Abstract
Background
Gender divergence on the impact of multiple cardiovascular (CV) risk factors on the femoral artery intima-media thickness (IMT) has not studied in a biracial (black-white) community based asymptomatic young adults.
Methods
Femoral IMT was measured by B-mode ultrasonography in 1080 individuals (aged 24- 43 years; 71%white, 43% male) enrolled in the Bogalusa Heart Study.
Results
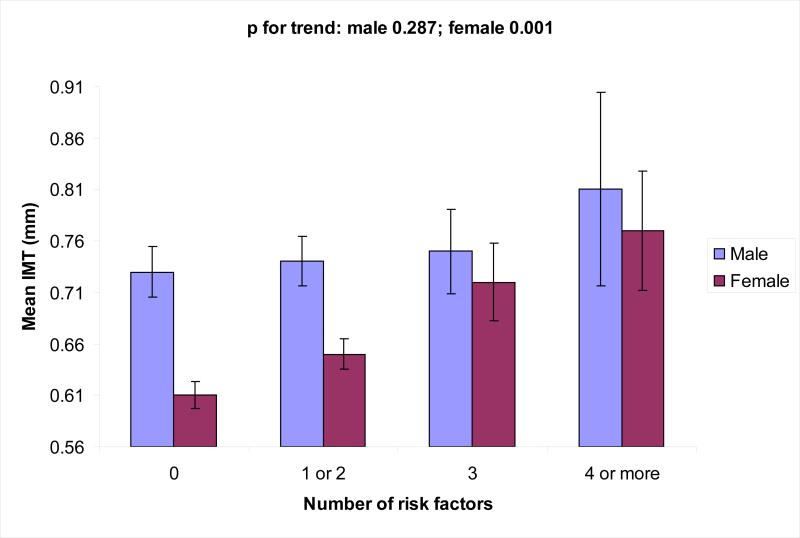
Femoral IMT showed a gender difference (males > females, p= 0.001), but no racial difference. In a multivariate model, age, cigarette smoking, systolic blood pressure and total to HDL cholesterol ratio related independently, in that order, to IMT in females; age and LDL cholesterol in males. In females, mean IMT increased with increasing number of risk factors defined as values above the age- race- and gender- specific 75th percentile of systolic blood pressure, waist circumference, total to HDL cholesterol ratio and insulin along with positive smoking status (p for trend = 0.001), with respective mean IMT (mm) values of 0.61, 0.65, 0.72, and 0.77, for 0, 1-2, 3 and 4-5 risk factors. There was no such significant trend in males.
Conclusions
Although males vs females had thicker IMT, the observed increasing trend of femoral IMT with increasing number of risk factors in asymptomatic young females suggests that females may be relatively more susceptible to the burden of multiple risk factors.
Keywords: Femoral artery, intima-media thickness, risk factors, gender difference, ultrasonography
Introduction
Peripheral arterial disease (PAD) is a clinical manifestation of atherosclerosis that causes significant morbidity and mortality from cardiovascular (CV) diseases.1 PAD is common in older adults, mostly asymptomatic, but is associated with clinically manifest CV diseases 2. In general the prevalence of PAD is over 10% in individuals aged more than 60 years old 3. Specifically, the prevalence of lower extremity PAD based on ankle-brachial index is approximately 10% to 20% of community dwelling individuals aged 65 and older.4 Males in general are considered to have more PAD than females.2,3 Although PAD is a leading cause of death and disability, it is under recognized and under-treated 3 especially in women in general medical practice.5
Epidemiologic studies such as the Framingham study have emphasized the importance of multiple risk factors profile in the prediction and prevention of CV diseases.6 Although the clinical manifestations of CV diseases occur during and after middle age, autopsy studies in youth have shown that CV risk factors are related to the early stages of coronary atherosclerosis7,8 Importantly, the extent of atherosclerosis increases markedly with multiple risk factors.9,17 It has also been shown that coronary artery disease risk factors are also associated with PAD.10,15 Carotid and femoral artery intima-media thickness (IMT) are considered surrogate indicators of atherosclerotic coronary and peripheral vascular diseases in middle-aged and older adults.11-14
Manifestations of PAD in relation to CV risk factors have been studied by ultrasound - assessed carotid and femoral artery IMT mainly in middle-aged and older adults.10-12 However, little is known on the impact of multiple CV risk factors on the femoral IMT in young adults by gender. The present study investigated whether gender influences the impact of multiple CV risk factors on the femoral artery IMT in the Bogalusa Heart Study cohort.
