Abstract
We herein report a rare case of squamous cell carcinoma of the hilar bile duct. A 66-year-old Japanese male patient was admitted to our hospital because of appetite loss and jaundice. Abdominal computed tomography revealed an enhanced mass measuring 10 × 30 mm in the hilar bile duct region. After undergoing biliary drainage, the patient underwent extended right hepatic lobectomy with regional lymph nodes dissection. The tumor had invaded the right portal vein. Therefore, we also performed resection and reconstruction of the portal vein. Histopathologically, the carcinoma cells exhibited a solid structure with differentiation to squamous cell carcinoma with keratinization and intercellular bridges. Immunohistochemical staining of the tumor cells revealed positive cytokeratin staining and negative CAM 5.2 staining. Based on these findings, a definitive diagnosis of well-differentiated squamous cell carcinoma of the hilar bile duct was made.
Key words: Squamous cell carcinoma, Extrahepatic bile duct, Extended right hepatic lobectomy
Introduction
Cases of biliary tract cancer are usually adenocarcinoma tumors. Although there have been many reported cases of adenosquamous carcinoma, there have been few reported cases of pure squamous cell carcinoma with no adenocarcinoma components, and the majority of these cases are already advanced at the time of diagnosis. According to Funakawa et al. [1], the incidence of squamous cell carcinoma arising in the extrahepatic bile duct is less than 1.4%. The first case of squamous cell carcinoma of the bile duct was reported by Cabot [2] in 1930. Since then, only 15 cases of squamous cell carcinoma originating in the extrahepatic bile duct have been reported, including the present case. We herein report a case of primary squamous cell carcinoma at the bifurcation level that may be only the 6th such case published in the literature, thus indicating that this condition is very rare. Due to the rare nature of the diagnosis, little information is available regarding the optimal management of these tumors. We describe this case while also reviewing the pertinent literature. Furthermore, we also discuss the potential mechanisms underlying squamous cell carcinoma of the biliary tree and the clinical characteristics and significance of chemotherapy or radiation therapy, and the prognosis.
Case Report
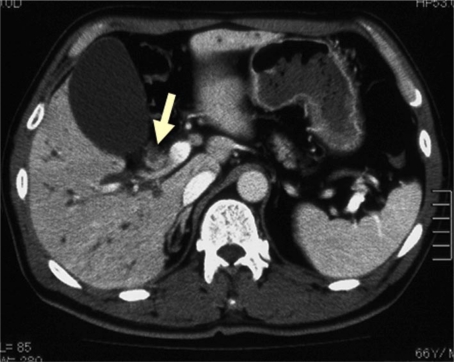
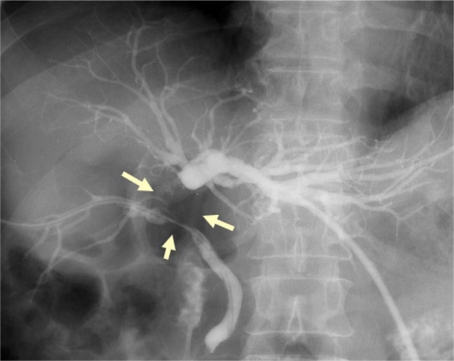
A 66-year-old Japanese male patient was admitted to our hospital because of appetite loss and jaundice. Physical examination revealed mild icteric sclerae. The patient's medical history was unremarkable. Laboratory data showed abnormal values for total bilirubin at 11.0 mg/dl (normal range 0.3-1.2), alkaline phosphatase of 2,278 IU/l (normal range 115-359), serum glutamic oxaloacetic transaminase of 175 IU/l (normal range 13-33), serum glutamic pyruvic transaminase of 287 IU/l (normal range 6-30), and C-reactive protein of 9.61 mg/dl (normal range <0.2), while all other laboratory data examined were within the normal ranges. The levels of carbohydrate antigen 19-9 (CA19-9) were 2,610 ng/ml (normal range <37), SPan-1 was 584 ng/ml (normal range <30), and DUPAN-2 was 508 ng/ml (normal range <150), while carcinoembryonic antigen at 2.6 ng/ml (normal range <5) was within normal range. Abdominal computed tomography (CT) revealed an enhanced mass measuring 10 × 30 mm in the hilar bile duct portion of the extrahepatic bile duct (fig. 1). MRI cholangiopancreatography revealed a defect from the junction of the common bile duct and the cystic duct to the bilateral hepatic duct. The patient underwent percutaneous transhepatic biliary drainage in the left lateral superior segmental duct (B3) and the right anterior inferior segmental duct (B5) for alleviation of the jaundice and evaluation of the biliary system (fig. 2). A percutaneous transhepatic cholangiogram revealed an obstruction of the first-order branch of the left bile duct, the anterior segmental bile duct and the posterior segmental bile duct. A diagnosis of a malignant tumor in the hilar bile duct was made, and the patient underwent extended right hepatic lobectomy with regional lymph node dissection. At laparotomy, an elastic hard mass was found in the hilar bile duct. The tumor had invaded the right portal vein. Therefore, we performed resection and reconstruction of the portal vein in addition. A choledochojejunostomy of B2+B3, B4 was performed using the Roux-en-Y method.
