Abstract
Objective
Examine the effect of prepregnancy weight and maternal gestational weight gain on postterm delivery rates.
Methods
This was a retrospective cohort study of term, singleton births (N=375,003). We performed multivariable analyses of the association between postterm pregnancy and both prepregnancy body mass index (BMI) and maternal weight gain.
Results
Prolonged or postterm delivery (41 or 42 weeks) was increasingly common with increasing prepregnancy weight (p<0.001) and increasing maternal weight gain (p<0.001). Underweight women were 10% less likely to deliver postterm than normal weight women who gain within the recommendations (aOR 0.90 (95% CI 0.83, 0.97)). Overweight women who gain within or above recommendations were also at increased risk of a 41 week delivery. Finally, obese women were at increased risk of a 41 week delivery with increasing risk with increasing weight (below, within, and above recommendations aOR 1.19, 1.21, and 1.27, respectively).
Conclusion
Elevated prepregnancy weight and weight gain both increase the risk of a postterm delivery. While most women do not receive preconceptional care, restricting weight gain to the within the recommended range can reduce the risk of postterm pregnancy in normal, overweight, and obese women.
Keywords: postterm, prepregnancy weight, prolonged delivery, gestational weight gain
INTRODUCTION
The percentage of pregnant women classified as obese (having a body mass index (BMI) > 29 kg/m2) at their first prenatal visit more than doubled from 1980 to 1999 with more than 35% of pregnant women obese by 1999.1 This high obesity rate has been shown to increase the risk of maternal, labor, and neonatal adverse outcomes including preeclampsia, cesarean section, macrosomia, shoulder dystocia, late fetal death, congenital malformations, meconium aspiration syndrome, and increased neonatal intensive care unit admissions.2–4
Postterm delivery is also associated with increased risk of perinatal complications, including perinatal mortality, birth injury, low Apgar scores, macrosomia, meconium aspiration syndrome, NICU admission, and cesarean delivery.5–8 Although the American College of Obstetricians and Gynecologists (ACOG) currently recommends induction of labor at 42 weeks of completed gestation as a means to reduce the risk of maternal and neonatal complications, the risk for these complications has generally been shown to increase with increasing gestational age after 39 or 40 weeks.5–10 Several large studies found an increase in prolonged pregnancy (41 weeks or beyond) or postterm (42 weeks and beyond) pregnancy in obese women but failed to control for weight gain during the pregnancy.2–4,11–12
Given this background, we sought to estimate the risk of prepregnancy weight and maternal weight gain on delivery rates at or beyond 41 weeks of gestation.
MATERIALS AND METHODS
We conducted a population-based retrospective cohort study of all live, singleton infants born to Missouri residents between 2000 and 2006 and delivered at 37 weeks gestation and beyond. Data were obtained from Missouri birth certificate records linked to hospital discharge data. Both data sources were obtained by the State of Missouri with 100% linkage prior to data sharing. If the birth certificate record and/or the hospital discharge data indicated the presence of a condition (e.g. hypertension), then the condition was considered present. Other factors, such as birth weight and gestational age, were only reported on the birth record.
Exclusion criteria were 1) major congenital anomaly (8181 women), 2) maternal diabetes mellitus (21,394), 3) maternal chronic hypertension (6658), or 4) previous cesarean delivery (66,168). We also excluded infants with a gestational age of 43 weeks or beyond due to potential inaccuracy (13,721). We excluded all births that were missing information on maternal prepregnancy BMI or maternal weight gain (21,072).
