Abstract
Aims
To describe the levels and identify independent predictors of caregiver burden in partners of patients with heart failure.
Background
Care and support from a partner are important for the well-being of patients with heart failure and may potentially delay disease progression. However, caregiving may be associated with burden and stress and it is therefore important to understand which factors that influence caregiver burden. Theoretical models of caregiving describe the concept of burden as an outcome variable, including decreased well-being and health.
Methods
Data for this descriptive cross-sectional study were collected between January 2005 and September 2008. The dependent variable consisted of the Caregiver Burden Scale total score index. Socio-demographic and clinical characteristics, health-related quality of life, symptoms of depression, perceived control, and knowledge on heart failure were included in a regression analysis to determine independent predictors of caregiver burden.
Results
The 135 partners had a mean-age of 69 years and 75% were females. Caregiver burden was perceived as medium in 30% of the partners. The patients’ Physical Component Score of SF-36 (p<0.001), partners’ Mental Component Score of SF-36 (p<0.001) and perceived control (p<0.01) accounted for 39% of the variance in caregiver burden.
Conclusion
Caregiver burden was lower when the mental health of the partner and the physical health of the patient were better and the partner experienced higher control over the heart disease. A partner-centered approach to educate and support partners of patients with heart failure is essential to improve the life situation for patient–partner dyads.
Keywords: Caregiver burden, Depression, Health-related quality of life, Heart failure, Partner, Nursing
1. Introduction
Patients with chronic Heart Failure (HF) constitute of a large group within the health care. The prevalence of symptomatic chronic HF is estimated to 2% of the population, approximately 15 million in the extended Europe. The condition is a leading cause of hospitalisation for elderly patients at high health care costs. Prognosis of HF is poor and half of the patients die within 4 years [1].
1.1. Caregiving
A caregiver is normally defined as unpaid relatives or friends who support people with disabilities [2]. If a patient with a chronic disease has a partner living in the same household in a marriage-like relationship it is most often that this partner provides most of the caregiving. The extent of caregiving by partners of patients with chronic illness such as HF has increased [3]. The main focus in health care is still on the patients and their needs, but the awareness of partners’ and families’ role and situation is increasing [3].
Strong social support is associated with better outcomes of cardiovascular disease [4]. Partners have a very important role in enhancing patient adherence to complex medical treatment, encouraging self-care behaviour such as symptom monitoring and life style changes, and influencing the well-being of the patient. Living alone increases the risk of psychological stress and is more often associated with poor adherence and self care and recurrent hospitalisations [5–7], while high marital quality has been found to significantly improve 8-year survival in patients with chronic HF [8]. However, informal caregiving and support for patients with chronic HF can negatively affect the partners’ well-being and consequently affect the health and well-being of patients with chronic HF [9].
1.2. Caregiver burden
Caregiving responsibilities of the partners have increased as hospital length of stay became shorter. At discharge, the responsibilities for self-care management are put on the patient and partner [10]. Partners also often support patients in their different daily activities. The most prominent caregiving areas for partners have been found to be practical related support such as taking care of the household, shopping, and taking care of the household finances [11,12]. The reason for the partners support was mainly emotional bonds. The partner provided assistance and psychosocial support for a longer period of time than for example daughters [13]. Caregiving can be associated with increased self-esteem, pride, gratification and a closer relationship with the patient [14]. However, potentially harmful caregiver behaviour was more likely in partner caregiving situations than for other family members and friends. The risk profile for negative caregiver outcomes included greater patient needs for care, cognitive impairment, more physical symptoms, and a risk for clinical depression in the caregiver [15].
Previous studies have identified relatively high levels of deteriorating mental health and quality of life among partners of patients with HF [6,16,17]. Home care during deterioration of HF, gave the patients security, freedom and increased awareness of their symptoms. However, many partners felt anxious when they were alone and fully responsible for the care [18]. Depressive symptoms and stress among partners were associated with the number of caregiving tasks and with the perceived difficulty in performing caregiving activities. Burden, stress, and depression have been found to be significantly associated with the caregiving role in the HF population and therefore highlight the importance of support to improve patient and partner outcomes [19]. The most difficult caregiving tasks were those dealing with patients’ behaviour problems and the most negative outcome of caregiving was having less time for activities with friends [20]. Partners who felt more burdened in the caregiving role and had less control over the health outcomes of the patient were at greater risk for impaired emotional well-being [21]. Knowledge about HF was described by partners as important for managing the caregiver role [22].
While caregiving in other chronic conditions has been described in greater depth, the burden of partners caring for patients with chronic HF [23] has rarely been described in detail and the factors influencing caregiver burden are poorly understood [7].
2. The study
2.1. Aims
The aims of the study were to describe levels of caregiver burden and identify independent predictors of caregiver burden in partners of patients with chronic HF during the early post-discharge phase.
3. Methods
3.1. Design
The study had a descriptive correlational cross-sectional design. As described in the background, previous studies have found that socio-demographic and clinical characteristics, health-related quality of life, symptoms of depression, perceived control, and knowledge on chronic heart failure of partners and patients may be independent predictors of caregiver burden.
