Abstract
Background
Enterococcus faecalis and Enterococcus faecium are associated with faecal pollution of water, linked to swimmer-associated gastroenteritis and demonstrate a wide range of antibiotic resistance. The Coomera River is a main water source for the Pimpama-Coomera watershed and is located in South East Queensland, Australia, which is used intensively for agriculture and recreational purposes. This study investigated the diversity of E. faecalis and E. faecium using Single Nucleotide Polymorphisms (SNPs) and associated antibiotic resistance profiles.
Results
Total enterococcal counts (cfu/ml) for three/six sampling sites were above the United States Environmental Protection Agency (USEPA) recommended level during rainfall periods and fall into categories B and C of the Australian National Health and Medical Research Council (NHMRC) guidelines (with a 1-10% gastrointestinal illness risk). E. faecalis and E. faecium isolates were grouped into 29 and 23 SNP profiles (validated by MLST analysis) respectively. This study showed the high diversity of E. faecalis and E. faecium over a period of two years and both human-related and human-specific SNP profiles were identified. 81.8% of E. faecalis and 70.21% of E. faecium SNP profiles were associated with genotypic and phenotypic antibiotic resistance. Gentamicin resistance was higher in E. faecalis (47% resistant) and harboured the aac(6')-aph(2') gene. Ciprofloxacin resistance was more common in E. faecium (12.7% resistant) and gyrA gene mutations were detected in these isolates. Tetracycline resistance was less common in both species while tet(L) and tet(M) genes were more prevalent. Ampicillin resistance was only found in E. faecium isolates with mutations in the pbp5 gene. Vancomycin resistance was not detected in any of the isolates. We found that antibiotic resistance profiles further sub-divided the SNP profiles of both E. faecalis and E. faecium.
Conclusions
The distribution of E. faecalis and E. faecium genotypes is highly diverse in the Coomera River. The SNP genotyping method is rapid and robust and can be applied to study the diversity of E. faecalis and E. faecium in waterways. It can also be used to test for human-related and human-specific enterococci in water. The resolving power can be increased by including antibiotic-resistant profiles which can be used as a possible source tracking tool. This warrants further investigation.
Background
Poor microbiological quality of water results from contamination by microorganisms of human or animal origin and leads to the risk of gastro-enteritis in humans [1,2]. The assurance of the microbiological quality of environmental water used as a source for recreational water is a global issue [3]. Total coliforms, faecal coliforms, Escherichia coli and enterococci are commonly used microbial indicators of water quality [4]. However, several studies of both recreational and drinking water samples suggested that enterococci are more relevant indicators of faecal contamination than faecal coliforms and E. coli [5,6]. Previous epidemiological studies demonstrated a correlation between the concentration of enterococci in surface waters and an increase in swimmer-associated gastroenteritis [5-8]. The United States Environmental Protection Agency (USEPA) advises various limits as guidelines for recreational water quality. For freshwater, the present single-sample advisory limit is 61 cfu/100 ml for enterococci. The 5-day geometric mean should not exceed 33 cfu/100 ml for enterococci [9]. According to the Australian National Health and Medical Research Council (NHMRC) guidelines, there are four microbial assessment categories, A-D, based on enterococcal counts per ml (A ≤ 40, B 41-200, C201-500 and D > 501) together with associated health risks [10].
Enterococci are members of the natural intestinal flora of animals and humans and are released into the environment directly or via sewage outlets [11]. Certain members of the genus, particularly E. faecalis and E. faecium, are becoming increasingly important as opportunistic pathogens [7,12,13]. Most important and a contributing factor to the pathogenesis of enterococci is their resistance to a wide range of antibiotics [14]. Enterococci have been found to be increasingly resistant to multiple anti-microbial drugs in last few years [15-17]. Enterococci show either intrinsic resistance where resistance genes are located on the chromosome, or they possess acquired resistance determinants which are located on plasmids or transposons [18]. Examples of the intrinsic antibiotic resistance include resistance to beta-lactams, cephalosporins, sulfonamides, and low levels of clindamycin and aminoglycosides [18,19]. Resistance to chloramphenicol, erythromycin, high levels of clindamycin and aminoglycosides, tetracycline, high levels of beta-lactams, fluoroquinolones, and glycopeptides such as vancomycin are examples of acquired resistance [19].
The distribution of infectious enterococcal strains into the environment via water could increase the prevalence of these strains in the human population. Environmental water quality studies may benefit from focusing on a subset of Enterococcus spp. that are consistently associated with sources of faecal pollution such as domestic sewage, rather than testing for the entire genus. E. faecalis and E. faecium are potentially good focal species for such studies, as they have been consistently identified as the dominant Enterococcus spp. in human faeces [20-22] and sewage [23]. The characterisation of E. faecalis and E. faecium is important in studying their population structures, particularly in environmental samples. Different methods have been developed for the characterisation of enterococci [24-28]. However, there is a need to develop and apply new robust, rapid and cost effective techniques which are likely to yield more definitive results for the routine monitoring of E. faecalis and E. faecium. This was addressed in our previous study where we developed a single-nucleotide polymorphisms (SNP) based genotyping method to study the population structure of E. faecalis and E. faecium [29]. A set of eight high-D SNPs was derived from the E. faecalis and E. faecium Multilocus Sequence Typing (MLST) database, using the 'Minimum SNPs' software program, which provided a high Simpson's index of diversity (D), calculated with respect to the MLST database. An allele-specific real-time PCR (AS Kinetic PCR) method was developed to interrogate these high-D SNPs [29]. SNP interrogation is an efficient means of classifying E. faecalis and E. faecium into groups that are concordant with the population structure of these organisms [29]. In this study we have applied this rapid SNP genotyping method to determine the diversity of enterococci in the Coomera River, South East Queensland, Australia over a period of two years and also investigated the antibiotic resistance determinants associated with E. faecalis and E. faecium SNP genotypes.
Methods
Study site
The Pimpama-Coomera watershed is located in South East Queensland, Australia and is used intensively for agriculture and recreational purposes and has a strong anthropogenic impact. The main water source is the Coomera River, which flows for 90 km from its headwaters in the Lamington National Park. The upper reaches of the river passes through mainly rural areas comprising crops and cattle grazing. In the middle to lower reaches, land uses include farming and cropping. In the 1970s and 1980s the river was widened 20 km upstream from the mouth as a consequence of sand and gravel extraction operations. The lower reaches of the Coomera River passes through highly developed areas including canal estates such as Santa Barbara, Hope Island, Sanctuary Cove and the Coomera Mooring Marina. Most of the sewage system collection is gravity fed and follows natural catchment drainage lines until the wastewater is treated at the central treatment plant. After treatment, the water is released into the Gold Coast Seaway located south of the Coomera River estuary. Despite the existence of such an effective treatment system, high numbers of coliforms were observed over a long period of time in the estuary.
Sampling
Environmental water samples were collected during four seasonal trips at the same time each day from six designated sites of the Coomera River, from May 2008 to July 2009. Hot-spots selected for sampling included: Coomera Marina (C1), Santa Barbara (C2), Sanctuary Cove (C3), Jabiru Island (C4), Paradise Point (C5) and Coombabah (C6). These sites were suggested by the Gold Coast City Council as being problematic sites with a history of high numbers of faecal coliforms. The positions of these sampling sites are shown in Figure 1. The exact location and characteristics of sampling sites are summarised in Table 1.
Figure 1.
Water sampling sites along the Coomera River, South-East Queensland, Australia. C1 - Coomera marina, cattle/kangaroo feeding, house-boat mooring site; C2 - Santa Barbara, well used park, BBQ, toilets and fishing, private houses about 100 m away; C3 - Sanctuary Cove, canal estate, modern houses and apartments, modern infrastructure, commercial/light industrial area; C4 - Jabiru Island, busy through road, disused sand mine, no houses, small park with toilets; C5 - Paradise Point, public swimming area, mouth of river, much water traffic; C6 - Coombabah; established suburban area, bush island opposite.
