Abstract
INTRODUCTION
Usually, cervical pedicle screw fixation has been considered too risky for neurovascular structures. The purpose of this study was to investigate the method and efficacy of the cervical pedicle screw system for fracture-dislocation of the cervical spine because of its rigid fixation.
PATIENTS AND METHODS
A prospective study was conducted involving 48 patients with cervical spine fracture-dislocation who underwent cervical pedicle screw fixation surgery between January 2003 and January 2007. All patients had various degrees of cord injury, and they were classified according to the American Spinal Cord Injury Association (ASIA) Impairment Scale: 18 cases were grade A, 15 grade B, 10 grade C, and 5 grade D.
RESULTS
Six months after the operation, all patients had achieved solid bony fusion and stable fixation of the related segments. Thirty patients with incomplete spinal cord injury improved their ASIA Impairment Scale classification by 1 to 2 grades after the operation. Eighteen patients with complete spinal cord injury had no improvement in neural function. However, nerve root symptoms such as pain and numbness were alleviated to some extent.
CONCLUSIONS
The cervical pedicle screw system is an effective and reliable method for the restoration of cervical stability. Sufficient pre-operative imaging studies of the pedicles and strict screw insertion technique should be emphasised.
Keywords: Lower cervical spine, Fracture-dislocation, Cervical pedicle screw
Injury of lower cervical spine is one of the most common and potentially most devastating injuries involving the axial skeleton. An effective cervical internal fixation system for lower cervical fracture-dislocation should provide immediate stabilisation to limit spinal cord injury, protect spinal cord function, relieve nerve root symptoms, enhance bony fusion, correct the spine deformity and reduce the application of external fixation.1 Some posterior instrumentation, such as spinous process wiring, sublaminar wires and lamina hooks, could not give adequate stability to the cervical spine;2–4 they can be applied only when the lamina is intact. If laminar fracture exists or laminectomy is needed for decompression, extended fixation and bone grafting over the decompressed segment are required. The lateral mass screw system was thought to be the reliable instrumentation.5–8 However, because it involves pure posterior column fixation, the pull-out strength is limited. Some patients also need strong external immobilisation, such as a halo vest, to secure the bony fusion Moreover, it cannot be used in the presence of osteoporosis or lateral mass destruction caused by the fracture or disease.
Abumi et al.9 first reported the results of pedicle screw fixation for traumatic lesion of cervical spine in 1994. Cervical pedicle screw fixation is a three-column fixation system with many biomechanical advantages. Results of biomechanics research indicate that the stability of cervical pedicle screw fixation is significantly higher than that of cervical lateral mass screw fixation and even higher than combined anterior and posterior fixation. Johnston et al.10 investigated the pull-out strengths after cyclic uniplanar loading of cervical pedicle screws and lateral mass screws. Cervical pedicle screws demonstrated a significantly lower rate of loosening at the bone-screw interface, as well as higher strength after fatigue testing.10 Rhee et al.11 compared five different posterior fixation constructs in a cadaveric model. The results showed the pedicle screw fixation provided the construct with the highest normalised stiffness for stabilising the cervical spine.11 We conducted a prospective study involving 48 patients with lower cervical spine fracture-dislocation who underwent cervical pedicle screw fixation surgery between January 2003 and January 2007 in our hospital to investigate its clinical effectiveness.
Patients and Methods
From January 2003 to January 2007, 48 patients (32 males and 16 females) with a mean age of 46.2 years (range, 23-65 years), were included in the present study. Twenty-five cases of lower cervical fracture-dislocation were caused by traffic accidents, eight cases by heavy object crashes, 11 cases by falling from high places, and four cases by accidental falls. Three injuries were located at C4, four at C4-5, 17 at C5, 9 at C5-6 and 15 at C6. Eight cases were vertical compression injuries, 22 flexion-compression injuries, and 18 flexion-rotation injuries. Eight cases had unilateral facet joint fracture-dislocation, 16 cases bilateral facet joint fracture-dislocation, 17 cases bilateral facet joint fracture-dislocation with vertebral body compression fracture, and seven cases burst fracture of cervical spine with dislocation. All patients had various degrees of cord injury, and they were classified according to the American Spinal Cord Injury Association (ASIA) Impairment Scale 12: 18 cases were grade A, 15 grade B, 10 grade C, and 5 grade D.