Fig. 1.
Abdominal CT showed a mass measuring 10 × 30 mm in the hilar bile duct. This figure show a 10 × 10 mm tumor (arrow).
Fig. 2.
A percutaneous transhepatic cholangiogram revealed an obstruction of the first-order branch of the left bile duct, the anterior segmental bile duct and the posterior segmental bile duct.
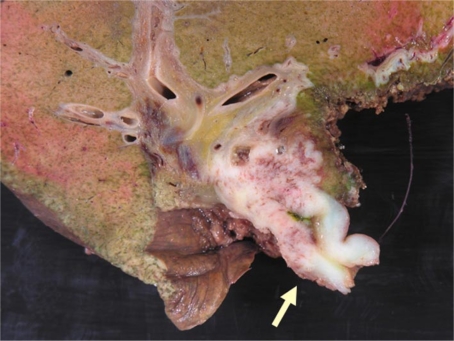
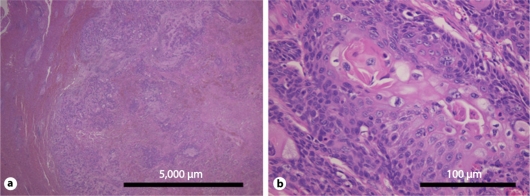
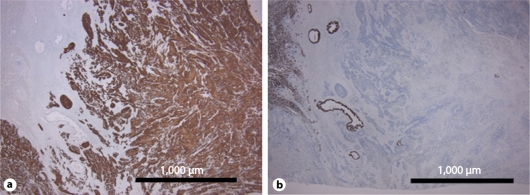
The resected specimen exhibited the nodular invasion type, measured 10 × 30 mm and had partly invaded to the portal vein and liver (fig. 3). Histopathologically, HE staining revealed that the tumor cells were arranged via keratinization and intercellular bridges (fig. 4). There was one lymph node metastasis at the cystic duct, and no carcinoma was present at the surgical margin of the left hepatic duct. Immunohistochemical staining of the tumor cells revealed positive cytokeratin staining and negative CAM 5.2 staining (fig. 5). Based on these findings, a definitive diagnosis of a well-differentiated squamous cell carcinoma of the hilar bile duct was made.
Fig. 3.
Macroscopically, the tumor was of the nodular invasion type, measured 10 × 30 mm and partly invaded the portal vein and the liver.
Fig. 4.
Histopathologically, HE staining showed the tumor cells arranged via keratinization and intercellular bridges.
Fig. 5.
Immunohistochemical staining of the tumor cells showed cytokeratin (positive) and CAM 5.2 (negative) reactions. a Cytokeratin, 40× magnification. b CAM 5.2, 40× magnification.
Six months after the operation, serum CA19-9 levels rapidly increased. Abdominal CT and 18F-fluorodeoxyglucose positron emission tomography were performed and revealed solitary liver metastasis. First-line chemotherapy with cisplatin (80 mg/m2 on day 1 every 4 weeks) and 5-fluorouracil (800 mg/m2 on days 1-5 every 4 weeks) was stopped because severe side effects (nausea and high fever) occurred. Second-line chemotherapy with gemcitabine (600 mg/m2 on days 1, 8 and 15 every 4 weeks) and S-1 (80 mg/day for 14 days followed by 7 days of rest) was administered for 3 months. However, the metastatic tumor progressively increased. The patient succumbed to progressive hepatic metastasis 12 months after the operation.
