Abstract
Ribbing disease is a rare form of sclerosing dysplasia characterized by benign endosteal and periosteal bone growth confined to the diaphyses of the long bones, usually the tibiae and femora. It occurs after puberty and is more commonly seen in women. The most common presenting symptom is pain that is usually self-limited; however, progression is known. The etiology and optimal treatment for the disease are as yet undefined. We present here the case of a 31-year-old woman with clinical, radiological and bone scan manifestations of Ribbing disease corroborated by bone biopsy. Radiographs demonstrated cortical thickening of the diaphyses of both tibiae. 99mTc-methylene diphosphonate bone scan revealed intense irregular uptake in diaphyseal region of both tibiae. Magnetic resonance imaging showed cortical thickening with bone marrow edema in bilateral tibial diaphysis with minimal adjacent soft tissue edema. Bone biopsy revealed predominantly dense lamellar bone with irregular sized and spaced haversian systems. Serum and urine markers of bone metabolism were within normal limits. The patient was treated with analgesics, and had partial relief from pain. Medullary rimming is the next treatment option in case pain progresses. This report emphasizes the role of bone scan in the diagnosis of this rare condition.
Keywords: Bone scan, dysplasia, leg pain, ribbing disease
INTRODUCTION
Ribbing disease (multiple diaphyseal sclerosis) is a rare form of bone dysplasia characterized by formation of exuberant but benign endosteal and periosteal new bone formation. It is an uncommon cause of bilateral leg pain in young females. It is either unilateral or asymmetrical and asynchronously bilateral, and has been reported only in long bones especially diaphysis of tibia and femur in postpubertal young adults. Most patients with Ribbing disease present with pain. It is often initially diagnosed as low-grade osteomyelitis, but it may also be confused with other causes of increased bone density on radiological investigations (sclerosing dysplasia) like Camurati-Engelmann disease, Van Buchem disease, Erdheim-Chester disease, etc. 99mTc-methylene diphosphonate (MDP) bone scan has been described as a useful tool in diagnosing this entity and excluding other bone dysplasiae. We report here a case of Ribbing disease, the diagnosis of which became possible due to bone scan.
CASE REPORT
A 31-year-old female presented to an orthopedician with bilateral leg pain since 1 year. Pain started in the right leg 6 months before the left leg, and at the time of presentation she had persistent pain on both sides, more on the right. She had no other site of pain. There was no history of fever, trauma or undue stress on the bones. There was no history of autoimmune diseases in her family. On examination, the patient did not have signs suggestive of vascular or muscular etiology of leg pain. There was no bony tenderness. She underwent a radiograph of both legs which showed cortical thickening of the diaphyses of both tibiae [Figure 1]. Keeping the differentials of shin splints/stress fracture versus chronic osteomyelitis in mind, she was referred for a bone scan. A three-phase 99mTc-MDP bone scan [Figure 2] showed intense irregular uptake in the diaphyseal region of both tibiae in delayed static images. Increased tracer activity was also noted in blood pool images in both legs. There were no other sites of bone involvement. The bone scan raised suspicion of a bone dysplasia involving only the tibiae bilaterally. The patient further underwent magnetic resonance imaging (MRI) which revealed cortical thickening with bone marrow edema in bilateral tibial diaphysis along with minimal adjacent soft tissue edema [Figure 3]. The patient's hematological parameters were within normal limits. There was no leukocytosis. Serum and urine markers of bone metabolism were also nondiagnostic. The patient then underwent a tibial biopsy which revealed predominantly dense lamellar bone with irregular sized and spaced haversian systems [Figure 4]. The bony lamellae were thick, sclerotic with few osteocytes. Taking all the clinical, biochemical, imaging and biopsy features into account, a diagnosis of Ribbing disease was made. The patient was already on low-dose analgesics since 6 months. The dose of these was increased in view of incomplete relief from pain. She is currently under follow-up and may need medullary rimming in case of failure to respond to peak analgesic dose.
Figure 1.

Radiograph of bilateral legs anteroposterior view shows cortical thickening of the diaphyses of both tibiae, left more than right
Figure 2.
