Abstract
Background:
Bhutan has attained universal child immunization since 1991. Since then, immunization coverage is maintained at high level through routine immunization, periodic National Immunization Days, and mop up campaigns. Despite high immunization coverage, every year, significant numbers of clinically suspected measles cases were reported.
Objective:
To assess the cause of continuing high “suspected measles cases” and take appropriate public health measures.
Materials and Methods:
Febrile rash outbreaks occurred in several districts in 2003. These episodes were investigated. Simultaneously, a retrospective data search revealed evidence of congenital rubella syndrome (CRS) in the country.
Results:
Thirty five percent of the tested samples were positive for rubella but none for measles. There were evidences of the presence of CRS. This was discussed in the annual health conference 2004, amongst health policy makers and district heads who recommended that a possibility of inclusion of rubella as an antigen be looked into. A nationwide measles and rubella immunization campaign was conducted in 2006 followed by introduction of rubella vaccine in the immunization schedule.
Conclusion:
Febrile rash can be caused by a host of viral infections. Following universal measles immunization, it is pertinent that febrile rash be looked in the light of rubella infections. Following the introduction of rubella vaccination in the national immunization schedule, there has been significant reduction of febrile rash episodes, cases of rubella, and congenital rubella syndrome.
Keywords: Campaign, congenital rubella syndrome, immunization, measles, rubella
Introduction
With a total population of 634,982, Bhutan is one of the smallest and the most sparsely populated country in South Asia. The population is young, with under 15 population estimated to be 42.1%.(1)
Bhutan achieved universal child immunization in 1991, and since then has been maintaining 95% coverage for the primary series of vaccines.(2) Measles vaccine coverage has been more than 85% since 1994, and possibly over 96% according to the 2000 cluster survey.(3) Despite high coverage, a large number of cases of measles continued to be reported throughout the country.(3) Between 1993 and 2002, a total of 3,201 cases of measles were reported, while there were virtually no reports of other vaccine preventable diseases.
Common pathogens causing measles-like illnesses are viruses such as rubella, dengue, parvovirus B19, human herpes virus, and coxsackie virus. It is difficult to differentiate them clinically, and as shown by Oliveria and associates, serological tests are cheap and reliable mode of confirming the diagnosis.(4)
Materials and Methods
Serological surveillance
Febrile rash outbreaks occurred in eight of 20 districts in the country in 2002, which continued through to 2003. These districts were scattered throughout the country. A total of 201 serum samples were tested for anti-measles IgM and anti-rubella IgM collected by individual health units and tested by the Public Health laboratory at Thimphu.
Retrospective search of data
A retrospective data search was made to ascertain evidences of CRS in the country. This required reviewing inpatient record, patient referral record, outpatient records at the JDWNR hospital Ophthalmology department and records maintained by the Physiotherapy department.
Results
Serological evaluation of the samples revealed that none of the sample tested positive for measles, whereas 35% tested positive for rubella.(4) The samples were positive from 77% of the districts indicating that rubella was widespread in the country. Review of inpatient record revealed clinical diagnosis of CRS in two patients in 2003 at the JDWNR Hospital and five patients at the Regional referral hospital. Thirty one out of 87 children recorded at the Pediatrics department at JDWNR Hospital with developmental and behavioral abnormalities in 1999 and 2000 were compatible with clinically confirmed case of CRS. Sixteen children who attended the physiotherapy clinic in 2004 were examined over a period of six months and 7 children fitted in the WHO case definition of clinically confirmed CRS.
Retrospective analysis of outpatient data of ophthalmology department at the JDWNR Hospital showed that the clinic had recorded 13 children with congenital cataract between 2001 to 2003. Foetal congenital anomalies occur with rubella infection before 11 weeks of pregnancy.(5) Studies show that up to 25% of congenital cataract follows rubella infection in pregnancy.(6,7)
A total of 44 children were referred to tertiary cardiac centers outside the country from January 2000 to May 2004 with congenital heart conditions. A total of 49 new congenital heart examinations were made since October. 2003 till March 2004 at the national referral hospital. Studies in some countries have revealed that upto 56% of congenital heart diseases are associated with rubella infection during pregnancy.(8)
Retrospective analysis of records and other studies highlighted evidence of existence of congenital rubella syndrome (CRS) in significant proportions in the Bhutanese community.