The primary exposures of interest were self-reported maternal prepregnancy weight and maternal weight gain obtained from the birth certificate. Prepregnancy weight was categorized based on World Health Organization categories as follows: underweight (BMI <18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2).8 Maternal weight gain was categorized based on the Institute of Medicine (IOM) guidelines as follows: BMI <18.5 kg/m2 may gain 28–40 pounds (lbs), BMI 18.5–24.9 kg/m2 may gain 25–35 lbs, BMI 25–29.9 kg/m2 may gain 15–25 lbs, and BMI ≥30 kg/m2 may gain 11–20 lbs.8 To avoid confounding due to greater weight gain simply from a longer gestation, maternal weight gain per week was calculated as maternal weight gain divided by the length of gestation. Maternal weight gain per week was categorized as above, below, or within the IOM guidelines based on a standard length of gestation from conception to delivery of 38 weeks.
The primary outcome of interest was postterm delivery based on the calculated gestational age. Given the controversy regarding the definition of postterm delivery and to maintain clinical relevance in an era when many clinicians induce labor prior to 42 weeks of gestation, outcomes were reported for infants born at 41 and 42 weeks of gestation.5,10 The calculated gestational age is computer-generated by the State of Missouri Vital Statistics based on the length of pregnancy, birth weight, and clinical estimate per recommendations from the National Center for Health Statistics.13–16 The length of pregnancy is the number of weeks between the date of last menstrual period and date of birth. If the last menstrual period is missing, it is imputed.17,18
Several maternal socio-demographic characteristics that have been shown to be associated with postterm gestation and maternal obesity were evaluated as potential confounders in this study. Maternal education was categorized as high, average, or low based on age and years of education.19 More than 12 years of education was considered high regardless of age. Using the R-GINDEX, prenatal care was categorized as no care, inadequate, adequate, intermediate, intensive, or missing based on when prenatal care was initiated, total number of prenatal care visits, and gestational age at delivery.20
Bivariate analyses were completed using Chi-square tests. Subanalyses were performed for nulliparous and multiparous women, respectively. Multivariable logistic regression was used to calculate adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) for the association between maternal and infant factors and delivery at 41 and 42 weeks gestation. Interactions were noted between prepregnancy BMI and weight gain and kept in the models. Regression models were adjusted for maternal race, age, education, smoking status, prenatal care, insurance status, parity, and infant gender. Mulitcollinearity of prepregnancy BMI and weight gain was ruled out based on a variance inflation factor of 1.05.
We completed stratified regression analyses to evaluate the interaction between prepregnancy BMI and maternal weight gain. In order to assess effect magnitude, calculations were made for the number needed to treat.21 All analyses were completed using SAS version 9.1 (SAS Institute Inc., Cary, NC). Approval for human subjects research and a waiver of informed consent were received from the Institutional Review Board at Saint Louis University and the Missouri Department of Health and Senior Services, Section for Epidemiology for Public Health Practice.
RESULTS
The final study cohort included 339,126 women. 287,706 (84.8%) women delivered at 37 to 40 weeks gestation. 38,028 women (11.2%) delivered at 41 weeks gestation while 13,392 women (4.0%) delivered at 42 weeks gestation. Many women were overweight or obese prior to pregnancy and gained more than the recommended (Table 1). Excess weight gain occurred more often in women with elevated BMI (Table 2).
Table 1.