Table 1.
Sampling site locations and characteristics
| Code | Site name (GISb map reference) |
Site characteristics |
|---|---|---|
| C1 | Coomera marina (-27.861672, 153.339089) |
Cattle/kangaroo feeding, house-boat mooring site |
| C2 | Santa Barbara (-27.855165, 153.350612) |
Well used park, BBQ, toilets and fishing, private houses about 100 m away |
| C3 | Sanctuary Cove (-27.851617, 153.362140) |
Canal estate, modern houses and apartments, modern infrastructure, commercial/light industrial area |
| C4 | Jabiru Island (-27.879057, 153.380685) |
Busy through road, disused sand mine, no houses, small park with toilets |
| C5 | Paradise Point (-27.886359, 153.396596) |
Public swimming area, mouth of river, much water traffic |
| C6 | Coombabah, Estuary (-27.896607, 153.366845) |
Established suburban area, bush island opposite |
b Global information system
Water samples were collected in sterile bottles according to the sampling procedures described in the USEPA microbiology methods manual [9]. The sampling depth for surface water samples were 6-12 inches below the water surface. Samples were transported in a cooler on ice packs to the laboratory where they were prepared for analyses immediately upon arrival and were tested within 6 h of collection for the presence of enterococci.
Isolation and identification of enterococci
The environmental water samples were mixed thoroughly, and undiluted samples or a 1:10 dilution of water samples were filtered through 0.45 μm membrane filters (MilliporeCorporation, Bedford, MA, USA), placed onto membrane-Enterococcus Indoxyl β-D-Glucoside Agar (mEI) (Becton-Dickinson, Sparks, MD, USA) according to the USEPA specifications [30]. Triplicate samples were collected from each site and each sample was treated separately. The addition of Indoxyl-β-D-Glucoside, Nalidixic acid, 0.1 N NaOH, and Triphenyltetrazolium Chloride to mEI agar (Difco) allowed for a single 24 h incubation period at 41°C [31]. E. faecium ATCC 27270, E. faecalis ATCC 19433 and E. coli ATCC 25922 were used as positive and negative controls respectively to validate the mEI agar. Colonies producing a blue halo were typically observed for enterococci and counted, the result expressed as cfu/ml for each water sample.
Statistical analysis
The Mann-Whitney U-test at 5% significance level was performed to determine whether there was a significant increase of total enterococcal counts (cfu/ml) at each location after rainfall events.
Identification of E. faecium and E. faecalis
Typical colonies on the membranes were identified to the genus and species level by Gram-stain, catalase test, the ability to tolerate 6.5% NaCl and biochemical tests [32]. The isolates identified as E. faecium and E. faecalis were used in this study and species identification was confirmed by performing real-time PCR to detect the ddlE. faecalis and ddlE. feacium genes. The primers used were: 5'CAAACTGTTGGCATTCCACAA3' and 5'TGGATTTCCTTTCCAGTCACTTC3' (E. faecalis forward and reverse primers respectively); and 5'GAAGAGCTGCTGCAAAATGCTTTAGC3' and 5'GCGCGCTTCAATTCCTTGT3' (E. faecium forward and reverse primers respectively) [29].
Antibiotic susceptibility testing
Antibiotic resistance phenotypes were determined by the disc diffusion method according to the Clinical and Laboratory Standards Institute (CLSI) recommendations [33]. Saline suspensions of isolated colonies selected from an 18-24 hour Brain Heart Infusion agar (Oxoid, Australia) plates were prepared and suspension turbidity was adjusted to an equivalent of a 0.5 Mc Farland standard and inoculated onto Mueller Hinton agar (Oxoid, Australia) using sterile cotton swabs. Antibiotic discs for ampicillin (AMP, 10 μg), ciprofloxacin (CIP, 5 μg), gentamicin (GEN, 10 μg), tetracycline (TET, 30 μg), and vancomycin (VAN, 30 μg), were placed onto the surface of each inoculated plate. The diameters of antibiotic inhibition zones were measured and recorded as susceptible (S), intermediate resistant (IR) or resistant (R) according to CLSI M02-A10. E. faecalis ATCC 29212 and Staphylococcus aureus ATCC 25923 were used for quality control.
DNA Extraction
Enterococcal strains were sub-cultured into Brain Heart Infusion broth (Oxoid, Australia) and incubated at 37°C overnight. A 400 μl aliquot of an overnight culture was used for DNA extraction. The Corbett X-tractor Gene automated DNA extraction system was used to extract DNA from all cultured isolates (Corbett Robotics, Australia) using the Core protocol No.141404 version 02. The automated DNA extraction system allows for the simultaneous extraction of DNA from 96 isolates. The quality and quantity of the DNA was high, yielding 98 ug/ml DNA on average and with a mean 260:280 absorbance ratio of 1.85.
SNP profiling of E. faecium and E. faecalis by Allele-specific Real-Time PCR
A method for a highly-discriminatory SNP genotyping method for E. faecium and E. faecalis, has been developed by our group [29]. In total, 55 E. faecalis and 53 E. faecium isolates were genotyped by the SNP method using Allele-specific real-time PCR (RotorGene 6000, Corbett Robotics). Each reaction contained 2 μl of DNA which was added to 8 μl of reaction master mix containing 5 μl of 2 × SYBRGreen® PCR Mastermix (Invitrogen, Australia) and 0.125 μl of reverse and forward primers (20 μM stock, final concentration 0.5 μM) [29]. Cycling conditions were as follows: 50°C for 2 min, 95°C for 10 minutes, followed by 40 cycles of 95°C for 15 seconds, 60°C for 60 seconds, and a melting stage of 60°C-90°C. Each isolate was tested in duplicate and No Template Controls (NTCs) were used for each primer set as well. An isolate specific SNP profile for all E. faecium and E. faecalis was generated consisting of the polymorphism present at each of the SNPs. A complete description of the relationship between the SNP profiles of each isolate and MLST-defined population structure was determined for both E. faecalis and E. faecium, using the MLST database and the "working backwards" mode of the Minimum SNPs program.
SNP validation by sequencing of MLST housekeeping genes
E. faecalis and E. faecium isolates representing each possible SNP were used to validate the polymorphism present at each position. Sequencing was performed to confirm the SNP profiles using MLST sequencing primers listed at http://efaecalis.mlst.net/misc/info.asp and http://efaecium.mlst.net/misc/info.asp. PCR products were prepared for sequencing using the high pure PCR product purification kit (Roche, Indianapolis, USA) according to manufacturer's instructions. Between 18 -30 ng DNA template was mixed with the relevant sequencing primer at a final concentration of 9.6 pmol in a 12 μl reaction containing the Big Dye terminator mix (Australian Genome Research Facility - AGRF). Sequencing reactions were performed using a protocol of 96°C for 1 min, 96°C for 10 s, 50°C for 5 s and 60°C for 4 min on the AB3730XL platform. Sequencing data were analyzed using Chromas (version 1.43, Technelysium, Tewantin, Australia) and Vector NTI (version 11, Invitrogen, Australia) software programs.
Real-Time PCR for the detection of antibiotic resistance
Primer design
Real-Time PCR primers for genes encoding vancomycin (vanA, vanB), tetracycline (tet(L), tet(M), tet(S)), ciprofloxacin (gyrA), ampicillin (pbp 5) and gentamicin (aac(6')-aph(2')) resistance were designed using the Primer Express 2.0 primer design software program (Applied BioSystems) (Table 2). Primers were synthesised by Sigma-Aldrich, Castle Hill, New South Wales, Australia.
Table 2.