Disease burden and social and economic consequences
Rubella can become a major public health issue when infection occurs during first trimester of pregnancy. This can result in miscarriage or development of CRS in the foetus. Most anomalies occur if rubella infection occur before 11 weeks of pregnancy;(5) however studies show that up to 25% of congenital cataract follows rubella infection in pregnancy.(6,7)
Rubella occurs as epidemics every 5 to 9 years. The WHO estimates incidence of CRS between 0.5–2.2/1000 live births during epidemics in developing countries(7) and interpolating it for Bhutan it was estimated that there would be 22–44 cases each year.
The economic costs of treatment are not available for Bhutan but reports from Barbados and Guyana show that lifetime cost of maintaining a child with CRS ranged between US $50,000–63,990, respectively.(9) In the Caribbean it was estimated that the cost of eliminating rubella through vaccination was US $4.5 million as compared to US $60 million for treating CRS.(9) Experiences from other countries cost benefit analysis of rubella and CRS prevention show huge social and economic benefits of prevention over treatment.(10)
Planning for mass immunization
The data(11) on burden of disease was presented to the highest policy and decision makers of the country. The issue of rubella and congenital rubella syndrome was debated extensively in the 2004 annual health conference in Thimphu. The conference endorsed that “rubella is an urgent problem in the country and recommended that the Ministry of Health immediately consider possibility of introducing rubella vaccination.”(12)
Experts from WHO SEARO and Geneva also conducted field visits and further recommended introduction of rubella vaccinations in Bhutan.(13,14)
A onetime mass rubella immunization campaign followed by routine rubella vaccination was proposed with an aim to eliminate CRS at the earliest through mass immunization of women (reproductive age group) and children (9 months–15 years) and to control rubella through universal vaccination of infants and young children thereby maintaining high immunization levels, and assuring high levels of immunity in women of child bearing age. This was recommended as the fastest method to eliminate CRS and was effectively implemented in Cuba and Malaysia.(15)
Fund for the immunization was mobilized followed by the formation of central and district level committees with representatives from the sectors, members of local religious body, and district and block development bodies. At the same time, the Ministry developed and distributed Information Education and Communication for Health (IEC) materials and engaged in micro planning the mass immunization.
Cold chain facilities were assessed, refurbished, and replenished. Estimates of vaccine and consumables made, procured, and distributed accordingly.
The campaign
The campaign was carried out for 5 consecutive days (between 16th to 26th March 2006). This involved a total of 1,495 immunization posts. The first 2 days focused entirely on school children and the next three days (with a gap of 5 days) for the remaining target population in pre-determined posts. A group of international observers monitored the immunization activity.
Coverage
A total of 332,041 individuals were immunized with MR vaccine against an enumerated target of 338,760. The overall coverage of the campaign was 98.17% [Figure 1].
Figure 1.
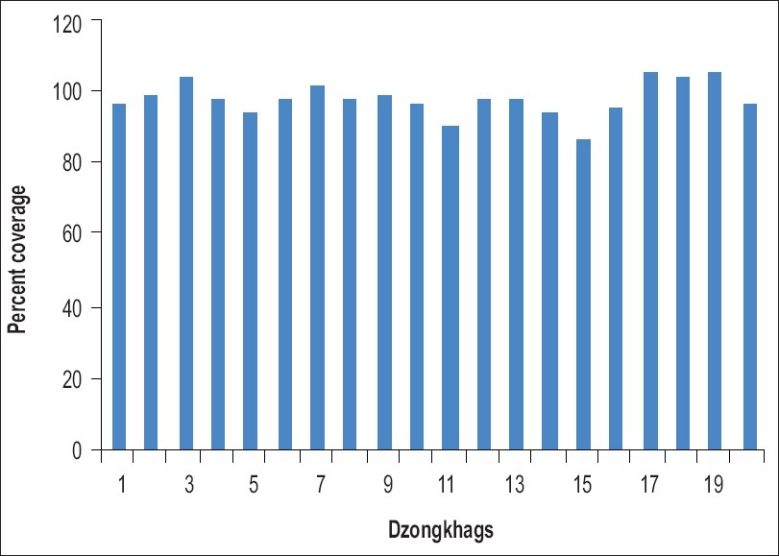
Immunization coverage of 20 districts (Dzongkhags)
Rapid convenient assessments of twenty house hold cluster was conducted immediately after the campaign. The assessments revealed coverage of 98 to 99% in children and 93 to 97% in women. The main reasons of non-receipt of vaccine in children were sicknesses, while it was pregnancy in women.
