Abstract
Background:
The relationship between periodontal diseases in pregnancy and children born prematurely or with low birth weight has been increasingly investigated, showing positive and negative results, respectively. Objective: To evaluate the association between Maternal Periodontitis and Preterm delivery or Low Birth Weight.
Materials and Methods:
In this case-control study, 104 pregnant women without systemic disease or other risk factors for preterm labor were chosen. The control group (n = 52) had term labor (infants ≥37 weeks) and the case group (n = 52) had preterm labor (infants <37 weeks). Plaque index, bleeding index, and birth weight were measured.
Results:
The data of plaque index (cases 1.21±0.56; controls 0.63±0.31), bleeding index (cases, 2.08±0.62; controls, 1.52±0.61), birth weight (cases, 2.01±0.36; controls 2.87±0.32), and Probing Pocket Depth (PPD) ≥4mm and Clinical Attachment Level (CAL) ≥3mm in at least 4 teeth (odds ratio 137.50, P value < 0.0001) revealed a statistically significant difference between the two groups P< 0.05).
Conclusions:
A noticeable relationship between periodontal health and duration of pregnancy; periodontal disease could be a risk factor for preterm labor. Oral hygiene maintenance should be a part of prenatal care protocol.
Keywords: Low birth weight, periodontal disease, pregnancy, preterm labor, risk factors
Introduction
Periodontal research has emerged and evidences are published referring to the connection between periodontal infection and systemic diseases.[1]
Various factors have been found to associate with preterm and/or low birth weight infants. Maternal risk factors include age, height, weight, socio-economic status, ethnicity, smoking, alcohol, nutritional status, and stress.[2] In addition, parity, birth interval, previous complications, pre- and ante-natal care, maternal hypertension, infections, and cervical incompetence may also be important.[3] However, a significant proportion of low birth-weight is of unknown etiology. Among these birth weight is identified as one of the most important determinants to survive a newborn infant in all population groups.[4]
Even after taking increased care to avoid these known obstetric risk factors which were identified in approximately one fourth of preterm low birth cases, there still has been a relatively small decrease in the proportion of preterm low birth weight leading to a continued search for other causes and most of them are identified to be direct result of preterm labour or premature rupture of membranes, linking lower genital tract infection.[5,6]
Since the role of infection is receiving increasing attention, and the maternal infection on preterm delivery remained controversial, which may support an indirect effect as a consequence of the production of increased levels of inflammatory mediators shortening the gestational age. It is also plausible that micro-organisms may gain direct access to the amniotic fluid and fetus in several ways: Ascending via the vagina through the cervix into the choriodecidual sac during pregnancy or via the endometrium, which may be chronically infected prior to pregnancy, or alternatively through a hemotogenous route.[7]
An association has been established between severe periodontitis, and a variety of systemic conditions. Among these are cardiovascular disease, including endocarditis and coronary heart disease, insulin dependent diabetes mellitus, and respiratory disease.[8] The 1996 study by Offenbacher and colleagues suggested that maternal periodontal disease could lead to a seven-fold increased risk of delivery of a PLBW infant. Moreover, it has been observed in animal models that infection with Gram-negative periodontitis-associated micro-organisms may adversely affect pregnancy outcomes. As pointed out by Offenbacher et al,[9] these findings have been shown potential significance to risk assessment of PLBW, to oral health care during pregnancy. Since then numerous studies have been published establishing the link[10–15] and some studies failed[16–19] to establish association between maternal periodontitis and preterm low birth weight. Hence an attempt has been made to find the relationship between maternal periodontal disease and preterm low-birth weight infants in southern part of India.
Materials and Methods
A case-control study was conducted involving population attending the Govt. Maternity Hospital and Narayana Medical College Hospital, Nellore.
A sample of 134 systemically healthy women were examined and 104 were selected and divided into 52 cases and 52 controls depending on, mothers who had newborn's weight was less than 2500 g, Women who had spontaneous pre-term labour, women with threatening pre-term labour and were treated, to maintain pregnancy as long as possible or preterm premature rupture (less than 37 weeks of gestation) of membranes. Exclusion criteria include the women with systemic medical problems, chronic infectious diseases, those who are receiving antibiotics at the time of the examination, and those who had taken dental treatment within 6 months.