Oligonucleotide primers for Real-Time PCR detection of genes encoding for resistance to vancomycin (vanA, vanB, vanC1, vanC2), tetracycline (tet(L), tet(M), tet(S)), ciprofloxacin (gyrA), ampicillin (pbp5) and gentamicin (aac(6')-aph(2'))
| Target gene | Primer name | Primer sequence (5' to3') | Positive control |
|---|---|---|---|
| van A | vanAFa | TGTGCGGTATTGGGAAACAG | ATCC 51559 |
| vanARb | GATTCCGTACTGCAGCCTGATT | ||
| van B | vanBF | TCTGCTTGTCATGAAAGAAAGAGAA | ATCC 700802 |
| vanBR | GCATTTGCCATGCAAAACC | ||
| tet(L) | tetLF | GGGTAAAGCATTTGGTCTTATTGG | RBH200523 |
| tetLR | ATCGCTGGACCGACTCCTT | ||
| tet(M) | tetMF | GCAGAATATACCATTCACATCGAAGT | RBH200535 |
| tetMR | AAACCAATGGAAGCCCAGAA | ||
| tet(S) | tetSF | CCATTGATATCGAAGTACCTCCAA | RBH200535 |
| tetSR | AGGAAGTGGTGTTACAGATAAACCAA | ||
| gyr A | gyrAF | CGGATGAACGAATTGGGTGTGA | ATCC 51559 |
| gyrAR | AATTTTACTCATACGTGCTT | ||
| pbp 5 | pbp5F | GTTCTGATCGAACATGAAGTTCAAA | ATCC 51559 |
| pbp5R | TGTGCCTTCGGATCGATTG | ||
| aac(6')-aph(2') | acc-aphF | TCCTTACTTAATGACCGATGTACTCT | ATCC 700802 |
| acc-aphR | TCTTCGCTTTCGCCACTTTGA |
Fa forward primer, Rb reverse primer
Real-Time PCR
Each reaction contained 2 μl of DNA which was added to 18 μl of reaction master mix containing 10 μl of 2 × SYBRGreen® PCR Mastermix (Invitrogen, Australia) and 0.25 μl of reverse and forward primers (20 μM stock, final concentration 0.5 μM). Cycling conditions were as follows: 50°C for 2 min, 95°C for 10 minutes, followed by 40 cycles of 95°C for 15 seconds, 60°C for 60 seconds, and a melting stage of 60°C-90°C. Each isolate was tested in duplicate. No Template Controls (NTCs) and previously characterized positive controls were used for each primer set as well.
Mutation detection in the gyrA and pbp5 genes
All ciprofloxacin- and ampicillin-resistant and intermediate-resistant isolates were screened for gene mutations. The gyrA and pbp5 genes were amplified and sequenced. Primers used were: 5'CGGGATGAACGAATTGGGTGTGA3'and 5' AATTTTACTCATACGTGCTTCGG 3' (gyrA forward and reverse respectively); and 5' CGGGATCTCACAAGAAGAT 3'and 5' TTATTGATAATTTTGGTT 3' (pbp5 forward and reverse respectively) [34-36]. Sequencing reactions were prepared as for the SNP validation step described above. Sequence data was analysed using Chromas (version 1.43, Technelysium, Tewantin, Australia) and Vector NTI (version 11, Invitrogen, Australia) software programs.
Results and Discussion
The poor microbiological quality of recreational waters is a global issue [37,38]. There is a great need to rapidly and accurately determine human faecal contamination of recreational waters. We applied a SNP genotyping method to water samples collected from the Coomera River, South East Queensland, Australia, to determine the distribution and diversity of E. faecalis and E. faecium strains and establish the antibiotic profiles associated with different SNP profiles.
Total enterococccal counts in the Coomera River, over a two year period
Enumeration of enterococcal strains was performed at each of the six sampling sites along the Coomera River, and these counts were compared to the single-sample advisory limit specified by the US Environmental Protection Agency (USEPA) and the Australian NHMRC Guidelines for water quality assessment. Previous studies have found that the concentration of faecal indicator bacteria in surface waters is influenced by storm water runoff and can increase dramatically during rainfall events in comparison to baseline conditions [39-42]. Similarly, we found an increase in the number of enterococci at three of the sampling sites after rainfall events (August 2008 and March 2009). There was a substantial increase in enterococcal colony counts at Jabiru Island (C4), Paradise Point (C5) and Coombabah (C6) after rainfall events. These findings were confirmed by the Mann-Whitney test which showed that enterococcal counts after rainfall events differ significantly between the different locations; C4-C5 (p = 0.004) compared to C1-C3 (p = 0.029), (additional file 1). These counts were well above the USEPA recommended level (61 cfu/100 ml). According to the Australian NHMRC Guidelines these locations are categorised into the microbial water quality assessment category B (41-200 cfu/100 ml), except for Jabiru Island (March 2009), which was category C (201-500 cfu/100 ml). Category B indicates a 1-5% gastrointestinal illness risk and category C indicates a 5-10% gastrointestinal illness risk. In contrast, even though counts for the other sampling points, Marina (C1), Sanctuary Cove (C2) and Santa Barbara (C3) increased after rainfall, they were within the acceptable range for enterococci in fresh recreational water. Table 3 lists the total enterococcal counts (cfu/ml) for each of the sampling sites across the different sampling times.
Table 3.
Total enterococcal counts at different sampling points at different sampling times
| Site marked on the map | Site name | Average concentration of enterococci cfua/100 mL, ± STDb | |||
|---|---|---|---|---|---|
| May-08 | Aug-08C | Mar-09C | Jul-09 | ||
| C1 | Coomera marina | 0 (0) |
3 ± 1.41 (3)d |
21.5 ± 2.12 (20) |
4.5 ± 0.71 (5) |
| C2 | Santa Barbara | 0 (0) |
2.5 ± 0.70 (3) |
3.5 ± 0.71 (4) |
0 (0) |
| C3 | Sanctuary Cove | 1.5 ± 0.7 (1) |
32.5 ± 2.1 (20) |
8.5 ± 2.12 (9) |
3 ± 0 (3) |
| C4 | Jabiru Island | 5.5 ± 0.7 (6) |
78 ± 4.2 (25) |
230 ± 28.28 (30) |
2.5 ± 0.70 (3) |
| C5 | Paradise Point | 9 ± 1.4 (10) |
185 ± 7.0 (25) |
160 ± 14.14 (25) |
22 ± 1.41 (20) |
| C6 | Coombabah | 7.5 ± 0.71 (8) |
165 ± 7.0 (25) |
125 ± 7.07 (25) |
4 ± 0 (4) |
a colony forming units
b standard deviation
c samples collected after rainfall event
d number of isolates analysed
These high counts can be explained by the transportation of faecal indicator bacteria by storm water run-off [39-41] and soil leaching [37] immediately after a rainfall event. Storm water run-off occurs when rainfall is unable to infiltrate the soil surface (after soil saturation) and runs over land to transport soil particles, faecal and associated bacteria [39,42]. Increased urbanization and land usage changes in the South-East region of Queensland, has had an adverse impact on the quality of natural water resources [43]. One potential source of bacterial contamination may be the accidental sewage discharge from a large number of yachts and houseboats owned by residents with boat-moorings in these waterways. Furthermore, it is speculated that higher enterococcal counts at Jabiru Island (C4), Paradise Point (C5) and Coombabah (C6), compared, to Marina (C1), Sanctuary Cove (C2) and Santa Barbara (C3) may be due to their physical locations along the Coomera River and the impact of their surroundings. At Jabiru Island (C4), there is sand mine and the water is turbid particularly during rainfall periods. Previous studies have demonstrated that indicator organisms attach to sand particles [44]. Soil resuspension can be enhanced by rainfall, and as a result, higher enterococcal counts are possible. Paradise Point (C5) is a highly populated area and is used for bathing primarily. At Coombabah (C6), there is a waste-water treatment plant near the sampling site, and during rainfall periods, it is possible that there is a mixing of the treatment plant effluent with surrounding water bodies which contributes to high enterococcal counts. In addition, sampling sites C4-C6 are located at the lower reaches of the Coomera River, where enterococci can accumulate from the upstream regions of the river.