Population Characteristics (N=339,126)
| Total | Delivery at 41 weeks (38,028, 11.2%) | Delivery at 42 weeks (13.392, 4.0%) | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Characteristic | N | (%)a | N | (%)b | N | (%)c |
| Prepregnancy Weight (kg/m2) | ||||||
| Underweight | 19,354 | (5.7) | 1,930 | (5.1)f | 853 | (6.4)e |
| Normal | 180,056 | (53.1) | 19,621 | (51.6)f | 6866 | (51.3)f |
| Overweight | 76,792 | (22.6) | 8,797 | (23.1)d | 2997 | (22.4) |
| Obese | 62,924 | (18.6) | 7,680 | (20.2) f | 2676 | (20.0) f |
| Maternal weight gain | ||||||
| Below IOM recs | 52,559 | (15.5) | 5,126 | (13.5)f | 1935 | (14.5) f |
| Within IOM recs | 111,386 | (32.9) | 11,572 | (30.4) f | 4094 | (30.6)f |
| Above IOM recs | 175,181 | (51.7) | 21,330 | (56.1) f | 7363 | (55.0) f |
| Maternal race | ||||||
| White | 269,934 | (79.7) | 30,254 | (79.7) | 10,822 | (80.9) f |
| African American | 44,958 | (13.6) | 5022 | (13.2)d | 1685 | (12.6) f |
| Hispanic | 13,710 | (4.1) | 1767 | (4.7) f | 537 | (4.0) |
| Other | 8,961 | (2.7) | 924 | (2.4) e | 327 | (2.5) |
| Maternal Age (years) | ||||||
| < 18 | 14,013 | (4.1) | 1,849 | (4.9) f | 747 | (5.6) f |
| 18- <35 | 294,993 | (87.0) | 33,426 | (87.9) f | 11,719 | (87.5)d |
| ≥ 35 | 30,118 | (8.9) | 2,743 | (7.2) f | 926 | (6.9) |
| Medicaid | 151,839 | (44.9) | 18.373 | (48.5) f | 6968 | (52.2) f |
| Maternal Education | ||||||
| High | 169,350 | (50.3) | 18,002 | (47.6) f | 5696 | (42.8) f |
| Average | 118,956 | (35.3) | 13,957 | (36.9) f | 5217 | (39.2) f |
| Low | 48,667 | (14.4) | 5,829 | (15.4) f | 2404 | (18.1) f |
| Nulliparous | 154,518 | (45.8) | 20,471 | (54.1) f | 6796 | (51.0) f |
| Smoker | 60,114 | (17.7) | 6,939 | (18.3) f | 3010 | (22.5) f |
| Prenatal Care Utilization | ||||||
| Missing | 5,450 | (1.6) | 623 | (1.6) | 198 | (1.5) |
| None | 1,700 | (0.5) | 186 | (0.5) | 81 | (0.6) |
| Inadequate | 15,158 | (4.5) | 2,033 | (5.4) f | 731 | (5.5) f |
| Adequate | 161,975 | (48.0) | 10,298 | (27.1) f | 1942 | (14.5) f |