Methods
Study Subjects
As part of the adult survey, 1080 subjects, aged 24-43 years (71% white, 43% male) residing in the semi-rural biracial (65% white, 35% black) community of Bogalusa, Louisiana were examined in 2001-2002. Tulane University Health Sciences Center Institutional Review Board approved the study. Informed consent was obtained from all participants.
General Examination
Trained field observers followed standardized protocols as described previously.16,18 Duplicate measurements of height to the nearest 0.1 cm and weight to the nearest 0.1 kg were made and the mean values were used to calculate body mass index (BMI= weight in kilograms divided by the square of the height in meters, wt/ ht2) as a measure of overall adiposity. Mean values of waist circumference measured in triplicate were used as an indicator of visceral fatness. Measurements of right upper arm length and circumference were used for proper blood pressure cuff size selection. Two randomly assigned observers measured blood pressure (3 measurements each) using the right arm of subjects, seated and relaxed. Systolic and diastolic blood pressure levels were recorded as the first and fifth korotkoff phases using mercury sphygmomanometers. Blood pressure levels were reported as the mean of 6 replicate measurements. Information on smoking status (yes/no) was obtained as part of a medical / health habit questionnaire. Individuals were considered smokers if they reported current use of cigarettes or having stopped smoking within the past year.
Laboratory Analysis
Subjects were instructed to fast for 12 hours and the compliance was determined by interviewing on the morning examination. Serum cholesterol and triglycerides levels were assayed using an enzymatic procedure on the Hitachi 902 automatic Analyzer (Roche Diagnostics, Indianapolis, IN). Serum lipoprotein cholesterol levels were analyzed by a combination of heparin-calcium precipitation and agar-agarose gel electrophoresis procedures.19 The laboratory has been monitored for precision and accuracy by the Lipid Standardization and Surveillance Program of the Center for Disease Control and Prevention (Atlanta, Georgia). A commercial radioimmunoassay kit was used for measuring plasma immunoreactive insulin levels (Phadebas insulin kit; Pharmacia Diagnostics, Piscataway, NJ). Plasma glucose levels were measured as part of a multiple chemistry profile (SMA20) by a glucose oxidase method.
Femoral Ultrasonography
Trained sonographers performed B-mode ultrasound examinations with a Toshiba Sonolayer SSH160A (Toshiba Medical, Tokyo, Japan) equipped with a 7.5-MHz linear array transducer on subjects in the supine position. Images of maximum far wall IMTs were recorded at left common femoral artery according to previously developed protocols as for carotid vessels in the Atherosclerosis Risk in Communities Study.20 Images were recorded on super VHS tapes and read by certified readers from the Vascular Ultrasound Research Laboratory using a semiautomatic ultrasound image processing program developed by the California Institute of Technology Jet Propulsion Laboratory (Pasadena California) according to strict protocols.20,21 Duplicate measurements on 69 subjects showed correlation coefficients of 0.63, p = 0.0001.
Statistical Analyses
All statistical analyses were performed using SPSS system version 12.0 for Windows. All p values were 2 tailed. Femoral artery IMT measurements, triglycerides, insulin and glucose were log transformed to reduce skewness. Differences between groups’ means were assessed using independent t–test or ANOVA as appropriate. After assessing the interaction between gender and risk factors, analysis was performed stratified by gender.
Analysis of covariance controlling for age was used to assess the gender differences in IMT and CV risk factor variables. Post hoc tests used the Sidak method for multiple comparisons when appropriate. Partial Pearson correlation coefficients were used to assess the bivariate relation between IMT and risk factor variables, controlling for age and race. Chi-squire test was used for categorical variables to assess the gender differences.