The diversity and the distribution of E. faecalis and E. faecium SNP profiles in the Coomera River
It is more important to focus on E. faecalis and E. faecium rather than the total enterococcal count as they pose a definite human health risk and are the predominant enterococcal species in human faeces and sewage. In total, 55 E. faecalis and 47 E. faecium strains were isolated from six different sampling sites along the Coomera River. In this study, we applied a recently developed SNP genotyping method to the Coomera River to determine the diversity of E. faecalis and E. faecium genotypes. This method represents an efficient means of classifying E. faecalis and E. faecium into groups that are concordant with their population structure [29]. For the purpose of clarity, we define the SNP profiles into two main groups. The first group is the human-specific SNP profile group; these profiles are associated with enterococcal strains that originate from human samples only, as defined by the MLST database, as well as our previous study [27]. The second group is the human-related SNP profile group; these profiles are associated with enterococcal strains that originate from mixed sources (human and animal) according to the MLST database, but we found these profiles for enterococcal isolates from human specimens as well [27].
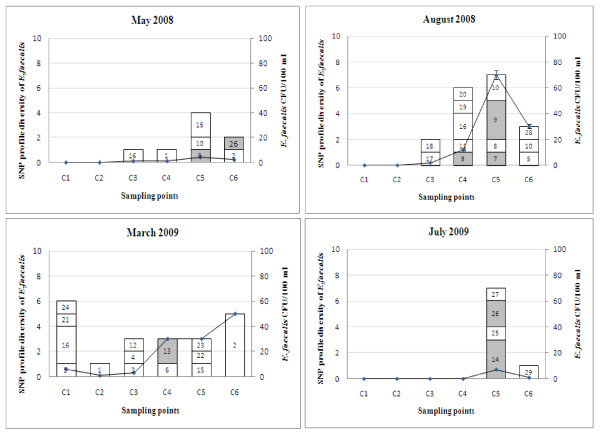
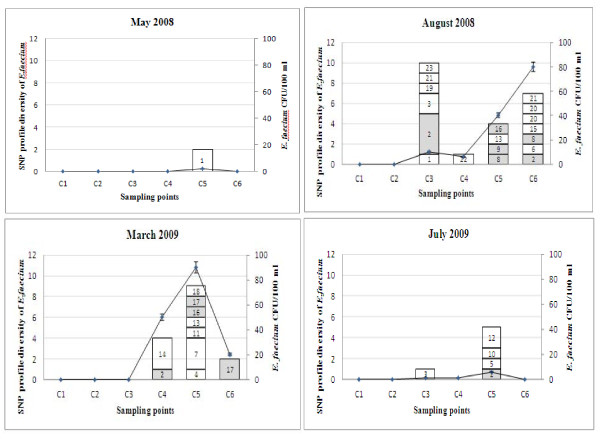
The SNP profiles of the Coomera enterococcal strains were compared to known human-related and human-specific SNP profiles described previously [29]. SNP profiles were validated by gene sequencing using MLST primers for E. faecalis and E. faecium. Enterococcal strains with new SNP profiles (3 and 10 profiles for E. faecalis and E. faecium respectively) were also sequenced, and added to the MLST database (Tables 4 and 5). The Coomera isolates were grouped into 29 and 23 SNP profiles for E. faecalis and E. faecium respectively (Tables 4 and 5). These results confirm that the enterococcal population in the Coomera River is diverse. Figures 2 and 3 illustrate the distribution of these SNP profiles at all sampling points over the two year study period. In addition, we found that both E. faecalis and E. faecium populations were more diverse during rainfall periods (August 2008 and March 2009).
Table 4.
SNP and antibiotic resistance gene profiles of E. faecalis isolates and their corresponding Sequence Types (STs)
| SNP profile | SNP ID | No of isolates | Antibiotic resistance [Identified genetic determinants] | Corresponding sequence Types (STs) for SNP profiles in MLST |
|---|---|---|---|---|
| ACCAAACC | 1 | 2 | Cip IR [gyrA]; Tet R [ tetM] | ST4, ST22, ST32, ST129, ST202 |
| ACCAAACT | 2 | 5 | Tet R [tetM] | ST274 |
| ACCAAACT | 2 | 1 | Gen IR [aac(6')-aph(2')] Tet R [ tetM] | |
| ACCGAGCT | 3 | 1 | No antibiotic resistance detected | ST277 |
| ACCGAGTT | 4 | 1 | No antibiotic resistance detected | ST123 |
| ACCGTGCC | 5 | 2 | Gen IR [aac(6')-aph(2')] | ST76 |
| ACTAAGCT | 6 | 1 | Gen R [aac(6')-aph(2')] | ST278 |
| ACTATGCCa | 7 | 1 | Gen R [aac(6')-aph(2')] | ST79, ST82 |
| ACTGTGTC | 8 | 1 | No antibiotic resistance detected | ST414N |
| ATCAAACC | 9 | 3 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST5, ST21, ST46, ST50, ST70, ST145, ST152, ST157 |
| ATCAAACC | 9 | 1 | Gen IR [aac(6')-aph(2')] | |
| ATCAAACC | 9 | 1 | Gen R [aac(6')-aph(2')] | |
| ATCGTGCC | 10 | 4 | Gen IR [aac(6')-aph(2')] | ST143 |
| ATCGTGTT | 11 | 1 | Gen R [aac(6')-aph(2')] | ST230 |
| ATTAAACC | 12 | 1 | Cip IR [gyrA] | ST255 |
| ATTAAGCT | 13 | 2 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST139, ST181, ST183, ST241 |
| ATTATGCC | 14 | 3 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST170 |
| GCCAAACT | 15 | 1 | No antibiotic resistance detected | ST410 |
| GCCATGCT | 16 | 1 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST81, ST164 |
| GCCATGCT | 16 | 7 | Gen R [aac(6')-aph(2')] | |
| GCCGTACC | 17 | 1 | No antibiotic resistance detected | ST110 |
| GCCGTGCC | 18 | 1 | No antibiotic resistance detected | ST27, ST124 |
| GCCGTGCT | 19 | 1 | Gen R [aac(6')-aph(2')] | ST418N |
| GCCGTGTC | 20 | 1 | No antibiotic resistance detected | ST86 |
| GCTATACC | 21 | 1 | Gen R [aac(6')-aph(2')] | ST39, ST45, ST69, ST96, ST116 |
| GCTGTACC | 22 | 1 | No antibiotic resistance detected | ST260, ST396 |
| GCTGTGTT | 23 | 1 | No antibiotic resistance detected | ST201 |
| ATTAAGCC | 24 | 1 | Gen IR [aac(6')-aph(2')] | ST419N |
| GTCGTATT | 25 | 1 | Gen R [aac(6')-aph(2')] | ST125, ST165, ST167 |
| GTCGTGTT | 26 | 2 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST36, ST118, ST180 |
| GTCGTGTT | 26 | 1 | Cip IR [gyrA] | |
| GTTATGCC | 27 | 1 | Gen R [aac(6')-aph(2')] | ST108, ST122 |
| GTTGAGTC | 28 | 1 | Gen R [aac(6')-aph(2')]; Cip IR [gyrA] | ST64, ST101, ST161, ST205 |
| GTTATGCT | 29 | 1 | No antibiotic resistance detected | ST175 |
aSNP profiles which were present in hospital isolates are bold and underlined
SNP profiles in bold text are isolates with the same SNP profiles but with different antibiotic resistant gene profiles.
Amp; ampicillin, Cip; ciprofloxacin, Gen; gentamicin, Tet; tetracycline,
R Resistant, IR Intermediate resistant
N New sequence types identified in the present study
Table 5.