Study design
A detailed Ethical Committee Approval was taken prior to the commencement of the study. The nature of study was explained to subjects and consent was obtained for their participation prior to commencement of the study. Case defined as premature delivery (WHO 1950) occurring at less than 37 weeks of gestation, and is generally accompanied by low birth weight, i.e., a birth weight less than 2500 g. Control defined as mothers with delivery occurring after 37 weeks without any previous complications, and newborn with birth weight of ≥2500 g.
History of information about age, education status of parents, occupation, socio-economic status of the family, psychological stress levels of the pregnant women, number of previous pregnancies, previous preterm low birth weights, and miscarriages was noted. Recording of following clinical parameters were done using Sillness and Loe Plaque Index (PI), Muhlemann and Son Sulcus bleeding Index (SBI), Probing pocket depth (PPD), and Clinical attachment level (CAL). Reproducibility trials were performed on 20 subjects before starting the study. PPDs and CAL were measured to the nearest mm at 6 sites per tooth, i.e., around mesio-buccal, mid-buccal, disto-buccal, mesio-lingual, mid-lingual, and disto-lingual using William's periodontal probe*. The probing depth was used for categorizing a mother with chronic periodontitis. According to Gomes-Filho,[20] woman with probing depth ≥4 mm and CAL ≥3mm at the same site in at least four teeth is considered as chronic localized periodontitis. Weight of the newborn was analyzed using a manual machine (Docbel, Braun company Pvt. Ltd.) by the gynecologist. The patient's hospital record was verified to confirm the data obtained for any variation. All the periodontal examinations were completed within 3 days post-partum as defined by Offenbacher et al.[9]
*Hu-friedy
Results
A statistical analysis was performed using SPSS system, containing descriptive statistics and univariate / multivariate logistic regression analyses. Categorical variables were compared by the chi-square test or Fisher's exact test and continuous variables by the Student's t test. Univariate and multivariate logistic regression analyses were constructed for preterm low birth weight, starting with all variables included in the univariate analyses. Statistical significance was defined as P < 0.05.
When comparison of means and standard deviations of different-variables in cases and controls were done,bleeding index, plaque index and birth weight, education status of the mother are highly significant at 1% level where as age does not show any significance as shown in Table 1.
Table 1.
Comparision of different variables in case and control groups
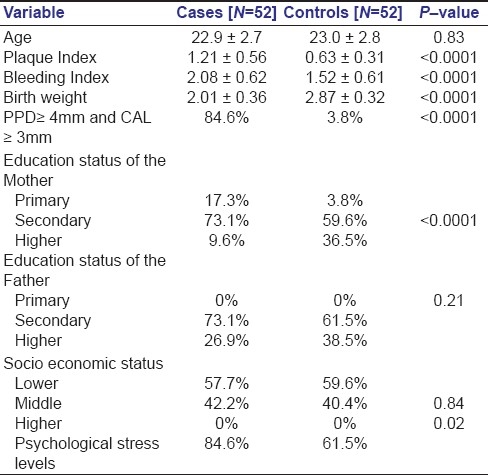
The Comparison of mean values of different subjective variables in both groups graphically represented in Figure 1.
Figure 1.
Comparison of mean values of different subjective variables in case and control groups.