Vaccine wastage was minimal of 5.5%. It ranged between 2.9% and 16.2% in different districts. Maximum wastage was reported from those districts that had lesser and scattered population.
Adverse event following immunization
All vaccines were detained for 30 minutes following immunization. No anaphylaxis was reported from any vaccination post. Headache, fever, and body ache were the commonest complaints (55%) followed by pain at injection site (24%), nausea, and joints pain among those who complained. Hysterical reactions in girls were reported from several posts; however, they were all transient and recovered uneventfully. There was no report of encephalopathy or aseptic meningitis. No death was reported. All AEFI cases recovered without squeal.
Discussion
Relying on Bhutan's strengths of well distributed health facilities and past experiences of conducting mass immunization, measles rubella mass immunization campaign was the most pragmatic approach to control rubella and eliminate CRS in the shortest possible time.
Preparation for the campaign embraced a bottom up approach. The key to the success of the campaign were an accurate estimate of the target population, good grass root level planning, commitment of health workers, efficient vaccine delivery, high quality immunization services, good social mobilization, public support, and strong political will.
There are two important caveats to routine infant rubella immunization; to ensure that the child bearing population is protected against rubella and to maintain a high coverage of rubella vaccination indefinitely. Failure to maintain rubella vaccine coverage above 80% can result in an increase in the incidence of CRS on the long term.(16)
Following the campaign, monovalent measles vaccine in vogue was replaced with combined MR vaccine. Further, keeping Bhutan's commitment to the international goal of measles elimination, a booster dose of MR was recommended to be administered routinely to every child at 24 months. Additional efforts such as surveillance, continuing IEC, and availability of vaccine are required to sustain high rubella coverage to avert breakthrough epidemics.
Comparison with similar campaigns
In the United Kingdom, all children 5 – 16 year were offered MR vaccine in November 1994. The campaign was carried out through schools. Coverage of 90% was achieved.(17) In New Zealand, MR immunization was carried out in schools and in the community with a coverage of 56–85%.(18) Albania carried out a nationwide immunization campaign in November 2000 that included children 1-14 years of age with a coverage of 99%.(19) Similarly, Hong Kong Special Administrative Region carried out a mass immunization campaign with MMR in 1997, covering children between 1–19 years of age. The overall coverage was 77% with highest coverage of 90% in 6-11 years age group, 65% coverage in 1–5 years, and 74% in 12–19 years group.(20)
All these campaigns achieved a high coverage; however, none included women of reproductive age. The Bhutan campaign covered children of wider age range of 9 months to 15 years and reproductive age women 15 to 44 years achieving a very high coverage. This was done to maximize immunization coverage for rubella and to lead towards measles elimination.
It was once again demonstrated that despite limited resources, with strong political commitment and efficient planning and coordination, public health campaigns of such magnitude can be successfully implemented.
Impact of rubella immunization
Zero reporting of all febrile rash cases in up to 15 years of age along with mandatory serology for rubella and measles was introduced following the campaign. IgM positive rate for rubella has progressively declined for 2007 and 2008 reaching an all time low of 1.4% for the later. One sample tested positive for rubella and two for measles out of 36 samples collected in 2009 and 3.3% for 2010 [Figure 2].
Figure 2.
