Abstract
Background & objectives:
Diabetic foot ulcers are the most common cause of non-traumatic lower extremity amputations in developing countries. The aim of this pilot study was to evaluate the safety of using a polyherbal formulation in healing diabetic foot ulcers in comparison with standard silver sulphadiazine cream among patients with type 2 diabetes.
Methods:
A total of 40 (M:F=29:14) consecutive type 2 diabetes patients with foot ulcers were enrolled in this study. They were randomly assigned to two groups of 20 each; Group 1 was treated with polyherbal formulation and group 2 with silver sulphadiazine cream. All the patients were followed up for a period of 5 months. The baseline ulcer size was noted and photograph of the wound was taken at the baseline and at each follow up visit. Number of days taken for healing of the wound was recorded.
Results:
The mean age of patients, duration of diabetes and HbA1c% were similar in both the study groups. The mean length and width of the ulcers was also similar in both the groups at baseline visit. There was a significant decrease in the size of the wound (length and width) in both the study groups (P<0.001). The mean time taken for the healing of the ulcer was around 43 days in both groups.
Interpretation & conclusions:
Diabetic wound cream prepared by using polyherbal formulation was found to be effective as well as safe in healing diabetic foot ulcers like the standard silver sulphadiazine cream.
Keywords: Diabetic foot ulcers, polyherbal formulation, treatment, type 2 diabetes
Type 2 diabetes is a chronic disorder and its prevalence is projected to increase globally. The increasing prevalence of type 2 diabetes and its complication are among the most serious public health concerns around the world. Developing countries, especially India, face a major problem due to high prevalence of diabetes1. Diabetic foot disease is the most significant complication of diabetes and it is a common cause of non-traumatic lower extremity amputations in the industrialized world. Foot infection is a leading cause for hospital admission among diabetes patients in India2,3. The risk of lower extremity amputation is 15 to 46 times higher in diabetes patients than in persons who do not have diabetes4,5.
Foot ulceration is a disabling complication of diabetes, and the lifetime risk of a person with diabetes developing this complication may be as high as 25 per cent6. The most frequent underlying aetiologies are neuropathy, trauma, deformity, high plantar pressures and peripheral arterial disease7. More than 80 per cent of amputations in patients with diabetes are preceded by non-healing foot ulcers8.
Wound may be produced by physical, chemical, thermal, microbial or immunological insult to the tissue. Diabetic foot wounds are defined as any break in the cutaneous barrier, usually extending through the full thickness of the dermis9. There have been different methods for infection control and treatment of diabetic foot ulcers. Their main goal is to accelerate the wound healing and tissue repair. The process of wound healing consists of integrated cellular and biochemical events leading to reestablishment of structural and functional integrity with regain of strength of injured tissue.
Various herbal products have been used in the management and treatment of wounds over the years. Many substances like tissue extracts10, vitamins and minerals and a number of plant products11 have been reported to possess pro-healing effects. Wound healing herbals encourage blood clotting, fight infection and accelerate the healing of wounds. The aim of this pilot study was to evaluate the safety of using a polyherbal formulation cream in promoting the healing of diabetic foot ulcers in comparison with the standard silver sulphadiazine cream among type 2 diabetes patients.
Material & Methods
This study was a uni-centre, open label, phase III, comparative study. Consecutive type 2 diabetes patients who presented with an ulcer up to Wagner's grade III classification12 (Grade I, superficial ulcer; grade II deep ulcer probing to tendon, capsule or bone; grade III deep ulcer with abscess, osteomyelitis or joint sepsis;) were enrolled in this study at Diabetes Research Centre, Chennai, between August 2008 and February 2009. Subjects who had clinical signs of severe infection, wound that had exposed bone and unwillingness to participate in the study were excluded. The study protocol was approved by the ethics committee of the institution. The patients were fully informed regarding the composition of the cream and its role in treating infection. All the study participants gave written informed consent.