3.2. Sample
The study sample was recruited between January 2005 and September 2008 among partners to patients hospitalised with HF exacerbation at the departments of emergency medicine and cardiology at a university hospital as well as all previously hospitalised patients visiting a nurse-led HF clinic at a county hospital. Potential partners were identified by their cohabitation with the HF patient by hospital screening lists that were checked every week. The inclusion criterion for the partners was to cohabit in a marriage-like relationship with a patient diagnosed with HF based on the European Society of Cardiology guidelines [1], in NYHA class II–IV. Exclusion criteria for the partners were dementia, or other severe psychiatric illness, severe drug abuse, difficulties in understanding or reading the Swedish language or participating in other clinical trials. The partners that fulfilled the inclusion criteria and the patients they lived with were initially informed verbally of the study through a telephone call or during a visit to the heart failure clinic. Partners and patients who were interested in taking part in the study were given additional written information.
3.3. Data collection and instruments
A questionnaire packet was sent out to the partner and the patient who agreed to participate. Permission to use and instructions for scoring each instrument were obtained from the appropriate publisher.
Caregiver Burden Scale (CBS)
A 22-item scale developed in Swedish that measures caregiver burden as subjectively experienced by caregivers of chronically disabled individuals. Responses are scored on a scale from 1 to 4 (not at all, seldom, sometimes, and often). The total burden index is the mean of all 22 items and higher scores indicate greater burden. The total burden index can be divided into three groups; low burden (1.00–1.99), medium burden (2.00–2.99) and high burden (3.00–4.00). The CBS can also be divided into five indexes: General strain (8 items) dealing with the lack of personal freedom in relation to caregiving. Isolation (3 items) includes limited social interaction and private time for the partner. Disappointment (5 items) deals with loneliness, physical burden, financial impact and the feeling that life is unfair. Emotional involvement (3 items) concerns embarrassment, hurt and anger due to the patient’s behaviour. Environment (3 items) contains items about partners’ experiences of not being able to handle practical problems related to the care of the patient [24,25]. A previous study on reliability showed high internal consistency for the five indexes found in a factor analysis with Cronbach’s alpha values between 0.70 and 0.87, except for the index environment (0.53). [25].
Short Form (SF)-36
A generic 36-item scale which evaluates health in 8 dimensions. The dimensions are weighed together in two consecutive indexes; Physical Component Score (PCS) and Mental Component Score (MCS). The physical part is made up of the dimensions of physical functioning, physical role functioning, bodily pain and general health and the mental part of the four dimensions of vitality, social functioning, emotional role functioning and mental health. A higher score indicates better health [26]. The instrument has been validated in Swedish. Cronbach’s alpha estimates exceeded the 0.80 level [27].
Beck Depression Inventory (BDI)-II
is a 21-question multiple-choice self-report inventory with each answer being scored on a scale value of 0 to 3. Higher total scores indicate more severe depressive symptoms. The cut off scores used are: 0–13: no depression; 14–19: mild depression; 20–28: moderate depression; and 29–63: severe depression [28,29]. The instrument has been validated in Swedish. The reliability coefficient alpha showed > 0.86 [29].
Control Attitude Scale (CAS)
A 4-item tool designed to measure a person’s perceptions of control over their cardiovascular-related health. The CAS can also be used in partners (family version). Perceived control is important for psychological well-being and recovery. The first question addresses how much control the patient has over his situation and the second question addresses how much control the patient thinks the partner has. The last two questions address how helpless patients feel and how helpless the patient thinks their partner feels. The questions to the partner are directed at the levels of control and helplessness they perceive and how much control and helplessness they think the patient has. Response statements are scored on a scale from 1 (none) to 7 (very much). The total score range is 4 to 28, with higher scores reflecting higher levels of perceived control [30,31]. The psychometric testing is in progress for the Swedish translation and the preliminary testing has shown reliability coefficient alpha > 0.80 for the patient version and 0.60 to 0.70.for the partner version.
Knowledge Questionnaire (RAND)
This 21-item questionnaire was used to assess knowledge of HF including HF symptoms and management among patients and partners. Three questions in the instrument asked patients and partners to rank their understanding of HF, their understanding of the way medicines work and their understanding of prevention of HF deterioration. Responses to these questions and a single item with an open-ended answer regarding weight were not reported in this paper. The rest of the items were summed to obtain a total knowledge score where a correct answer scored one and wrong answer scored zero [32]. The knowledge questionnaire was developed in the REACT study for acute myocardial patients [33]. It was later adapted to HF patients and internal consistency reliability found to be 0.83 [32]. The Swedish forward–backward translation used in the study has not yet been further validated.
Charlson Co-morbidity Index (CCI)
An instrument used to classify co-morbid conditions which might influence mortality. An index is calculated by adding the weighted scores, theoretical range 0 to 34 (0 means no co-morbid disease). Data have shown that this index independently predicts short-term and long-term mortalities as well as health care costs. [34,35].
Demographic data including health history was collected using a self-administrated questionnaire identifying age, gender, education, habits like smoking, alcohol consumption and physical activity, psychosocial support. Body mass index and NYHA class were also recorded.