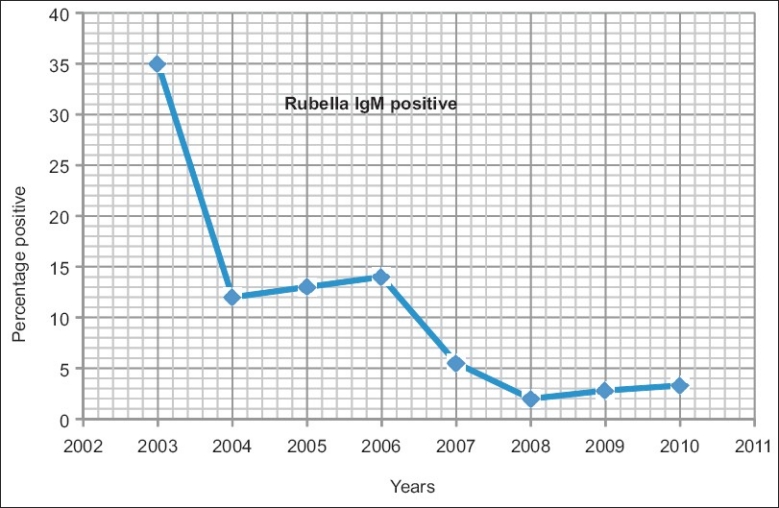
IgM positive rates in febrile rash cases
Febrile rash cases has decreased significantly to an average of 63 (range 52 to 67) each year from 399 (range 148–683) before the campaign. The proportion of measles positive among febrile rash has increased from 3 to 3.7% in 2003 to 2006 to 10 to 20% between 2007 and 2010. This could possibly be due to a significant drop in the cases of rubella and a decrease in total case load with similar basal measles transmission rates.
No new case of congenital rubella syndrome was reported from any hospital.
Striving towards measles elimination
Although the campaign was targeted controlling rubella and eliminating CRS, the goal of measles elimination was always kept in mind. Since the WHO has set the goal in the regions of the Americas, the Eastern Mediterranean, and Europe,(21–23) it is prudent that other countries follow suit.
Measles elimination is the interruption of transmission of measles in a sizeable geographical area in which vaccination would nevertheless need to continue because of the continued threat of reintroduction of the virus. The WHO and UNICEF have recommended, that a “second opportunity” for measles and rubella immunization be provided to all children through routine immunization.(23)
Immunization was initiated in Bhutan in 1979 with six antigens, measles, being one of them. The first 30 cluster coverage survey in 1990 ascertained measles coverage of 93% (95% CI, 83%–100%). Subsequent survey in 2002 established enhanced measles coverage of 96% (95% CI, 86%–100%). Measles mass immunization campaign was carried out nationwide in1995 and 2000 with an achievement of more than 99% coverage. The joint WHO and UNICEF review of immunization in July 2009 has revealed coverage of 99% for measles.(24)
It is pertinent that Bhutan maintains very high measles immunization coverage. Two doses of MR vaccination is mandatory requirement for the child's school entry which further ensures that these are received by six years of age.
Conclusion
Bhutan is one among the very few countries in the region that have championed mass MR immunization of children and women of child bearing age. This will limit circulating rubella virus in communities and decrease or eliminate CRS. Surveillance of CRS must be initiated at all health centers, screening all newborn and zero reporting. Periodic sero-surveillance of ante-natal mothers must be performed to study susceptibility of rubella infection. The campaign has doubly strengthened Bhutan's efforts towards measles elimination.
Early awareness gave enough opportunity to the target population for informed decision making. Meticulous bottom up micro-planning and good IEC coverage were some effective tools for the communities to garner ownership of such program. High commitment at all levels, appropriate training of manpower, clear policy, and operational guidelines were other important key to success of the program.
Footnotes
Source of Support: This article is a description of a public health activity. The source of funding was inbuilt in the project, supported by the UNICEF, WHO, HealthTrust Fund, Bhutan and the Royal Government of Bhutan. It did not require separate source of funding
Conflict of Interest: None declared.