Active ingredients of diabetic wound care cream: (Polyherbal formulation):
Glycyrrhiza glabra 0.20 per cent (Yastimadhu Athimathuram) - It improves normal cell multiplication in a wound and in combination with ketaki and Shorea robusta (kumkilium) it forms a fine protective layer over the wound, accelerating the growth of normal tissue, which gets absorbed into the tissue later.
Musa paradisiaca 19.42 per cent (Kadali vazhaikilangu Kadali) - It tightens the open wound, reduces the wound area and accelerates wound healing. It also reduces the kelloid growth and accelerates the normal tissue growth.
Curcuma longa 2.43 per cent (Manjal turmeric) - It possess anti-inflammatory activity, antiseptic and helps in wound healing. It effectively controls normalcy of tissue glucose level in the wound area. It helps in the natural repair of micro vascular structure.
Pandanus odaratissimus 9.70 per cent (Thazhai / Chevuda Ketaki) - This contains natural fibres with microcrystalline calcium embedded in it which forms foundation layer for the tissue growth like natural fibrogen network over which normal dermal layer can grow.
Aloe vera 4.85 per cent (Sothukathazhai) - It increases the cytogenesis, cleanses the wound and controls the tissue glucose level. Various constituents of aloe vera have been shown to have anti-inflammatory activity as well as it stimulates the wound healing.
Cocos nucifera oil (Kera thailam, coconut milk) - It supplies nutrition and polysaccharides and enhances the growth of the tissue.
A total of 40 (M: F=26:14) patients with type 2 diabetes were randomly assigned into two groups: group 1 (n=20) was treated with diabetic wound cream (a polyherbal formulation prepared by Cholayil Product and Services, Chennai, India); group 2 (n=20) was treated with silversulphadiazine cream. The enrollment of the subjects was done after the debridement of the ulcer. The polyherbal formulation cream had various constituents having antimicrobial, anti-inflammatory properties. Cream was employed in the treatment owing to its assured safety and efficacy.
Age and duration of diabetes was recorded for all patients. HbA1c % was estimated by immunoturbidimetric method13. The diagnosis of lower-extremity vascular insufficiency was made clinically on the basis of absence of both pedal pulses of the involved foot and/or an ankle-brachial pressure index of <0.914. Neuropathy was diagnosed by vibration perception threshold (VPT)15 and a value of >25 V was considered as abnormal. The anatomic location of the wound, tissues and vascular status was recorded for all the patients. All the patients were followed for a period of 5 months.
The baseline ulcer size was between 2-50 cm2. The ulcer tracing was done for each patient in a sterile acetate sheet. The photographs of the wound was taken at the baseline i.e., before the application of the cream and at each follow up visit. The ulcers greatest length and width was measured at baseline and follow up. Patients were initially seen in the diabetic foot clinic on a weekly basis and were provided with the best possible care for their ulcers at each visit. Broad spectrum antibiotics were prescribed if ulcers showed clinical signs of infection. The dressings were changed daily after a wash with normal saline followed by the local application of the diabetic wound cream or silver sulphadiazine cream as a thin layer. Patients were advised to do dressing daily, either in the out patient clinic of our hospital or nearby local hospital or with the aid of the community nurse who provides home care for patients with ambulatory problems.
Duration of ulcer before enrollment in the study and the number of days taken for healing of the wound were recorded. Offloading of the wounds was done by standard method in both the groups. Clinical outcome was documented as a part of routine practice. Healing was defined as complete epithelialization either by secondary intention or by split skin graft.
Statistical analysis: SPSS package (version 10.0) was used for doing statistical analysis. Mean±SD for continuous variables and proportions were reported as relevant. Student's ‘t’ test, Chi-square test and Friedman's non parametric repeated measures comparison were used to test the significance, and P<0.05 was considered significant.
Results
Of the 40 patients enrolled in this study, 38 adhered to the protocol (group 1; n=19 and group 2; n=19). One patient in group 1 was excluded from the study because of severe infection and one patient in group 2 died during the study period (unrelated cause). The follow up period in both the groups was five months. There were no adverse events reported in both the groups.