| Intermediate | 125,173 | (36.9) | 21,900 | (57.6) f | 8805 | (65.8) f |
| Intensive | 22,382 | (6.6) | 2,207 | (5.8) f | 831 | (6.2) d |
| Male infant | 166,849 | (49.2) | 19,378 | (51.0) f | 6860 | (51.2) f |
Percentages total 100% within each characteristic.
Chi-square comparing 41 weeks versus term.
Chi-square comparing 42 weeks versus term.
p<0.05.
p<0.01.
p<0.001
Table 2.
Maternal weight gain by prepregnancy BMI category
| Prepregnancy weight | Maternal Weight Gain
|
|||||
|---|---|---|---|---|---|---|
| Below IOM | Within IOM | Above IOM | ||||
| N | (%)* | N | (%) | N | (%) | |
| Underweight | 4720 | (24.4) | 8866 | (45.8) | 5768 | (29.8) |
| Normal | 30,168 | (16.8) | 70,241 | (39.0) | 79,647 | (44.2) |
| Overweight | 6542 | (8.5) | 18,024 | (23.5) | 52,226 | (68.0) |
| Obese | 11,129 | (17.7) | 14,255 | (22.7) | 37,540 | (60.0) |
Percent across prepregnancy weight category
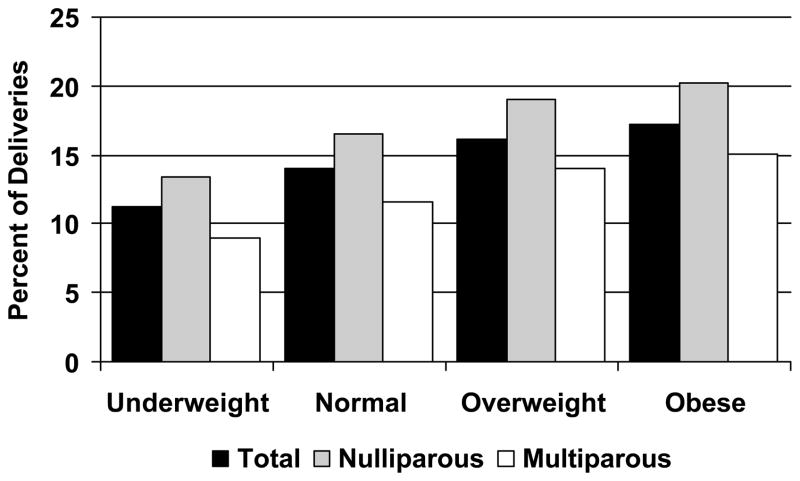
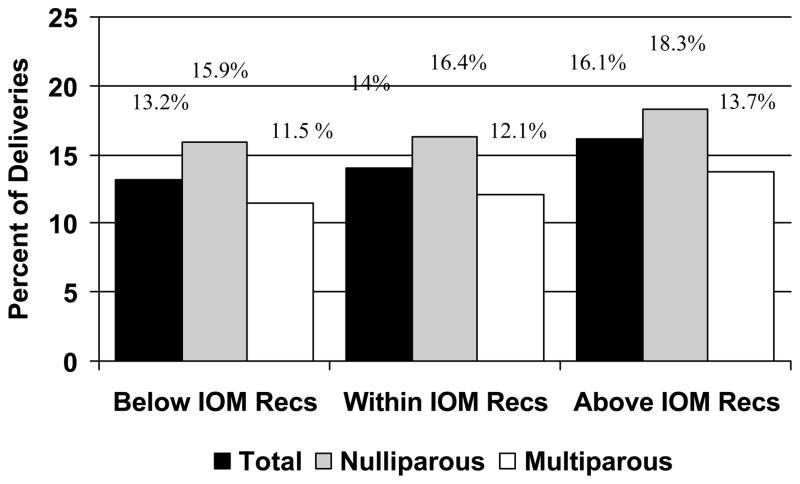
Figure 1 shows the increasing trend in delivery at 41 weeks of gestation with increasing prepregnancy BMI and maternal weight gain overall and for nulliparous and multiparous women (p<0.001). Although it did not reach statistical significance, 4.9% of underweight women delivered at 42 weeks gestation versus 4.3% of normal, 4.4% of overweight, and 4.8% of obese women. The same trend held for increasing weight gain (p<0.001). Similar trends were noted for delivery at 42 weeks’ gestation that did not reach statistical significance (data not shown).
Figure 1.
Figure 1a. Percent of infants born at ≥41 weeks of gestation across maternal BMI category
Figure 1b. Percent of infants born at ≥41 weeks of gestation across maternal weight gain category
When controlling for potential confounders, obese women are at increased risk for postterm delivery (Table 3). In addition, weight gain above the recommendations is also associated with increased risk of postterm delivery except for women who are underweight.
Table 3.