Stepwise linear regression methods were used to assess the independent relation between risk factor variables and femoral IMT using significance levels to enter 0.05 and to stay within 0.10. Multiple regression analysis was performed stratified by gender. Independent variables included age, race, BMI, waist circumference, systolic and diastolic blood pressure, LDL cholesterol, HDL cholesterol, total cholesterol to HDL cholesterol ratio, log triglycerides, log insulin and cigarette smoking (yes or no).
The effect of multiple risk factors on IMT of femoral artery was examined by comparing the mean IMT values of individuals with 0, 1or 2, 3, and 4 or more risk factors in males and females. Risk factors included cigarette smoking, and adverse levels of total cholesterol to HDL cholesterol ratio, insulin level, waist circumference and systolic blood pressure. The adverse levels were defined as age-, race-, gender- specific values above the 75th percentiles for the study group. Linear trend tests were used to assess the impact of multiple risk factors on IMT of femoral artery.
Results
The mean levels of anthropometric, hemodynamic and metabolic variables in the study cohort by race and gender are listed in Table 1. BMI was higher in black females than white females, while waist circumference was higher in white males than white females. Males vs females and blacks vs whites displayed higher systolic and diastolic blood pressure, LDL cholesterol, total cholesterol to HDL cholesterol ratio and glucose. Females vs males and blacks vs whites had lower triglycerides. White males vs white females and white males vs black males showed lower HDL cholesterol. There was no significant difference in age, insulin and smoking status. Mean and selected percentiles of femoral artery IMT by race and gender are presented in Table 2. Age-adjusted femoral IMT showed gender difference (males > females, p = 0.001) only among whites and no race difference in both genders. Partial correlations between CV risk variables and femoral IMT (adjusted for age and race) are listed in Table 3. In general, bivariate correlations are greater in females. In females, IMT was significantly and positively associated with BMI, waist circumference, systolic blood pressure, diastolic blood pressure, LDL cholesterol, total cholesterol to HDL cholesterol ratio and triglycerides. In females IMT was inversely correlated with HDL cholesterol. The magnitude of correlation was relatively higher between blood pressure and IMT. Only systolic blood pressure and LDL cholesterol were correlated with IMT in males. Most CV risk factor variables were significantly correlated with femoral IMT in females, with the exception of insulin and glucose. Insulin and glucose were not significantly associated with IMT in either males or females.
Table 1.
Anthropometric, hemodynamic, and metabolic characteristics of study cohort by race and gender. The Bogalusa Heart Study
| Comparison* |
||||||
|---|---|---|---|---|---|---|
| Variables† | White male (n = 348) | Black Male (n = 117) | White Female (n = 419) | Black Female (n = 196) | Race | Gender |
| Age (years) | 36.7 ± 4.3 | 36.6 ± 4.3 | 36.5 ± 4.3 | 35.6 ± 4.7 | ns | ns |
| BMI (kg/m2) | 29.0 ± 5.6 | 29.3 ± 7.2 | 28.3 ± 6.9 | 31.2 ± 8.1 | 0.001b | ns |
| Waist (cm) | 99.0 ± 14 | 96.4 ± 18 | 87.0 ± 16 | 92.9 ± 17 | ns | 0.0001a |
| Systolic BP (mmHg) | 118 ± 11 | 128 ± 17 | 111 ± 11 | 119 ± 16 | 0.0001 | 0.0001 |
| Diastolic BP (mm Hg) | 74.7 ± 8.2 | 80.7 ± 13 | 69.9 ± 9.0 | 74.1 ± 11 | 0.0001 | 0.0001 |
| LDL cholesterol (mg/dl) | 130 ± 35 | 127 ± 45 | 124 ± 32 | 115 ± 31 | 0.005 | 0.001 |
| HDL cholesterol (mg/dl) | 41.5 ± 12 | 49.8 ± 16 | 50.6 ± 13 | 52.0 ± 13 | 0.0001c | 0.0001a |
| Triglycerides (mg/dl) | 166 ± 131 | 122 ± 81 | 124 ± 74 | 87.8± 37 | 0.0001 | 0.0001 |
| Total / HDL chol. | 4.99 ± 1.5 | 4.21 ± 1.5 | 4.03 ± 1.2 | 3.63 ± 1.1 | 0.0001 | 0.0001 |
| Insulin (μU/ml) | 13.2 ± 10 | 12.0 ± 9.7 | 11.5 ± 8.3 | 15.5 ± 20 | ns | ns |
| Glucose (mg/dl) | 87.5 ± 19 | 91.3 ± 34 | 82.8 ± 18 | 87.3 ± 30 | 0.01 | 0.0001 |
| Smoking (%) | 32.5 | 41.9 | 32.5 | 35.2 | ns | ns |
values for continuous variables are mean ± SD
Analysis of Covariance (p value adjusted for age).
