Abstract
INTRODUCTION
Femoro-acetabular impingement (FAI) was first described in 1999 as abnormal abutment between the acetab-ulum and the femoral head and neck. Since then, it has been shown to be responsible for many acetabular labral tears and is implicated in the aetiology of osteoarthritis of the hip. This review introduces the concept of FAI and reports the key aspects of its diagnosis and management.
MATERIALS AND METHODS
A comprehensive search of the literature was conducted using the Pubmed database. Articles relating to the aetiology, pathophysiology, clinical features, diagnosis and treatment of FAI were reviewed. Search terms included femoro-acetabular impingement, arthroscopic treatment, open treatment, aetiology, pathophysiology. The search was limited to articles published in English. All articles were read in full by the authors and selected for inclusion based on relevance to the article.
RESULTS
An increasing number of studies relating to FAI have been produced in the 10 years since its recognition. A range of clinical and radiological features have been described. Surgical management can be performed using a number of techniques, with promising results from various studies. Early treatment with open surgery has paved the way for less invasive and arthroscopic approaches, with short-to-medium term data demonstrating favourable functional results for arthroscopic treatment of FAI.
CONCLUSIONS
A greater awareness of the diagnostic features of FAI, and the various management options available, will allow timely diagnosis and treatment of a relatively newly recognised syndrome. Early treatment may then help to prevent progression to end-stage osteoarthritis of the hip.
Keywords: Hip joint, Impingement, Acetabulum, Arthroscopy, Osteoarthritis, Hip
Femoro-acetabular impingement (FAI) is defined as abnormal abutment between the femoral head, or the femoral head-neck junction, and the acetabulum.1 It was initially described by Myers et al. in 1999, who noted abnormal abutment between the femoral neck and the acetabular rim in a cohort of patients undergoing peri-acetabular osteotomy. In the ensuing decade, FAI has become the subject of a large number of studies examining the anatomical, clinical, and radiological features of FAI, and outcomes of various methods of surgical management. FAI has been shown to be responsible for a large proportion of tears of the acetabular labrum - a major cause of hip pain in young adults.2 Furthermore, it is now established that FAI is a major aeti-ological factor in the development of osteoarthritis of the hip, a condition which is expected to become increasingly prevalent in the coming years.3,4
A number of conditions are associated with FAI. Slipped upper femoral epiphysis (SUFE) in childhood has been shown by various authors to produce FAI in later life.5,6 In addition, Legg-Calve-Perthes disease,7 developmental hip dysplasia,8 and malunited fractures of the femoral neck9 are also associated with the anatomical abnormalities which cause FAI.
A number of studies have demonstrated a genetic component to osteoarthritis, with evidence from family and twin studies indicating vertical transmission of primary osteoarthritis in Caucasians.10–12 Furthermore, it has been shown that genetic factors are largely responsible for variations in hip and acetabular morphology and cartilage thickness.13 FAI resulting from abnormal hip joint anatomy is responsible for a proportion of cases of osteoarthritis and is, therefore, likely to involve a significant genetic component in its aetiology. With wider recognition of the causes and sequalae of FAI, early diagnosis and effective treatment may help to prevent progression to osteoarthritis, and reduce the subsequent need for hip arthroplasty and its associated risks.
Pathophysiology
FAI is divided into two distinct pathomechanical types - cam type and pincer type (Fig. 1). Cam-type FAI refers to an abnormality in the shape of the femoral head and neck. The lesion is an osseous prominence at the femoral head-neck junction which is thought to resemble a cam, a term applied to an eccentric prominence in a rotating mechanism which converts rotary motion into linear motion. When the hip as flexed, the osseous prominence makes contact with the anterosuperior aspect of the acetabulum, resulting in a mechanical blockage to continued flexion and/or rotation within the acetabulum. The shear forces transferred from the cam to the acetabulum cause progressive cartilage erosion, delamination, and progression to osteoarthritis of the hip joint.14 There is frequently concomitant damage to the adjacent acetabular labrum, producing localised inflammatory changes and tears. Cam lesions are greatest at the lateral and anterior aspects of the femoral neck in younger, predominantly male patients, whereas in older, female patients, the lesion is seen more commonly at the anterior aspect of the head-neck junction.15
Figure 1.