Surgical procedure
After general anaesthesia, the patient was placed in the prone position with the cervical spine maintained in the neutral position by continuous skull traction. A posterior midline incision was made, the paraspinous muscles were dissected, the lateral mass and its lateral margin were exposed sufficiently, and decompression and reduction were carried out according to various fracture-dislocation types. After the screw insertion site was localised on the posterior surface of the articular process, the cortical bone in the insertion point was removed with a high-speed burr, and the screw trajectory was identified. According to the pre-operative imaging and intra-operative C-arm X-ray imaging, a Kirschner wire was inserted into the pedicle. If laminectomy was needed, the medial wall of the pedicle was identified with a nerve dissector, the Kirschner wire was inserted under direct visualisation, and a probe was used to determine whether all four pedicle walls were composed of cortical bone. Then, pedicle screws of appropriate diameters were inserted along the trajectory of the channel. Suitable rods were selected, bent, and placed, and caps were screwed tightly. If the lamina was preserved, lamina bone grafting was carried out; if the lamina was resected, the cartilage surface of the facet joint to be fixed was removed with a rongeur and cancellous bone fragments were implanted. The internal fixation system used in the current study was the VERTEX fixation system (Medtronic Sofamor Danek, Inc., Minneapolis, MN, USA).
Postoperative management
After the operation, the skull traction was removed and a neck collar was placed. Sitting and walking were allowed on the first day after the operation in patients with incomplete spinal cord injury, and the neck collar was worn for 6–8 weeks.
Outcome evaluations
X-ray, computed tomography (CT) with a bone window, and magnetic resonance imaging (MRI) were performed before surgery in all patients. These radiological evaluations (X ray, CT and MRI) were also performed 3, 6, 12, and 24 months after surgery to assess stability, deformity, and fusion. The ASIA Impairment Scales were also assessed in each follow-up.
Results
No vertebral artery injury, spinal cord injury, or nerve root injury occurred during the operation in the current study. On the CT scan, no screw was found to penetrate the pedicle. The radiographic results of the imaging studies also showed that all 48 patients had achieved solid bony fusion 6 months after the operation (Figs 1–3). At the final fellow-up, no breakage or loosening of screw and rod happened. Thirty patients with incomplete spinal cord injury improved their ASIA Impairment Scale classification by 1 to 2 grades after the operation. Eighteen patients with complete spinal cord injury had no improvement in their neural function; however, their nerve root symptoms such as pain and numbness were relieved to some extent. The status of neural recovery is shown in Table 1.
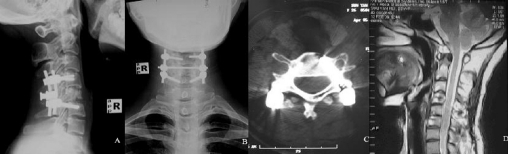
Figure 1.
A 27-year-old woman with C5 fracture-dislocation by traffic accident. (A) Plain lateral radiograph cervical spine. (B) Axial CT scan cervical spine. (C) A sagittal MRI scan showing spinal cord impingement. The MRI signal had changed.
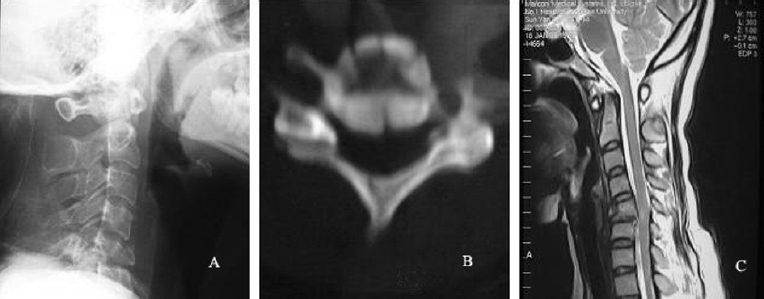
Figure 3.
Twelve months after initial surgery. (A) Plain lateral radiographs, (B) axial CT scan and (C) a sagittal MRI scan demonstrating restoration of favourable spinal alignment and solid bony union. The screws on both sides were in place.
Table 1.