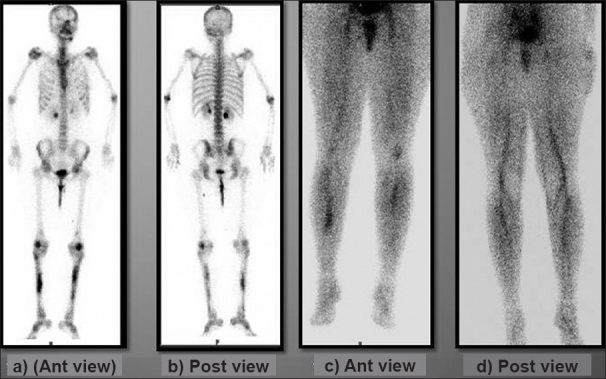
(a and b) Anterior and posterior delayed phase images of 99mTc-MDP bone scan showing irregular increased uptake in the diaphyseal region of both tibiae; rest of the skeleton shows physiologic uptake. (c and d) Anterior and posterior pool phase images of 99mTc-MDP bone scan show increased uptake in the bilateral mid-calf region of both legs
Figure 3.
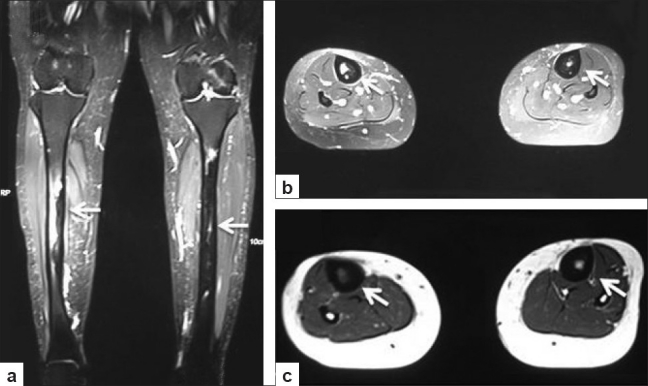
Short tau inversion recovery coronal (a) and axial (b) images show cortical thickening (arrows) with bone marrow edema in bilateral tibial diaphysis. Also noted is minimal adjacent soft tissue edema. T1W axial (c) image shows diffuse cortical thickening better
Figure 4.
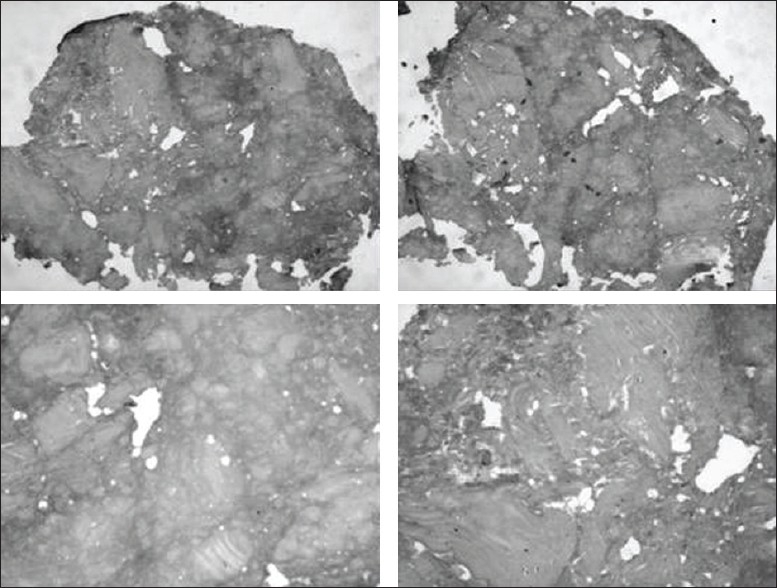
Photomicrographs of tibial biopsy specimen stained with H and E at low power (4×) show predominantly dense lamellar bone with irregular sized and spaced haversian systems. The bony lamellae are thick, sclerotic with few osteocytes. Photomicrographs at higher magnification (40×) demonstrate dense lamellar bone with fragments of normal cortical bone. The haversian canals are variable in caliber, irregular spaced and are increased in number
DISCUSSION
Ribbing described a family with six siblings for the first time in 1947 in which four of them had asymmetrical diaphyseal sclerosis of long bones. He designated the term hereditary multiple diaphyseal sclerosis. This was later found to be an uncommon cause of leg pain and in further case studies was called Ribbing disease.