All the study patients had the presence of neuropathy. More than 60 per cent of patients had plantar forefoot ulcers in both the study groups. There was no significant difference in the location of the wound between the groups. The distribution of ulcers according to Wagner's grade was also similar in both the study groups. Wagner grade I and II foot ulcers were viable and grade III ulcers were non-viable tissues. Ulcers with abscess had foul odour. Presence of osteomyelitis and peripheral arterial disease among the study patients was similar in both the groups. Duration of ulcer before enrollment in the study did not differ between the groups (Table I). Age and duration of diabetes was similar in both the groups. HbA1c% was also similar in both the groups (Table II). Table III shows the details of size of the wound at baseline and during follow up visits (after one, 3, 5 months). The mean length of the wound and mean width was similar between the groups at baseline. There was a significant decrease noted in the size of the wound viz., length and width in both the study groups at follow up visit (P<0.001). The healing of wound and the decrease in wound size was shown in the Fig. (Panel a; group 1, Panel b; group 2). Number of days taken for healing of the wound was similar in both the groups. The mean time taken for the healing of the wound was around 43 days in both the groups. There was no significant difference in healing time between the study groups. Recurrence of ulcers was similar in both the groups.
Table I.
Details of foot ulcers at baseline and presence of peripheral arterial disease among the study groups
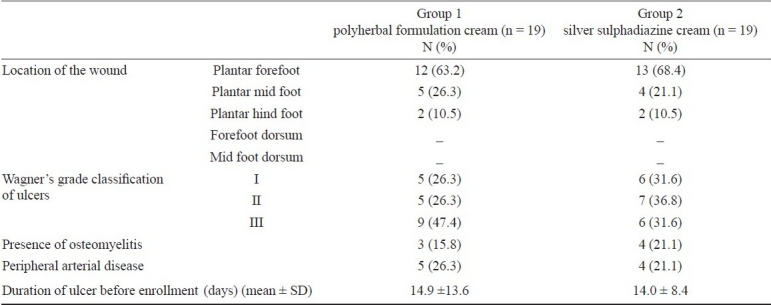
Table II.
Characteristics of the study groups
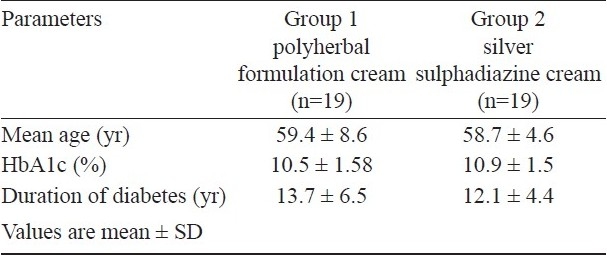
Table III.
Length and width of the wound at the baseline and during follow up visits in each group
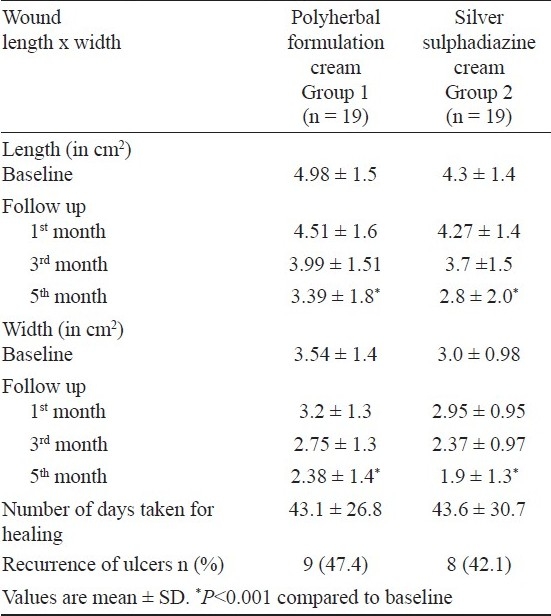
Fig.