3.4. Data analysis
Descriptive statistics were computed for all study variables. The amount of missing data was low (0.7–8.1%) in all instruments. If only one item in a subscale of SF-36 was missing that item was imputed by the mean of the subscale; otherwise missing items were not replaced. Missing data for other instruments were not replaced and the scale/subscale would be recorded missing for the person.
The relationship between socio-demographic and clinical characteristics and each of the variables of interest was analysed using Pearson moment correlations for normally distributed scores or Spearman rank order correlation for non-normally distributed scores.
Linear regression analyses with caregiver burden as dependent variable were done in the following steps. The variables (gender, age, symptoms of depression, health-related quality of life, perceived control, knowledge of HF, co-morbidity in the patient and partner and severity of HF measured by NYHA class) were first entered separately into the equations as independent predictor variables. Second the independent variables were grouped in three groups: 1. Characteristics, 2. Physical and 3. Mental variables. On the basis of the univariate analyses, variables that were significantly predictive of caregiver burden at a significance level of p ≤ 0.05 or less were entered into stepwise forward regressions within each group [36]. Beta values were reported for univariate analysis, analysis within groups and for the final model. In the final step those variables associated with caregiver burden in previous multivariate regression with a p-value < 0.1 were included to identify the combination of variables with the most predictive power. The significance level was set at p ≤ 0.05 for the final stepwise regression analysis and the percentage of variance (the r2-value) was reported for the final model. Statistical analyses were performed using SPSS 15.0.
The sample size was calculated to allow for regression analysis. The analysis was done in three steps. A maximum of six variables were included at the same time in the regression analysis and as 15 participants are recommended per variable a sample size of 90 was required [36].
3.5. Ethical considerations
Throughout the study the principles outlined in the Declaration of Helsinki have been followed. Permission to carry out the study was granted from the Regional Ethical Review Board in Linköping, Sweden. All partners and patients were approached in a sensitive manner and received verbal and written information about the study. The partners and patients that chose to participate gave written informed consent before entering the study and they were assured confidentiality and that a decision to withdraw from the study would not affect their future care.
4. Results
4.1. Characteristics of the sample
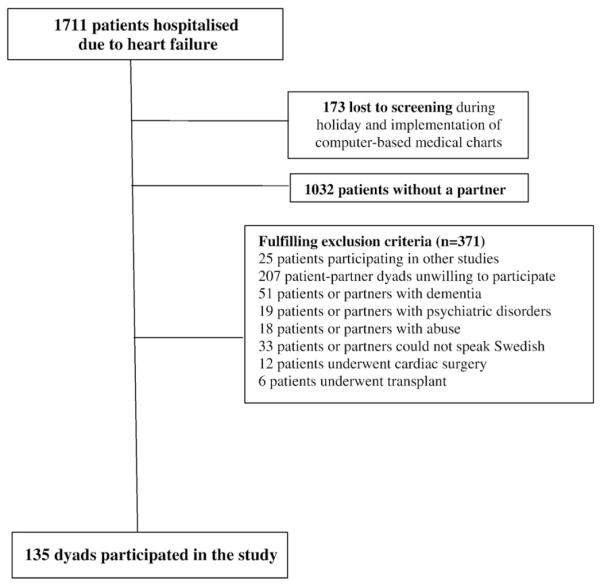
As shown in Fig. 1, 1711 patients were hospitalised due to HF exacerbation during the time of study inclusion. More than half of the screened patients with HF did not have a partner and 371 dyads fulfilled the exclusion criteria the most common of which was unwillingness to participate often secondary to patient and/or the partner felt too ill or fatigued (n = 207).
Fig. 1.
Flow chart illustrating the sampling process.
The demographic characteristics of the patient–partner dyads are presented in Table 1. A typical partner was female living with a retired patient with HF in NYHA class III. The mean CCI for patients of 2.7 (SD 1.9, range 1–11) was higher compared to their partners 0.7 (SD 1.2, range 0–8) (p = 0.008) which supports previously reported research that purports that patients with chronic HF suffer from several co-morbidities (e.g. hypertension, diabetes, obesity, and renal disease) [1].
Table 1.
Characteristics of the dyads (N = 135) consisting of patients with heart failure and their partners.