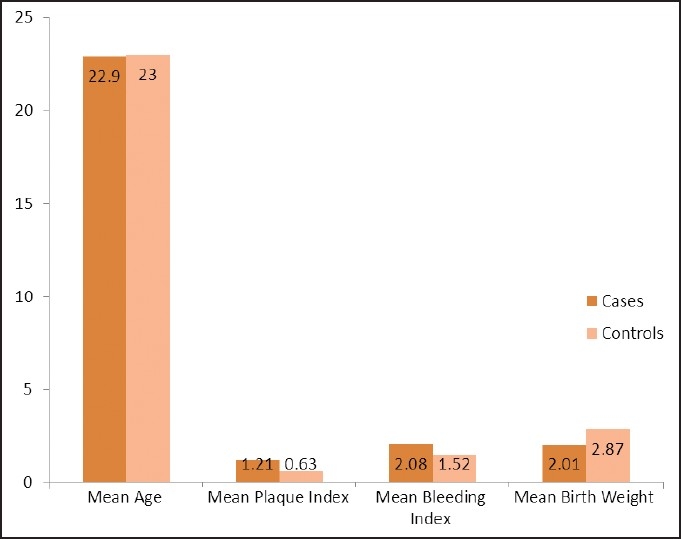
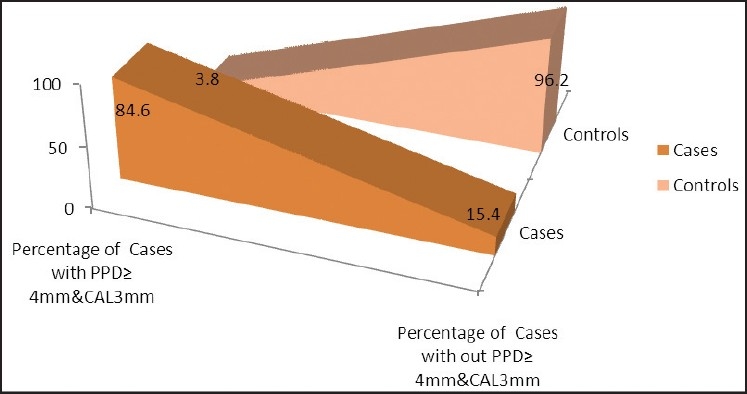
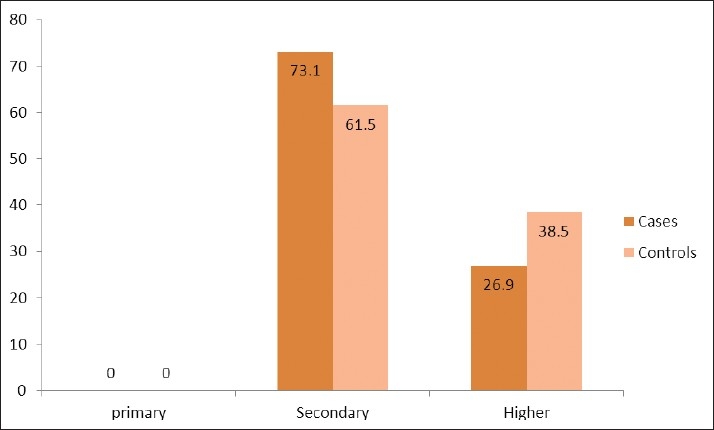
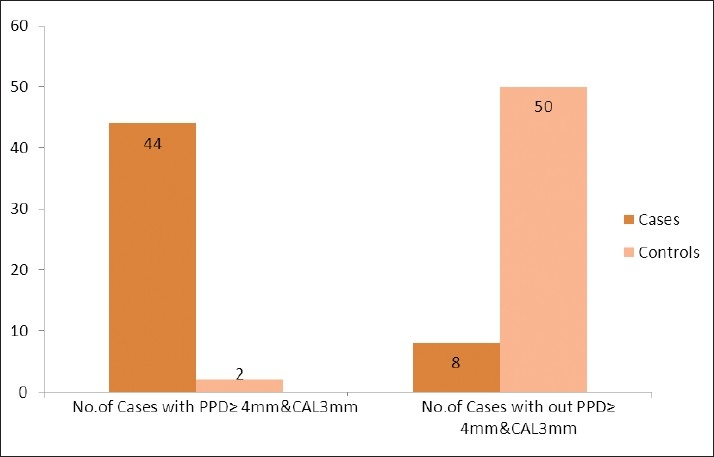
When the percentage-with and without (PPD) ≥ 4 mm and CAL ≥ 3 mm in at least 4 teeth was compared between cases (84.6 %) and control (3.8%) groups, there was high significance observed at 1% level as shown in Figure 2. When the education status of the mothers was compared at different levels between cases and controls, high significance was observed at 1% level. Whereas the education status of the fathers was compared, there was no significance observed as represented in Figure 3 and 4, respectively.
Figure 2.
Percentages of cases with and without PPD≥4mm and CAL≥3mm in at least 4 teeth.
Figure 3.
Comparison of the education status of the mother at different levels in case and control groups.
Figure 4.
Comparison of education status of the father at different levels in case and control groups.