Discussion
The majority of malignant tumors arising in the biliary tree are adenocarcinomas; squamous cell carcinomas are very rare. The potential mechanisms of squamous cell carcinoma of the biliary tree include transformation of the adenocarcinoma to squamous cell carcinoma, derivation from metaplastic squamous epithelium of the glandular tissue, derivation from ectopic squamous epithelium, and derivation from undifferentiated basal cells [1]. In a study on adenosquamous carcinoma, which occurs relatively frequently in cases of gallbladder cancer, Kohno et al. [3] observed images of tissue migration from adenocarcinoma to squamous cell carcinoma and found that the growth rate of squamous cell carcinoma exceeded that of adenocarcinoma, thus suggesting that adenocarcinoma can transform into squamous cell carcinoma. However, since Cabot [2] developed the theory of canceration from squamous metaplasia of the biliary mucosa caused by inflammatory irritation, derivation from metaplastic squamous epithelium of glandular tissue has been considered to be the primary mechanism, and this hypothesis has been primarily supported by cases of pure squamous cell carcinoma with no adenocarcinoma components. Sewkani et al. [4] have listed ascariasis, choledochal cyst, Caroli disease, and primary sclerosing cholangitis as causative diseases. According to Hayafuchi and Kato [5], there is an undifferentiated basal cell layer in cases of cholecystitis complicated by gallstones, and the authors hypothesize that this layer contributes to squamous cell carcinoma of the gallbladder. In the present case, the immunostaining analyses revealed that the entire tumor was positive for cytokeratin and negative for CAM 5.2, and squamous cell carcinoma was observed in all cells of the cancerous region. Furthermore, because no images of metaplastic changes to squamous epithelium or migration from adenocarcinoma to squamous cell carcinoma were observed, it was difficult to explain the present mechanism.
There have been few reported cases of extrahepatic bile duct cancer patients who presented with histological findings of squamous epithelium, and since Cabot [2] reported the first case in 1930, there have been 15 cases, including the present patient, indicating the rarity of this condition (table 1). The ages of the patients ranged from 24 to 86 years (mean 62.9), and 10 male and 5 female subjects were reported. The site of occurrence was the hilar region in 6 cases, the proximal region in 2 cases, the distal region in 6 cases, and an unknown region in 1 case, and many of these tumors were observed in the hilar bile duct and the distal bile duct. The methods of diagnosis included postoperative histopathological diagnosis in 9 cases, biopsy in 3 cases [4, 8, 15], and autopsy in 3 cases. Consequently, the possibility that the 3 biopsied cases were also adenosquamous carcinoma cannot be ruled out. Surgical treatment was performed in 9 cases and included 6 cases of pancreaticoduodenectomy, 2 cases of extended left hepatic lobectomy, and 1 case of extended right hepatic lobectomy, while other treatments included palliative therapy such as bypass surgery, biliary stenting and chemoradiation therapy. The mean patient survival period was 11.1 months (range 3-27).
Table 1.
15 cases of squamous cell carcinoma of the extrahepatic bile duct
| First author | Year | Age | Sex | Position | Operation | Chemotherapy | Radiation | Prognosis |
|---|---|---|---|---|---|---|---|---|
| Cabot [2] | 1930 | 58 | M | proximal | unknown | X | X | unknown |
| Burger [6] | 1978 | 24 | F | distal | pancreaticoduodenectomy | O | X | 8 m, dead |
| Gulsrud [7] | 1979 | 68 | M | unknown | cholecystectomy with T tube | X | X | 6 m, dead |
| Aranha [8] | 1980 | 58 | F | hilar | T tube, cholecystectomy | X | O | 3 m, dead |
| Clements [9] | 1990 | 73 | M | hilar | biliary stent | X | X | unknown |
| Hirayasuyama [10] | 1990 | 68 | M | distal | pancreaticoduodenectomy | O | X | 3 m, alive |
| Sakata[ll] | 1991 | 68 | M | distal | pancreaticoduodenectomy | X | X | 2 y 3 m, alive |
| Shibata [12] | 1994 | 50 | M | hilar | extended left hepatic lobectomy | X | X | 10 m, alive |
| Nakazaki [13] | 1996 | 75 | M | distal | pancreaticoduodenectomy | X | X | 6 m, alive |
| Cho [14] | 2000 | 63 | M | distal | pancreaticoduodenectomy | X | X | unknown |
| Gatof[15] | 2004 | 86 | F | proximal | cholecystectomy, biliary stent | X | O | 18 m, dead |
| Sewkani [4] | 2005 | 60 | M | distal | pancreaticoduodenectomy | X | X | unknown |
| Abbas [16] | 2008 | 86 | F | hilar | extended left hepatic lobectomy | X | O | 18 m, alive |