| Patient | Partner | |
|---|---|---|
| Age mean, min–max (SD) | 71, 32–90 (±12) | 69, 28–90 (±12) |
| Male | 101 (75%) | 34 (25%) |
| NYHA | ||
| Class II | 46 (34%) | |
| Class III | 70 (52%) | |
| Class IV | 19 (14%) | |
| Myocardial infarction | 46 (35%) | 11 (8%) |
| Atrial fibrillation | 77 (57%) | 10 (7%) |
| Hypertension | 53 (39%) | 42 (31%) |
| Stroke | 16 (12%) | 7 (5%) |
| Lung disease | 20 (16%) | 16 (13%) |
| Diabetes | 28 (21%) | 13 (10%) |
| Education level | ||
| Compulsory school | 15 (11%) | 15 (11%) |
| Elementary school | 61 (45%) | 62 (46%) |
| Upper secondary school | 38 (28%) | 39 (29%) |
| University | 12 (9%) | 13 (10%) |
| Missing | 9 (7%) | 6 (4%) |
| Smoking history | ||
| Never smoked | 58 (43%) | 70 (52%) |
| Previous history of smoking | 61 (45%) | 41 (30%) |
| Current smokers | 6 (4%) | 14 (10%) |
| Missing | 10 (7%) | 10 (7%) |
| Alcohol consumption | ||
| Never | 34 (25%) | 30 (22%) |
| 1 glass or less/week | 49 (36%) | 50 (37%) |
| 2–7 glasses/week | 32 (24%) | 38 (28%) |
| >7 glasses/week | 7 (5%) | 6 (4%) |
| Missing | 11 (8%) | 11 (8%) |
| Physical activity | ||
| >3 h/week | 39 (29%) | 64 (47%) |
| 1–3 h/week | 39 (29%) | 37 (27%) |
| <60 min/week | 28 (21%) | 19 (14%) |
| Performed no physical activity | 20 (15%) | 5 (4%) |
| Missing | 9 (7%) | 10 (7%) |
| BMI mean (SD) | 27 (±4) | 26 (±5) |
| Missing | 6 (4%) | 15 (11%) |
SD = Standard Deviation.
NYHA = New York Heart Association Classification.
BMI = Body Mass Index.
4.2. Level of caregiver burden
Questionnaire packages were sent to 135 partners and patients with chronic HF and all of them participated in the study. One of the partners did not complete the Caregiver Burden Scale, beside that there were no missing data in the dependent variables.
The mean caregiver burden reported by the partners was 1.77. Sixty-eight percent of the partners (n = 91) reported low levels of caregiver burden, 30% (n = 40) reported medium and 2% (n = 3) high levels of caregiver burden. The items on the CBS were divided into five indexes: general strain, isolation, disappointment, emotional involvement and environment. Results are shown in Table 2. The dimension that had the highest value was general strain dealing with the lack of personal freedom, followed by isolation involving limited social interaction and disappointment comprising of loneliness, physical burden, financial impact and the feelings that life was unfair.
Table 2.
Result of the subscales of Caregiver Burden Scale (n = 134).
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Total | 1.77 | 0.54 | 1.00 | 3.32 |
| General strain | 1.88 | 0.64 | 1.00 | 3.75 |
| Isolation | 1.80 | 0.77 | 1.00 | 4.00 |
| Disappointment | 1.72 | 0.63 | 1.00 | 3.80 |
| Emotional involvement | 1.66 | 0.63 | 1.00 | 4.00 |
| Environment | 1.63 | 0.56 | 1.00 | 3.00 |
4.3. Predictors of caregiver burden in partners
Age, gender and knowledge of chronic HF were not significantly related to caregiver burden.
In the stepwise final model, the Mental Component Score of SF-36 (p < 0.001) of the partner and the Physical Component Score of SF-36 (p < 0.001) of the patient and the perceived control measured by CAS of the partner (p < 0.01) accounted for 39% of the variance of the total level of caregiver burden (see Table 3). The regression analysis showed that poorer mental health and a lower perceived control in the partners and poorer physical health of patients predicted a higher caregiver burden.
Table 3.
Predictors of caregiver burden.
| Univariate analysis |
Stepwise selection within groups |
Stepwise final model |
|||||
|---|---|---|---|---|---|---|---|
| Mean | Beta | p | Beta | p | Beta | p | |
| 1. Characteristics | |||||||
| Patient age, mean (SD) |
0.97 | 0.267 | |||||
| Gender patient, men |
−0.001 | 0.988 | |||||
| CCI, patient | 2.7 | 0.283 | 0.001 | 0.242 | 0.003 | 0.094 | 0.3 |
| CCI, partner | 0.7 | 0.083 | 0.3 | ||||
| CAS, patient | 16.1 | −0.292 | 0.001 | −0.151 | 0.07 | 0.106 | 0.21 |
| CAS, partner | 15.9 | −0.430 | 0.001 | −0.344 | 0.001 | −0.21 | 0.01 |
| knowledge on CHF, patient |
13.0 | −0.024 | 0.8 | ||||
| knowledge on CHF, partner |
12.7 | −0.055 | 0.5 | ||||
| 2. Physical | |||||||
| SF-36-PCS, patient |
33.1 | −0.373 | 0.001 | −0.372 | 0.001 | −0.313 | 0.001 |
| SF-36-PCS, partner |
46.1 | −0.162 | 0.064 | −0.118 | 0.2 | ||
| NYHA class, patient |
0.215 | 0.01 | 0.132 | 0.1 | |||
| 3. Mental | |||||||
| BDI patient | 11.9 | 0.309 | 0.001 | 0.069 | 0.5 | ||
| BDI partner | 7.0 | 0.365 | 0.001 | 0.060 | 0.6 | ||
| SF-36-MCS, patient |
41.4 | −0.406 | 0.001 | −0.265 | 0.01 | −0.123 | 0.1 |
| SF-36-MCS, partner |
46.8 | −0.482 | 0.001 | −0.417 | 0.001 | −0.38 | 0.001 |
SD = Standard Deviation.
NYHA = New York Heart Association Classification.