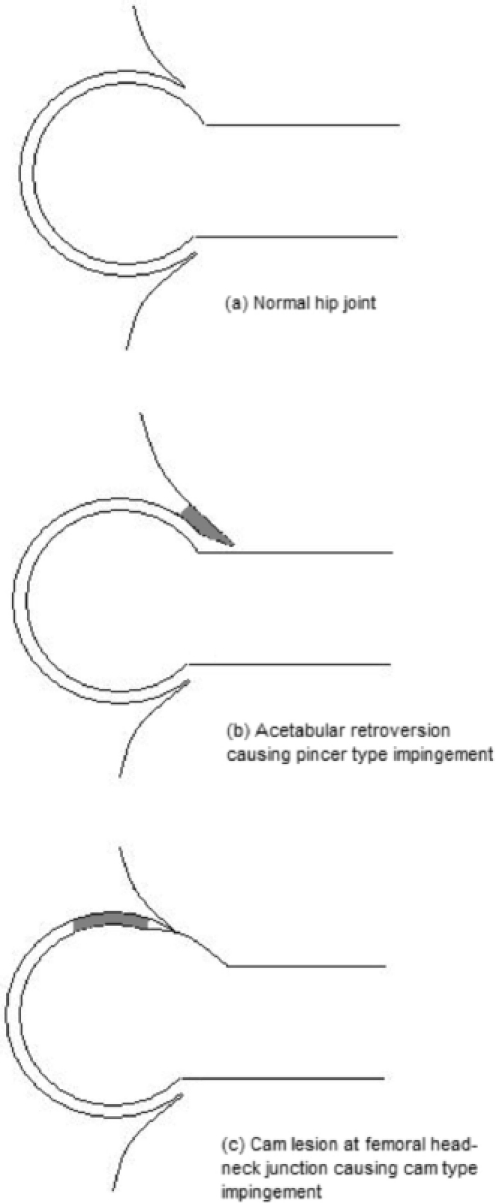
Mechanisms of femoroacetabular impingement. Pincertype FAI occurs due to acetabular retroversion, leading to labral and acetabular damage at the anterior rim (B; shaded area). Cam-type FAI results from a prominent head-neck junction, leading to chondral damage within the anterosuperior acetabulum (C; shaded area).
Pincer-type FAI is due to an abnormality on the acetabular side, with the anterior rim of the acetabulum covering the anterior aspect femoral head over a greater area than usual. This may be due to acetabular retroversion, in contrast to normal acetabular anteversion. Alternatively, it may be due to a generalised deepening of the acetabulum, as seen in acetabular pro-trusio. The resultant anterior coverage of the femoral head by acetabular bone causes impingement in hip flexion, with direct contact between the femoral head-neck junction and the acetabular labrum. Labral inflammatory changes, tears, and subsequent bony damage to the acetabular rim ensue, with pain and stiffness in extremes of flexion, and internal/external rotation. There may also be reciprocal damage to posterior acetabular cartilage, due to posterior displacement of the femoral head within the acetabulum at the point of contact between the femoral neck and the anterior acetabulum.15 Patients may have isolated pincer- or cam-type FAI, or a combination of both a cam lesion and pincer impingement due to an acetabular abnormality.16
Clinical features
The diagnosis of FAI is made from characteristic clinical findings and subsequent imaging studies. Clinical features of FAI include pain on the affected side, felt in the groin in 83% of patients.17 Pain may also be felt in the gluteal region, trochanteric region, or in the thigh. Symptoms most commonly begin as an intermittent discomfort, often during or following periods of repetitive hip motion (e.g. running, walking), progressing to more constant and intense pain. Stiffness is common, with reductions in the range of hip flexion, and internal rotation in particular. Patients may also complain of clicking, popping, or snapping sensations in the affected hip.18
Examination findings usually include pain and stiffness in extremes of flexion and internal rotation. Flexion is often limited to approximately 90°, and reduced compared with contralateral hips, and internal rotation may be severely restricted to just a few degrees. There is usually a positive impingement sign, with pain on adduction of a flexed, internally rotated hip.19 The FABER test (flexion, abduction, external rotation), in which the patient crosses the leg on the affected side over the other, in a figure-of four configuration, with the examiner measuring the distance from the ipsilateral knee to the bed when applying downward pressure to the knee, can be performed. The test is positive if the distance measured is greater than the equivalent measurement on the opposite side, when the manoeuvre is repeated for the contralateral leg.