Neurological outcomes measured with the American Spinal Cord Injury Association (ASIA) Impairment Scale
| Pre-operation | n | Final follow-up | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| A | 18 | 18 | 0 | 0 | 0 | 0 |
| B | 15 | 0 | 2 | 0 | 5 | 8 |
| C | 10 | 0 | 0 | 0 | 3 | 7 |
| D | 5 | 0 | 0 | 0 | 1 | 4 |
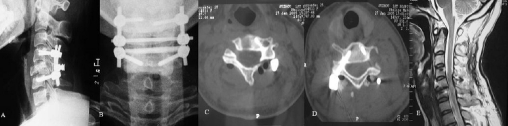
Figure 2.
(A) Lateral and (B) anteroposterior radiographs were obtained after cervical pedicle screw fixation. (C,D) CT scans showing the screws in place. (E) A sagittal MRI scan showing satisfactory reduction and redecompression of the spinal cord.
Discussion
At present, the method of cervical pedicle screw insertion is controversial. The main question is whether the pedicle screw should be inserted manually or using a computer-assisted navigation system. Ludwig et al.13 compared the accuracy of screw insertion using the latest computer-assisted navigation system versus the Abumi method. Fifty screws were inserted into five cadaver specimens using the computer-assisted navigation system, and 67 screws were inserted into seven cadaver specimens using the Abumi technique. The results showed that the rates of pedicle per-foration of the two methods were 18% and 12%, respectively, with no statistically significant difference observed. Furthermore, it was found that the perforation rate was relatively high in cases with pedicle diameters of less than 4.5 mm. The results showed that the computer-assisted navigation system cannot improve the accuracy and safety of screw insertion compared with the conventional technique.13 Richter et al.14 reported that a computer-assisted navigation system could reduce the screw misplacement rate compared with the conventional method. Mao et al.15 inserted a pedicle screw using a self-made, three-dimensional, localisation device, with the result showing improved accuracy. We believe that the screw insertion method should be selected depending on the clinical experience of the surgeon, the medical facilities available in the hospital, and the patient's financial concerns. Even if a computer-assisted navigation system is used, the considerable cervical motion that occurs when the probe explores the channel inside the pedicle decreases the accuracy of screw insertion. Furthermore, clinical application of the navigation system is not easy because of its complicated procedure, extended operation time, likely operation mistakes and incorrect information feedback. Therefore, the surgeon should have experience with the conventional screw fixation method.
Despite the availability of detailed descriptions of the insertion point, trajectory, and length of the cervical pedicle screw, no quantitative standard exists for the insertion point because of differences in the anatomical structure of the pedicle and its peripheral structures related to differences in individual patient characteristics, sex, and disease. Therefore, the selection of the screw insertion point and trajectory must be tailored to individual circumstances. Our experience indicates that a detailed pre-operative imaging study of the patient should be carried out, including antero-posterior, lateral, and both oblique views of the cervical spine by plain radiography and CT scanning. The cervical lateral mass should be exposed adequately during the operation, and the screw insertion point should be selected properly. Generally, the screw insertion point is located at the midpoint of the right upper quadrant of the lateral mass in C3-6, and at the midline of the lateral mass near the inferior margin of the upper facet process in C7. In the sagittal plane, screws should be inserted at a 10° cephalad tilt in C3-4, at a 10° caudal tilt in C6-7, and vertically in C5. The cortical bone in the entrance point is removed with the electric drill, and the entrance of the pedicle is revealed after expanding the point. This step is important because it can further identify the entrance area in the pedicle. The Kirschner wire is then inserted slowly and carefully into the pedicle, with close attention paid to the amount of resistance felt. As the Kirschner wire is advanced along the medullary cavity of the pedicle, the resistance force should be modest and consistent; if the resistance force increases or no resistance is felt, the direction of the wire should be changed slightly to locate a site offering modest resistance. This individualised screw insertion was performed successfully during the operation for all 48 patients in the current study. No vertebral artery injury, spinal cord injury, or nerve root injury occurred during the operation, and no related complications happened after the operation.
