Abstract
Background
Overall, the incidence of papillary thyroid cancer in Hispanic women residing in the United States (US) is similar to that of non-Hispanic white women. However, little is known as to whether rates in Hispanic women vary by nativity, which may influence exposure to important risk factors.
Methods
Nativity-specific incidence rates among Hispanic women were calculated for papillary thyroid cancer using data from the California Cancer Registry (CCR) for the period 1988–2004. For the 35% of cases for whom birthplace information was not available from the CCR, nativity was statistically imputed based on age at Social Security number issuance. Population estimates were extracted based on US Census data. Incidence rate ratios (IRR) and 95% confidence intervals (CI) were also estimated.
Results
In young (age <55 years) Hispanic women, the incidence of papillary thyroid cancer among US-born (10.65 per 100,000) was significantly greater than that for foreign-born (6.67 per 100,000; IRR=1.60, 95% CI: 1.44–1.77). The opposite pattern was observed in older women. The age-specific patterns showed marked differences by nativity: among foreign-born, rates increased slowly until age 70 years, whereas, among US-born, incidence rates peaked during the reproductive years. Incidence rates increased over the study period in all subgroups.
Conclusion
Incidence rates of papillary thyroid cancer vary by nativity and age among Hispanic women residing in California. These patterns can provide insight for future etiologic investigations of modifiable risk factors for this increasingly common and understudied cancer.
Keywords: papillary thyroid cancer, incidence rates, nativity, Hispanic women, cancer surveillance
INTRODUCTION
About fifteen percent of the US population identifies themselves as Hispanic, a US federal designation for persons whose ancestral origin is a Spanish-speaking country 1, 2. In California, 35% of the population is Hispanic, among whom 77% are of Mexican heritage and 9% Central American; 40% are born outside the US 3. The US Hispanic population is substantially younger (median age=25.9 years) than the general US population (median age=35.3 years) and growing substantially faster (58% population increase from 1990 to 2000 among Hispanics, compared to 23% for the total US population) 2. Thus, cancers that disproportionately affect young people, such as thyroid cancer in women, are of potential concern for this rapidly growing segment of the US population.
Risk factors differ by histologic type of thyroid cancer. Papillary carcinoma (including its variant mixed papillary/follicular carcinoma) is the most common type of thyroid cancer, accounting for about 85% of all thyroid cancers in areas that do not experience iodine deficiency, such as the US4. In the US, papillary thyroid cancer is about three times more common in women than men and, among women, peaks in incidence at about age 45 years 4. Age-adjusted thyroid cancer incidence rates in Hispanic women in the US and Canada are about 10% lower than in non-Hispanic (NH) white women 2, 5. The GLOBOCAN project estimates that thyroid cancer incidence rates among women in Mexico are about 75% lower than those in the total US population 6. Across Central and South America (excluding Brazil), thyroid cancer incidence rates vary five-fold, from 1.9 per 100,000 women in Argentina to 10.2 per 100,000 in Ecuador (for the period 1998–2002 and standardized to the 1960 world population) 7; comparable rates for California Hispanics and NH whites are 8.3 and 9.0 per 100,000 women, respectively. Understanding how cancer rates vary by nativity, particularly in an ethnic group with a large immigrant population, such as US Hispanics, can provide valuable insights into the etiology and prevention of that cancer. Differences in rates by nativity may point to readily modifiable risk factors (e.g., diet, physical activity, goitrogenic exposures, and factors associated with immigration and acculturation), whereas similar rates may suggest genetic and stable environmental causes. The only prior report of differences in thyroid cancer incidence by birthplace in Hispanic women was conducted in the early 1970s in Los Angeles County, California 8. These investigators found that Spanish-surnamed women who were not born in Mexico were about 45% more likely to develop thyroid cancer than Mexico-born women and hypothesized that these differences were due to environmental factors. However, their “not Mexico-born” group included not only women born in the US, but also those born in Spanish-speaking countries other than Mexico and presumably those with unknown birthplace, although the proportion of the population with unknown birthplace was not specified. Using updated, statewide California Cancer Registry (CCR) data with enhanced nativity information, the present analysis examines variation in papillary thyroid cancer incidence rates by nativity among Hispanic women in California, the US state with the largest Hispanic population 9.