| Price [17] | 2008 | 41 | F | hilar | biliary stent | o | O | unknown |
| Our case | 2010 | 66 | M | hilar | extended right hepatic lobectomy | O | X | 12 m, dead |
Squamous cell carcinoma of the biliary tree is characterized by the fact that the cell properties and prognosis differ depending on the site of occurrence of the tumor. Compared to cases of adenocarcinoma, cases of squamous cell carcinoma of the gallbladder tend to be locally limited, despite a large tumor diameter, and are more susceptible to tumor mass formation and invasion into neighboring organs with a low rate of hematogenous or lymphatic metastasis [18]. Therefore, a good prognosis can be expected by performing complete resection with lymph node dissection. At the same time, regarding intrahepatic cholangiocarcinoma, Nakajima and Kondo [19] compared 11 cases of intrahepatic cholangiocarcinoma involving squamous and adenosquamous carcinoma and 82 cases of adenocarcinoma, and concluded that the former cases tend to be discovered as advanced cancer with a large tumor diameter, present with widespread metastasis and have a poor prognosis. At the same time, regarding squamous cell carcinoma of the extrahepatic bile duct, it is difficult to systematically assess the characteristics because there are so few cases of these tumors. Based on these previous cases, there are many advanced tumors, including hepatic metastasis, vascular invasion, lymph node metastasis, and local invasion into the surrounding organs, and it was assumed that the patient prognosis is poor. Aranha et al. [8] have reported that development similar to adenocarcinoma is observed, invasion outside the bile duct and liver invasion occur progressively, and there is a tendency of metastasis to the local lymph nodes. Moreover, Okabayashi et al. [20] performed a comparative study of adenocarcinoma and adenosquamous carcinoma of the extrahepatic bile duct, thus concluding that adenocarcinoma progressed faster and had a higher malignancy compared to adenosquamous carcinoma. In the present case, the tumor diameter was 10 × 30 mm, there was marked local invasion including lymph node metastasis at the cystic duct, and vascular invasion into the main trunk of the right portal vein was observed. The histological findings included well-defined invasion into the liver parenchyma, and vascular invasion into the portal vein was observed. Therefore, the hepatic metastasis that occurred 6 months after the operation was suggestive of hematogenous metastasis caused by portal invasion.
There is no established chemotherapy or radiation therapy for squamous cell carcinoma of the biliary tree. Various treatments have been used in reported cases of squamous cell carcinoma of the gallbladder, including UFT+brisplatin, MF therapy, 5-fluorouracil arterial injection, and MFC therapy [21]. There have been only 2 reported cases of chemotherapy for squamous cell carcinoma of the extrahepatic bile duct, and there are also cases of concomitant and sequential administration of 4 agents comprising cyclophosphamide, doxorubicin, methotrexate [6], and procarbazine and cases of FP therapy [10]. Moreover, regarding radiation therapy, Abbas et al. [16] reported a case of squamous cell carcinoma of the hilar bile duct treated with intraoperative irradiation of the resection stump and external radiation for 6 weeks after operation, and the patient survived for 18 postoperative months. In the present patient, our policy was to conduct a postoperative follow-up examination, but because recurrence was observed 6 months after operation, the patient was treated with postoperative chemotherapy (first line: cisplatin and 5-fluorouracil, second line: S-1 and gemcitabine). From approximately 11 months after operation, marked general malaise and anorexia were observed, and approximately 12 months after operation, the patient succumbed to the disease. We therefore conclude that it is necessary to carefully investigate the indications of postoperative adjuvant chemotherapy and radiation therapy, and the details of chemotherapy when considering the properties of squamous cell carcinoma.
Conclusion
We reported in this paper a case of squamous cell carcinoma of the hilar bile duct and reviewed the previous reports. The majority of malignant tumors arising in the biliary tree are adenocarcinomas; squamous cell carcinomas are very rare. The majority of these cases are already advanced at the time of diagnosis. Based on these previous cases, there are many advanced tumors, including hepatic metastasis, vascular invasion, lymph node metastasis, and local invasion into the surrounding organs, and it is assumed that the prognosis is poor.