Diagnosis
Cam lesions are recognisable on plain anteroposterior radiographs of the pelvis with prominent, convex head neck junctions, reduced head-neck offset, and asphericity of the femoral head. This appearance of the proximal femur has in the past been referred to as ‘pistol grip deformity’, which has been linked with osteoarthritis of the hip since the 1970s.20,21
Acetabular retroversion is seen in anteroposterior radiographs as a ‘cross-over sign’. Described by Reynolds and colleagues,22 this refers to the appearance of the lateral margin of the anterior acetabular rim lying laterally in its superior portion to that of the posterior margin. The anterior rim is seen to cross the posterior rim as they are both followed inferiorly, with the anterior margin becoming medial to the posterior margin at its caudal aspect. There may also be acetabular protrusio, visible as a generalised deepening of the acetabulum on anteroposterior radiographs with the dome appearing to breach the pelvic brim. Additionally, radiographic evidence of osteoarthritis of the hip joint may be present in the presence of long-standing FAI.23
On lateral cross-table radiographs of the hip, femoral head asphericity in patients with cam-type FAI can be visualised, and ‘alpha angle’ can be measured.24 A quantification of femoral head asphericity, this refers to the angle between a radial line from the centre of rotation of the femoral head to the anterior head-neck junction, and a line from the centre of rotation running parallel with the longitudinal axis of the femoral neck. Alpha angle of greater than 55° has been shown to be associated with an increased likelihood of FAI.21,25 Alternatively, frog-leg lateral views have been shown to demonstrate cam lesions accurately.26 Asphericity and alpha angle can also be assessed using the Dunn 45° view, a lateral radiograph projection with the hip in 45° of flexion, with a lesser degree of internal rotation and abduction.27
Magnetic resonance imaging (MRI) for the diagnosis of FAI has been used with increasing frequency in recent years. Using gadolinium-enhanced MR arthrography, Noztli et al.25 produced the first quantitative study of femoral head asphericity, describing the alpha angle and reporting that values of greater than 55° are indicative of FAI. Using MRI, cam lesions of the femoral head have been shown to be greater at anterosuperior aspects of the femoral neck in cam impingement compared with pincer-type FAI. Furthermore, postero-inferior chondral damage within the acetabulum may be seen, caused by a backwards levering motion of the femoral head, as the proximal femur impinges anteriorly during flexion.28
It is worth noting that measurements of alpha angle based on MRI studies have been shown to be subject to poor intra-observ-er reliability, with variability between measurements of up to 30%.29 However, it remains a widely used method for the quantification of abnormal proximal femoral morphology relating to FAI, despite recent evidence suggesting that clinical features alone may be more reliable a predictor of FAI.30
Measurements in head-neck offset can also be undertaken using MRI, and evidence of chondral damage and delamination within the acetabulum or on the femoral head may also be characterised.31 Defects of the acetabular labrum, such as cystic degeneration and tears, are most reliably imaged using MR arthrography.32
In addition to MRI, computed tomography is being used with increasing frequency. Using 3-dimensional reconstruction of computed tomography imaging (3D-CT), cam lesions can be assessed, and alpha angle quantified. The beta angle can also be measured, which is the angle at which the posterior aspect of the femoral head becomes aspherical. In addition, calculation of the alpha-beta angle ratio has been shown to be a more sensitive diagnostic measurement than alpha angle alone in patients with symptomatic FAI, using 3D-CT.33 Chondral defects are particularly visible using 3D-CT, such as chondral delamination in the anterosuperior acetabulum due to cam-type impingement In addition, the contour of the head-neck junction can be accurately visualised in 3D-CT, aiding the operating surgeon with the planning of subsequent treatment.