It is important to differentiate this entity from the more common causes of bony leg pain like stress fractures, shin splints, osteomyelitis, fibrous dysplasia, osteoid osteoma, osteosarcoma, and other rarer causes like adamantinoma, melorheostosis, hyperphosphatasia, histiocytosis, lymphoma, intramedullary sclerosis, endosteal hyperostosis and sclerosteosis.
Bone dysplasiae like Engelmann disease are a close differential of Ribbing disease. The distinction between Ribbing disease and Camurati-Engelmann disease (progressive diaphyseal dysplasia) has been unclear. Engelmann disease has been more frequently reported in literature. It is a progressive disorder associated with pain, muscle weakness, fatigue, waddling gait, and anemia. Though Engelmann disease and Ribbing disease may appear to be identical radiographically, Seeger et al. pointed to certain clinical and histologic differences. Engelmann disease presents during childhood, while Ribbing disease usually presents after puberty. Engelmann disease presents with bilateral and symmetric bone involvement, whereas Ribbing disease is either unilateral or asymmetrically and asynchronously bilateral. Engelmann disease affects diaphyses of long bones and bones formed by intramembranous ossifications; hence, the skull is involved almost as frequently as the long bones. Ribbing disease has been reported only in the long bones.[1] While Engelmann disease features trabecular thickening, normal or enlarged haversian systems, and both osteoblastic and osteoclastic activity, implying bone formation and resorption, histologic study in Ribbing disease shows osteoblastic activity alone and progressive obstruction of the haversian systems.[2] It is thought that there may be a difference in the mode of inheritance. Engelmann disease is autosomal dominant, with considerable variation in penetrance. Autosomal recessive inheritance appears to be demonstrated in Ribbing disease. Makita et al. reported a three-generation Japanese family with Engelmann disease with a wide variation in phenotype among the affected family members. Of the 12 patients, 7 had full manifestations of Engelmann disease, while the other 5 exhibited only segmental (rhizomelic and/or mesomelic) involvement and asymmetric diaphyseal sclerosis without any clinical symptoms, resembling Ribbing disease. The authors proposed that Engelmann disease and Ribbing disease represent phenotypic variations of the same disorder.[3]
Ribbing's disease presents with pain, and recent studies have demonstrated that marrow edema is often associated with, and may be responsible for, at least in part, this pain.[4] The MRI appearance and the prominent finding of pain in Ribbing disease may be useful in helping to differentiate Ribbing disease from intramedullary osteosclerosis,[5] another diaphyseal dysplasia disease which bears perhaps the greatest clinical and radiographic similarity to Ribbing disease. It does not appear that the MRI finding of marrow edema is characteristic of intramedullary osteosclerosis.[6] This finding leads to what has been thought to be a potential treatment for Ribbing disease, the creation of a wide surgical “window” at the site of pain.[7] One may also consider the diagnosis of painful transient tibial edema,[8] which clinically resembles the presentation here. However, in that condition, the radiographs are usually normal.
In Ribbing disease, markers for bone formation like alkaline phosphatase and osteocalcin are not elevated. In addition, the markers of bone resorption like N-telopeptide, pyridinoline and deoxypyridinoline cross-links are also normal. Together, these measures of bone metabolism would suggest that Ribbing disease is not a “high turnover” bone state, a finding which may help to differentiate it from Camurati-Engelmann disease.[9] This seems to be inconsistent with the increased tracer uptake on 99mTc-MDP bone scan. In most bone diseases, where there is increased tracer uptake on bone scan, the markers of bone turnover are usually increased.[10] The lack of elevation in bone turnover markers may be explained by the limited amount of the skeleton involved as reflected by the focal nature of the uptake. That is, the area of involved bone may have been too small to affect the overall turnover markers. However, this is not necessarily inconsistent with the limited literature at the histological level that is available about Ribbing disease, which fails to identify a pattern suggestive of either a preponderance of osteoblastic or osteoclastic activity.[1]
The treatment of ribbing disease is mainly symptomatic and is done with nonsteroidal anti-inflammatory drugs in increasing dose as required. However, biphosphonates have been used in some cases of Ribbing and Camurati-Engelmann diseases, with discordant outcome; however, the low bone turnover that seems to characterize this disease and the prevalence of osteoblastic activity over the osteoclastic action are probably the reasons why osteoclast inhibitors may have limited success.[11] Medullary rimming is a treatment option where medical management fails.