CCI = Charlson Co-morbidity Index.
CAS = Control Attitude Scale.
CHF = Chronic Heart Failure.
BDI = Beck Depression Inventory.
PCS = Physical Component Score.
MCS = Mental Component Score.
More co-morbidities and lower perceived control over the disease in patients as well as poorer mental function in the patients were significant predictors of caregiver burden in the stepwise forward regressions within each group. However, they did not reach significance in the final model.
5. Discussion
5.1. Levels of caregiver burden
Two thirds of the partners in our study experienced low levels of caregiver burden which is consistent with findings in other studies showing that informal caregiving in partners of patients with a variety of chronic diseases also led to new roles and responsibilities that can be associated with positive effects for the partner [14,37,38]. However, it is important to note that almost one third of the partners experienced medium levels of caregiver burden. General strain was the subscale where the partners in our study felt most burdened. Lukkarinen and Kyngas [39] and Pressler et al.[20] also found that partners experienced limitations in their daily life and lost some of their personal freedom when using their resources to help a patient suffering from cardiovascular disease. Partners who experienced general strain while providing informal care to patients with chronic diseases also experienced decreased mental and physical health [15,40]. Health care professionals should be aware of the fact that partners who perceive medium levels of caregiver burden are risk for feeling ill themselves and for an untimely death [40].
5.2. Predictors of caregiver burden in partners
Our findings that higher caregiver burden was associated with more physical and mental health problems are similar to findings from Saunders [41]. Andren and Elmstahl [42] found that partners with a low sense of coherence and poorer health experienced a greater burden especially in the isolation, disappointment and emotional involvement indexes. A qualitative study by Martensson et al. [22] showed that when partners were recognised and treated as valuable individuals they were less burdened. This included that partners had someone to turn to and were included in the physical care. By contrast, partners felt like outsiders when held at a distance by the patient, became socially isolated and lacked support from their children, friends and professionals [19,22].
We found that a higher degree of caregiver burden was related to worse physical function of the patient. This is from a clinical point of view not surprising since patients with more symptomatic and severe stages of HF are more impaired in their daily life and need more assistance from their partner. Several studies have confirmed that symptoms like fatigue and dyspnoea improved when patients engaged in physical activity and these consequently impacted rates of hospital readmissions and well-being [43]. However, Molloy et al. [44] found that when frail, older patients with chronic HF were involved in an exercise intervention, the partners’ caregiver burden increased [44]. A limitation in this study was that the partners were not actively involved in the intervention. It would therefore be interesting to evaluate if an intervention incorporating the partners could reduce caregiver burden.
Our study results suggest that perceived control was an important factor contributing to less caregiver burden in partners of patients with a deteriorating health due to chronic HF. Perceived control has previously been shown to be important for psychological recovery [21,31,45] and is relevant for effective self treatment of disease. There is a general agreement that high levels of perceived control are important for well-being in older adults [46].
Saunders [47] reported that variables such as the partners’ advanced age and more patient co-morbidities were associated with caregiver burden [47]. As in many previous studies most of the partners in our study were females (75%). Men with HF often have a partner, while women are diagnosed with HF 10 years later in life than men and more often widowed or have an ill partner. Previous research have shown that female partners report a higher need for support than male partners [11,48]. However, our results suggest that age, gender and disease severity or co-morbidities do not affect the experience of caregiver burden after controlling for other factors. The reason why the patients’ self-assessed physical health was a significant predictor of caregiver burden while more objective measures of disease severity (NYHA class assessed by nurses/physicians) and comorbidity did not affect caregiver burden might be explained by the fact that perceived health is affecting people’s daily life more than objective measures.
Aldred et al. found that the patients with chronic HF experienced social isolation and concerns about the future. They lacked support from health care professionals and few had the possibility to discuss prognosis and options for palliation and support. Many patients were concerned with the burden that chronic HF placed on their partner, even though the partners did not always describe feeling burdened [3]. EU policymakers and guidelines have highlighted the need to optimise health care resources for dependent older people by supporting the partners, especially by delivering financial service, and targeted support for the most burdened partners with practical and flexible respite, day care and information services [13].
We chose to examine caregiver burden in the HF population because while the previous research showed that partners experience anxiety and depression, few studies have described the burden on the partners. In some aspects HF can be compared to other severe chronic diseases where partners are caregivers, but the disease does not seem to be so burdensome for the partner in comparison with other chronic illnesses. Other studies of partners to patients with stroke and dementia [24,25,42] have shown greater caregiver burden compared to our findings in partners of patients with HF. For example, HF affects the mental function less than stroke and dementia do which might explain why partners of patients with HF experience lower levels of caregiver burden. However, one third of the partners in our study experienced a medium degree of caregiver burden. Therefore evaluating caregiver burden in relation to HF is of clinical relevance and to address needs of support from nurses in order to avoid suffering, deteriorating health and untimely death in partners.