whites only
females only
males only
ns, not significant; BP, blood pressure.
BMI, body mass index; LDL, low density lipoprotein; HDL, high density lipoprotein.
Table 2.
Mean (± SD) and selected percentiles of femoral artery intima-media thickness in young adults by race and gender
| Race/gender | Mean ± SD (mm) | Selected Percentiles | ||||
|---|---|---|---|---|---|---|
| 5th | 10th | 50th | 90th | 95th | ||
| White male (n =348)a | 0.75±0.37 | 0.47 | 0.49 | 0.66 | 1.05 | 1.37 |
| Black male (n =117) | 0.70±0.19 | 0.49 | 0.53 | 0.68 | 0.88 | 1.06 |
| White female (n =419)a | 0.64±0.26 | 0.43 | 0.46 | 0.57 | 0.88 | 1.18 |
| Black female (n =196) | 0.66±0.22 | 0.44 | 0.46 | 0.60 | 0.91 | 1.15 |
| Total (n =1080) | 0.69±0.29 | 0.44 | 0.47 | 0.61 | 0.96 | 1.19 |
males > females among whites (adjusted for age); p = 0.001
SD, standard deviation.
Table 3.
Partial correlation coefficients between intima-media thickness of femoral artery and cardiovascular risk factor variables in study cohort by gender
| Male* | Female* | |
|---|---|---|
| BMI | 0.01 | 0.12b |
| Waist | -0.002 | 0.14c |
| Systolic BP | 0.10a | 0.19c |
| Diastolic BP | 0.07 | 0.15c |
| LDL cholesterol | 0.09a | 0.08a |
| HDL cholesterol | -0.004 | - 0.10a |
| Triglycerides | 0.02 | 0.13b |
| Total cholesterol /HDL cholesterol | 0.04 | 0.13b |
| Insulin | - 0.02 | 0.02 |
| Glucose | -0.04 | -0.02 |
Adjusted for age and race.
p <0.05
p < 0.01
p < 0.001.
BP, blood pressure, BMI, body mass index; LDL, low density lipoprotein.
HDL, high density lipoprotein.
Predictor variables of IMT of femoral artery by gender are listed in Table 4. In both males and females, age was the major contributor to the explained variance of IMT followed by cigarette smoking, systolic blood pressure and total cholesterol to HDL cholesterol ratio, in that order in females; LDL cholesterol in males. The independent variables listed explained 9% in females vs 5% in males of the variability in femoral IMT.
Table 4.
Predictors of intima-media thickness of femoral artery in young adults by gender
| Male | Female | ||||||
|---|---|---|---|---|---|---|---|
| Predictors | Beta-coefficient | Partial R2 | P value | Predictors | Beta-coefficient | Partial R2 | P value |
| Age (years) | 0.015 | 0.043 | 0.0001 | Age (years) | 0.009 | 0.049 | 0.0001 |
| LDL chol | 0.001 | 0.008 | 0.049 | Smoking | 0.041 | 0.018 | 0.001 |
| Systolic BP(mmHg) | 0.004 | 0.017 | 0.0001 | ||||
| Total/HDL | 0.021 | 0.007 | 0.036 | ||||
| Total R2 = 0.05 | Total R2 = 0.09 | ||||||
Stepwise regression model included age (years), race, waist circumference, BMI, systolic and diastolic blood pressure, log insulin, log triglycerides, LDL cholesterol, HDL cholesterol, total cholesterol / HDL cholesterol ratio and cigarette smoking (yes/no).