When the socio-economic status of the families was compared at different levels between cases and controls, there was no observable significance and represented graphically in Figure 5. When the psychological stress level of the mothers was compared between cases (84.6%) and controls (38.5) high significance was observed at 1% level and graphically represented as shown in Figure 6.
Figure 5.
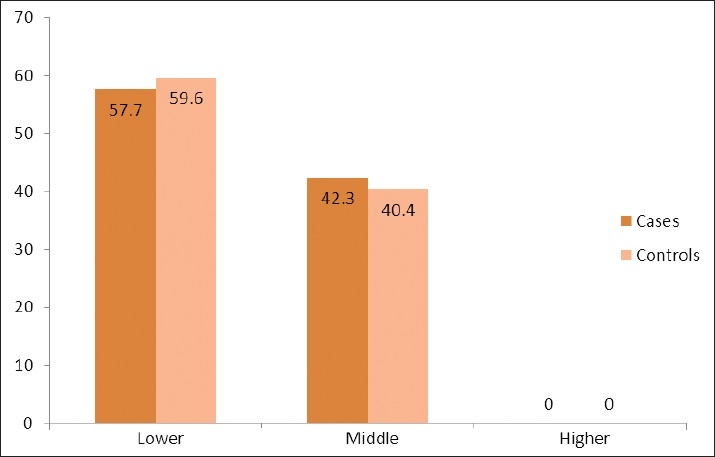
Comparison of socio-economic status of the family at different levels in case and control groups.
Figure 6.
Comparison of psychological stress levels in case and control groups.
Significant associations were found between PLBW and periodontal disease (P< 0.001) when Univariate logistic regression was done in pregnant women. Plaque index, bleeding index, psychological stress were the parameters significantly associated with PLBW in the univariate analysis. Other non significant variables include age of the mother, father education status, socio economic status of the family and no. of abortion as shown in the Table 2.
Table 2.
Univariate logistic regression analysis
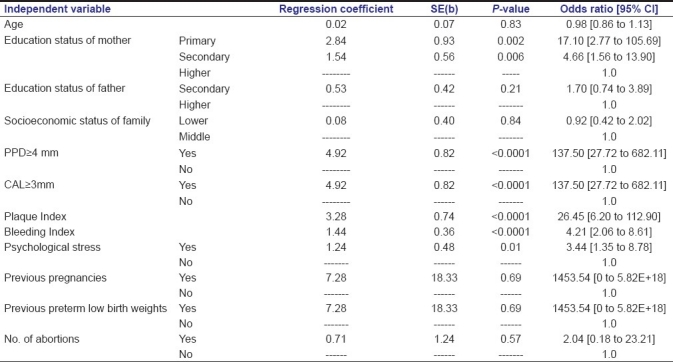
(PPD) ≥4 mm and CAL ≥3 in at least 4 teeth is the only variable which is significant at 1% level, when multiple logistic regression analysis was done, with a regression coefficient of 4.92 and odds ratio is 137.50 as shown in Table 3.
Table 3.
Multiple logistic regression analysis
![]()
Discussion
Most of the confounding variables were found to be well known risk factors associated with PLBW explaining PB and/or LBW showing highly significant relationship between periodontitis and PLBW. However age of the mother did not show much of significance, this could be attributed to antenatal factors such as socioeconomic factors, infections and other complications.
The Plaque index showed highly significant differences (P<0.001 with an odds ratio 26.45) in both cases and controls. It is in accordance with the study conducted by yalcin et al.[21] This could be because; during pregnancy the oral microflora uses the progesterone and estrogen hormones as vitamin k growth factors and they form the plaque on the gingival and tooth surfaces.[22] In contrary studies conducted by Radnai et al,[1] showed insignificant plaque index values (P=0.198) in cases and controls.