Multivariable Logistic Regression Predicting Delivery at 41 and 42 Weeks Gestation*
| Prepregnancy by Weight Gain | Model 1* | Model 2* | ||
|---|---|---|---|---|
|
| ||||
| Delivery at 41 weeks | Delivery at 42 weeks | |||
| aOR | 95% CI | aOR | 95% CI | |
| Underweight/Below | 0.73 | (0.66, 0.82) | 0.92 | (0.79, 1.09) |
| Underweight/Within | 0.90 | (0.83, 0.97) | 0.96 | (0.86, 1.08) |
| Underweight/Above | 1.01 | (0.92, 1.10) | 1.40 | (1.24, 1.58) |
|
| ||||
| Normal/Below | 0.89 | (0.85, 0.93) | 0.92 | (0.85, 0.99) |
| Normal/Within | referent | referent | ||
| Normal/Above | 1.17 | (1.13, 1.21) | 1.17 | (1.11, 1.24) |
|
| ||||
| Overweight/Below | 0.97 | (0.89, 1.06) | 1.12 | (0.98, 1.27) |
| Overweight/Within | 1.07 | (1.01, 1.13) | 1.07 | (0.98, 1.17) |
| Overweight/Above | 1.20 | (1.16, 1.25) | 1.15 | (1.08, 1.22) |
|
| ||||
| Obese/Below | 1.19 | (1.12, 1.27) | 1.18 | (1.06, 1.31) |
| Obese/Within | 1.21 | (1.14, 1.28) | 1.28 | (1.17, 1.41) |
| Obese/Above | 1.27 | (1.22, 1.33) | 1.24 | (1.16, 1.33) |
Multivariable logistic regression adjusted for maternal race, age, education, smoking status, prenatal care, insurance status, parity, and infant gender
Assuming a causal relationship between maternal prepregnancy weight/weight gain and postterm delivery and given that the adjusted odds ratio is 1.27 for obese women who gain within the recommendations (with a baseline risk of reaching 41 weeks’ gestation for normal women who gain within the recommendations of 18.8%), 32 fewer obese women would prevent one delivery at 41 weeks gestation. 40 normal weight women would need to gain within rather than above the recommendations to prevent 1 delivery at 41 weeks gestation.
COMMENT
High gestational weight gain and elevated prepregnancy BMI were both associated with delivery at 41 weeks of gestation, while weight gain below the IOM guidelines and low prepregnancy BMI reduced the risk of delivery at 41 weeks gestation. Obstetric complications have increased over the last decade as prevalence of maternal obesity has continued to rise.1,11 Since the IOM guidelines were published, concern has been raised about the high upper limit for weight gain recommended in the guidelines.22 Although the recent revised guidelines narrowed the range of weight gain for obese women, the controversy is likely to continue.23 Our study is the first to identify prolonged or postterm delivery as a complication of elevated maternal weight gain regardless of prepregnancy BMI. Although this risk appears to be small, given the prevalence of obesity in the population the benefit of effective interventions may be large. For example, given a number need to treat of 32, a 5% reduction in obesity in this population would have reduced the number of postterm deliveries by almost 100 infants.
Although weight gain below the IOM guidelines was protective of delivery at 41 weeks gestation for normal and underweight women, concern may exist that low weight gain leads to increased risk of other complications. However, previous studies found that weight gain below the IOM guidelines did not increase the risk of infant complications and was even protective of certain adverse infant outcomes such as large-for-gestational age.24–27
The causal link between overweight women and postterm delivery is unclear and may be related to inaccurate dates, variations in care, or an unknown biologic mechanism. Last menstrual period may be an unreliable indicator of length of gestation, particularly in obese women who are at increased risk for abnormal ovulation.28–30 Thus, ultrasound dating early in the first trimester may diminish the increased “risk” of postterm delivery in obese women.31–32 However, inaccurate dating does not explain why women with a normal prepregnancy weight who gain excessive weight are also at increased risk of postterm delivery.
Obese women are at increased risk for maternal complications including chronic hypertension and diabetes; however, we excluded women with these complications and controlled for level of prenatal care. In addition, these patterns were similar when examining individuals who were likely to have undergone an elective induction (data not shown). Physicians may alter the care of obese women, avoiding inductions in the hopes of avoiding cesarean deliveries.33 However, this again does not explain why excessive weight gain in women with normal prepregnancy BMI also increases risk. Thus, there may be a biologic mechanism such as those related to corticotrophin-releasing hormone levels underlying these findings.34–35
These analyses utilize a retrospective cohort of birth certificates and hospital discharge data; reliability and validity, therefore, are a concern. To minimize measurement error and misclassification bias, we used the clinical estimate of gestational age for our outcome measure. Studies have shown that last menstrual period and ultrasound may be unreliable, particularly in obese women, although evidence points to a lengthening of the delivery date which would underestimate rather than overestimate gestational age at delivery biasing towards the null with respect to the analyses presented here.36–37 The primary predictor, prepregnancy weight based on self-report on the birth certificate, has been validated.38–39 There is some concern that overweight and obese women may underestimate their prepregnancy weight which will lead to an overestimate of weight gain in this population.38 This study is limited to term infants because appropriate weight gain for a preterm delivery has not been established preventing the evaluation of preterm delivery as a potential outcome in this study. Finally, although multivariable analyses were utilized to minimize the effect of confounders, potentially unknown or unidentified confounders may exist including maternal medical complications such as lupus and renal disease.
