Abstract
Background
Corneal ulcers often lead to scarring and astigmatism, and significant loss of vision is a common consequence.
Objective
To determine the rate of graft rejection, one of the most serious concerns with this procedure, and to evaluate the recovery of visual function in those patients for whom the operation was successful.
Methods
We describe a retrospective study of 33 corneal ulcer patients undergoing penetrating keratoplasty (PK) at the Tabriz Nikookari Eye Hospital.
Results
Mean age of the patients was 44 ± 14 years. Most common risk factors for active keratitis were trauma, dry eye, and malnutrition. Culture-positive results included bacterial keratitis (n = 15) and fungal keratitis (n = 5). Perforation was a significant risk factor for therapeutic failure (P < 0.05). Age or gender had no statistically significant effects on the PK outcome (P > 0.05). Postoperative visual acuity had a significant association with preoperative visual acuity (P < 0.01). Graft rejection rate (27.2%) was similar to that reported in the literature.
Conclusion
Although lamellar keratoplasty has recently been established, there are practical reasons for continuing the use of PK in centers such as ours, with due attention to the requirement for topical immunosuppression to diminish the rate of graft rejection and antimicrobial treatment to prevent postoperative infection.
Keywords: keratitis, ulcerative, graft rejection, perforation
Introduction
Corneal ulcers often lead to scarring and astigmatism, and significant loss of vision is a common consequence. In severe cases, perforation, scleral involvement, and endophthalmitis may occur. Corneal ulcer together with ocular trauma are the major causes of blindness in developing countries.1 Different types of ulcers result from different pathological processes and require different management approaches.2 Keratitis is usually caused by bacteria and fungi.3,4 Recently, fungal causation associated with soft contact lens use has become an increasing cause of concern.5 Chemical burns by strong acids or alkalis are relatively prevalent among young patients.6
If corneal perforation seems likely, urgent management is required, since corneal perforation has high morbidity,7 and keratoplasty is a common procedure.2 Amniotic membrane transplantation has proved successful as an adjunctive method for corneal re-epithelization,3,8 but has not replaced keratoplasty, partly because of availability of donor tissue. Penetrating keratoplasty (PK) is a well established technique; however, long-recognized complications such as postoperative infection, corneal and macular edema, astigmatism, retinal detachment, and high rates of immune reactions and graft failure remain significant concerns.9–15
In this paper we describe a retrospective study of patients with corneal ulcer with or without serious vision loss who had undergone PK at Tabriz Nikookari Eye Hospital. Our aim was to determine the rate of graft rejection, one of the most serious concerns with this procedure, and to evaluate the recovery of visual function in those patients for whom the operation was successful.
Methods
Thirty-three patients aged between 5 and 80 years who underwent PK because of corneal ulcer in Tabriz Nikookari Eye Hospital between 2000 and 2003 were retrospectively evaluated.16,17 The indications for PK were recurrent or unhealing corneal ulcer (n = 8, 24.2%) or perforation (n = 25, 75.7%). The age, gender, etiology of corneal ulcer, and associated diseases were recorded for each patient.18,19 Post-PK follow-up period ranged from 3 to 24 months (mean = 11.6 months). On presentation and at time of PK, corneal scrapings were cultured to identify the organisms. Therapeutic success was defined as complete eradication of infection after PK with appropriate adjunctive medical therapy. Therapeutic failure was defined as recurrent corneal infection that progressed to endophthalmitis or phthisis bulbi despite medical therapy requiring evisceration.
Patients diagnosed with bacterial keratitis received appropriate antibiotics in culture-positive cases. In culture-negative cases, two broad-spectrum topical antibiotics were prescribed; gentamicin (14 mg/mL) and cefazolin (50 mg/mL) alternately every 10 minutes for the first hour then hourly for the next 24–48 hours, then tapering gradually according to the treatment response. Oral or intravenous antibiotics such as ciprofloxacin and ceftazidime were prescribed when the infiltrate encroached the limbus or if perforation was present or deemed impending. Patients with fungal keratitis received hourly topical amphotericin B 0.1% and natamycin 5%. In addition, patients with suspected anterior chamber (AC) or scleral involvement received preoperative oral ketoconazole 400 mg daily for 1–4 weeks. For bacterial keratitis, topical steroids generally were commenced only 1–5 days after surgery. For fungal keratitis, topical steroids use was on average delayed by 1–3 weeks, whereas amphotericin B 0.1% and natamycin 5% were tapered over 8–12 weeks. Postoperative oral ketoconazole was prescribed in all patients with perforation, when infection had breached the AC through suture tracks or previous surgical wounds, and in patients with obvious limbal or scleral extension, particularly if culture results showed Candida or Aspergillus species.