References
- 1.Year Book.National Statistical Bureau, Royal Government of Bhutan. 2001:13–7. [Google Scholar]
- 2.Thimphu: PHD, Department of Health Services, Ministry of Health and Education; 2003. Public Health Division, National EPI Services Manual; pp. 8–10. [Google Scholar]
- 3.Annual health report. Thimphu: Ministry of Health and Education; 2001. Health Division; pp. 26–8. [Google Scholar]
- 4.Oliveria SA, Siqueria MM, Camacho LA, Nogueira RM, Spinetti CC, Cubel-Garcia RC, et al. The aetiology of maculopapular rash disease in Niteroi, State of Rio de Janerio, Brazil: implications for measles surveillance. Epidemiol Infect. 2001;127:509–16. doi: 10.1017/s0950268801005908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Behrman RE, Kliegman RM, Jenson HB. 17th ed. Philadelphia: WB Saunders Company; 2003. Nelson Textbook of Paediatrics; p. 1035. [Google Scholar]
- 6.Cutts FT, Robertson SE, Diaz-Ortega JL, Samuel R. Control of rubella and congenital rubella syndrome (CRS) in developing countries: Part1.Burden of disease from CRS. Bull World Health Organ. 1997;75:55–68. [PMC free article] [PubMed] [Google Scholar]
- 7.Robertson SE. Report on Rubella and CRS in Bhutan, WHO, Vaccines and Immunologicals. 2004 [Google Scholar]
- 8.Eckstein M, Vijayalakshmi P, Killedar M, Gilbert C, Foster A. Aetiology of childhoodcataract in south India. Br JOphthalmol. 1996;80:628–32. doi: 10.1136/bjo.80.7.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kommu R, Chase H. Washington, USA: PAHO; 1998. Follow up of rubella issues and costing of CRS in Barbados. Final report of the fourth meeting of the English speaking Caribbean EPI Managers, Castries, Saint Lucia, 18-20 November 1997. [Google Scholar]
- 10.Hinman AR, Irons B, Lewis M, Kandola K. Economic analyses of rubella and rubella vaccines: Aglobal review. Bull World Health Organ. 2002;80:264–70. [PMC free article] [PubMed] [Google Scholar]
- 11.Thimphu: Public Health division, Ministry of Health; 2004. Technical core group. Report of the Retrospective study on burden of rubella and CRS in Bhutan. March 2004. [Google Scholar]
- 12.Annual Health Conference; Ministry of Health, Royal Government of BhutanRecommendations. 2004 Apr;:21. [Google Scholar]
- 13.Appraisal report on Rubella, Public Health Laboratory, Department of Public Health, Ministry of Health. 2004 Mar [Google Scholar]
- 14.Robertson SE. Report on Rubella and CRS onvisit to Bhutan,14-26. 2004 [Google Scholar]
- 15.Robertson SE, Cutts FT, Samuel R, Diaz-Ortega JL. Control of Rubella and congenital rubella syndrome (CRS) in developing countries, Part 2: Vaccination against rubella. Bull World Health Organ. 1997;75:69–80. [PMC free article] [PubMed] [Google Scholar]
- 16.Ions B, Lewis MJ, Dhal-Regis M, Castillo-Solórzano C, Carrasco PA, de Quadros CA. Strategies to eradicate rubella in English speaking Caribbean. Am J Public Health. 2000;90:2545–9. doi: 10.2105/ajph.90.10.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gay N, Ramsay M, Cohen B, Hesketh L, Morgan-Capner P, Brown D, et al. The epidemiology of measles in England and Wales since the 1994 vaccination campaign. Commun Dis Rep CDR Rev. 1997;7:R17–21. [PubMed] [Google Scholar]
- 18.Mansoor O, Blakely T, Baker M, Tobias M, Bloomfield A. A measles epidemic controlled by immunization. N Z Med J. 1998;111:467–71. [PubMed] [Google Scholar]
- 19.Bino S, Kakarriqi E, Xibinaku M, Ion-Nedelcu N, Bukli M, Emiroglu N, et al. Measles-rubella mass immunization campaign in Alabania, November 2000. J Infect Dis. 2003;187(Suppl 1):S223–9. doi: 10.1086/368055. [DOI] [PubMed] [Google Scholar]
- 20.Chuang SK, Lau YL, Lim WL, Chow CB, Tsang T, Tse LY. Mass measles immunization campaign: Experience in the Hong Kong Special Administrative Region of China. Bull World Health Organ. 2002;80:585–91. [PMC free article] [PubMed] [Google Scholar]
- 21.Gay NJ. Eliminating measles-no quick fix. Bull World Health Organ. 2000;78:949. [PMC free article] [PubMed] [Google Scholar]
- 22.Center of Disease Control and Prevention, Global Control and Regional Elimination 1998-1999. CDC Morbidity and Mortality Weekly Report (MMWR) 1999;48:1124–30. [PubMed] [Google Scholar]
- 23.Center of Disease Control and Prevention, Epidemiology of Measles-United States, 1998. CDC Morbidity and Mortality Weekly Report (MMWR) 1999;48:749–53. [PubMed] [Google Scholar]
- 24.Report on WHO/UNICEF review of immunization in Bhutan from 1980 to 2008. 2009 Jul;:5–8. [Google Scholar]