51.7% of the cohort gained more than the IOM recommendations, including 44.2% of women with normal prepregnancy weight, and national data suggests that the rate of excessive weight gain has continued to increase.41 Effective weight loss and weight limiting interventions have been developed and require dissemination and implementation.42–44 Given that the majority of women do not present for preconceptional counseling, efforts by clinicians who care for pregnant women should focus on curtailing excessive weight gain which may decrease the rate of postterm pregnancy and the resulting complications.
Acknowledgments
Financial Support: KL2RR024994
ABBREVIATIONS
- IOM
Institute of Medicine
- BMI
body mass index
- WHO
World Health Organization
Footnotes
Meetings: Presented at the Society for Maternal-Fetal Medicine 2008 annual meeting and the Southern Society for Pediatric Research 2009 annual meeting
References
- 1.Lu GC, Rouse DJ, DuBard M, Cliver S, Kimberlin D, Hauth JC. The effect of the increasing prevalence of maternal obesity on perinatal morbidity. Am J Obstet Gynecol. 2001;185(4):845–9. doi: 10.1067/mob.2001.117351. [DOI] [PubMed] [Google Scholar]
- 2.Usha Kiran TS, Hemmadi S, Bethel J, Evans J. Outcome of pregnancy in a woman with an increased body mass index. BJOG. 2005;112(6):768–772. doi: 10.1111/j.1471-0528.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 3.Stotland NE, Washington AE, Caughey AB. Prepregnancy body mass index and the length of gestation at term. Am J Obstet Gynecol. 2007;197(4):378, e1–5. doi: 10.1016/j.ajog.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 4.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004;103(2):219–24. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 5.Norwitz ER, Snegovskikh VV, Caughey AB. Prolonged pregnancy. When should we intervene? Clin Obstet Gynceol. 2007;50(2):547. doi: 10.1097/GRF.0b013e31804c9b11. [DOI] [PubMed] [Google Scholar]
- 6.Caughey AB, Musci TJ. Complications of term pregnancies beyond 37 weeks of gestation. Obstet Gyencol. 2004;103(1):57–62. doi: 10.1097/01.AOG.0000109216.24211.D4. [DOI] [PubMed] [Google Scholar]
- 7.Caughey AB, Stotland NE, Washington AE, Escobar GJ. Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am J Obstet Gynecol. 2007;196(2):155, e1–6. doi: 10.1016/j.ajog.2006.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894(i-xii):1–253. [PubMed] [Google Scholar]
- 9.Ramos GA, Caughey AB. The interrelationship between ethnicity and obesity on obstetric outcomes. Am J Obstet Gynecol. 2005;193(3 Pt 2):1089–93. doi: 10.1016/j.ajog.2005.06.040. [DOI] [PubMed] [Google Scholar]
- 10.Caughey AB, Bishop JT. Maternal complications of pregnancy increase beyond 40 weeks of gestation in low-risk women. J Perinatol. 2006;26:540–545. doi: 10.1038/sj.jp.7211560. [DOI] [PubMed] [Google Scholar]
- 11.Ehrenberg HM, Dierker L, Milluzzi C, Mercer BM. Prevalence of maternal obesity in an urban center. Am J Obstet Gynceol. 2002;187(5) doi: 10.1067/mob.2002.127125. [DOI] [PubMed] [Google Scholar]
- 12.Sebire NJ, Jolly M, Wadsworth J, Joffe M, Beard RW, Regan L, Robinson S. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obesity. 2001;25:1175–1182. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 13.Qin C, Hsia J, Berg CJ. Variation between last-menstrual-period and clinical estimates of gestational age in vital records. Am J Epidemiol. 2008;167:646–652. doi: 10.1093/aje/kwm345. [DOI] [PubMed] [Google Scholar]
- 14.Mustafa G, David RJ. Comparative Accuracy of Clinical Estimate versus Menstrual Gestational Age in Computerized Birth Certificates. Public Health Rep. 2001;116:15–21. doi: 10.1093/phr/116.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexander GR, Tompkins ME, Petersen DJ, Hulsey TC, Mor J. Discordance between LMP-based and clinically estimated gestational age: implications for research, programs, and policy. Public Health Rep. 1995;110:395–402. [PMC free article] [PubMed] [Google Scholar]
- 16.State of Missouri Department of Health and Senior Services. [accessed September 30, 2009.]; http://www.dhss.mo.gov/LiveBirths/DataElements.html.