Data were recorded as mean ± SD or frequency, as appropriate, and were compared using Student’s t-test or a chi-square test using SPSS for Windows (v 11.5; SPSS, Inc, Chicago, IL). A P value < 0.05 was considered statistically significant.
Results
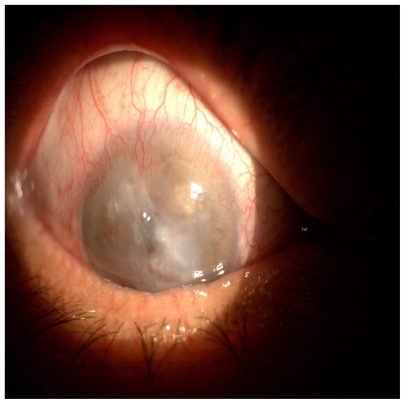
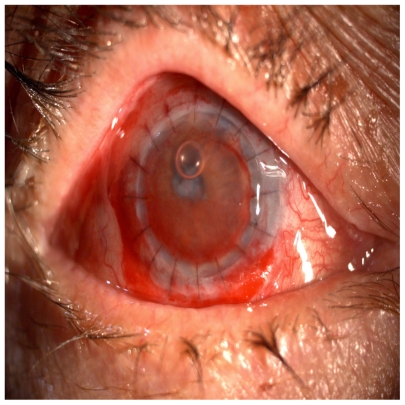
Thirty-three patients, 23 males and ten females, were enrolled in the present study. Mean age of patients was 44 ± 14 years (range: 5–80 years). The major risk factors for active keratitis were trauma (n = 5), dry eye (n = 4), malnutrition (n = 4), previous eye surgery (n = 3), and chemical burn (n = 3). Figures 1 and 2 show preoperative and postoperative images of the corneal ulcers, respectively. Postoperatively, visual acuity improved in 24 patients (72.7%) and high astigmatism occurred in 14 (35%), but there was no association with age or gender in either case (P > 0.1).
Figure 1.
Corneal ulcer before the penetrating keratoplasty.
Figure 2.
Outcome of the penetrating keratoplasty in a patient with corneal ulcer.
Culture-positive results included bacterial keratitis (n = 15) and fungal keratitis (n = 5). The most common isolated bacterium and fungus were Staphylococcus epidermidis (n = 10), and Fusarium species (n = 2). Thirteen patients had culture-negative results; the clinical appearance in eleven patients strongly resembled that of bacterial keratitis and they received treatment accordingly. Among these culture-negative patients, two therapeutic failures occurred.
Twenty-seven patients (81.8%) achieved therapeutic success. Therapeutic failure occurred in 4 eyes with limbal extension and two eyes with perforated ulcer. Three eyes had fungal keratitis. Infection recurrence time varied from 4 days to 1 year, most recurrences (n = 4) appearing within 6 weeks of surgery. Possible risk factors for failure were analyzed. Perforation was a significant risk factor (P < 0.05), but limbal extension was not shown to be a definite predictor for therapeutic failure (P > 0.05) in our cases.
General complications included endothelial rejection (n = 9), glaucoma (n = 7), and phthisis bulbi (n = 2). Glaucoma was controlled by medication. Rejection was reversed in six eyes, whereas three cases of rejection resulted in late graft failure. Graft rejection presented as photophobia, eye redness, visual blurring, and pain, in descending order of frequency. Age or gender had no statistically significant effects on PK outcome (P = 0.447 and 0.715, respectively). Five patients underwent simultaneous cataract surgery. Postoperative visual acuity had a significant association with preoperative visual acuity (P < 0.01).