SNP and antibiotic resistance gene profiles of E. faecium isolates and their corresponding Sequence types (STs)
| SNP Profile | SNP ID | No. of Isolates | Antibiotic resistance [Identified genetic determinants] | Corresponding sequence Types (STs) for SNP profiles in MLST |
|---|---|---|---|---|
| AAACTTTC | 1 | 3 | No antibiotic resistance detected | ST 544, ST 583 |
| AACCCTTCa | 2 | 1 | Amp R [pbp5]m; Tet R [tetM] | ST 602 N |
| AACCCTTCa | 2 | 3 | Cip IR [gyrA] | |
| AACCCTTCa | 2 | 2 | No antibiotic resistance detected | |
| AATCCTTC | 3 | 1 | Gen IR [aac(6')-aph(2')]; Cip IR [gyrA] | ST8, ST9, ST58, ST134, ST194, ST198, ST237, ST244, ST248, |
| AATCCTTC | 3 | 2 | No antibiotic resistance detected | ST259, ST266, ST298, ST309, ST370, ST402, ST425, |
| AATCTTTC | 4 | 1 | No antibiotic resistance detected | ST40, ST100, ST163, ST211, ST221, ST223, ST226, |
| AGCCCCTC | 5 | 1 | Gen IR [aac(6')-aph(2')] | ST 607 N |
| AGCCCTCT | 6 | 1 | No antibiotic resistance detected | ST508 |
| AGCCCTTT | 7 | 2 | Cip IR [gyrA] | ST 603 N |
| AGCCCTTT | 7 | 1 | No antibiotic resistance detected | |
| AGCCTTTC | 8 | 2 | No antibiotic resistance detected | ST 604 N |
| AGCTCTCC | 9 | 2 | Gen IR [aac(6')-aph(2')];Cip R [gyrA]m;Amp R [pbp5]m | ST260, ST262, ST273, ST322 |
| AGTCCTTC | 10 | 2 | Gen IR [aac(6')-aph(2')]; Cip R [gyrA]m | ST13, ST14, ST48, ST79, ST82, ST120, ST157, ST195, ST200, ST241 |
| Tet R [tetL & S] | ST242, ST310, ST311, | |||
| AGTCCTTT | 11 | 1 | Gen IR [aac(6')-aph(2')]; Cip IR [gyrA] | ST15, ST70 |
| AGTCTTTT | 12 | 2 | Cip IR [gyrA] | ST 605 N |
| GACCCTCC | 13 | 1 | Gen IR [aac(6')-aph(2')] | ST 608 N |
| GACCCTCC | 13 | 1 | Cip IR [gyrA] | |
| GACCCTTT | 14 | 1 | Cip IR [gyrA]; Tet R [tetL & M] | ST 609 N |
| GACCCTTT | 14 | 2 | Tet R [tetL,M & S] | |
| GATCCTTC | 15 | 1 | Gen IR [aac(6')-aph(2')] | ST 610 N |
| GGCCCCCC | 16 | 2 | Cip IR [gyrA] | ST501, ST511, ST516, ST518, ST521, ST522, ST529, ST530, ST565, ST588, ST592, ST599 |
| GGCCCTCC | 17 | 3 | Amp R [pbp5]m; Tet IR [tetL & tetM] | ST162 |
| GGCCCTTC | 18 | 2 | Cip IR [gyrA] | ST 611 N |
| GGCCTCCC | 19 | 1 | No antibiotic resistance detected | ST 606 N |
| GGTCCCCC | 20 | 2 | Cip IR [gyrA] | ST22, ST23, ST24, ST27, ST28, ST33, ST36, ST55, ST59, ST106, |
| ST111, ST119, ST122, ST131, ST136, ST159, ST214, ST263, ST269, | ||||
| ST270, ST315, ST372, ST379, ST422, ST435 | ||||
| GGTCCTCC | 21 | 1 | Cip R [gyrA]m | ST1, ST2, ST3, ST4, ST32, ST34, ST35, ST41, ST43, ST72, |
| ST87, ST90, ST104, ST109, ST128, ST139, ST146, ST215, ST250, ST253 | ||||
| ST257, ST291, ST292, ST330, ST426, ST427, | ||||
| GGTCCTTT | 22 | 1 | Cip IR [gyrA] | ST6, ST88, ST149, ST170, ST247, ST255, ST354 |
| GGTCCTTC | 23 | 2 | No antibiotic resistance detected | ST7, ST21, ST25, ST26, ST29, ST37, ST57, ST66, ST68, ST83, |
| ST89,ST97,ST99,ST112,ST113,ST115,ST124, ST129, ST143, ST158, | ||||
| ST160, ST176, ST183, ST210, ST236, ST243, ST245, ST246, ST251, | ||||
| ST265, ST271, ST272, ST277, ST281, ST284, ST297, ST358, ST381, | ||||
| ST384, ST395, ST401, ST418, ST433, ST437, | ||||
aSNP profiles which were present in hospital isolates are bold and underlined
SNP profiles in bold text are isolates with the same SNP profiles but with different antibiotic resistant gene profiles.
Amp; ampicillin, Cip; ciprofloxacin, Gen; gentamicin, Tet; tetracycline,
R Resistant, IR Intermediate resistant, m mutation
N New sequence types identified in the present study
Figure 2.
Distribution of the E. faecalis SNP genotypes at six sampling points over a two year period. Shaded areas indicate common SNP profiles for both human and water isolates. E. faecalis cfu/ml is indicated by the line graph. Total number of E. faecalis analysed during each sampling; May 2008 - 8 isolates, August 2008 - 18 isolates, March 2009 - 21 isolates and July 2009 - 8 isolates.
Figure 3.
Distribution of the E. faecium SNP genotypes at six sampling points over a two year period. Shaded areas indicate common SNP profiles for both human and water isolates. E. faecium cfu/ml is indicated by the line graph. Total number of E. faecium analysed during each sampling; May 2008 - 2 isolates, August 2008 - 23 isolates, March 2009 - 16 isolates and July 2009 - 6 isolates.
Of all the SNP profiles described in this study, six SNP profiles ACTATGCC, ATCAAACC, ATTAAGCT, ATTATGCC, GTCGTGTT and GTTGAGTC (ID no: 7, 9, 13, 14, 26 & 28) of E. faecalis and five E. faecium SNP profiles AACCCTTC, AGCCTTTC, AGCTCTCC, GGCCCCCC and GGCCCTCC (ID no: 2, 8, 9, 16 & 17) have previously been described and distributed amongst human strains in Brisbane, Australia [29]. SNP profiles 7, 9, 13, 14 & 26 of E. faecalis and 16 of E. faecium have previously been found to correspond to not only human E. faecalis and E. faecium strains listed in the MLST database, but these SNP profiles also include strains originating from other sources such as animals. These SNP profiles are therefore classified as human-related SNP profiles [29]. E. faecalis SNP profile 28 and E. faecium SNP profiles 2, 8, 9 and 17 are found only in humans and classified as human-specific. eBURST analysis of both the E. faecalis and E. faecium MLST database, which now include the new STs found in this study, are included as additional file 2. The new E. faecium STs, ST602 (SNP profile 2) and ST604 (SNP profile 8), found in this study are human-specific and not related to the major clonal complex-17 (CC17), as shown in the eBURST diagram (Additional file 2). A very important finding of this study was the isolation of E. faecium strains (4.25%) with SNP profile AGCTCTCC (ID no. 9) from water, as we have previously demonstrated that this is a human-specific SNP profile which represents a major clonal complex-17 (CC17) of E. faecium strains that cause the majority of hospital outbreaks and clinical infections across five continents [45,46]. Of major concern is the fact that the majority of the members of this cluster are vancomycin-resistant and CC17 strains are generally resistant to ampicillin and carry genes for putative virulence factors, such as esp [47]. The dissemination of these types of strains in natural waterways is of concern and further investigations are warranted to establish the genetic similarity between water E. faecium strains and those originating from clinical sources.