Significant differences were found in bleeding index (P <0.001 with an odds ratio 4.21) in both cases and controls. This is in agreement with Zadeh-Modarres et al,[23] indicating that the control group had a better periodontal condition than the case group. The increased circulating levels of progesterone in turn cause dilation of gingival capillaries, permeability, and gingival exudates that may explain the redness and increased bleeding tendency during pregnancy. And the physiological female sex hormones during pregnancy also influence the gingival tissues.[22]
Our results established strong evidence that maternal periodontal disease is an independent risk factor for an adverse outcome of pregnancy (Preterm Low Birth Weight) showing significant differences (P<0.0001) in both cases and controls. This is in agreement with several studies conducted in different population groups by Offenbacher et al,[9] Goepfort,[10] Marin et al,[11] Moliterno et al,[12] Siqueria et al,[13] Zadeh-Modarreas,[23] Agueda et al[14] and Pitiphat et al.[15] This could be due to one of the two mechanisms. First, women with periodontal disease may experience more frequent and severe bacteremia than periodontally healthy women. As a result, the uterine cavity may become exposed to or colonized by periodontal bacteria or their byproducts (e.g., lipopolysaccharides). Once they reach the maternal-fetal unit, oral bacteria may elicit an inflammatory cascade that leads to preterm labour. A second putative mechanism does not require oral bacteria to colonize the uterine cavity. Rather, cytokines generated within the diseased periodontal tissue may enter the systemic circulation and precipitate a similar cascade, again leading to spontaneous preterm labour and birth.[24]
In contrary, studies conducted by several authors[5,16–19] did not provide connecting link between maternal periodontitis and preterm delivery.
Highly significant (P<0.0001) association between probing pocket depth and preterm low birth weight was consistent when using at least one site with (PPD) ≥4 mm and CAL ≥3 mm in at least 4 teeth. In controls, only 3.8% women showed (PPD) ≥4 mm and CAL ≥3 mm when at least 4 teeth were considered indicating significant periodontal disease progression during pregnancy. This is in concurrence with studies conducted by Goepfort[14] and Agueda et al.[18] This is in perverse with studies conducted by Gursoy et al.[19]
A significant association between periodontal disease and adverse pregnancy outcome was observed in population groups with a incidence of preterm deliveries, from economically disadvantaged families shown by Lopez et al,[25] However, the present study, reports no relationship between socioeconomic status and adverse pregnancy outcomes. This is in accordance with, most studies conducted[5,16] in European countries and Canada.
In the present study, periodontal status of the mother was found to be influenced greatly by educational status (P <0.05) of the pregnant women. This is in agreement with Siqueria et al,[13] Toygar et al.[26] On the contrary, an insignificant difference (P>0.05) was found in some studies Davenport et al.[5] This could be because educated mothers would take more preventive measures than less or uneducated mothers.
On the other hand, periodontal status of the mother was not influenced by the father educational status (P>0.05). Similar results were obtained in a study conducted by Radnai et al.[1]
According to our study mother's psychological stress levels and preterm low birth weight deliveries had significant (P<0.05) association. This could be explained that the stressful events would stimulate pituitary – hypothalamus – adrenal axis and release cortisol hormone into circulation. The systemically released hormone enters into saliva and would cause reduction of inflammatory cells inhibiting the immune response thereby causing the inflammation of the periodontium.[27]
Association between number of abortions and preterm low birth weight deliveries were found insignificant (P>0.05). This is in accordance with Augeda et al.[14] On the other hand, Marin et al,[11] found significant results between number of abortions and preterm low birth weight. The presences of specific genetic and environmental factors influence the pregnant women to induce abortion.[5]
An insignificant (P>0.05) association was observed between previous preterm low birth weight and preterm low birth weight deliveries in our study. On contrary, Augeda et al,[14] Davenport et al,[5] found significant results between previous preterm low birth weights and preterm low birth weight. This could be because the majority of the deliveries in our study are first deliveries.
Association of number of previous deliveries and preterm low birth weight was insignificant (P>0.05) in our study. This is in accordance with study conducted by Davenport et al.[5] Since most of the pregnant women admitted for first delivery, they must have shown an insignificant association.
On the basis of these findings, periodontal infections in pregnant women can be viewed as a potential obstetric risk factor. The fact being periodontal infections are both preventable and readily treated, this study findings provide opportunities for intervention strategies to reduce the incidence of preterm low birth weight.
Conclusions
From the results obtained, the following conclusions were arrived at
-
1.
Periodontal disease in pregnant women is an important obstetric risk factor for preterm low birth weight.
-
2.
Chronic periodontitis is associated with preterm low birth weight in pregnant women among this part of India.
-
3.