Discussion
Our corneal ulcer patients covered a wide age and gender range. Therefore, our finding that age and gender had no significant influence on our outcome measures could be generally valid. For those patients in whom the graft was not rejected, visual function markedly improved, supporting the view that PK is a valuable procedure for patients with corneal ulcer in spite of the associated risks. The graft rejection rate (27.2% of the total cohort) is broadly consistent with values in the literature.20–22
The immune reaction associated with microbial keratitis and corneal transplant rejection has been studied in detail and was reviewed by Dana et al.23 Essentially, local Langerhans cells and other antigen-presenting cells are activated, pro-inflammatory cytokines such as interleukin-1 and tumor necrosis factor-α are upregulated, and a range of immune functions ensues, resulting in the recruitment of neutrophils and T helper type 1 lymphocytes and matrix metalloproteinase activation. The consequences can entail considerable corneal injury. Systemic immunosuppressants are not recommended for PK patients, but topical steroids supplemented with agents such as cyclosporine have been shown to be effective in reducing allograft rejection rates and should be considered.24–26
Recent advances in lamellar keratoplasty accompanied by antimicrobial treatment have also improved the success rate in terms of visual function and infection.27 It is less invasive than PK and vision is recovered more rapidly after the operation, and since long-term corneal sutures are not required, the problems associated with such sutures are eliminated. On the other hand, there is an absolute requirement for specially prepared donor tissue and surgeons with specific training or experience with the technique. In centers such as ours, these are currently not options. Therefore, with due attention to the need for topical immunosuppression and treatment to combat postoperative infection, there is a strong case for continuing the use of PK for corneal ulcer patients.
In summary, although the mainstay of initial management of severe infective keratitis remains aggressive antimicrobial therapy to limit spread to the sclera and AC, the role of timely surgical intervention in the form of therapeutic keratoplasty should be considered in view of the relatively successful outcomes in our series of patients with severe, end-stage disease. The timing of surgery is critical for good therapeutic outcomes, which we believe may be enhanced by earlier rather than later intervention, because scleral or intraocular extension of infection is likely to result in poorer outcomes.
Footnotes
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–221. [PMC free article] [PubMed] [Google Scholar]
- 2.Tuli SS, Schultz GS, Downer DM. Science and strategy for preventing and managing corneal ulceration. Ocul Surf. 2007;5:23–39. doi: 10.1016/s1542-0124(12)70050-2. [DOI] [PubMed] [Google Scholar]
- 3.Nubile M, Carpineto P, Lanzini M, Ciancaglini M, Zuppardi E, Mastropasqua L. Multilayer amniotic membrane transplantation for bacterial keratitis with corneal perforation after hyperopic photorefractive keratectomy: case report and literature review. J Cataract Refract Surg. 2007;33:1636–1640. doi: 10.1016/j.jcrs.2007.04.040. [DOI] [PubMed] [Google Scholar]
- 4.Bhartiya P, Daniell M, Constantinou M, Islam FM, Taylor HR. Fungal keratitis in Melbourne. Clin Experiment Ophthalmol. 2007;35:124–130. doi: 10.1111/j.1442-9071.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- 5.Belliappa S, Hade J, Kim S, Ayres BD, Chu DS. Surgical outcomes in cases of contact lens-related Fusarium keratitis. Eye Contact Lens. 2010;36:190–194. doi: 10.1097/icl.0b013e3181e3ef26. [DOI] [PubMed] [Google Scholar]
- 6.Merle H, Gérard M, Schrage N. Ocular burns. J Fr Ophtalmol. 2008;31:723–734. doi: 10.1016/s0181-5512(08)74391-2. French. [DOI] [PubMed] [Google Scholar]
- 7.Portnoy SL, Insler MS, Kaufman HE. Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989;34:47–58. doi: 10.1016/0039-6257(89)90129-x. [DOI] [PubMed] [Google Scholar]