Note the contrast of smoking and systolic BP in females compared to males.
BP, blood pressure (mmHg); LDL, low density lipoprotein; HDL, high density lipoprotein.
The unit of cholesterol measurements is mg/dl.
The effect of multiple risk factors on IMT of femoral artery in males vs females is shown in Figure 1. There was no significant increasing trend of IMT seen with increasing number of risk factors in males; in contrast, for females mean IMT increased with increasing number of risk factors defined as values above the age-, race-, and gender- specific 75th percentile of systolic blood pressure, waist circumference, total cholesterol to HDL cholesterol ratio and insulin along with cigarette smoking (p for trend = 0.001).
Figure 1.
The effect of multiple risk factors on intima-media thickness (IMT) of femoral artery in males and females. A highly significant trend of increasing thickness is shown with greater number of risk factors in females. No such trend of increasing thickness is shown in males. Risk factors included were total cholesterol to HDL cholesterol ratio, waist circumference, systolic blood pressure, insulin level (>75th percentile specific for age, race, gender) and smoking. HDL, high density lipoprotein. Bar represents standard error of mean.
Discussion
The present study shows significant gender divergence on the impact of multiple CV risk factors on the femoral IMT in asymptomatic healthy younger adults. Age, cigarette smoking, systolic blood pressure and total cholesterol to HDL cholesterol ratio are independent predictors of the femoral artery IMT in females; whereas age and LDL cholesterol only are predictors of IMT in males. Further, females with multiple CV risk factors displayed increased IMT of femoral artery in contrast to males, although greater overall thickness of femoral arteries was noted in males. These observed associations in females, within a large sample of community-based cohort, free from the selection bias of a patient population, are indicative of the burden of multiple CV risk factors on the early stages of atherosclerosis in extra coronary arteries and, by inference, coronary arteries. The noninvasive ultrasonographic evaluation of femoral IMT in this study expands earlier autopsy findings from the Bogalusa Heart Study and the Pathobiological Determinants of Atherosclerosis in Youth Study, showing a strong association between traditional CV risk factors and early phases of atherosclerosis in young adults.8,9 Young females had a greater extent of fatty streaks in the abdominal aorta than males but the same extent of raised lesions.8 Females and males had a similar extent of fatty streaks in the right coronary artery, but females had much less extensive raised lesions.8 In these studies, aorta and coronary artery lesions lagged in severity in females than males. It needs to be determined if the observed increasing trend of IMT with greater number of risk factors in the premenopausal setting, is the stage for greater clinical atherosclerotic events in post menopausal females.
The observed independent associations of age, cigarette smoking, systolic blood pressure and total cholesterol to HDL cholesterol ratio with IMT in females are in expected directions and consistent with previous findings made primarily in middle-aged and older populations.22 Of particular interest, the measured risk factors in multivariate analysis contributed relatively more in the variance of IMT in females compared to males (9% vs 5%). This suggests variations in susceptibility to IMT of femoral artery and to the extent of atherosclerosis in lower extremities between males and females as affected by risk factors in general. The observed increasing trend of IMT with increasing number of CV risk factors in females indicates that females may be more susceptible than males to vascular changes related to risk factors even though cardiac events are greater in males at a younger age.
The findings of this study that the femoral IMT increased considerably in asymptomatic, younger female adults with multiple CV risk factors support the concept of the importance of multivariate risk profile and the attendant accelerated atherosclerosis systemically. Multiple risk factors are established for its clinical manifestations in middle-aged and older populations as enunciated by the Framingham Study.6 The traditional CV risk factors evaluated in this study related to metabolic syndrome, with the exception of cigarette smoking which are found at the high risk group are patho-physiologically related and coexist frequently in youth.23 The multiple risk factors included smoking which also has an effect on atherosclerotic disease. The observed deleterious impact of multiple risk factors on the femoral IMT in females parallel the earlier autopsy results showing marked increases in the extent of coronary atherosclerosis in young subjects with increasing number of risk factors but with a lag in severity in females.9
In bivariate analysis, triglycerides was associated with femoral IMT in females. Findings from the other studies suggest an association between triglycerides and carotid IMT in women but not in men, 24 although some inconsistent association has been reported.25 It is known that diabetes greatly accelerates peripheral vascular disease and the significant correlation of risk factors associated with metabolic syndrome such as obesity, systolic blood pressure, total cholesterol to HDL cholesterol ratio, and triglycerides with IMT in this study of young female adults can be a subtle predictor of future disease at this site. Despite the less severity of atherosclerosis in females, the trend of acceleration of IMT related to multiple risk factors is greater in females.