6. Study limitations
This study is limited by its cross-sectional study design which does not permit causal conclusions. Other variables that were not measured in the current study could have contributed to caregiver burden among partners of patients with chronic HF. The sample size was quite small, which can partially be attributed to the large number of patients with chronic HF screened who did not live with a partner. However, the sample size was sufficient for the regression analysis performed [36]. Several partners were excluded due to unwillingness to participate as a result of the patient and/or the partner being too ill or fatigued which might decrease the generalisability of the findings to partners most affected by the chronic HF. The gender distribution in our study was unequal, but mirrors the reality that women provide informal care more often than men [13]. The sample in our study was quite homogenous. The patients were moderately to severely ill and the partners were included in the study during a post-discharge phase after deterioration of heart failure and no patients had mild heart failure. On the other hand few patients in our study had an advanced chronic HF (NYHA IV) needing end-of-life care. In patients with more advanced chronic HF, Aldred et al. [3] found that most aspects of life were curtailed, especially every day activities, for both patients and their partners [3]. This means that the finding maybe cannot be generalised to partners of patients with mild or very advanced heart failure and also that the result may be generalised with caution to male caregiving partners.
The dyads were asked to fill in the questionnaire individually, but as the questionnaires were completed at home, we could not confirm that patients and partners did indeed complete the questionnaires independently. Finally, all instruments except the knowledge scale had a Swedish well-documented and satisfactory validity and reliability. The results on knowledge should therefore be interpreted with caution. There is a lack of well validated knowledge scales [49], but two scales namely the Patient Knowledge Questionnaire for Heart failure patients [50] and the Dutch Heart Failure Knowledge Scale [51] are available. Despite the limited testing of reliability and validity these scales might have been the better options to use [49]. Despite these study limitations, this study is one of the major studies published to date on chronic HF dyads and findings can be used in developing interventions to potentially reduce partners’ burden and enhance better health-related quality of life and increased levels of perceived control.
7. Conclusion
Almost one third of partners of patients with HF experienced a medium level of caregiver burden. Caregiver burden was lower when the mental health of the partner was better, the physical health of the patient was better and when the partner experienced higher control over the cardiovascular-related health of the patient. The most burdensome areas in relation to caregiving were decreased personal freedom and limited social interaction.
A partner-centered approach to educate and support patients with HF and their partners is essential to ensure an adequate life situation for the dyads.
The issue of if and how HF partners experience caregiver burden is complex and warrants further research. Larger longitudinal studies following caregiver burden and its predictors over time would therefore be of interest to perform.
8. Clinical and research implications
Interventions to improve self-care in patients with chronic HF should also include their partners in order to strengthen the relationship during the illness process.
Interventions to reduce the caregiver burden should focus on providing the patient–partner dyads with strategies for improving mental and physical health, self care and coping through professional support. Interventions including exercise training, education and psychosocial support for the dyads need to be further evaluated in randomised studies.
Nurses should assist the patient–partner dyads to change factors that contribute to physical and emotional distress by changing thoughts and behaviour in a positive manner and assisting the dyads in resolving problems related to chronic HF.
Acknowledgement
We thank Linköping University, Swedish Institute for Health Sciences, Sweden, the Swedish Research Council and the Vårdal Foundation for financial support. We also thank patients with chronic heart failure and their partners who participated in the study, Annette Waldemar, Lillevi Nestor from Heart Failure clinic in Norrköping and the secretaries Lotta Björk and Berit Andersson for the help to find the study participants.
References
- [1].Dickstein KC-SA, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Eur J Heart Fail. 2008;10:933–89. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- [2].National Alliance for Caregiving A . Caregiving in the U.S. National Alliance for Caregiving, AARP; Bethesda, MD: Apr, 2004. [Google Scholar]