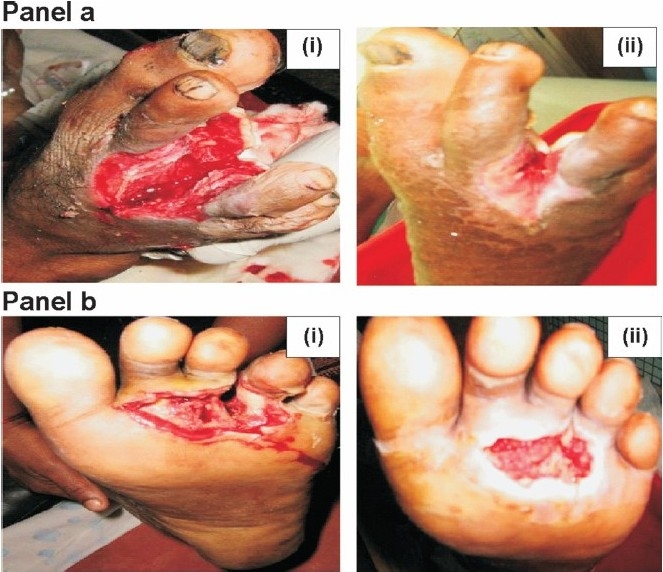
Panel a: Wound healing in the group 1. (i) Pre application of the polyherbal cream (ii) 28th day of application Panel b: Wound healing in group 2 (i) Pre application of the silver sulphadiazine cream (ii) 29th day of application.
Discussion
Wound healing is a complex process that involves expression of growth factors that promote various cellular processes, production of new connective tissue matrix and collagen deposition16. This process is delayed in diabetes patients due to vascular insufficiency and decreased blood flow17,18. Various methods have been used for promotion of wound healing. Recent clinical trials proved that herbal extracts are also safe and effective for treatment of diabetic foot ulcers19,20. The results of the present study showed that diabetic wound care cream prepared by using polyherbal formulation was found to be effective as well as safe in healing of diabetic foot ulcers. The healing process of the wound with polyherbal formulation cream in diabetic foot ulcers was similar when compared with subjects treated with silver sulphadiazine cream. There was a significant decrease in wound size in both the study groups.
Evidence showed that healing progression at 2nd to 4th wk predicts eventual wound closure17,21. Our study showed that time taken for healing of wound was approximately 43 days in both the herbal cream treated versus silver sulphadiazine cream treated subjects. The healing process was similar in both the study groups. It has been reported that a herbal drug named ANGIPARS (daily intravenous infusion) was effective in treating diabetic foot ulcers without any adverse side effects. The wound size was reduced 50 per cent during a 8 wk period22.
It has been proved that silver has bactericidal action against a number of microorganisms. In the last few years, a number of silver- containing dressings have been developed and used to treat acute and chronic wounds23. In the first randomized controlled trial of silver dressings in diabetic foot ulcers, 134 patients with neuropathic foot ulcers were randomly assigned to either Aquacel Ag (AQAg; ConvaTec, Chester, UK) or Algosteril calcium alginate (CA) (Smith & Nephew, Hull, UK) dressings and a secondary foam dressings. The mean time to healing was 53 days in the AQAg-treated ulcers and 58 days for the CA treated ulcers. Ulcers treated with AQAg, however, showed greater depth reduction than CA-treated ulcers24. The polyherbal formulation cream used in this study showed similar effects compared to silver containing cream treated subjects with diabetic foot ulcers.
The herbal formulation cream used in this study contains Glycyrrhiza glabra, Musa paradisiaca, Curcuma longa, Pandanus odaratissimus, Aloe vera and Cocos nucifera oil ingredients of plant origin. These ingredients are known to possess anti-inflammatory and anti-bacterial action. Polyherbal preparations containing Glycyrrhiza glabra have been reported to promote gain in tensile strength in incision wound model, but do not modify the granulation phase of healing25. Curcumin (difeurloylmethane) from curcuma rhizomes showed faster closure of wounds and increased collagen, TGF-b1 and fibronectin in animal studies26. Curcuma longa also contains protein, fats, vitamins all of which have an important role in would healing and regeneration. The anti-inflammatory property and the presence of vitamin A and proteins result in the early synthesis of collagen fibres27. Aloe vera has been historically used for many of the same conditions for which it is used today–particularly minor cuts and burns. Test tube studies suggest polysaccharides, such as acemannon, help promote skin healing by anti-inflammatory, antimicrobial, and immune-stimulating actions. Aloe's effects on the skin may also be enhanced by its high concentration of amino acids, as well as vitamin E, vitamin C, zinc, and essential fatty acids28. The daily application of polyherbal cream with all the above ingredients may promote wound healing in diabetes patients with foot ulcers. Usage of this cream is not cumbersome and it does not involve complicated dressing procedures. Diabetes is a major public health problem in developing countries and is associated with high costs of treating diabetic foot problems. So, usage of this cream may have an impact on treatment of diabetes foot ulcers in India.