Management
Although a number of authors have shown an association between FAI and subsequent osteoarthritis of the hip joint, not all patients with FAI will progress to end-stage disease requiring intervention. It is estimated that one-third of patients with mild osteoarthritis in the presence of FAI will take more than 10 years to develop end-stage osteoarthritis, if at all.34 The bony abnormalities responsible for FAI are of unknown prevalence, and many patients are asymptomatic and unaware of subtle anatomical aberrations. Incidental cam lesions or acetabular retroversion, potentially causing labral damage due to pincer mechanisms, do not necessarily require operative intervention. A watch-and-wait approach and close follow-up with a lower limb/pelvic reconstruction service may be indicated, given the risks associated with either arthroscopic or open surgical correction. However, clinicians should be aware that delay of surgical correction may lead to chondral damage and disease progression, to a stage where joint preservation procedures may be of little benefit.35
Progression to osteoarthritis of the hip is not ubiquitous and pathology may be confined to labral injury. As such, conservative treatment with activity modification to reduce unnecessary hip motion and restriction of athletic activities may help, in conjunction with non-steroidal anti-inflammatory preparations.36 A peri-acetabular osteotomy may be used for retroversion of the acetabulum without additional treatment of abnormal femoral anatomy.
Operative treatment of FAI is principally aimed at reducing cam lesions and increasing femoral head-neck offset (osteo-chondroplasty), and treating associated soft tissue lesions such as labral tears.37 Acetabular recession with labral re-attachment is increasingly used for pincer lesions but great care is needed to ensure that overall coverage of the hip is not adversely reduced.38
Open surgical dislocation of the hip with osteochondroplasty was the mainstay of early surgical management.39–42 Subsequently, mini-open anterior approaches with the use of arthroscopic assistance were developed, producing encouraging results in a number of studies.43–15 More recently, as proficiency with arthroscopic techniques has improved, arthroscopic osteochondroplasty and labral debridement have become increasingly popular for the treatment for FAI, with promising functional results in a range of studies.
In a prospective analysis of 112 patients undergoing primary hip arthroscopy for symptomatic FAI, Philippon et al.46 demonstrated a significant improvement in pre-operative Harris hip scores (HHS) from a mean of 58 to a postoperative mean of 84, at a mean follow-up of 2.3 years. Eighty-nine cases underwent both osteochondroplasty and peri-acetabular osteotomy for mixed FAI, 23 patients underwent osteoplasty only for isolated CAM lesions, and 3 underwent acetabular trimming for isolated pincer FAI.
These results were echoed by Byrd and Jones,47 in a prospective study of 207 hips with cam-type (163 hips) or combined cam and pincer (44 hips) FAI in a total of 200 patients. At a minimum follow-up of 12 months (mean, 16 months; range, 12-24 months) mean HHS improved by a mean of 20 points (range, -17 to 60), with 83% of patients showing an improvement at their most recent follow-up. Of the patients followed up for 2 years, all HHS scores were maintained from the 12-month values. Similar results have been produced in a number of smaller retrospective series,48–53 but outcome data past the 2-year follow-up mark are scarce.
In addition to osteochondroplasty, there is evidence to suggest that repair of the acetabular labrum is associated with a more favourable functional outcome. In a retrospective comparative study of 75 hips with either pincer- or combined cam- and pin-cer-type FAI, all with associated labral defects treated by either arthroscopic debridement (36 hips) or repair (39 hips), a better clinical and radiological outcome was seen in the labral repair group compared with the debridement group.54 Further prospective work is required to assess the benefit of arthroscopic labral repair versus debridement, in addition to osteochondroplasty, in the treatment of cam or combined cam and pincer FAI.