- 17.Piper JM, Mitchel EF, Jr, Snowden M, Hall C, Adams M, Taylor P. Validation of 1989 Tennessee birth certificates using maternal and newborn hospital records. Am J Epidemiol. 1993;137:758–768. doi: 10.1093/oxfordjournals.aje.a116736. [DOI] [PubMed] [Google Scholar]
- 18.Cooper WO, Hernandez-Diaz S, Arbogast PG, Dudley JA, Dyer S, Gideon PS, Hall K, Ray WA. Major congenital malformations after first-trimester exposure to ACE inhibitors. New Engl J Medicine. 2006;354:2443–2451. doi: 10.1056/NEJMoa055202. [DOI] [PubMed] [Google Scholar]
- 19.Peterson DJ, Alexander GR. Seasonal variation in adolescent conceptions, induced abortions, and late initiation of prenatal care. Public Health Rep. 1992;107:701–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Alexander GR, Cornely DA. Prenatal care utilization: its measurement and relationship to pregnancy outcomes. Am J Prev Med. 1987;3:243–253. [PubMed] [Google Scholar]
- 21.Wen L, Badgtett R, Cornell J. Number needed to treat: a descriptor for weighing therapeutic options. Am J Health-Syst Pharm. 2005;62:2031–36. doi: 10.2146/ajhp040558. [DOI] [PubMed] [Google Scholar]
- 22.Feig DS, Naylor CD. Eating for two: are guidelines for weight gain during pregnancy too liberal? Lancet. 1998;351:1054–5. doi: 10.1016/S0140-6736(97)06261-2. [DOI] [PubMed] [Google Scholar]
- 23.Rasmussen KM, Yaktine AL, editors. Committee to Reexamine IOM Pregnancy Weight Guidelines, Institute of Medicine, National Research Council. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academy Press; 2009. [Google Scholar]
- 24.Stotland NE, Cheng YW, Hopkins LM, Caughey AB. Gestational weight gain and adverse neonatal outcome among term infants. Obstet Gynecol. 2006;108:635–643. doi: 10.1097/01.AOG.0000228960.16678.bd. [DOI] [PubMed] [Google Scholar]
- 25.Bianco AT, Smilen SW, Davis Y, Lopez S, Lapinski R, Lockwood CJ. Pregnancy outcome and weight gain recommendations for the morbidly obese woman. Obstet Gynecol. 1998;91:97–102. doi: 10.1016/s0029-7844(97)00578-4. [DOI] [PubMed] [Google Scholar]
- 26.Kiel DW, Dodson EA, Artal R, Boehmer TK, Leet TL. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110(4):752–758. doi: 10.1097/01.AOG.0000278819.17190.87. [DOI] [PubMed] [Google Scholar]
- 27.Carmichael SL, Abrams B. A critical review of the relationship between gestational weight gain and preterm delivery. Obstet Gynecol. 1997;80:865–873. doi: 10.1016/s0029-7844(97)00047-1. [DOI] [PubMed] [Google Scholar]
- 28.Kramer MS, McLean FH, Boyd ME, Usher R. The validity of gestational age estimation by menstrual dating in term, preterm, and postterm gestations. JAMA. 1988;260:3306–8. [PubMed] [Google Scholar]
- 29.Harlow SD, Ephross SA. Epidemiology of menstruation and its relevance to women’s health. Epidemiol Rev. 1995;17:265–86. doi: 10.1093/oxfordjournals.epirev.a036193. [DOI] [PubMed] [Google Scholar]