Systolic blood pressure is consistently related to IMT independent of age in previous studies.24 In this study, although males had thicker IMT than females, interestingly, systolic blood pressure is not the predictor of femoral IMT in males. In females, smoking, systolic blood pressure and total cholesterol to HDL cholesterol ratio are significant in predicting IMT of femoral artery. This implies that in females, hemodynamic factors such as shear stress and atherogenic burden from increased total cholesterol to HDL cholesterol ratio are determinants of subclinical atherosclerosis. It has been shown that females especially white females are more closely related with unfavorable arterial hemodynamics and related arterial stenosis.26 Such changes is noted in this study may relate to hemodynamic effects on arterial structure changes including endothelial and IMT changes related to smaller diameter vessels in women.
Further, studies showed smoking is associated with IMT, particularly with carotid IMT and PAD, as well as with coronary artery disease in males and females.24 Smoking was associated with more extensive fatty streaks and raised lesions in the abdominal aorta but the effect of smoking was similar in males and females.8 Although there are conflicting results regarding the effect of smoking on IMT in women, results are consistent in males in this regard.27 However, results from the present study indicate that smoking is a significant predictor of femoral IMT in females not in males. The pathophysiology of this association is not clear as there is no significant difference in cigarette smoking status in males and females in this study.
Studies suggest that gender difference in atherosclerosis differ in vascular sites; greater in coronary vessels than in other vascular beds 28,29 remarkably, the differences in the aorta and the arteries of the lower extremities are virtually absent.28 But our study shows that there is a significant gender difference on the impact of multiple CV risk factors on femoral IMT, a surrogate indicator of lower extremity atherosclerosis. The different mechanism (s) underlying the observed male-female divergence on the impact of multiple CV risk factors on femoral IMT remain to be established. Gender specific hemodynamic and metabolic characteristics likely contribute to the observed divergences. Further, genetic and socioeconomic factors may also play a role in this regard.30
Atherosclerosis is a gradually progressive phenomenon and single measurements of CV risk factors with IMT may not truly reflect an individual's past exposure to risk factors.24 Studies of IMT at one site like the femoral may only reflect symptoms from local atherosclerosis rather than generalized atherosclerosis. The changes may not reflect the end event from the extensive atherothrombotic process such as occurs to produce clinical coronary artery disease or of more proximal abdominal aorta-iliac-femoral changes. Yet, ultrasonography of the femoral arteries is practical and provides a noninvasive and relatively inexpensive method to assess systemic atherosclerosis.
Compared with the carotid artery, the femoral artery is more difficult to examine because of the location, especially in obese subjects. Having measurement of only one femoral arterial site is a limitation of the current study. Lack of power analysis to specifically show the differences on the impact of the CV risk factors on femoral IMT in asymptomatic males and females is another limitation of the current study. Furthermore, specific power analysis was not performed to examine whether the risk factors have similar or differential impact on IMT.
In conclusion, the impact of CV risk factors on femoral IMT, a surrogate measure of atherosclerosis was found to be greater in females. Although males vs females had thicker IMT, the observed increasing trend of femoral IMT with increasing number of risk factors in asymptomatic younger female adults suggests that females are relatively more susceptible to the atherosclerotic effect of risk factors including effects of diabetes. These results indicate that gender should be considered in CV risk profiling.
Acknowledgements
The Bogalusa heart Study is a joint effort of many individuals whose cooperation is gratefully acknowledged. We especially thank the participants of this study.