Despite improvements in arthroscopic techniques and the increasing number of surgeons performing such procedures, arthroscopic treatment of FAI remains a relatively new technique. As a result, medium- to long-term data relating to hip arthroscopy for FAI are elusive. Open surgery remains a viable treatment option, but differences in recovery times compared with arthroscopic treatment make this a less attractive option. In one study of open treatment of FAI, Beaule et al.42 reported an improvement in mean pre-operative WOMAC score from 61.2 to 81.4 at a mean follow-up time of 3.1 years (P < 0.001). The postoperative recovery period involved partial weight-bearing with the use of crutches for 6 weeks, followed by physiotherapy for a further 6-8 weeks. Of the 34 patients studied, 9 required further surgery for removal of metal from the greater trochanter due to persistent bursitis. Additionally, 6 patients were dissatisfied with the outcome.
By contrast, arthroscopic treatment allows weight-bearing as tolerated in the immediate postoperative period, with range-of-motion and strengthening exercises commenced early. Some authors continue to protect from impact loading for a period of 5 months. In addition, microfracture of chondral surfaces due to significant cartilage loss would necessitate protected weight-bearing status for the first 2 months.40 Following this period, most patients are able to resume a normal level of activity although athletes frequently require a further 1-3 months before a return to full levels of activity.47
Conclusions
Femoro-acetabular impingement is increasingly being recognised as a cause of hip pain in young, active individuals. As arthroscopic treatment becomes more wide-spread, data on the medium- to long-term outcomes will provide surgeons with agreed standards for treatment. Awareness of the clinical and radiological features of FAI, in addition to treatment options available and their efficacy, will aid clinicians in early diagnosis. This may help to prevent progression to osteoarthritis, and the consequent need for hip arthroplasty procedures.
References
- 1.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop. 1999;363:93–9. [PubMed] [Google Scholar]
- 2.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop. 2004;429:262–71. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–8. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 5.Fraitzl CR, Kafer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis. J Bone Joint Surg Br. 2007;89:1592–6. doi: 10.1302/0301-620X.89B12.19637. [DOI] [PubMed] [Google Scholar]
- 6.Rab GT. The geometry of the slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Paediatr Orthop. 1999;19:419–24. doi: 10.1097/00004694-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Friend L, Kelly BT. Femoroacetabular impingement and labral tears in the adolescenthip: diagnosis and surgical advances. Curr Opin Paediatr. 2009;21:71–6. doi: 10.1097/mop.0b013e328320a945. [DOI] [PubMed] [Google Scholar]
- 8.Li P, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop. 2003;416:245–53. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 9.Eijer H, Myers SR, Ganz R. Femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–81. doi: 10.1097/00005131-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Chapman K, Takahashi A, Meulenbelt I, Watson C, Rodriguez-Lopez J, et al. A meta-analysis of European and Asian cohorts reveals a global role of a functional SNP in the 5' UTR of GDF5 with osteoarthritis susceptibility. Hum Mol Genet. 2008;17:1497–504. doi: 10.1093/hmg/ddn038. [DOI] [PubMed] [Google Scholar]
- 11.Spencer JM, Loughlin J, Clipsham K, Carr AJ. Genetic background increases the risk of hip osteoarthritis. Clin Orthop. 2005;431:134–7. doi: 10.1097/01.blo.0000149242.85548.00. [DOI] [PubMed] [Google Scholar]
- 12.MacGregor AJ, Li Q, Spector TD, Williams FM. The genetic influence on radiographic osteoarthritis is site specific at the hand, hip and knee. Rheumatology. 2009;48:277–80. doi: 10.1093/rheumatology/ken475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antoniades L, Spector TD, MacGregor AJ. The genetic contribution to hip joint morphometry and relationship to hip cartilage thickness. Osteoarthritis Cartilage. 2001;9:593–5. doi: 10.1053/joca.2001.0426. [DOI] [PubMed] [Google Scholar]
- 14.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement. Current status and future perspectives. Clin Orthop. 2009;467:616–22. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ito K, Minka-II MA, Leunig S, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head neck-offset. J Bone Joint Surg Br. 2001;83:171–6. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 16.Siebenbrock KA, Kalbernatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelvises from cadavers. Clin Orthop. 2003;407:241–8. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 17.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage. J Bone J Surg Br. 2005;87:1012–8. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 18.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Heyes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop. 2009;467:638–44. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–7. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald SJ, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9. [Google Scholar]