There were a few limitations in the present study. First, the small sample size, secondly the microbiological investigations were not done. The prolonged use of the herbal cream which may have beneficial or probable side effects was not assessed. Lastly, this study was not a randomized clinical trial.
In conclusion, daily application of polyherbal cream could reduce the wound size significantly approximately in a mean period of 6 wk without any adverse side effects. The polyherbal cream may be effective in treating diabetic foot ulcers along with current standard care. It may be an alternative to silver sulphadiazine cream used in healing diabetic foot ulcers. It must however, be stressed that good wound care practices including sharp debridement, infection control and offloading play an important role in healing a diabetic foot ulcer.
Acknowledgments
The authors thank Cholayil Product and Services, Koyambedu, Chennai, India for providing the polyherbal cream with their formulation.
Footnotes
Conflict of Interest: None.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Time of act: diabetes and foot care. Brusseles: International Diabetes Federation; 2005. International Diabetes Federation; pp. 1–198. [Google Scholar]
- 3.Vijay V, Snehalatha C, Ramachandran A. Socio-cultural practices that may affect the development of the diabetic foot. IDF Bull. 1997;42:10–2. [Google Scholar]
- 4.Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. 1996;19:48–52. doi: 10.2337/diacare.19.1.48. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong DG, Lavery LA, Quebedeaux TL, Walker SC. Surgical morbidity and the risk of amputation due to infected puncture wounds in diabetic versus non-diabetic adults. South Med J. 1997;90:384–9. doi: 10.1097/00007611-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–28. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- 7.Frykberg RG, Armstrong DG, Giurini J, Edwards A, Kravette M, Kravitz S, et al. Diabetic foot disorders: A clinical practice guideline.American College of Foot and Ankle Surgeons. J Foot Surg. 2000;39(Suppl 5):51–60. [PubMed] [Google Scholar]
- 8.Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation: basis for prevention. Diabetes Care. 1990;13:513–21. doi: 10.2337/diacare.13.5.513. [DOI] [PubMed] [Google Scholar]
- 9.Cianci P. Consensus Development Conference on Diabetic Foot Wound Care: a randomized controlled trial does exist supporting use of adjunctive hyperbaric oxygen therapy. Diabetes Care. 2000;23:873–4. doi: 10.2337/diacare.23.6.873. [DOI] [PubMed] [Google Scholar]
- 10.Udupa SL, Shaila HP, Udupan AL, Ramesh KV, Kulkarni DR. Wound healing properties of some medicinal plants. Biochem Arch. 1991;7:207–12. [Google Scholar]
- 11.Dahanukar SA, Kulkarni RA, Rege NN. Pharmacology of medicinal plants and natural products. Indian J Pharmacol. 2000;32:S81–118. [Google Scholar]
- 12.Wagner FW. The dysvascular foot: a system of diagnosis and treatment. Foot Ankle. 1981;2:64–122. doi: 10.1177/107110078100200202. [DOI] [PubMed] [Google Scholar]
- 13.Hamwi A, Schweiger CR, Veitl M, Schmid R. Quantitative measurement of HbA1c by an immunoturbidemetric asssay compared to a standard HPLC method. Am J Clin Pathol. 1995;104:89–95. doi: 10.1093/ajcp/104.1.89. [DOI] [PubMed] [Google Scholar]