Antenatal factors and periodontal status contribute for preterm low birth weight in pregnant women.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Radnai M, Gorzo I, Urban E, Eller J, Novak T, Pal A. Possible association between mother's periodontal status and preterm delivery. J Clin Periodontol. 2006;33:791–6. doi: 10.1111/j.1600-051X.2006.00986.x. [DOI] [PubMed] [Google Scholar]
- 2.Vererk PH, Noord-Zaadstra BM, Florey CD, de Jonge GA, Verloove-Vanhorick SP. The effect of moderate maternal alcohol consumption on birthweight and gestational age in a low risk population. Early Hum Dev. 1993;32:121–9. doi: 10.1016/0378-3782(93)90006-g. [DOI] [PubMed] [Google Scholar]
- 3.Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Martin DH, Cotch MF. Association between bacterial vaginosis and pre term low birth weight infant. N Engl J Med. 1995;333:1515–25. doi: 10.1056/NEJM199512283332604. [DOI] [PubMed] [Google Scholar]
- 4.Mealy BL. Influence of periodontal infections on systemic health. Periodontol 2000. 1999;21:197–209. doi: 10.1111/j.1600-0757.1999.tb00176.x. [DOI] [PubMed] [Google Scholar]
- 5.Davenport ES, Williams CE, Sterne JA, Murad S, Sivapathasundram V, Curtis MA. Maternal Periodontal Disease and Preterm Low Birth weight: Case-Control Study. J Dent Res. 2002;81:313–8. doi: 10.1177/154405910208100505. [DOI] [PubMed] [Google Scholar]
- 6.Williams CE, Davenport ES, Sterne JA, Sivapathasundaram V, Fearne JM, Curtis MA. Mechanisms of risk in preterm low-birth weight infants. Periodontol 2000. 2000;23:142–50. doi: 10.1034/j.1600-0757.2000.2230115.x. [DOI] [PubMed] [Google Scholar]
- 7.Romero R, Mazor M. Infection and preterm labour. Clin Obstet Gynaecol. 1988;31:553–84. doi: 10.1097/00003081-198809000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Seymour RA, Steele JG. Is there a risk between periodontal disease and coronary heart disease? Br Dent J. 1998;184:33–8. doi: 10.1038/sj.bdj.4809536. [DOI] [PubMed] [Google Scholar]
- 9.Offenbacher S, Katz V, Fertik G, Collins J, Boyd D, Maynor G, et al. Periodontal Infection as a Possible Risk Factor for Preterm Low Birth Weight. Ann Periodontol. 1996;3:1103–13. doi: 10.1902/jop.1996.67.10s.1103. [DOI] [PubMed] [Google Scholar]
- 10.Goepfert AR, Jeffcoat MK, Andrews WW, Faye-Petersen O, Cliver SP, Goldenberg RL, et al. Periodontal Disease and Upper Genital Tract Inflammation in Early Spontaneous Preterm Birth. Obstet Gynecol. 2004;104:777–83. doi: 10.1097/01.AOG.0000139836.47777.6d. [DOI] [PubMed] [Google Scholar]
- 11.Marin C, Segura-Egea JJ, Martinez-Sahuquillo A, Bullon P. Correlation between infant birth weight and mother's periodontal status. J Clin Periodontol. 2005;32:299–304. doi: 10.1111/j.1600-051X.2005.00661.x. [DOI] [PubMed] [Google Scholar]
- 12.Moliterno LF, Monteiro B, da silva Figueredo CM, Fischer RG. Association between periodontitis and low birth weight: A case – control study. J Clin Periodontol. 2005;32:886–90. doi: 10.1111/j.1600-051X.2005.00781.x. [DOI] [PubMed] [Google Scholar]
- 13.Siqueria FM, Cota LO, Costa JE, Haddad JP, Lana AM, Costa FO. Intrauterine Growth Restriction, Low Birth weight, and Preterm Birth: Adverse Pregnancy Outcomes and Their Association with Maternal Periodontitis. J Periodontol. 2007;78:2266–76. doi: 10.1902/jop.2007.070196. [DOI] [PubMed] [Google Scholar]