METHODS
Cancer incidence data for this analysis were obtained from the CCR, which is part of the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Program. Reporting of cancer cases to the CCR is mandated by law and data sharing agreements with 13 states yields an estimated completeness rate of 99 percent 10. Hispanic women with thyroid cancer (International Classification of Diseases for Oncology version 3 (ICD-O-3) site code C73.9) were included in the present analysis if they were diagnosed between January 1, 1988 and December 31, 2004, were residents of California at the time of diagnosis, and were diagnosed with a papillary thyroid carcinoma or its variant mixed papillary-follicular carcinoma (ICD-O-3 histology codes 8050, 8260, or 8340–8344). Comparable NH white and black women were also included in the analyses as a reference. The North American Association of Central Cancer Registries (NAACCR) Hispanic Identification Algorithm (NHIA), which is based on surname, maiden name, and/or birthplace, was used to improve classification of Hispanic ethnicity 11.
Information on birthplace is routinely collected by the CCR from hospital medical records and death certificates. Our prior research shows that these data, when available, are highly accurate at the level of US- and foreign-born 12, 13. Among Hispanic women in the present analysis, medical record information on birthplace was available for 64% of women and death certificate information was available for an additional 1%. For women whose birthplace was not available from these two sources, we used the first five digits of the Social Security number (SSN) to impute nativity, as described previously 14; these first five digits correspond with the year of issuance. Women whose SSN was issued prior to age 20 were assumed to be US-born, while women who were age 20 or older at issuance were assumed to be born outside the US 15, 16. This age cut-point was determined based on self-reported birthplace data derived from a series of epidemiologic studies in which cancer patients participated 13. This approach maximizes predictive value and minimizes misclassification as determined by examining receiver operating characteristic curves (which plots sensitivity versus (1-specificity) and determines the point at which sensitivity and specificity are at their maximum) and resulted in a sensitivity of 81% and specificity of 80% for detecting foreign-born status among Hispanics in this population. The optimal positive predictive value of this single age cut-point was also confirmed by using a logistic regression model with age at SSN issue (the independent variable) as a continuous predictor of the log odds of foreign-born status (the dependent variable). When the log odds of being foreign born is greater than zero, we classified an individual as foreign born. The cutoff was then set to the minimum age (here age 20) at which the log odds is greater than zero. This model was highly statistically significant. Thirty-one percent of the nativity data were determined by this method. For the remaining 4% of women for whom SSN information was not available, nativity was randomly assigned based on the age-, sex-, and ethnicity-specific distributions of nativity among all cancer cases reported to the registry.
Hispanic population estimates by sex and five-year age groups were obtained from the 1990 and 2000 Census Summary Files 3 for the state of California. Data from the 20% Integrated Public-Use Microdata Sample of the censuses were used to estimate the age distribution of foreign-born persons; estimates were smoothed using the smooth spline function in the R statistical software package 17–20. For intercensal years, the percent of foreign-born persons was estimated using linear interpolation and extrapolation methods. Estimates were adjusted to match total Hispanic population estimates, by age and year, as provided by the California Department of Finance (for years 1988–1989) and the US Census (for years 1990–2004).
SEER*Stat software 21 was used to compute age-adjusted and age-specific incidence rates per 100,000 women, standardized to the 2000 US standard million population, and 95% confidence intervals (CI). Incidence rate ratios (IRR) and corresponding CIs were calculated to estimate the magnitude of the difference between rates for US- and foreign-born women, with the latter being the reference group. Time trends in incidence rates between 1988 and 2004 were examined using Joinpoint Regression software 22, 23 to calculate the annual percent change (APC). This software calculates APCs by fitting a series of least squares regression lines to the natural logarithm of the age-adjusted incidence rates (the dependent variable), using calendar year as the independent regression variable. This method allows for the identification of all changes in the slope of the regression (trend) line that represent statistically significant contributions to the explanatory model based on the Permutation Test and the Bayesian Information Criterion; the points at which the trend lines change are termed the “joinpoints”.
RESULTS
Of 4,884 Hispanic women with incident papillary thyroid cancer, 2,306 (47%) were US-born, compared to 57% of the female Hispanic population in California. The age-adjusted papillary thyroid cancer incidence rate for US-born Hispanic women (8.53 per 100,000) was significantly higher than the rate for foreign-born Hispanic women (7.38 per 100,000) (IRR=1.16, 95% CI: 1.09–1.23; Table 1). Both rates were significantly greater than those experienced by NH black women. Age-adjusted rates for NH white women fell approximately mid-way between those for foreign-born and US-born Hispanics.