Overall, these human-related and human-specific enterococcal SNP profiles were found at Jabiru Island (SNP ID 9 &13 of E. faecalis and SNP ID 2 of E. faecium) and Coombabah (SNP ID 28 of E. faecalis and SNP ID 2, 8 and 17 of E. faecium) after rainfall events, where the total enterococcal count was above the USEPA acceptable level. A likely reason for this occurrence is the terrestrial run-off during high rainfall. In contrast, at Paradise Point, the human-related E. faecalis and E. faecium SNP profiles were detected irrespective of rainfall. SNP profiles 7, 9, 14 & 26 of E. faecalis, and SNP profiles 2, 8, 9, 16 and 17 of E. faecium were found at Paradise Point. Furthermore, SNP profiles 9, 14 and 26 of E. faecalis and SNP profile 2 of E. faecium were found in the absence of rain. In comparison to other sites, Paradise Point had the highest number of human-related and human-specific SNP profiles. Paradise Point is primarily used for public bathing, and therefore the presence of these human-related and human-specific enterococcal SNP profiles indicates human faecal contamination of this area.
Antibiotic resistance profiles related to SNP profiles
Tables 4 and 5 summarize the antibiotic resistance profiles for the E. faecalis and E. faecium strains tested in this study. Disc susceptibility results are included in additional files 3 and 4. The outcome of the antimicrobial disc susceptibility tests followed by PCR, revealed that 81.8% of E. faecalis SNP profiles and 70.21% of E. faecium SNP profiles were associated with antibiotic resistance. The highest percentage of antibiotic resistant E. faecalis was found at Paradise Point (C5) 37.7% followed by Coombabah (C6) 22.2%, Jabiru Island (C4) 19.1%, Marina (C1) 15.5%, Santa Barbara (C3) 4.4% and Sanctuary Cove (C2) 2.2%. No antibiotic resistant E. faecium strains were found at Marina (C1) and Sanctuary Cove (C2). The highest percentage of antibiotic resistant E. faecium was found at Paradise Point (C5) 51.5% followed by Coombabah (C6) 21.2%, Jabiru Island (C4) 15.1% and Santa Barbara (C3) 12.1%. Phenotypic and genotypic antibiotic resistance profiles of E. faecalis and E. faecium at individual sampling sites are listed in additional files 5 and 6.
Gentamicin resistance was more prevalent in E. faecalis (47% resistant and 16% intermediate resistant) and these strains contained the aac(6')-aph(2') gene. Whereas ciprofloxacin resistance is more common in E. faecium (12.7% resistant and 36.2% intermediate-resistant). According to previous studies, one of the factors used to determine ciprofloxacin resistance is the association with mutations in the DNA gyrase genes [34]. The sequencing results revealed that there were no mutations detected in gyrA gene of intermediate resistant strains, however, amino acid changes were detected in five E. faecium isolates that were disc-resistant to ciprofloxacin. Amino acid changes at position 83 (serine to arginine) were found in two isolates belonging to SNP ID 9, whereas the remaining three isolates, belonging to SNP ID 10 and 21 had an amino acid change at position 87 (glutamate to lysine). According to previous studies, glutamate at position 87 can also be replaced by glycine in ciprofloxacin-resistant isolates, but this was not detected in our environmental isolates [34]. Tetracycline resistance was less common among E. faecalis (14%) and E. faecium (12.7%) strains. Of these, the tet(L) and tet(M) genes were the predominant genetic determinants. This finding is consistent with previous studies [48]. Ampicillin resistance was found in only six E. faecium strains. Ampicillin resistance was observed in both multi-drug resistant strains and in human-related strains. Previous studies have shown an amino acid substitution in ampicillin-resistant enterococci. Potentially significant mutations that confer ampicillin resistance are methionine to alanine substitution at position 485, an additional serine at position 466, and replacement of a polar amino acid with a non-polar one (alanine or isoleucine) at position 558, 562, or 574. A glutamate to valine substitution at position 629 has also been associated with ampicillin resistance [49]. In the present study, an ampicillin-resistant E. faecium isolate with SNP ID 2 had alanine at position 485 and all the other ampicillin- resistant E. faecium strains had valine at position 629 (SNP ID 9 and 17). Vancomycin resistance was not detected in any of the environmental isolates tested. Multi-antibiotic resistance was found in both E. faecalis (27%) and E. faecium (22%). Of these isolates, all E. faecalis harboured only two resistance genes. Eight E. faecium isolates with SNP IDs 9, 10 and 17 harbored more than three antibiotic resistance genes. However, it is interesting to note that SNP ID no. 9, which represents CC17, had multi-antibiotic resistance and contained the aac(6')-aph(2') gene and had mutations in the gyrA and pbp5 genes. This supports the notion that members of CC17 are reservoirs of multidrug-resistance genes in the environment [50]. Hospital SNP profiles for both E. faecalis and E. faecium. (Bold and underlined text in Tables 4 and 5), were antibiotic-resistant by both disc and PCR methods.
The SNP profiles in bold text in Tables 4 and 5 highlight the isolates that had the same SNP profile but had different antibiotic-resistant gene profiles which resulted in sub-dividing the SNP profiles. A possible explanation for this is that the SNPs interrogated by our method, are located in housekeeping genes, which are considered conservative, whereas, antibiotic resistance determinants are "mobile" except for the gyrA and pbp5 genes. E. faecalis SNP IDs 2, 16 and 26 and E. faecium SNP IDs 3, 7, 13 and 14 were sub-divided into two groups. In addition, E. faecalis isolates with SNP ID 9 and E. faecium SNP ID 2 can be can be sub-divided in to three groups. These antibiotic-resistant profiles can be used to increase the resolving power of the SNP typing method.
Conclusion
This study describes the prevalence and distribution of E. faecalis and E. faecium SNP profile genotypes in the Coomera River. The SNP genotyping method demonstrates a high diversity in the E. faecalis and E. faecium population in the Coomera River. In addition, at three sampling sites (Jabiru Island, Paradise Point and Coombabah), the enterococcal counts were above the USEPA acceptable levels after rainfall events. According to the Australian NHMRC Guidelines these sampling sites are category B and C areas according to the microbial water quality assessment (after rainfall), with category B indicating a 1-5% gastrointestinal illness risk and category C indicating a 5-10% gastrointestinal illness risk. We have also demonstrated the application of the SNP genotyping method to identify both human-related and human-specific E. faecium and E. faecalis strains in environmental water sources. This method shows promise as a rapid and robust test to determine human faecal contamination of environmental water sources. Some strains were antibiotic resistant and these antibiotic resistant profiles can be used as binary markers to increase the discriminatory power of the SNP genotyping method.
Authors' contributions
IUR performed the experiments, analysed the data and drafted the manuscript. MH assisted with the drafting of the manuscript. FH conceived the study, contributed to the experimental design, co-ordinated data analysis and assisted with the drafting of the manuscript. All authors have read and approved the final manuscript.
Supplementary Material
Statistical analysis Mann-Whitney test. This test was performed to determine whether there was a significant increase in total enterococcal counts (cfu/ml) at each location after rainfall events.
e-BURST diagrams of both E. faecium and E. faecalis MLST databases. Each diagram shows the new STs found in the present study compared to all the STs currently listed in both databases.
Disc susceptibility test results for E. faecalis. This table lists the antibiotic disc susceptibility profiles for all E. faecalis isolates tested in this study.
Disc susceptibility test results for E. faecium. This table lists the antibiotic disc susceptibility profiles for all E. faecium isolates tested in this study.
Phenotypic and genotypic antibiotic resistance profiles of E. faecalis isolated at each site. Antibiotic resistance profiles together with the E. faecalis SNP profiles of strains isolated at all the sampling sites are listed here.
Phenotypic and genotypic antibiotic resistance profiles of E. faecium isolated at each site. Antibiotic resistance profiles together with the E. faecium SNP profiles of strains isolated at all the sampling sites are listed here.
Contributor Information
Irani Rathnayake, Email: i.rathnayake@qut.edu.au.
Megan Hargreaves, Email: m.hargreaves@qut.edu.au.
Flavia Huygens, Email: f.huygens@qut.edu.au.