This study was supported by grants HD-061437 and HD-062783 from the National Institute of Child Health and Human Development, 0855082E from American Heart Association, and AG-16592 from the National Institute on Aging.
Footnotes
Disclosure: The authors declared no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326(6):381–386. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 2.Newman AB, Siscovick DS, Manolio TA, et al. Atherosclerosis: Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Circulation. 1993;88(3):837–845. doi: 10.1161/01.cir.88.3.837. [DOI] [PubMed] [Google Scholar]
- 3.Criqui MH. Peripheral arterial disease-epidemiological aspects. Vasc Med. 2001;6(3 Suppl):3–75. doi: 10.1177/1358836X0100600i102. [DOI] [PubMed] [Google Scholar]
- 4.Schroll M, Munck O. Estimation of peripheral arteriosclerotic disease by ankle blood pressure measurements in a population study of 60 year-old men and women. J Chronic Dis. 1981;34:261–269. doi: 10.1016/0021-9681(81)90031-x. [DOI] [PubMed] [Google Scholar]
- 5.McDermott MM, Kerwin DR, Liu K, et al. Prevalence and significance of unrecognized lower extremity peripheral arterial disease in general medicine practice. J Gen Intern Med. 2001;16:384–390. doi: 10.1046/j.1525-1497.2001.016006384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kannel WB. Contributions of the Framingham Study to the conquest of coronary artery disease. Am J Cardiol. 1988;62:1109–1112. doi: 10.1016/0002-9149(88)90558-9. [DOI] [PubMed] [Google Scholar]
- 7.Newman WP, III, Freedman DS, Voors AW, et al. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. N Eng J Med. 1986;314:138–144. doi: 10.1056/NEJM198601163140302. [DOI] [PubMed] [Google Scholar]
- 8.McGill HC, Jr, McMahan CA, Malcom GT, et al. Effects of serum lipoproteins and smoking on atherosclerosis in young men and women. The PDAY Research Group. Pathobiological Determinants of atherosclerosis in Youth. Arterioscler Thromb Vasc Biol. 1997;17:95–106. doi: 10.1161/01.atv.17.1.95. [DOI] [PubMed] [Google Scholar]
- 9.Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 10.Grobbee DE, Bots ML. Carotid artery intima-media thickness as an indicator of generalized atherosclerosis. J Intern Med. 1994;236:567–573. doi: 10.1111/j.1365-2796.1994.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 11.Allan PL, Mowbray PI, Lee AJ, et al. Relationship between carotid intima-media thickness and symptomatic and asymptomatic peripheral arterial disease: The Edinburgh Artery Study. Stroke. 1997;28:348–353. doi: 10.1161/01.str.28.2.348. [DOI] [PubMed] [Google Scholar]
- 12.Suurkula M, Fagerberg B, Wendelhag I, et al. Atherosclerotic disease in the femoral artery in hypertensive patients at high cardiovascular risk. The value of ultrasonographic assessment of intima-media thickness and plaque occurrence. Risk Intervention Study (RIS) Group. Arterioscler Thromb Vasc Biol. 1996;16:971–977. doi: 10.1161/01.atv.16.8.971. [DOI] [PubMed] [Google Scholar]
- 13.Burke GL, Evans GW, Riley WA, et al. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults: the Atherosclerosis (ARIC) Study Investigators. Stroke. 1995;26:386–391. doi: 10.1161/01.str.26.3.386. [DOI] [PubMed] [Google Scholar]
- 14.Crouse JR, III, Tang R, Espeland MA, et al. Associations of extra cranial carotid atherosclerosis progression with coronary status and risk factors in patients with and without coronary artery disease. Circulation. 2002;106:2061–2066. doi: 10.1161/01.cir.0000033833.54884.34. [DOI] [PubMed] [Google Scholar]
- 15.Wendelhag I, Wiklund O, Wikstrand J. Atherosclerotic changes in the femoral and carotid arteries in familial hypercholesterolemia. Ultrasonographic assessment of intima-media thickness and plaque occurrence. Arterioscler Thromb. 1993;13:1404–1411. doi: 10.1161/01.atv.13.10.1404. [DOI] [PubMed] [Google Scholar]