Table 1.
Age-adjusteda papillary thyroid cancer incidence rates (per 100,000) in non-Hispanic (NH) white, NH black, and Hispanic women, California 1988–2004.
| Casesb | Populationb | Rate | 95% CI | IRRc | 95% CI | |
|---|---|---|---|---|---|---|
| NH white | 12,045 | 142,863,244 | 8.01 | 7.86 – 8.15 | ||
| NH black | 659 | 19,418,799 | 3.73 | 3.44 – 4.03 | ||
| Hispanic | 4,884 | 80,015,852 | 7.80 | 7.56 – 8.04 | ||
| US-born | 2,306 | 45,755,983 | 8.53 | 8.15 – 8.92 | 1.16 | 1.08 – 1.23 |
| Foreign-born | 2,578 | 34,259,869 | 7.38 | 7.07 – 7.70 | 1.0 |
Age-standardized to the 2000 United States population.
17-year aggregate.
Incidence rate ratio (IRR) comparing US-born to foreign-born (reference) Hispanic women.
A significant annual increase in papillary thyroid cancer rates was evident in all the groups investigated, ranging from 3.9% to 4.8% per year (for the period 1988 to 2004) among foreign-born and US-born Hispanic women, respectively, to 5.3% per year (for the period 1993 to 2004) among NH white women (Figure 1; Table 2). When examined by age group (Table 3), the rate of increase did not differ significantly for younger (age<55 years) and older women. The difference in incidence between US-born and foreign-born Hispanic women was greatest in the most recent time period (IRR=1.25, 95% CI: 1.14–1.37 for 2000–2004; Table 2). However, the US-born excess was evident only among young (age <55 years) women (US- vs foreign-born IRR=1.60, 95% CI: 1.44–1.77 for 2000–2004), whereas among older Hispanic women, those who are foreign-born experienced a higher incidence of thyroid cancer (US- vs foreign-born IRR=0.74, 95% CI: 0.61–0.91 for 2000–2004; Table 3). The highest incidence rates observed (16.68 per 100,000) were for foreign-born Hispanic women during the most recent time period. Figure 2 illustrates age-specific incidence rates for US- and foreign-born Hispanic women and compares them to those rates among NH white and black women. Overall, age-specific patterns were similar for US-born Hispanics and NH whites. In these groups, incidence rates peaked near the end of the reproductive period (at age 40–44 years) and declined thereafter. In contrast, incidence among foreign-born Hispanic women and NH black women increased steadily with age, peaking at age 70–74 years, with significantly higher rates among foreign-born Hispanics than NH blacks from age 25 years onward. The incidence rates in US-born Hispanic women between ages 15 and 44 years were significantly greater than those observed for foreign-born Hispanic women. Among older women, incidence rates for foreign-born women were only statistically greater than for US-born women for those age 70–74 years.
Figure 1.
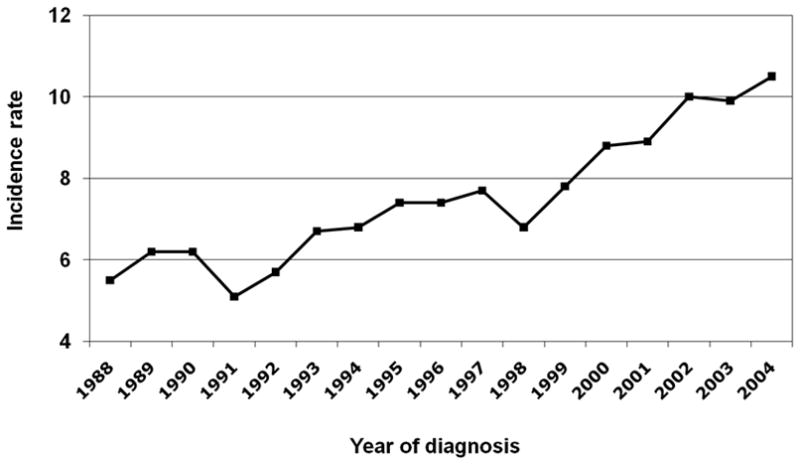
Age-adjusted papillary thyroid cancer incidence rates (per 100,000) in Hispanic women, by calendar year, California.