- 30.Nestler JE. Obesity, insulin, sex steroids and ovulation. International J Obesity. 2000;24(2):S71–S73. doi: 10.1038/sj.ijo.0801282. [DOI] [PubMed] [Google Scholar]
- 31.Savitz DA, Terry JW, Dole N, Thorp JM, Siega-Riz AM, Herring AM. Comparison of pregnancy dating by last menstrual period, ultrasound scanning, and their combination. Am J Obstet Gynecol. 2002;187(6):1660–1666. doi: 10.1067/mob.2002.127601. [DOI] [PubMed] [Google Scholar]
- 32.Høgberg U, Larsson N. Early dating by ultrasound and perinatal outcome: a cohort study. Acta Obstet Gynecol Scand. 1997;76:907–12. doi: 10.3109/00016349709034900. [DOI] [PubMed] [Google Scholar]
- 33.Bhattacharya S, Campbell DM, Liston WA, Bhattacharya S. Effect of Body Mass Index on pregnancy outcome in nulliparous women delivering singleton babies. BMC Public Health. 2007;7:168. doi: 10.1186/1471-2458-7-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olson MB, Shaw LJ, Kaizar EE, Kelsey SF, Bittner V, Reis SE, et al. WISE Study Group. Obesity distribution and reproductive hormone levels in women: a report from the NHLBI-sponsored WISE study. J Womens Health (Larchmt) 2006;15(7):836–42. doi: 10.1089/jwh.2006.15.836. [DOI] [PubMed] [Google Scholar]
- 35.Smith R. Mechanisms of Disease: Parturition. N Engl J Med. 2007;356:271–83. doi: 10.1056/NEJMra061360. [DOI] [PubMed] [Google Scholar]
- 36.Simic M, Wåhlin IA, Marsál, Källén K. Maternal obesity is a potential source of error in mid-trimester ultrasound estimation of gestational age. Ultrasound Obstet Gynecol. 2010;35(1):48–53. doi: 10.1002/uog.7502. [DOI] [PubMed] [Google Scholar]
- 37.Brewer CJ, Balen AH. The adverse effects of obesity on conception and implantation. Reproduction. 2010;140:347–364. doi: 10.1530/REP-09-0568. [DOI] [PubMed] [Google Scholar]
- 38.Lederman SA, Paxton A. Maternal reporting of prepregnancy weight and birth outcome: consistency and completeness compared with the clinical records. Matern Child Health J. 1998;2:123–126. doi: 10.1023/a:1022996924094. [DOI] [PubMed] [Google Scholar]
- 39.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 40.Stevens-Simon C, Roghmann KJ, McAnarney ER. Relationship of self-reported prepregnant weight and weight gain during pregnancy to maternal body habitus and age. J Am Diet Assoc. 1992;92:85–87. [PubMed] [Google Scholar]
- 41.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. 2003;52:1–113. [PubMed] [Google Scholar]
- 42.Tsai AG, Wadden TA. Systematic review: An evaluation of major commercial weight loss programs in the United States. Ann Intern Med. 2005;142:56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 43.Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gyn. 2004;191:530–536. doi: 10.1016/j.ajog.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 44.Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes. 2002;26:1494–502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]