- [3].Aldred H, Gott M, Gariballa S. Advanced heart failure: impact on older patients and informal carers. J Adv Nurs. 2005;49:116–24. doi: 10.1111/j.1365-2648.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- [4].Daugherty J, Saarmann L, Riegel B, Sornborger K, Moser D. Can we talk? Developing a social support nursing intervention for couples. Clin Nurs Specialist. 2002;16:211–8. doi: 10.1097/00002800-200207000-00011. [DOI] [PubMed] [Google Scholar]
- [5].Luttik ML, Jaarsma T, Moser D, Sanderman R, van Veldhuisen DJ. The importance and impact of social support on outcomes in patients with heart failure: an overview of the literature. J Cardiovasc Nurs. 2005;20:162–9. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- [6].Luttik ML, Jaarsma T, Veeger NJ, van Veldhuisen DJ. For better and for worse: quality of life impaired in HF patients as well as in their partners. Eur J Cardiovasc Nurs. 2005;4:11–4. doi: 10.1016/j.ejcnurse.2004.12.002. [DOI] [PubMed] [Google Scholar]
- [7].Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs. 2008;23:258–65. doi: 10.1097/01.JCN.0000305093.20012.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. Am J Cardiol. 2006;98:1069–72. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- [9].Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail. 2005;7:592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- [10].Mistiaen P, Duijnhouwer E, Wijkel D, de Bont M, Veeger A. The problems of elderly people at home one week after discharge from an acute care setting. J Adv Nurs. 1997;25:1233–40. doi: 10.1046/j.1365-2648.1997.19970251233.x. [DOI] [PubMed] [Google Scholar]
- [11].Luttik ML, Jaarsma T, Veeger N, Tijssen J, Sanderman R, van Veldhuisen DJ. Caregiver burden in partners of Heart Failure patients; limited influence of disease severity. Eur J Heart Fail. 2007;9:695–701. doi: 10.1016/j.ejheart.2007.01.006. [DOI] [PubMed] [Google Scholar]
- [12].Luttik ML, Jaarsma T, Tijssen JG, van Veldhuisen DJ, Sanderman R. The objective burden in partners of heart failure patients; development and initial validation of the Dutch Objective Burden Inventory. Eur J Cardiovasc Nurs. 2008;7:3–9. doi: 10.1016/j.ejcnurse.2007.02.005. [DOI] [PubMed] [Google Scholar]
- [13].Lamura G, Mnich E, Nolan M, Wojszel B, Krevers B, Mestheneos L, et al. Family carers’ experiences using support services in Europe: empirical evidence from the EUROFAMCARE study. Gerontologist. 2008;48:752–71. doi: 10.1093/geront/48.6.752. [DOI] [PubMed] [Google Scholar]
- [14].Rees J, O’Boyle C, MacDonagh R. Quality of life: impact of chronic illness on the partner. J R Soc Med. 2001;94:563–6. doi: 10.1177/014107680109401103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, Lance CE. Risk factors for potentially harmful informal caregiver behavior. J Am Geriatr Soc. 2005;53:255–61. doi: 10.1111/j.1532-5415.2005.53111.x. [DOI] [PubMed] [Google Scholar]
- [16].Martensson J, Dracup K, Canary C, Fridlund B. Living with heart failure: depression and quality of life in patients and spouses. J Heart Lung Transplant. 2003;22:460–7. doi: 10.1016/s1053-2498(02)00818-5. [DOI] [PubMed] [Google Scholar]
- [17].Pihl E, Jacobsson A, Fridlund B, Stromberg A, Martensson J. Depression and health-related quality of life in elderly patients suffering from heart failure and their spouses: a comparative study. Eur J Heart Fail. 2005;7:583–9. doi: 10.1016/j.ejheart.2004.07.016. [DOI] [PubMed] [Google Scholar]
- [18].Dinesen B, Nohr C, Andersen SK, Sejersen H, Toft E. Under surveillance, yet looked after: telehomecare as viewed by patients and their spouse/partners. Eur J Cardiovasc Nurs. 2008;7:239–46. doi: 10.1016/j.ejcnurse.2007.11.004. [DOI] [PubMed] [Google Scholar]
- [19].Saunders MM. Family caregivers need support with heart failure patients. Holistic Nurs Pract. 2003;17:136–42. doi: 10.1097/00004650-200305000-00004. [DOI] [PubMed] [Google Scholar]
- [20].Pressler SJ, Gradus-Pizlo I, Chubinski SD, Smith G, Wheeler S, Wu J, et al. Family caregiver outcomes in heart failure. Am J Crit Care. 2009;18:149–59. doi: 10.4037/ajcc2009300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dracup K, Evangelista LS, Doering L, Tullman D, Moser DK, Hamilton M. Emotional well-being in spouses of patients with advanced heart failure. Heart Lung. 2004;33:354–61. doi: 10.1016/j.hrtlng.2004.06.003. [DOI] [PubMed] [Google Scholar]
- [22].Martensson J, Dracup K, Fridlund B. Decisive situations influencing spouses’ support of patients with heart failure: a critical incident technique analysis. Heart Lung. 2001;30:341–50. doi: 10.1067/mhl.2001.116245. [DOI] [PubMed] [Google Scholar]
- [23].Gure TR, Kabeto MU, Blaum CS, Langa KM. Degree of disability and patterns of caregiving among older Americans with congestive heart failure. J Gen Intern Med. 2008;23:70–6. doi: 10.1007/s11606-007-0456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Andren S, Elmstahl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci. 2005;19:157–68. doi: 10.1111/j.1471-6712.2005.00328.x. [DOI] [PubMed] [Google Scholar]
- [25].Elmstahl S, Malmberg B, Annerstedt L. Caregiver’s burden of patients 3 years after stroke assessed by a novel Caregiver Burden Scale. Arch Phys Med Rehabil. 1996;77:177–82. doi: 10.1016/s0003-9993(96)90164-1. [DOI] [PubMed] [Google Scholar]