Table 2.
Age-adjusted papillary thyroid cancer incidence ratesa (per 100,000) by calendar period in NH white, black, and Hispanic women, California 1988–2004.
| 1988–1994
|
1995–1999
|
2000–2004
|
APCb (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Population | Rate (95% CI) | Cases | Population | Rate (95% CI) | Cases | Population | Rate (95% CI) | ||
| NH white | 3,986 | 59,971,664 | 6.35 (6.15–6.55) | 3,495 | 41,527,978 | 8.00 (7.73–8.27) | 4,564 | 41,363,602 | 10.30 (10.00–10.61) | 1.7 (−0.3–3.8), 5.3 (4.8–5.9)c,d |
| NH black | 218 | 7,649,571 | 3.23 (2.80–3.70) | 171 | 5,771,528 | 3.23 (2.76–3.76) | 270 | 5,997,700 | 4.82 (4.26–5.43) | 4.1 (2.3–5.9)d |
| Hispanic | 1,287 | 27,172,388 | 5.96 (5.60–6.33) | 1,428 | 24,208,499 | 7.52 (7.09–7.96) | 2,173 | 28,604,058 | 9.54 (9.12–9.98) | 4.3 (3.6–5.0)d |
| US-born | 652 | 15,435,339 | 6.46 (5.92–7.05) | 632 | 13,716,521 | 7.86 (7.20–8.57) | 1,022 | 16,604,123 | 11.03 (10.31–11.78) | 4.8 (3.8–5.8)d |
| Foreign-born | 643 | 11,767,968 | 5.77 (5.28–6.29) | 778 | 10,491,970 | 7.16 (6.61–7.75) | 1,157 | 11,999,931 | 8.81 (8.27–9.39) | 3.9 (2.9–4.9)d |
| IRRe | 1.12 (0.99–1.27) | 1.10 (0.98–1.24) | 1.25 (1.14–1.37) | |||||||
Age-standardized to the 2000 United States population.
Annual percent change(APC).
Joinpoint regression found multiple regression lines that fit the data: APC and 95% CIs are for 1988–1993 and 1993–2004, respectively.
p<0.05.
Incidence rate ratio (IRR) comparing US-born to foreign-born (reference) Hispanic women.
Table 3.
Papillary thyroid cancer incidence ratesa (per 100,000) by age group and calendar period in Hispanic women, California 1988–2004.
| 1988–1994
|
1995–1999
|
2000–2004
|
APCb (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Aggregate Population | Rate (95% CI) | Cases | Aggregate Population | Rate (95% CI) | Cases | Aggregate Population | Rate (95% CI) | ||
| Age <55 | ||||||||||
| US-born | 568 | 14,196,718 | 6.50 (5.93–7.12) | 537 | 12,719,188 | 7.52 (6.85–8.24) | 869 | 15,403,810 | 10.65 (9.90–11.44) | 4.5 (3.3–5.7) |
| Foreign-born | 496 | 10,377,516 | 4.48 (4.06–4.93) | 626 | 9,176,475 | 5.93 (5.45–6.45) | 852 | 10,198,961 | 6.67 (6.,22–7.17) | 3.5 (2.2–4.7) |
| IRRc | 1.45 (1.27–1.66) | 1.27 (1.12–1.44) | 1.60 (1.44–1.77) | |||||||
| Age ≥ 55 | ||||||||||
| US-born | 84 | 1,238,621 | 6.33 (4.96–7.99) | 95 | 997,333 | 9.13 (7.35–11.22) | 153 | 1,200,313 | 12.40 (10.51–14.53) | 6.0 (3.4–8.6) |
| Foreign-born | 147 | 1,390,452 | 10.51 (8.86–12.39) | 152 | 1,315,495 | 11.68 (9.86–13.76) | 305 | 1,800,970 | 16.68 (14.80–18.73) | 4.5 (2.8–6.2) |
| IRRc | 0.60 (0.45–0.81) | 0.78 (0.59–1.02) | 0.74 (0.61–0.91) | |||||||
Age-standardized to the 2000 United States population.