- 21.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–83. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 22.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–8. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 23.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis: relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489–97. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings in femoroacetabular impingement syndrome. Skelet Radiol. 2005;34:691–701. doi: 10.1007/s00256-005-0932-9. [DOI] [PubMed] [Google Scholar]
- 25.Notzli HP, Wyss TF, Stoeklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–60. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 26.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualised hip cam impingement abnormalities. Clin Orthop. 2007;462:115–21. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 27.Dunn DM. Anteversion of the neck of the femur: a method of measurement. J Bone Joint Surg Br. 1952;34:181–6. doi: 10.1302/0301-620X.34B2.181. [DOI] [PubMed] [Google Scholar]
- 28.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/ neck asphericity. Clin Orthop. 2006;445:181–5. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 29.Pfirrmann CWA, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–85. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 30.Lohan DG, Seeger LL, Motamedi K, Hame S, Sayre J. Cam-type femoral-acetabular impingement: is the alpha angle the best MR arthrography has too offer? Skelet Radiol. 2009;38:855–62. doi: 10.1007/s00256-009-0745-3. [DOI] [PubMed] [Google Scholar]
- 31.Beaule PE, Zaragoza EJ, Copelan N. Magnetic resonance imaging with gadolinium arthrography to assess acetabular cartilage delamination. A report of four cases. J Bone Joint Surg Am. 2004;86:2294–8. doi: 10.2106/00004623-200410000-00025. [DOI] [PubMed] [Google Scholar]
- 32.Leunig M, Werlen S, Ungersbock A, Ito K, Ganz R. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79:230–4. doi: 10.1302/0301-620x.79b2.7288. [DOI] [PubMed] [Google Scholar]
- 33.Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286–92. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 34.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:162–9. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 35.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement. Current status and future perspectives. Clin Orthop. 2009;467:616–22. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lavigne M, Parvizi J, Beck M, Siebenbrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement. Part 1. Techniques of joint preserving surgery. Clin Orthop. 2004;418:61–6. [PubMed] [Google Scholar]
- 37.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoroacetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–35. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 38.Siebenbrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–86. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 39.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–24. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 40.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop. 2004;418:67–73. [PubMed] [Google Scholar]
- 41.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88:1735–41. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 42.Baeule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Br. 2007;89:773–9. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 43.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop. 2009;467:747–52. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lincoln M, Johnson K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25:392–9. doi: 10.1016/j.arthro.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Hartmann A, Gunther KP. Arthroscopically assisted anterior decompression for femoroacetabular impingement: technique and early clinical results. Arch Orthop Trauma Surg. 2009;129:1001–9. doi: 10.1007/s00402-008-0806-4. [DOI] [PubMed] [Google Scholar]
- 46.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 47.Byrd JWT, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop. 2009;467:739–46. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–6. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Ilizaturri VM, Jr, Orozco-Rodrigues L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of CAM-type femoroacetabular impingement: preliminary report at 2 years minimum follow up. J Arthroplasty. 2008;23:226–34. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 50.Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90:1570–5. doi: 10.1302/0301-620X.90B12.21012. [DOI] [PubMed] [Google Scholar]
- 51.Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Tech Orthop. 2005;20:56–62. [PubMed] [Google Scholar]
- 52.Stahelin L, Stahelin T, Jolles BM, Herzog RF. Arthroscopic offset restoration in femoroacetabular cam impingement: accuracy and early clinical outcome. Arthroscopy. 2008;24:51–7. doi: 10.1016/j.arthro.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 53.Ilizaliturri VM, Jr, Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89:1025–30. doi: 10.1302/0301-620X.89B8.19152. [DOI] [PubMed] [Google Scholar]
- 54.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–76. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]


