genetics. New York, NY: Springer Science+Business Media; 2009. pp. 411–433. [Google Scholar]
- Rubinstein ML, Benowitz NL, Auerback GM, Moscicki AB. Rate of nicotine metabolism and withdrawal symptoms in adolescent light smokers. Pediatrics. 2008;122:e643–e647. doi: 10.1542/peds.2007-3679. doi:10.1542/peds.2007-3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinstein ML, Benowitz NL, Auerback GM, Moscicki AB. Withdrawal in adolescent light smokers following 24-hour abstinence. Nicotine & Tobacco Research. 2009;11:185–189. doi: 10.1093/ntr/ntn028. doi:10.1093/ntr/ntn028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha TD, Compton WM, Pulay AJ, Stinson FS, Ruan WJ, Smith SM, et al. Dimensionality of DSM-IV nicotine dependence in a national sample: An item response theory application. Drug and Alcohol Dependence. 2010;108:21–28. doi: 10.1016/j.drugalcdep.2009.11.012. doi:10.1016/j.drugalcdep.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute. SAS user guide, version 8.2. Cary, NC: Author; 1999. [Google Scholar]
- Scherrer JF, Waterman BM, Heath AC, Bucholz KK, True WR, Jacob T. Are substance use, abuse and dependence associated with study participation? Predictors of offspring nonparticipation in a twin-family study. Journal for the Studies on Alcohol and Drugs. 2004;65:140–144. doi: 10.15288/jsa.2004.65.140. Retrieved from http://www.jsad.com/jsad/article/Are_Substance_Use_Abuse_and_Dependence_Associated_with_Study_Participation/1119.html. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Light and intermittent smokers: Background and perspective. Nicotine & Tobacco Research. 2009;11:122–125. doi: 10.1093/ntr/ntn020. doi:10.1093/ntr/ntn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: A multidimensional measure of nicotine dependence. Nicotine & Tobacco Research. 2004;6:327–348. doi: 10.1080/1462220042000202481. doi:10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Stata Corp. STATA. College Station, TX: Author; 2003. [Google Scholar]
- Strong DR, Brown RA, Ramsey SE, Myers MG. Nicotine dependence measures among adolescents with psychiatric disorders: Evaluating symptom expression as a function of dependence severity. Nicotine & Tobacco Research. 2003;5:735–746. doi: 10.1080/1462220031000158609. doi:10.1080/1462220031000158609. [DOI] [PubMed] [Google Scholar]
- Wellman RJ, DiFranza JR, Pbert L, Fletcher KE, Flint A, Young MH, et al. A comparison of the psychometric properties of the hooked on nicotine checklist and the modified Fagerstrom tolerance questionnaire. Addictive Behaviors. 2006;31:486–495. doi: 10.1016/j.addbeh.2005.05.031. doi:10.1016/j.addbeh.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Wellman RJ, DiFranza JR, Savageau JA, Godiwala S, Friedman K, Hazelton J. Measuring adults’ loss of autonomy over nicotine use: The Hooked on Nicotine Checklist. Nicotine & Tobacco Research. 2005;7:157–161. doi: 10.1080/14622200412331328394. doi:10.1080/14622200412331328394. [DOI] [PubMed] [Google Scholar]
- White HR, Bray BC, Fleming CB, Catalano RF. Transitions into and out of light and intermittent smoking during emerging adulthood. Nicotine & Tobacco Research. 2009;11:211–219. doi: 10.1093/ntr/ntn017. doi:10.1093/ntr/ntn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xian H, Scherrer JF, Madden PA, Lyons MJ, Tsuang M, True WR, et al. Latent class typology of nicotine withdrawal: Genetic contributions and association with failed smoking cessation and psychiatric disorders. Psychological Medicine. 2005;35:409–419. doi: 10.1017/s0033291704003289. doi:10.1017/S0033291704003289. [DOI] [PubMed] [Google Scholar]