Annual percent change(APC); joinpoint regression found a single regression line fit the data (1988–2004); p<0.05.
Incidence rate ratio (IRR) comparing US-born to foreign-born (reference) Hispanic women.
Figure 2.
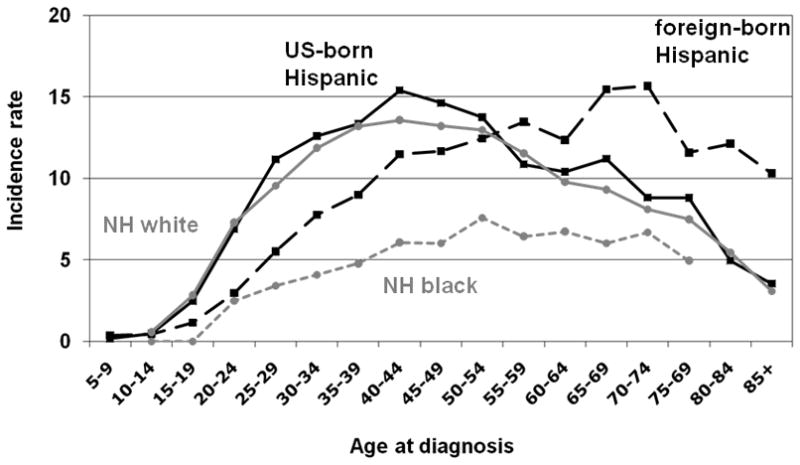
Age-specific papillary thyroid cancer incidence rates (per 100,000) in NH white (solid grey line), black (dashed grey line), and Hispanic women by birthplace (US-born, solid black line; foreign-born, dashed black line), California 1988–2004.
DISCUSSION
In the present study, we found marked differences in the age-adjusted and age-specific incidence rates of papillary thyroid cancer according to nativity among Hispanic women residing in California. The higher age-adjusted incidence rates among US-born Hispanic women compared to their foreign-born counterparts is consistent with the only previous evaluation of this issue conducted in the early 1970s 8. We further observed that the higher incidence in US-born Hispanics is limited to young women (age<55 years), with the opposite – higher rates in those who were foreign-born - being observed among older women. We found that these nativity differences, overall as well as in younger women, have increased with calendar time. Finally, we observed that among foreign-born Hispanic women, the age-specific incidence rates increased until about age 70 years and declined thereafter, mirroring the pattern seen in NH black women (although the absolute rates in Hispanic women were substantially higher). Whereas, in US-born Hispanic women, a pattern similar to that seen in NH white women was observed, i.e., an increase in rates peaking during the reproductive years and declining after the menopausal period. These nativity differences among Hispanic women are similar to those seen in Chinese, Korean, Filipina, and Vietnamese women 24.
Unlike many adult cancers where the age-specific rates increase with age into the 70’s or 80’s, thyroid cancer rates in white women, and as observed here, in US-born Hispanic women, peak during the reproductive years and declines thereafter 4. This finding is consistent with the thyroid cancer literature showing that pregnancy confers a transient (approximately 5-year) increased risk 25–28. However, it is not clear why foreign-born Hispanic women, and black women, do not experience the same pattern. Thyroid cancer risk factors in black women have not been evaluated, most likely due to the rarity of the disease in this population. However, the finding that foreign-born Hispanic women have a similar pattern of age-specific rates opens up new possibilities for further examining the differences in risk factors for these two distinct rate patterns.
The highest age-adjusted rates we observed in this study were among older (age ≥ 55 years) foreign-born Hispanic women. The fact that these rates were significantly higher than those among older US-born Hispanic women suggests that lifestyle and environmental factors that change with migration, such as diet or iodine status, may be acting on a background of earlier life exposures that differ between US and Mexican and Latin American residents, such as the presence of endemic goiter or the timing of pubertal development. This hypothesis is consistent with findings from a previous study of Asian women residing in California, where we found that a greater prevalence of prior proliferative benign thyroid disease (i.e., goiter or thyroid nodules), more recent migration (85% of women were foreign-born), and lower phytonutrient intake accounted for a substantial proportion of the difference in incidence between older ethnic groups experiencing high and low rates of thyroid cancer 29. It is also consistent with the observation that later age at menarche, a risk factor for thyroid cancer that may be more important for women age 45 and older than younger women 25, 28, 30, is more prevalent among foreign-born Hispanic women than those who are US-born 31.