Acknowledgements
We wish to acknowledge Dr. Barbara Murray and Karen Jacques-Plaz (University of Texas) for the supply of ST 2, 6, and 9 E. faecalis strains. We thank Tharindi Gunararhna for providing statistical analysis assistance. Irani U. Rathnayake is in receipt of an International Post Graduate Research Scholarship (IPRS) and the study is supported by the Institute of Sustainable Resources, QUT.
References
- Ratajczak M, Laroche E, Berthe T, Clermont O, Pawlak B, Denamur E, Petit F. Influence of hydrological conditions on the Escherichia coli population structure in the water of a creek on a rural watershed. BMC Microbiol. 2010;10 doi: 10.1186/1471-2180-10-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruss A. Review of epidemiological studies on health effects from exposure to recreational water. Int J Epidemiol. 1998;27(1):1–9. doi: 10.1093/ije/27.1.1. [DOI] [PubMed] [Google Scholar]
- Layton BA, Walters SP, Lam LH, Boehm AB. Enterococcus species distribution among human and animal hosts using multiplex PCR. J Appl Microbiol. 2010;109(2):539–547. doi: 10.1111/j.1365-2672.2010.04675.x. [DOI] [PubMed] [Google Scholar]
- Davis K, Anderson MA, Yates MV. Distribution of indicator bacteria in Canyon Lake, California. Water Res. 2005;39(7):1277–1288. doi: 10.1016/j.watres.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Grammenou P, Spiliopolullou I, Sazakli E, Papapetropoulou M. PFGE analysis of enterococci isolates from recreational and drinking water in Greece. J Water Health. 2006;4(2):263–269. [PubMed] [Google Scholar]
- Kinzelman J, Ng C, Jackson E, Gradus S, Bagley R. Enterococci as Indicators of Lake Michigan Recreational Water Quality: Comparison of Two Methodologies and Their Impacts on Public Health Regulatory Events. Appl Environ Microbiol. 2003;69(1):92–96. doi: 10.1128/AEM.69.1.92-96.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood VJ, Delahoya NC, Ulrich RM, Kramer MF, Whitlock JE, Garey JR, Lim DV. Molecular confirmation of Enterococcus faecalis and E. faecium from clinical, faecal and environmental sources. Lett Appl Microbiol. 2004;38(6):476–482. doi: 10.1111/j.1472-765X.2004.01518.x. [DOI] [PubMed] [Google Scholar]
- He J-W, Jiang S. Quantification of Enterococci and Human Adenoviruses in Environmental Samples by Real-Time PCR. Appl Environ Microbiol. 2005;71(5):2250–2255. doi: 10.1128/AEM.71.5.2250-2255.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USEPA. Bacterial water quality standards for recreational waters (freshwater and marine waters),status report EPA-823-R-03-008. Washington DC: US Environmental Protection Agency; 2003. [Google Scholar]
- NHMRC. The Guidelines for Managing Risks in Recreational Water. Canberra, Australia: NHMRC publications; 2008. [Google Scholar]
- Farrell DJ, Morrissey I, De Rubeis D, Robbins M, Felmingham D. A UK Multicentre Study of the Antimicrobial Susceptibility of Bacterial Pathogens Causing Urinary Tract Infection. J Infect. 2003;46(2):94–100. doi: 10.1053/jinf.2002.1091. [DOI] [PubMed] [Google Scholar]
- Das I, Gray J. Enterococcal bacteremia in children: a review of seventy-five episodes in a pediatric hospital. Pediatr Infect Dis J. 1998;17(12):1154–1158. doi: 10.1097/00006454-199812000-00011. [DOI] [PubMed] [Google Scholar]
- Low Donald E, Keller N, Barth A, Jones Ronald N. Clinical Prevalence, Antimicrobial Susceptibility, and Geographic Resistance Patterns of Enterococci: Results from the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis. 2001;32(S2):S133–S145. doi: 10.1086/320185. [DOI] [PubMed] [Google Scholar]
- Kuzucu C, Cizmeci Z, Durmaz R, Durmaz E, Ozerol IH. The prevalence of fecal colonization of enterococci, the resistance of the isolates to ampicillin, vancomycin, and high-level aminoglycosides, and the clonal relationship among isolates. Microb Drug Resist. 2005;11(2):159–164. doi: 10.1089/mdr.2005.11.159. [DOI] [PubMed] [Google Scholar]
- Mannu L, Paba A, Pes M, Floris R, Scintu MF, Morelli L. Strain typing among enterococci isolated from home-made Pecorino Sardo cheese. FEMS Microbiol Lett. 1999;170(1):25–30. doi: 10.1111/j.1574-6968.1999.tb13351.x. [DOI] [PubMed] [Google Scholar]
- Dicuonzo G, Gherardi G, Lorino G, Angeletti S, Battistoni F, Bertuccini L, Creti R, Rosa R, Venditti M, Baldassarri L. Antibiotic resistance and genotypic characterization by PFGE of clinical and environmental isolates of enterococci. FEMS Microbiol Lett. 2001;201(2):205–211. doi: 10.1111/j.1574-6968.2001.tb10758.x. [DOI] [PubMed] [Google Scholar]
- Gilmore MS, ed. The Enterococci: Pathogenesis, Molecular Biology and Antibiotic Resistance and Infection Control. Wiley; 2002. [Google Scholar]
- Salminen S, Wright AV. Lactic acid bacteria. Microbiological and functional aspects. New York: Mercel Dekker; 2004. [Google Scholar]
- Murray BE. The life and times of the Enterococcus. Clin Microbiol Rev. 1990;3(1):46–65. doi: 10.1128/cmr.3.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chenoweth C, Schaberg D. The epidemiology of Enterococci. Eur J Clin Microbiol Infect Dis. 1990;9(2):80–89. doi: 10.1007/BF01963631. [DOI] [PubMed] [Google Scholar]
- Gelsomino R, Vancanneyt M, Cogan TM, Swings J. Effect of Raw-Milk Cheese Consumption on the Enterococcal Flora of Human Feces. Appl Environ Microbiol. 2003;69(1):312–319. doi: 10.1128/AEM.69.1.312-319.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruoff KL, de la Maza L, Murtagh MJ, Spargo JD, Ferraro MJ. Species identities of enterococci isolated from clinical specimens. J Clin Microbiol. 1990;28(3):435–437. doi: 10.1128/jcm.28.3.435-437.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manero A, Vilanova X, Cerdà-Cuéllar M, Blanch AR. Characterization of sewage waters by biochemical fingerprinting of Enterococci. Water Res. 2002;36(11):2831–2835. doi: 10.1016/S0043-1354(01)00486-9. [DOI] [PubMed] [Google Scholar]
- Vos P, Hogers R, Bleeker M, Reijans M, Lee Tvd, Hornes M, Friters A, Pot J, Paleman J, Kuiper M. et al. AFLP: a new technique for DNA fingerprinting. Nucleic Acids Res. 1995;23(21):4407–4414. doi: 10.1093/nar/23.21.4407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodford N, Tysall L, Auckland C, Stockdale MW, Lawson AJ, Walker RA, Livermore DM. Detection of Oxazolidinone-Resistant Enterococcus faecalis and Enterococcus faecium Strains by Real-Time PCR and PCR-Restriction Fragment Length Polymorphism Analysis. J Clin Microbiol. 2002;40(11):4298–4300. doi: 10.1128/JCM.40.11.4298-4300.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zdragas A, Partheniou P, Kotzamanidis C, Psoni L, Koutita O, Moraitou E, Tzanetakis N, Yiangou M. Molecular characterization of low-level vancomycin-resistant enterococci found in coastal water of Thermaikos Gulf, Northern Greece. Water Res. 2008;42(4-5):1274–1280. doi: 10.1016/j.watres.2007.09.022. [DOI] [PubMed] [Google Scholar]
- Coque TM, Seetulsingh P, Singh KV, Murray BE. In: Molecular Bacteriology. Woodford N, Johnson AP, editor. Vol. 15. Humana Press; 1998. Application of Molecular Techniques to the Study of Nosocomial Infections Caused by Enterococci; pp. 469–493. [DOI] [PubMed] [Google Scholar]