- [26].Ware JE. SF-36 health survey manual and interpretation guide. The New Health Institute, New England Medical Center; Boston: 1993. [Google Scholar]
- [27].Sullivan M, Karlsson J, Ware JE., Jr The Swedish SF-36 Health Survey-I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med. 1995;41:349–58. doi: 10.1016/0277-9536(95)00125-q. [DOI] [PubMed] [Google Scholar]
- [28].Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- [29].Beck AT, Steer RA, Brown GK. Manual for the Beck depression Inventory-II (svensk version) Psykologiförlaget; Sandviken: 2005. [Google Scholar]
- [30].Moser DK, Dracup K. Psychosocial recovery from a cardiac event: the influence of perceived control. Heart Lung. 1995;24:273–80. doi: 10.1016/s0147-9563(05)80070-6. [DOI] [PubMed] [Google Scholar]
- [31].Moser DK, Dracup K. Impact of cardiopulmonary resuscitation training on perceived control in spouses of recovering cardiac patients. Res Nurs Health. 2000;23:270–8. doi: 10.1002/1098-240x(200008)23:4<270::aid-nur3>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- [32].Caldwell MA, Peters KJ, Dracup KA. A simplified education program improves knowledge, self-care behavior, and disease severity in heart failure patients in rural settings. Am Heart J. 2005;150:983. doi: 10.1016/j.ahj.2005.08.005. [DOI] [PubMed] [Google Scholar]
- [33].Simons-Morton DG, Goff DC, Osganian S, Goldberg RJ, Raczynski JM, Finnegan JR, et al. Rapid early action for coronary treatment: rationale, design, and baseline characteristics. REACT Research Group. Acad Emerg Med. 1998;5:726–38. doi: 10.1111/j.1553-2712.1998.tb02492.x. [DOI] [PubMed] [Google Scholar]
- [34].Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- [35].Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79:1640–4. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- [36].Field A. Discovering statistics using SPSS. 2nd ed SAGE publications; London: 2005. [Google Scholar]
- [37].Beach SR, Schulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15:259–71. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- [38].Bakas T, Pressler SJ, Johnson EA, Nauser JA, Shaneyfelt T. Family caregiving in heart failure. Nurs Res. 2006;55:180–8. doi: 10.1097/00006199-200605000-00004. [DOI] [PubMed] [Google Scholar]
- [39].Lukkarinen H, Kyngas H. Experiences of the onset of coronary artery disease in a spouse. Eur J Cardiovasc Nurs. 2003;2:189–94. doi: 10.1016/S1474-5151(03)00062-8. [DOI] [PubMed] [Google Scholar]
- [40].Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- [41].Saunders MM. Family caregiver support and hospitalizations of patients with heart failure. Home Healthcare Nurs. 2008;26:624–32. doi: 10.1097/01.NHH.0000341226.40640.ad. [DOI] [PubMed] [Google Scholar]
- [42].Andren S, Elmstahl S. The relationship between caregiver burden, caregivers’ perceived health and their sense of coherence in caring for elders with dementia. J Clin Nursing. 2008;17:790–9. doi: 10.1111/j.1365-2702.2007.02066.x. [DOI] [PubMed] [Google Scholar]
- [43].Dracup K, Evangelista LSHM, Erickson V, Hage A, Moriguchi J, Canary C, MacLellan WR, Fonarow GC. Effects of a home-based exercise program on clinical outcomes in heart failure. Am Heart J. 2007;154:877–83. doi: 10.1016/j.ahj.2007.07.019. [DOI] [PubMed] [Google Scholar]
- [44].Molloy GJ, Johnston DW, Gao C, Witham MD, Gray JM, Argo IS, et al. Effects of an exercise intervention for older heart failure patients on caregiver burden and emotional distress. Eur J Cardiovasc Prev Rehabil. 2006;13:381–7. doi: 10.1097/01.hjr.0000198916.60363.85. [DOI] [PubMed] [Google Scholar]
- [45].Dracup K, Westlake C, Erickson VS, Moser DK, Caldwell ML, Hamilton MA. Perceived control reduces emotional stress in patients with heart failure. J Heart Lung Transplant. 2003;22:90–3. doi: 10.1016/s1053-2498(02)00454-0. [DOI] [PubMed] [Google Scholar]
- [46].Jacelon CS. Theoretical perspectives of perceived control in older adults: a selective review of the literature. J Adv Nurs. 2007;59:1–10. doi: 10.1111/j.1365-2648.2007.04320.x. [DOI] [PubMed] [Google Scholar]
- [47].Saunders MM. Factors associated with caregiver burden in heart failure family caregivers. West J Nurs Res. 2008;30:943–59. doi: 10.1177/0193945908319990. [DOI] [PubMed] [Google Scholar]
- [48].Rohrbaugh MJ, Cranford JA, Shoham V, Nicklas JM, Sonnega JS, Coyne JC. Couples coping with congestive heart failure: role and gender differences in psychological distress. J Family Psychol. 2002;16:3–13. doi: 10.1037//0893-3200.16.1.3. [DOI] [PubMed] [Google Scholar]
- [49].Stromberg A. Measuring patients’ knowledge about heart failure. Eur J Cardiovasc Nurs. 2005;4:267–8. doi: 10.1016/j.ejcnurse.2005.10.007. [DOI] [PubMed] [Google Scholar]
- [50].Lainscak M, Keber I. Validation of self assessment patient knowledge questionnaire for heart failure patients. Eur J Cardiovasc Nurs. 2005;4:269–72. doi: 10.1016/j.ejcnurse.2005.04.010. [DOI] [PubMed] [Google Scholar]
- [51].van der Wal MH, Jaarsma T, Moser DK, van Veldhuisen DJ. Development and testing of the Dutch Heart Failure Knowledge Scale. Eur J Cardiovasc Nurs. 2005;4:273–7. doi: 10.1016/j.ejcnurse.2005.07.003. [DOI] [PubMed] [Google Scholar]