Finally of note is the rapid increase in thyroid cancer rates in all subgroups, regardless of ethnicity, nativity, and age. It has been suggested by some authors that the increase in thyroid cancer incidence in some populations is predominantly the result of improvements in diagnostic technology rather than a “true” increase in incidence 32. However, thyroid cancer has been increasing in a substantial number of populations worldwide 33, 34, and those findings, along with ours, demonstrating similar increases in populations that are unlikely to have similar access to or utilization of diagnostic technologies, provides increasing evidence that there are likely additional causes for the increasing rates of thyroid cancer.
While most Hispanic patients in our study had medical record-based information on birthplace, which has been shown to be highly accurate 12, 13, 35% were missing this information. Our research has shown that cancer cases with missing birthplace data are more likely to be alive, of younger age, and US-born than those with known data, and thus, random imputation of birthplace will underestimate rates in US-born and overestimate them in foreign-born persons 12, 13, 35, 36. The SSN-based imputation method used in the present study minimizes this misclassification enabling more accurate estimation of incidence rates by nativity. Thus, we were able to study of the impact of nativity on thyroid cancer rates taking full advantage of cancer registry data by including all patients rather than excluding those with unknown birthplace or randomly assigning birthplace to those with missing information, approaches that likely yield biased estimates. However, if patients use SSNs other than their own, there is the possibility of inaccurate imputation of birthplace. We could not find any information on how often this takes place among Hispanic populations in the context of health care. In addition, the sensitivity and specificity of our method is only ~80%, thus, some misclassification remains. Nonetheless, given that our best imputation is based on a single age cut-point, these inaccuracies are likely to be limited.
We also have some limitations with respect to the classification of women as Hispanic in the cancer registry records. Using self-reports as a “gold standard,” registry classification of Hispanics has been shown to have moderate sensitivity (69%–79%) and positive predictive value (72%–82%) 37, 38. However, the relative bias when calculating age-adjusted cancer incidence rates is minimal (<1%) because the misclassification of true Hispanics as non-Hispanics and true non-Hispanics as Hispanics is essentially equal in magnitude 38. Although the impact of such misclassification on age-specific rates has not been evaluated, the accuracy of reporting Hispanic ethnicity in registry data has improved over time 37, assisted in part by the use of the NAACCR NHIA algorithm.
In summary, we observed that the pattern of age-specific papillary thyroid cancer incidence rates is strongly influenced by nativity, with US-born Hispanic women having a substantially increased incidence of this cancer during early- and mid-adult life and foreign-born experiencing a greater burden during later life, possibly suggesting different etiologic factors or variation in the time-dependent influence of acculturation factors. In addition, we showed that the incidence of this cancer is increasing significantly over time in both nativity groups and among both younger and older women. Further research is needed to elucidate how immigration and acculturation influence other life events and exposures that may account for these elevated rates. In particular, examination of behavioral and cultural differences between US-born and foreign-born Hispanic women, as well as similarities and differences between US-born Hispanic women and foreign-born Hispanic and NH black women, may yield insight into the identification of modifiable risk factors that is critical for the prevention of this cancer.
Acknowledgments
Sources of Support: This research was supported by the National Cancer Institute’s (NCI) Surveillance, Epidemiology and End Results (SEER) Program under contract N01-PC-35136 awarded to the Cancer Prevention Institute of California (CPIC; formerly the Northern California Cancer Center) and by a SEER Rapid Response Surveillance Study under contracts N01-PC-35136 and N01-PC-35139. The collection of cancer incidence data used in this study was supported by the California Department of Health Services (CDHS) as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the NCI’s SEER Program under contract N01-PC-35136 awarded to the CPIC, contract N01-PC-35139 awarded to the University of Southern California, and contract N02-PC-15105 awarded to the Public Health Institute (PHI); and the Centers for Disease Control and Prevention’s (CDCP) National Program of Cancer Registries, under agreement #U55/CCR921930-02 awarded to PHI. The ideas and opinions expressed herein are those of the authors and endorsement by the State of California, CDHS, NCI, and CDCP or their contractors and subcontractors is not intended nor should be inferred.