References
- 1.Funakawa T, Fujishiro N, Kuno N. Squamous cell carcinoma of the extrahepatic bile duct (in Japanese) Ryoikibetsu Shokogun Shirizu. 1996;9:61–63. [PubMed] [Google Scholar]
- 2.Cabot RC. Case records of the Massachusetts General Hospital: Case 16261. N Eng J Med. 1930;202:1260–1262. [Google Scholar]
- 3.Kohno T, Hyuga T, Honda Y. A case of squamous cell carcinoma of the gallbladder (in Japanese with English abstract) Nippon Rinsho. 2001;62:3030–3034. [Google Scholar]
- 4.Sewkani A, Kapoor S, Sharma S. Squamous cell carcinoma of the distal common bile duct. JOP. 2005;6:162–165. [PubMed] [Google Scholar]
- 5.Hayafuchi N, Kato N. Squamous cell carcinoma and adenoacanthoma of biliary tracts (gall bladder and choledochus) Kyushu Kohnenbyo Nenpoh. 1975;3:11–16. [Google Scholar]
- 6.Burger RE, Meeker WR, Luckett PM. Squamous cell carcinoma of common bile duct. South Med J. 1978;71:216–219. doi: 10.1097/00007611-197802000-00036. [DOI] [PubMed] [Google Scholar]
- 7.Gulsrud PO, Feinberg M, Koretz RL. Rapid development of cirrhosis secondary to squamous cell carcinoma of the common bile duct. Dig Dis Sci. 1979;24:166–169. doi: 10.1007/BF01324747. [DOI] [PubMed] [Google Scholar]
- 8.Aranha GV, Reyes CV, Greenlee HB. Squamous cell carcinoma of the proximal bile duct – A case report. J Surg Oncol. 1980;15:29–35. doi: 10.1002/jso.2930150106. [DOI] [PubMed] [Google Scholar]
- 9.Clements D, Newman D, Etherington R. Squamous carcinoma in the liver. Gut. 1990;31:1333–1334. doi: 10.1136/gut.31.11.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirayasuyama H, Keida Y, Ohshiro N. A case of squamous cell carcinoma of the common bile duct (in Japanese) Okinawa Igaku Zasshi. 1990;27:70–73. [Google Scholar]
- 11.Sakata T, Takakura N, Ohkura M. A case report of squamous cell carcinoma of the distal extrahepatic bile duct (in Japanese with English abstract) Tandoh. 1991;5:188–192. [Google Scholar]
- 12.Shibata K, Takami M, Hujimoto T. A case of squamous cell carcinoma of the hepatic hilum with peculiar clinical course (in Japanese) Tan To Sui. 1994;15:929–934. [Google Scholar]
- 13.Nakazaki T, Tobinaga K, Taketomi K. A case of squamous cell carcinoma of the common bile duct (in Japanese with English abstract) Nippon Rinsho. 1996;57:2538–2541. [Google Scholar]
- 14.Cho T, Nakamura J, Tomita H. A case of squamous cell carcinoma of the distal extrahepatic bile duct (in Japanese with English abstract) Nippon Rinsho. 2000;61:1853–1856. [Google Scholar]
- 15.Gatof D, Chen YK, Shah RJ. Primary squamous cell carcinoma of the bile duct diagnosed by transpapillary cholangioscopy: case report and review. Gastrointest Endosc. 2004;60:300–304. doi: 10.1016/s0016-5107(04)01561-5. [DOI] [PubMed] [Google Scholar]
- 16.Abbas R, Willis J, Kinsella T. Primary squamous cell carcinoma of main hepatic bile duct. Can J Surg. 2008;51:85–86. [PMC free article] [PubMed] [Google Scholar]
- 17.Price L, Kozarek R, Agoff N. Squamous cell carcinoma arising within a choledochal cyst. Dig Dis Sci. 2008;53:2822–2825. doi: 10.1007/s10620-007-0182-x. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe M, Kurauchi N, Kamachi N. A case of squamous cell carcinoma of the gallbladder resected by hepatopancreaticoduodenectomy (in Japanese with English abstract) Nippon Rinsho. 2004;65:3010–3014. [Google Scholar]
- 19.Nakajima T, Kondo Y. A clinicopathologic study of intrahepatic cholangiocarcinoma containing a component of squamous cell carcinoma. Cancer. 1990;65:1401–1404. doi: 10.1002/1097-0142(19900315)65:6<1401::aid-cncr2820650626>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 20.Okabayashi T, Kobayashi M, Nishimori I. Adenosquamous cell carcinoma of the extrahepatic biliary tract: clinicopathological analysis of Japanese cases of this uncommon disease. J Gastroenterol. 2005;40:192–199. doi: 10.1007/s00535-004-1520-9. [DOI] [PubMed] [Google Scholar]
- 21.Horiguchi M, Iwabuchi M, Kawabata K. A resected case of squamous cell carcinoma of gallbladder diagnosed as bile duct carcinoma preoperatively and analysis of 28 resected cases from Japanese literatures since 1970 and questionnaire study (in Japanese with English abstract) Tandoh. 1999;13:21–31. [Google Scholar]