- Zhu X, Zheng B, Wang S, Willems RJL, Xue F, Cao X, Li Y, Bo S, Liu J. Molecular characterisation of outbreak-related strains of vancomycin-resistant Enterococcus faecium from an intensive care unit in Beijing, China. J Hosp Infect. 2009;72(2):147–154. doi: 10.1016/j.jhin.2009.02.014. [DOI] [PubMed] [Google Scholar]
- Rathnayake IU, Hargreaves M, Huygens F. Genotyping of Enterococcus faecalis and Enterococcus faecium Isolates by Use of a Set of Eight Single Nucleotide Polymorphisms. J Clin Microbiol. 2011;49(1):367–372. doi: 10.1128/JCM.01120-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USEPA. Method 1600: membrane filter test method for enterococci in water. EPA/821/R-02/022. Washington, D.C: Office of Water, U.S. Environmental Protection Agency; 2002. [Google Scholar]
- Messer JW, Dufour AP. A Rapid, Specific Membrane Filtration Procedure for Enumeration of Enterococci in Recreational Water. Appl Environ Microbiol. 1998;64(2):678–680. doi: 10.1128/aem.64.2.678-680.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facklam RR, Collins MD. Identification of Enterococcus species isolated from human infections by a conventional test scheme. J Clin Microbiol. 1989;27(4):731–734. doi: 10.1128/jcm.27.4.731-734.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CLSI. PERFORMANCE Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard-Tenth Edition. CLSI document M02-A10. Wayn: Clinical and Laboratory Standards Institute; 2009. [Google Scholar]
- Korten V, Huang WM, Murray BE. Analysis by PCR and direct DNA sequencing of gyrA mutations associated with fluoroquinolone resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1994;38(9):2091–2094. doi: 10.1128/aac.38.9.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rybkine T, Mainardi J-L, Sougakoff W, Collatz E, Gutmann L. Penicillin-Binding Protein 5 Sequence Alterations in Clinical Isolates of Enterococcus faecium with Different Levels of β-Lactam Resistance. J Infect Dis. 1998;178(1):159–163. doi: 10.1086/515605. [DOI] [PubMed] [Google Scholar]
- Leavis HL, Willems RJL, Top J, Bonten MJM. High-Level Ciprofloxacin Resistance from Point Mutations in gyrA and parC Confined to Global Hospital-Adapted Clonal Lineage CC17 of Enterococcus faecium. J Clin Microbiol. 2006;44(3):1059–1064. doi: 10.1128/JCM.44.3.1059-1064.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Armisen T, Servais P. Respective contributions of point and non-point sources of E. coli and enterococci in a large urbanized watershed (the Seine river, France) J Environ Manage. 2007;82(4):512–518. doi: 10.1016/j.jenvman.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Stumpf CH, Piehler MF, Thompson S, Noble RT. Loading of fecal indicator bacteria in North Carolina tidal creek headwaters: Hydrographic patterns and terrestrial runoff relationships. Water Res. 2010;44(16):4704–4715. doi: 10.1016/j.watres.2010.07.004. [DOI] [PubMed] [Google Scholar]
- Brownell MJ, Harwood VJ, Kurz RC, McQuaig SM, Lukasik J, Scott TM. Confirmation of putative stormwater impact on water quality at a Florida beach by microbial source tracking methods and structure of indicator organism populations. Water Res. 2007;41(16):3747–3757. doi: 10.1016/j.watres.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Jeng HAC, Englande AJ, Bakeer RM, Bradford HB. Impact of urban stormwater runoff on estuarine environmental quality. Estuar Coast Shelf Sci. 2005;63(4):513–526. doi: 10.1016/j.ecss.2004.11.024. [DOI] [Google Scholar]
- Parker JK, McIntyre D, Noble RT. Characterizing fecal contamination in stormwater runoff in coastal North Carolina, USA. Water Res. 2010;44(14):4186–4194. doi: 10.1016/j.watres.2010.05.018. [DOI] [PubMed] [Google Scholar]
- Tyrrel SF, Quinton JN. Overland flow transport of pathogens from agricultural land receiving faecal wastes. J Appl Microbiol. 2003;94:87–93. doi: 10.1046/j.1365-2672.94.s1.10.x. [DOI] [PubMed] [Google Scholar]
- Carroll SP, Dawes L, Hargreaves M, Goonetilleke A. Faecal pollution source identification in an urbanising catchment using antibiotic resistance profiling, discriminant analysis and partial least squares regression. Water Res. 2009;43(5):1237–1246. doi: 10.1016/j.watres.2008.12.017. [DOI] [PubMed] [Google Scholar]
- Shibata T, Solo-Gabriele HM, Fleming LE, Elmir S. Monitoring marine recreational water quality using multiple microbial indicators in an urban tropical environment. Water Res. 2004;38(13):3119–3131. doi: 10.1016/j.watres.2004.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leavis HL, Bonten MJM, Willems RJL. Identification of high-risk enterococcal clonal complexes: global dispersion and antibiotic resistance. Curr Opin Microbiol. 2006;9(5):454–460. doi: 10.1016/j.mib.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Top J, Willems R, Bonten M. Emergence of CC17 Enterococcus faecium: from commensal to hospital-adapted pathogen. FEMS Immunol Med Microbiol. 2008;52(3):297–308. doi: 10.1111/j.1574-695X.2008.00383.x. [DOI] [PubMed] [Google Scholar]
- Willems RJ, Bonten MJ. Glycopeptide-resistant enterococci: deciphering virulence, resistance and epidemicity. Curr Opin Infect Dis. 2007;20(4):384–390 310. doi: 10.1097/QCO.0b013e32818be63d. 1097/QCO.1090b1013e32818be32863d. [DOI] [PubMed] [Google Scholar]
- Maietti L, Bonvini B, Huys G, Giraffa G. Incidence of antibiotic resistance and virulence determinants among Enterococcus italicus isolates from dairy products. Syst Appl Microbiol. 2007;30(6):509–517. doi: 10.1016/j.syapm.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Mohn SC, Ulvik A, Jureen R, Willems RJL, Top J, Leavis H, Harthug S, Langeland N. Duplex Real-Time PCR Assay for Rapid Detection of Ampicillin-Resistant Enterococcus faecium. Antimicrob Agents Chemother. 2004;48(2):556–560. doi: 10.1128/AAC.48.2.556-560.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitas AR, Novais C, Ruiz-Garbajosa P, Coque TM, Peixe L. Dispersion of Multidrug-Resistant Enterococcus faecium Isolates Belonging to Major Clonal Complexes in Different Portuguese Settings. Appl Environ Microbiol. 2009;75(14):4904–4908. doi: 10.1128/AEM.02945-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Statistical analysis Mann-Whitney test. This test was performed to determine whether there was a significant increase in total enterococcal counts (cfu/ml) at each location after rainfall events.
e-BURST diagrams of both E. faecium and E. faecalis MLST databases. Each diagram shows the new STs found in the present study compared to all the STs currently listed in both databases.
Disc susceptibility test results for E. faecalis. This table lists the antibiotic disc susceptibility profiles for all E. faecalis isolates tested in this study.
Disc susceptibility test results for E. faecium. This table lists the antibiotic disc susceptibility profiles for all E. faecium isolates tested in this study.
Phenotypic and genotypic antibiotic resistance profiles of E. faecalis isolated at each site. Antibiotic resistance profiles together with the E. faecalis SNP profiles of strains isolated at all the sampling sites are listed here.
Phenotypic and genotypic antibiotic resistance profiles of E. faecium isolated at each site. Antibiotic resistance profiles together with the E. faecium SNP profiles of strains isolated at all the sampling sites are listed here.