The authors thank Dr. Tim Miller and Ms. Rita Leung, Sarah Shema, Jane Pham, Laura McClure, and Kari Fish for their help with the compilation of data used in this study.
Footnotes
Financial Disclosures: None of the authors have any financial disclosures to make.
References
- 1.Census Facts 2007. 2009 June; http://quickfacts.census.gov/qfd/states/06000.html.
- 2.Howe HL, Wu X, Ries LAG, Cokkinides V, Ahmed F, Jemal A, et al. Annual report to the nation on the status of cancer, 1975–2003, featuring cancer among U.S. Hispanic/Latino populations. Cancer. 2006;107:1711–42. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- 3.Ask. CHIS: UCLA Center for Health Policy Research; Jun, 2009. 2007 California Health Interview Survey. [Google Scholar]
- 4.Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlander N, et al. SEER Cancer Statistics Review, 1975–2006. Bethesda, MD: National Cancer Institute; http://seer.cancer.gov/csr/1975_2006/ based on November 2008 SEER data submission, posted to the SEER website, 2009. [Google Scholar]
- 5.Kwong SL, Perkins CI, Morris CR, Cohen R, Allen M, Schlag R, et al. Cancer in California: 1988–1998. California: Department of Health Services, Cancer Surveillance Section; Dec, 2000. [Google Scholar]
- 6.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008: Cancer Incidence, Mortality and Prevalence Worldwide: IARC CancerBase No. 10 [Internet] Lyon, France: International Agency for Research on Cancer; 2010. [Google Scholar]
- 7.Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, et al. IARC Scientific Publications No. 160. IX. IARC; 2007. Cancer Incidence in Five Continents. [Google Scholar]
- 8.Menck HR, Henderson BE, Pike MC, Mack T, Martin SP, SooHoo J. Cancer incidence in the Mexican-American. J Natl Cancer Inst. 1975;55:531–36. doi: 10.1093/jnci/55.3.531. [DOI] [PubMed] [Google Scholar]
- 9.US Census Bureau. Hispanics in the United States. 2006. [Google Scholar]
- 10.California Cancer Registry.
- 11.NAACCR Latino Research Work Group. NAACCR Guideline for Enhancing Hispanic/Latino Identification Algorithm [NHIA v2] North American Association of Cancer Registries (NAACCR); Sep, 2005. [Google Scholar]
- 12.Gomez SL, Glaser SL. Quality of birthplace information obtained from death certificates for Hispanics, Asians, and Pacific Islanders. Ethn Dis. 2004;14:292–95. [PubMed] [Google Scholar]
- 13.Gomez SL, Glaser SL. Quality of cancer registry birthplace data for Hispanics living in the United States. Cancer Causes Control. 2005;16:713–23. doi: 10.1007/s10552-005-0694-7. [DOI] [PubMed] [Google Scholar]
- 14.Keegan THM, John EM, Fish K, Alfaro-Velcamp T, Clarke C, Gomez SL. Breast cancer incidence patterns among California Hispanic women: Differences by nativity and residence in an enclave. Cancer Epidemiol Biomarkers Prev. 2010;19:1208–18. doi: 10.1158/1055-9965.EPI-10-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Block G, Matanoski GM, Seltser RS. A method for estimating year of birth using social security number. Am J Epidemiol. 1983;118:377–95. doi: 10.1093/oxfordjournals.aje.a113645. [DOI] [PubMed] [Google Scholar]
- 16.Shimizu H, Ross RK, Bernstein L, Yatani R, Henderson BE, Mack TM. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br J Cancer. 1991;63:963–66. doi: 10.1038/bjc.1991.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bates D, Chambers J, Dalgaard P, et al. The R Foundation for Statistical Computing. 2.8.0. R Program [R] [Google Scholar]
- 18.Chang ET, Keegan TH, Gomez SL, Le GM, Clarke CA, So SK, et al. The burden of liver cancer in Asians and Pacific Islanders in the Greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109:2100–08. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gomez SL, Le GM, Miller T, et al. Cancer Incidence Among Asians in the Greater Bay Area, 1990–2002. Fremont, CA: Northern California Cancer Center; 2005. [Google Scholar]