- 14.Apelqvist J, Castenfors J, Larsson J. Prognostic value of ankle and toe blood pressure levels in outcome of diabetic foot ulcers. Diabetes Care. 1989;12:373–8. doi: 10.2337/diacare.12.6.373. [DOI] [PubMed] [Google Scholar]
- 15.Young MJ, Breddy JL, Veves A, Boulton AJM. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds: a prospective study. Diabetes Care. 1994;17:557–60. doi: 10.2337/diacare.17.6.557. [DOI] [PubMed] [Google Scholar]
- 16.Wilte MB, Barbul A. General principles of wound healing. Surg Clin North Am. 1997;77:509–28. doi: 10.1016/s0039-6109(05)70566-1. [DOI] [PubMed] [Google Scholar]
- 17.Sheehan P, Jones P, Caselli A, Giurini JM, Veves A. Percent change in wound area of diabetic foot ulcers over a 4 weeks period is a robust predictor of complete healing in a 12 week prospective trial. Diabetes Care. 2003;26:1879–82. doi: 10.2337/diacare.26.6.1879. [DOI] [PubMed] [Google Scholar]
- 18.Goodson WH, Hunt TK. Studies of wound healing in experimental diabetes mellitus. J Surg Res. 1977;22:221–7. doi: 10.1016/0022-4804(77)90137-8. [DOI] [PubMed] [Google Scholar]
- 19.Singh SK. Role of combination of multiple herbal drugs (Septilin) in the prophylaxis of diabetic foot ulcer – A double blind trial. Indian J Dermatol. 2001;46:83–5. [Google Scholar]
- 20.Larijani B, Heshmat R, Bahrami A, Delshad H, Ranjbar OG, Mohammed K, et al. Effects of intravenous semelil (ANGIPARS™) on diabetic foot ulcers healing: a multicentric clinical trial. DARU. 2008;6(Suppl 1):35–40. [Google Scholar]
- 21.Kantor J, Margolis DJ. A multicentre study of percentage change in venous leg ulcer area as a prognostic index of healing at 24 weeks. Br J Dermatol. 2000;142:960–4. doi: 10.1046/j.1365-2133.2000.03478.x. [DOI] [PubMed] [Google Scholar]
- 22.Masoompour SM, Bagheri MH, Borhani Haghighi A, Novitsky YA, Sadeghi B, Gharibdoust F, et al. Effect of ANGIPARS™, a new herbal drug on diabetic foot ulcer: A phase 2 clinical study. DARU. 2008;16(Suppl 1):31–4. [Google Scholar]
- 23.White RJ, Cutting K, Kingley A. Topical antimicrobial in the control of wound bioburden. Ostomy Wound Manage. 2006;52:26–58. [PubMed] [Google Scholar]
- 24.Jude EB, Apelqvist J, Spraul M, Martini J. Prospective randomized controlled study of hydro fiber dressing containing ionic silver or calcium alginate dressings in non ischemic diabetic foot ulcers. Diabet Med. 2007;24:280–8. doi: 10.1111/j.1464-5491.2007.02079.x. [DOI] [PubMed] [Google Scholar]
- 25.Udupa SL, Rao SG, Kulkarni DR. Wound healing profile of septilin. Indian J Physiol Pharmacol. 1989;33:1–5. [PubMed] [Google Scholar]
- 26.Sidhu GS, Singh AK, Thaloor D, Banaudha KK, Patnaik GK, Srimal RC, et al. Enhancement of wound healing by curcumin in animals. Wound Repair Regen. 1998;6:167–77. doi: 10.1046/j.1524-475x.1998.60211.x. [DOI] [PubMed] [Google Scholar]
- 27.Kumar AS, Singh HP, Prakash P, Singh SP. Efficacy of some indigenous drugs in tissue repairs in buffaloes. Indian Vet J. 1993;70:42–4. [Google Scholar]
- 28.Jia Y, Zhao G, Jia J. Preliminary evaluation: The effects of Aloe ferox Miller and Aloe arborescens Miller on wound healing. J Ethnopharmacol. 2008;120:181–9. doi: 10.1016/j.jep.2008.08.008. [DOI] [PubMed] [Google Scholar]