The main serious complication of cervical pedicle screw fixation is injury to the spinal cord, nerve root, and vertebral artery caused by pedicle perforation at the time of insertion. A relatively high rate of perforation detected by imaging studies after cervical pedicle screw fixation is often reported, although the rate of related complications is very low. A study by Yoshimoto et al.16 in which 134 pedicle screws were inserted showed that 15 screws (11.2%) perforated the pedicle, but no postoperative complications associated with the cervical pedicle screw were observed. Abumi and Shono17 conducted a study involving insertion of 712 screws, of which 669 screws could be evaluated by imaging studies. Of these 669 screws, 45 (6.7%) were found to perforate the pedicle, but neurovascular injury occurred in only three cases.17 In our experience, if the primary direction of drilling deviated slightly toward one side of the pedicle, even if all four walls of the channel were detected as strong bony walls by the thin Kirschner wire or pedicle probe, 3.5-mm or 4.0-mm screws could produce a ‘squeeze effect’ inside the channel that could result in cortical bone breakage on one side. This occurred most readily in the thin lateral wall of the pedicle. We believe that this may explain the high perforation rate found on postoperative imaging. The rate of related neurovascular complications is still very low, however. Therefore, with sufficient pre-operative preparation and individualised screw insertion, cervical pedicle screw fixation is still a relatively safe and useful clinical technique.
Acknowledgments
Feng Zhou and Jun Zou contributed equally to this work.
References
- 1.Vaccaro AR, Cook CM, Mccullen G, Garfin SR. Cervical trauma: rationale for selecting the appropriate fusion technique. Orthop Clin North Am. 1998;29:745–54. doi: 10.1016/s0030-5898(05)70045-6. [DOI] [PubMed] [Google Scholar]
- 2.Coe JD, Warden KE, Sutterlin CE, III, McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine. 1989;14:1122–31. doi: 10.1097/00007632-198910000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Gill K, Paschal S, Corin J, Ashman R, Bucholz RW. Posterior plating of the cervical spine: A biomechanical comparison of different posterior fusion techniques. Spine. 1988;13:813–6. doi: 10.1097/00007632-198807000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Sutterlin CE, III, McAfee PC, Warden KE, Rey RM, Jr, Farey ID. A biomechanical evaluation of cervical spinal stabilization methods in a bovine model: static and cyclical loading. Spine. 1988;13:795–802. doi: 10.1097/00007632-198807000-00015. [DOI] [PubMed] [Google Scholar]
- 5.An HS, Gordin R, Renner K. Anatomic considerations for platescrew fixation of the cervical spine. Spine. 1991;16(Suppl):S548–51. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 6.Graham AW, Swank ML, Kinard RE, Lowery GL, Dials BE. Posterior cervical arthrodesis and stabilization with a lateral mass plate: clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine. 1996;21:323–8. doi: 10.1097/00007632-199602010-00014. [DOI] [PubMed] [Google Scholar]
- 7.Heller JG, Silcox DH, III, Sutterlin CE., III Complications of posterior cervical plating. Spine. 1995;20:2442–8. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 8.Wellman BJ, Follett KA, Traynelis VC. Complications of posterior articular mass plate fixation of the subaxial cervical spine in 43 consecutive patients. Spine. 1998;23:193–200. doi: 10.1097/00007632-199801150-00009. [DOI] [PubMed] [Google Scholar]
- 9.Abumi K, Ito H, Taneichi H, Kaneda K. Transpedicular screw fixations for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–72. doi: 10.1016/j.spinee.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 11.Rhee JM, Kraiwattanapong C, Hutton WC. A comparison of pedicle and lateral mass screw construct stiffnesses at the cervicothoracic junction: a biomechanical study. Spine. 2005;30:E636–40. doi: 10.1097/01.brs.0000184750.80067.a1. [DOI] [PubMed] [Google Scholar]
- 12.Marino RJ. International Standards for Neurological Classification of Spinal Cord Injury. 5th edn. Chicago, IL: American Spinal Injury Association; 2000. [DOI] [PubMed] [Google Scholar]
- 13.Ludwig SC, Kowalski JM, Edwards 2nd CC, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine. 2000;25:2675–81. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 14.Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine. 2005;30:2280–7. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 15.Mao GP, Zhao JN, Wang YR, Li JS, Chen YX, et al. Design of cervical pedicle locator and three-dimensional location of cervical pedicle. Spine. 2005;30:1045–50. doi: 10.1097/01.brs.0000161011.08086.5b. [DOI] [PubMed] [Google Scholar]
- 16.Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Spinal reconstruction using a cervical pedicle screw system. Clin Orthop. 2005;(431):111–9. doi: 10.1097/01.blo.0000150321.81088.ab. [DOI] [PubMed] [Google Scholar]
- 17.Abumi K, Shono Y. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–9. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]