- 20.Keegan TH, Gomez SL, Clarke CA, Chan JK, Glaser SL. Recent trends in breast cancer incidence among 6 Asian groups in the Greater Bay Area of Northern California. Int J Cancer. 2007;120:1324–29. doi: 10.1002/ijc.22432. [DOI] [PubMed] [Google Scholar]
- 21.Surveillance Research Program. SEER*Stat Software. 6.1.4. 2005. [Google Scholar]
- 22.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 23.Joinpoint Regression Program (version 3.4.3) http://surveillance.cancer.gov/joinpoint/
- 24.Horn-Ross PL, McClure LA, Chang ET, Clarke CA, Keegan THM, Rull RP, et al. Papillary thyroid cancer incidence rates vary significantly by birthplace in Asian American women. Cancer Causes Control. doi: 10.1007/s10552-010-9720-5. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brindel P, Doyon F, Rachedi F, Boissin J-L, Sebbag J, Shan L, et al. Menstrual and reproductive factors in the risk of differentiated thyroid carcinoma in native women in French Polynesia: a population-based case-control study. Am J Epidemiol. 2008;15:219–29. doi: 10.1093/aje/kwm288. [DOI] [PubMed] [Google Scholar]
- 26.Memon A, Darif M, Al-Saleh K, Suresh A. Epidemiology of reproductive and hormonal factors in thyroid cancer: evidence from a case-control study in the Middle East. Int J Cancer. 2002;97:82–89. doi: 10.1002/ijc.1573. [DOI] [PubMed] [Google Scholar]
- 27.Rossing MA, Voigt LF, Wicklund KG, Daling JR. Reproductive factors and risk of papillary thyroid cancer in women. Am J Epidemiol. 2000;151:765–72. doi: 10.1093/oxfordjournals.aje.a010276. [DOI] [PubMed] [Google Scholar]
- 28.Sakoda LC, Horn-Ross PL. Reproductive and menstrual history and papillary thyroid cancer risk: the San Francisco Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev. 2002;11:51–7. [PubMed] [Google Scholar]
- 29.Haselkorn T, Stewart SL, Horn-Ross PL. Why are thyroid cancer rates so high in Southeast Asian women living in the United States? The Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev. 2003;12:144–50. [PubMed] [Google Scholar]
- 30.Troung T, Orsi L, Dubourdieu D, Rougier Y, Hemon D, Guenel P. Role of goiter and of menstrual and reproductive factors in thyroid cancer: a population-based case-control study in New Caledonia (South Pacific), a very high incidence area. Am J Epidemiol. 2005;161:1056–65. doi: 10.1093/aje/kwi136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.John EM, Phipps AI, Davis A, Koo J. Migration history, acculturation, and breast cancer risk in Hispanic women. Cancer Epidemiol Biomarkers Prev. 2005;14:2905–13. doi: 10.1158/1055-9965.EPI-05-0483. [DOI] [PubMed] [Google Scholar]
- 32.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. J Am Med Assoc. 2006;295:2164–67. doi: 10.1001/jama.295.18.2164. [DOI] [PubMed] [Google Scholar]
- 33.Chen AY, Jemal A, Ward EM. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer. 2009;115:3801–07. doi: 10.1002/cncr.24416. [DOI] [PubMed] [Google Scholar]
- 34.Kilfoy BA, Zheng T, Holford TR, Han X, Ward MH, Sjodin A, et al. International patterns and trends in thyroid cancer incidence, 1973–2002. Cancer Causes Control. 2009;20:525–31. doi: 10.1007/s10552-008-9260-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Hlth. 2004;94:1977–84. doi: 10.2105/ajph.94.11.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin SS, O’Malley CD, Lui SW. Factors associated with missing birthplace information in a population-based cancer registry. Ethn Dis. 2001;11:598–605. [PubMed] [Google Scholar]
- 37.Clegg LX, Reichman ME, Hankey BF, Miller BA, Lin YD, Johnson NJ, et al. Quality of race, Hispanic ethnicity, and immigrant status, in population-based cancer registry data: implications for health disparity studies. Cancer Causes Control. 2007;18:177–87. doi: 10.1007/s10552-006-0089-4. [DOI] [PubMed] [Google Scholar]
- 38.Gomez SL, Glaser SL. Misclassification of race/ethnicity in a population-based cancer registry (United States) Cancer Causes Control. 2006;17:771–81. doi: 10.1007/s10552-006-0013-y. [DOI] [PubMed] [Google Scholar]