- 16.The Bogalusa Heart Study 20th Anniversary Symposium. Am J Med Sci. 1995;(suppl. 1):S1–S38. doi: 10.1097/00000441-199512000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Paul TK, Srinivasan SR, Chen W, et al. Impact of multiple cardiovascular risk factors on the femoral artery intima-media thickness in asymptomatic young adults: The Bogalusa Heart Study. Am J Cardiol. 2005;95:469–473. doi: 10.1016/j.amjcard.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Berenson GS, McMahon CA, Voors AW. Cardiovascular risk factors in Children: The Early Natural History of Atherosclerosis and Essential Hypertension. Oxford University Press; New York: 1980. p. 450. [Google Scholar]
- 19.Srinivasan SR, Berenson GS. Serum lipoproteins in children and methods for study. In: Lews LA, editor. Handbook of Electrophoresis. CRC; Boca Raton. FL: 1983. pp. 185–204. [Google Scholar]
- 20.Bond MG, Barnes RW, Wiley WA, et al. High-resolution B-mode ultrasound reading methods in the Atherosclerosis Risk in Communities (ARIC) cohort. The ARIC Study Group. J Neuroimaging. 1991;1:68–73. 168–172. [PubMed] [Google Scholar]
- 21.Tang R, Hennig M, Thomasson B, et al. Baseline reproducibility of B mode ultrasonic measurement of carotid artery intima-media thickness: the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens. 2000;18:197–201. doi: 10.1097/00004872-200018020-00010. [DOI] [PubMed] [Google Scholar]
- 22.Gariepy J, Simon A, Massonneau M, et al. Groupe PCVMETRA. Echographic assessment of carotid and femoral arterial structure in men with essential hypertension. Am J Hyperten. 1996;9:126–136. doi: 10.1016/0895-7061(95)00262-6. [DOI] [PubMed] [Google Scholar]
- 23.Bao W, Srinivasan SR, Wattigney WA, et al. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart Study. Arch Intern Med. 1994;154:1842–1847. [PubMed] [Google Scholar]
- 24.Stensland-Bugge E, Bonaa KH, Joakimsen O, et al. Sex differences in the relationship of risk factors to subclinical carotid atherosclerosis measured 15 years later. The Tromso Study. Stroke. 2000;31:574–581. doi: 10.1161/01.str.31.3.574. [DOI] [PubMed] [Google Scholar]
- 25.Heiss G, Sharrett AR, Barnes R, et al. Carotid atherosclerosis measured by B mode ultrasound in populations: associations with cardiovascular risk factors in the ARIC study. Am J Epidemiol. 1991;134:250–256. doi: 10.1093/oxfordjournals.aje.a116078. [DOI] [PubMed] [Google Scholar]
- 26.Iemolo F, Martiniuk A, Steinman Da, et al. Sex differences in carotid plaque and stenosis. Stroke. 2004;35:477–481. doi: 10.1161/01.STR.0000110981.96204.64. [DOI] [PubMed] [Google Scholar]
- 27.Gariepy J, Salomon J, Denarie N, et al. Sex and topographic differences in association between large artery wall thickness and coronary risk profile in a French working cohort: the AXA study. Arterioscler Thromb Vasc Biol. 1998;18:584–590. doi: 10.1161/01.atv.18.4.584. [DOI] [PubMed] [Google Scholar]
- 28.Kardys I, Vliegenthart R, Oudkerk M, et al. The female advantage in cardiovascular disease: do vascular beds contribute equally? Am J Epidemiol. 2007;166(4):403–412. doi: 10.1093/aje/kwm115. [DOI] [PubMed] [Google Scholar]
- 29.Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26 year follow-up of the Framingham population. Am Heart J. 1986;111:383–390. doi: 10.1016/0002-8703(86)90155-9. [DOI] [PubMed] [Google Scholar]
- 30.Winkleby MA, Kraemer HC, Ahn DK, et al. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third national Health and Nutrition examination Survey, 1988-1994. JAMA. 1998;280:356–362. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]