- 14.Agueda A, Ramon JM, Manau C, Guerrero A, Echeverria JJ. Periodontal disease as a risk factor for adverse pregnancy outcome: A prospective cohort study. J Clin Periodontol. 2008;35:16–22. doi: 10.1111/j.1600-051X.2007.01166.x. [DOI] [PubMed] [Google Scholar]
- 15.Pitiphat W, Joshipura KJ, Gillman MW, Williams PL, Douglass CW, Rich-Edwards JW. Maternal periodontitis and adverse pregnancy outcomes. Community Dent Oral Epidemiol. 2008;36:3–11. doi: 10.1111/j.1600-0528.2006.00363.x. [DOI] [PubMed] [Google Scholar]
- 16.Farrell MS, Ide M, Wilson RF. The relationship between maternal periodontitis, adverse pregnancy outcome and miscarriage in never smokers. J Clin Periodontol. 2006;33:115–20. doi: 10.1111/j.1600-051X.2005.00884.x. [DOI] [PubMed] [Google Scholar]
- 17.Skuldbol T, Johansen KH, Dahlen G, Stoltze K, Holmstrup P. Is pre-term labour associated with periodontitis in a Danish maternity ward? J Clin Periodontol. 2006;33:177–83. doi: 10.1111/j.1600-051X.2006.00899.x. [DOI] [PubMed] [Google Scholar]
- 18.Bassani DG, Olinto MT, Kreiger N. Periodontal disease and perinatal outcomes: A case-control study. J Clin Periodontol. 2007;34:31–9. doi: 10.1111/j.1600-051X.2006.01012.x. [DOI] [PubMed] [Google Scholar]
- 19.Gursoy M, Pajukanta R, Sorsa T, Kononen E. Clinical changes in periodontium during pregnancy and post- partum. J Clin Periodontol. 2008;35:576–83. doi: 10.1111/j.1600-051X.2008.01236.x. [DOI] [PubMed] [Google Scholar]
- 20.Gomes-Filho IS, Cruz SS, Rezende EJ, dos Santos CA, Soledade KR, Magalhaes MA, et al. Exposure measurement in the association between periodontal disease and prematurity/low birth weight. J Clin periodontol. 2007;34:957–63. doi: 10.1111/j.1600-051X.2007.01141.x. [DOI] [PubMed] [Google Scholar]
- 21.Yalcin F, Eskinazi E, Soydinc M, Basegmez C, Issever H, Isik G, et al. The effect of Sociocultural Status on Periodontal Conditions in Pregnancy. J Periodontol. 2002;73:178–82. doi: 10.1902/jop.2002.73.2.178. [DOI] [PubMed] [Google Scholar]
- 22.Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL., Jr Microbial complexes in subgingival plaque. J Clin periodontol. 1998;25:134–44. doi: 10.1111/j.1600-051x.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 23.Zadeh-Modarres S, Amooian B, Bayat-Movahed S, Mohamadi M. Periodontal Health In Mothers of Preterm and Term Infants. Taiwan J Obstet Gynecol. 2007;46:157–61. doi: 10.1016/S1028-4559(07)60010-2. [DOI] [PubMed] [Google Scholar]
- 24.Gibbs RS. The Relationship Between Infections and Adverse Pregnancy Outcomes: An Overview. Ann Periodontol. 2001;6:153–63. doi: 10.1902/annals.2001.6.1.153. [DOI] [PubMed] [Google Scholar]
- 25.Lopez NJ, Smith PC, Gutierrez J. Higher risk of preterm birth and low birth weight in women with periodontal disease. J Dent Res. 2002;81:58–63. doi: 10.1177/002203450208100113. [DOI] [PubMed] [Google Scholar]
- 26.Toygar HU, Seydaoglu G, Kurklu S, Guzeldemir E, Arpak N. Periodontal Health and Adverse Pregnancy Outcome in 3,576 Turkish Women. J Periodontol. 2007;78:2081–94. doi: 10.1902/jop.2007.070092. [DOI] [PubMed] [Google Scholar]
- 27.Genco RJ, Ho AW, Kopman J, Grossi SG, Dunford RG. Models to Evaluate the Role of Stress in Periodontal Disease. Ann periodontol. 1998;3:208–302. doi: 10.1902/annals.1998.3.1.288. [DOI] [PubMed] [Google Scholar]