Our case illustrates that a three-phase 99mTc-MDP bone scan has a very important role to play in the diagnosis of Ribbing disease. Firstly, it can rule out shin splints and stress fracture as the etiology of pain. Increased uptake restricted to the tibiae/femora can rule out other bone dysplasiae like Camurati-Engelmann disease, which have a more extensive involvement. Also, the nature and pattern of uptake can exclude primary neoplasms and metastases. A close differential on bone scan seems to be chronic osteomyelitis, especially since the onset of Ribbing disease may be unilateral and both diseases exhibit increased tracer activity on all three phases of the bone scan. Clinical history and examination may play a crucial role in such cases. Since the uptake of MDP is dependent on the osteoblastic response, it may be worthwhile trying to correlate the disease activity, patient symptomatology and tracer uptake.
We conclude that 99mTc-MDP bone scan is probably the most helpful investigation in cases of bony leg pain where dysplasiae like Ribbing disease are suspected.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Seeger LL, Hewel KC, Yao L, Gold RH, Mirra JM, Chandnani VP, et al. Ribbing disease (multiple diaphyseal sclerosis): Imaging and differential diagnosis. AJR Am J Roentgen. 1996;167:689–94. doi: 10.2214/ajr.167.3.8751682. [DOI] [PubMed] [Google Scholar]
- 2.Shier CK, Krasicky GA, Ellis BI, Kottamasu SR. Ribbing's disease: Radiographic-scintigraphic correlation and comparative analysis with Engelmann's disease. J Nucl Med. 1987;28:244–8. [PubMed] [Google Scholar]
- 3.Makita Y, Nishimura G, Ikegaw S, Ishii T, Ito Y, Okuno A. Intrafamilial phenotypic variability in Engelmann disease (ED): Are ED and Ribbing disease the same entity? Am J Med Genet. 2000;91:153–6. doi: 10.1002/(sici)1096-8628(20000313)91:2<153::aid-ajmg15>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 4.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–9. doi: 10.7326/0003-4819-134-7-200104030-00007. [DOI] [PubMed] [Google Scholar]
- 5.Chanchairujira K, Chung CB, Lai YM, Haghighi P, Resnick D. Intramedullary osteosclerosis: Imaging features in nine patients. Radiology. 2001;220:225–30. doi: 10.1148/radiology.220.1.r01jl24225. [DOI] [PubMed] [Google Scholar]
- 6.Bettini G, Bonvi V. Etiopathogenetic, clinical, and radiographic considerations on Ribbing's disease: Report of 2 cases of familial nature. Arch Putti. 1962;16:58–72. [PubMed] [Google Scholar]
- 7.Reinus WR, Fischer KC, Ritter JH. Painful transient tibial edema. Radiology. 1994;192:195–9. doi: 10.1148/radiology.192.1.8208937. [DOI] [PubMed] [Google Scholar]
- 8.Inaoka T, Shuke N, Sato J, Ishikawa Y, Takahashi K, Aburano T, et al. Scintigraphic evaluation of pamidronate and corticosteroid therapy in a patient with progressive diaphyseal dysplasia (Camurati-Engelmann disease) Clin Nucl Med. 2001;26:680–2. doi: 10.1097/00003072-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Mari C, Catafau A, Carrio I. Bone scintigraphy and metabolic disorders. Q J Nucl Med. 1999;43:259–67. [PubMed] [Google Scholar]
- 10.Chapurlat RD, Meunier PJ. Fibrous dysplasia of bone. Baillieres Best Pract Res Clin Rheumatol. 2000;14:385–98. doi: 10.1053/berh.1999.0071. [DOI] [PubMed] [Google Scholar]
- 11.Ziran N, Hill S, Wright ME, Kovacs J, Robey PG, Wientroub S. Ribbing disease: Radiographic and biochemical characterization, lack of response to pamidronate. Skeletal Radiol. 2002;31:714–9. doi: 10.1007/s00256-002-0552-6. [DOI] [PubMed] [Google Scholar]