- 8.Yildiz EH, Nurozler AB, Ozkan Aksoy N, Altiparmak UE, Onat M, Karaguzel H. Amniotic membrane transplantation: indications and results. Eur J Ophthalmol. 2008;18:685–690. doi: 10.1177/112067210801800504. [DOI] [PubMed] [Google Scholar]
- 9.Rao GN, Aquavella JV. Cephalosporium endophthalmitis following penetrating keratoplasty. Ophthalmic Surg. 1979;10:34–37. [PubMed] [Google Scholar]
- 10.Thiel HJ, Manthey KF. Incidence of immune reactions following penetrating keratoplasty (report on 100 consecutive interventions) Klin Monbl Augenheilkd. 1980;177:274–283. doi: 10.1055/s-2008-1057645. German. [DOI] [PubMed] [Google Scholar]
- 11.Kramer SG. Cystoid macular edema after aphakic penetrating keratoplasty. Ophthalmology. 1981;88:782–787. doi: 10.1016/s0161-6420(81)34952-5. [DOI] [PubMed] [Google Scholar]
- 12.Arentsen JJ, Laibson PR. Surgical management of pseudophakic corneal edema: complications and visual results following penetrating keratoplasty. Ophthalmic Surg. 1982;13:371–373. [PubMed] [Google Scholar]
- 13.Lavery GW, Lindstrom RL, Hofer LA, Doughman DJ. The surgical management of corneal astigmatism after penetrating keratoplasty. Ophthalmic Surg. 1985;16:165–169. [PubMed] [Google Scholar]
- 14.Musch DC, Meyer RF, Sugar A, Vine AK. Retinal detachment following penetrating keratoplasty. Arch Ophthalmol. 1986;104:1617–1620. doi: 10.1001/archopht.1986.01050230055030. [DOI] [PubMed] [Google Scholar]
- 15.Noorily SW, Foulks GN, McCuen BW. Results of penetrating keratoplasty associated with silicone oil retinal tamponade. Ophthalmology. 1991;98:1186–1189. doi: 10.1016/s0161-6420(91)32155-9. [DOI] [PubMed] [Google Scholar]
- 16.Sedghipour MR, Mousavi SH. Isolated microbes in patients admitted with corneal ulcer. Med J Tabriz Uni Med Sci. 2010;32:50–54. Persian. [Google Scholar]
- 17.Sedghipour MR, Shenasi A, Nourinia R. The results of corneal transplantation in perforated corneal ulcer. Iran J Ophthalmol. 2005;18:9–15. Persian. [Google Scholar]
- 18.Sedghipour MR, Mostafaei A, Taghari Y. Low-dose subconjunctional bevacizumab to augment trabeculectomy for glaucoma. Clin Ophthalmol. 2011;5:797–800. doi: 10.2147/OPTH.S17896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sedghipour MR, Sadigh AL, Motlagh BF. Revisiting corneal topography for the diagnosis of keratoconus: use of Rabinowitz’s KISA% index. Clin Ophthalmol. 2011 doi: 10.2147/OPTH.S24219. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sellami D, Abid S, Bouaouaja G, et al. Epidemiology and risk factors for corneal graft rejection. Transplant Proc. 2007;39:2609–2611. doi: 10.1016/j.transproceed.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Bosnar D, Dekaris I, Gabrić N, Markotić A, Lazić R, Spoljarić N. Influence of interleukin-1alpha and tumor necrosis factor-alpha production on corneal graft survival. Croat Med J. 2006;47:59–66. [PMC free article] [PubMed] [Google Scholar]
- 22.Trigui A, Smaoui M, Masmoudi J, Mhiri W, Maatoug S, Feki J. Corneal graft rejection: donor and receiver implication. J Fr Ophtalmol. 2005;28:631–634. doi: 10.1016/s0181-5512(05)81108-8. French. [DOI] [PubMed] [Google Scholar]
- 23.Dana MR, Qian Y, Hamrah P. Twenty-five-year panorama of corneal immunology: emerging concepts in the immunopathogenesis of microbial keratitis, peripheral ulcerative keratitis, and corneal transplant rejection. Cornea. 2000;19:625–643. doi: 10.1097/00003226-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Pleyer U. Immunomodulation in penetrating keratoplasty. Current status and perspectives. Ophthalmologe. 2003;100:1036–1044. doi: 10.1007/s00347-003-0954-4. German. [DOI] [PubMed] [Google Scholar]
- 25.Reis A, Birnbaum F, Reinhard T. Systemic immunosuppressives after penetrating keratoplasty. Ophthalmologe. 2007;104:373–380. doi: 10.1007/s00347-007-1517-x. German. [DOI] [PubMed] [Google Scholar]
- 26.Skeens HM, Holland EJ. Large-diameter penetrating keratoplasty: indications and outcomes. Cornea. 2010;29:296–301. doi: 10.1097/ICO.0b013e3181b6489e. [DOI] [PubMed] [Google Scholar]
- 27.Sharma N, Sachdev R, Jhanji V, Titiyal JS, Vajpayee RB. Therapeutic keratoplasty for microbial keratitis. Curr Opin Ophthalmol. 2010;21:293–300. doi: 10.1097/ICU.0b013e32833a8e23. [DOI] [PubMed] [Google Scholar]