Abstract
Objective
The purpose of this study was to evaluate the association of household income and formal education with risk of mortality after spinal cord injury (SCI).
Design
Cohort Study
Setting
Twenty hospitals designated as Model SCI Systems of care in the United States.
Participants
8,027 adults with traumatic SCI, seen in one of the Model SCI Systems, who had at least one follow-up assessment between 1995 and 2006. All participants were at least 1 year post-injury at the time of assessment. There were 57,957 person-years and 1,036 deaths. The follow-up period started with the first assessment between 1995 and 2006 and went until either the date of death or March 2009.
Interventions
not applicable.
Main Outcome Measures
Mortality status was determined by routine follow-up supplemented by using the Social Security Death Index. A logistic regression model was developed to estimate the chance of dying in any given year.
Results
Educational status and income were significantly predictive of mortality after adjusting for age, sex, race, and severity of injury. Compared to those with household income of $75,000 or greater, the odds of mortality was greater for who have income between $25,000–$75,000 (1.61) and still higher for those with less than $25,000 per year (2.41). Life expectancy differed more as a function of household income than the economic subscale of the Craig Handicap Assessment and Reporting Technique.
Conclusion
There was a clear gradation in survival based on familial income (high, middle low), not just an effect of the lowest income.
Keywords: spinal cord injury, mortality, risk, economics, income, life expectancy
Spinal cord injury is associated with elevated risk of premature mortality.1–3 Although the majority of research on mortality after SCI has historically focused on biographic and injury characteristics (e.g., age, sex, race, cause of injury, level of injury, neurologic completeness of injury, ventilator dependency), recent studies have included analysis of a wider array of predictive factors, including economic factors. These may be important to consider because they may serve as proxy variables for access to health care, assistance with activities of daily living, and overall living conditions.
In an analysis of data from the MSCIS in the United States, several predictor variables representing each level of a theoretical risk model4 were found to be predictive of mortality.5 Accounting for these variables led to substantial elevations in life expectancy under favorable circumstances. Other than biographic and injury characteristics, the biggest contributors to increased annual mortality rates were: being hospitalized in the previous year (OR = 1.65), having a household income level at or below the poverty level (OR = 1.62), and having a grade 3 or 4 pressure ulcer at the time of entry into the study (OR = 1.55). Conversely, having workers compensation insurance (generally considered the most comprehensive type of insurance coverage) led to a reduction in annual mortality rates of 57%. Under a very favorable set of assumptions involving good health, community integration, family finances, and health insurance, life expectancy was substantially increased.
This study was replicated by Strauss et al6 using updated data from the MSCIS, but they presented only one hypothetical example of life expectancy for a 25 year old compared with the two examples provided in the initial study.5 Because the workers compensation variable was no longer statistically significant (although it did still represent a 20% annual reduction in mortality rates), they eliminated this variable and measured favorable economics by dividing CHART economic self-sufficiency scores into 3 groups, reflecting unfavorable (<50), average (50–75), and favorable economics (>75). They found under poor economic conditions, life expectancy dropped to 55% of normal and ranged to a high of 66% of normal under favorable economics. This figure was lower than that cited in the study by Krause, DeVivo, and Jackson5 assuming favorable economics and other factors cited above. The investigators concluded: “Our research provides further support for the very plausible hypothesis that those near the poverty level have shorter life expectancies than others. However, the study provides no evidence for or against [italics added] the proposition that those with large net incomes have better life expectancies than persons with adequate, though more modest, resources…”5
Other studies have more directly addressed the univariate relationship between income and risk of mortality using non-MSCIS data. For instance, Krause7 found that income less than $25,000 was associated with 4.51 times greater odds of mortality over a 4-year interval than those with incomes of $75,000 or greater. In a study utilizing the same data set, but over an eight year interval, Krause and Carter8 found that income was 1 of 2 significant environmental predictors of mortality when controlling for biographic and injury characteristics. They later developed a full model including predictive variables from all 4 levels of the theoretical risk model, and income was 1 of 7 non-biographic and non-injury factors significantly related to the mortality rate.9 Whereas these studies did not report life expectancy, a more recent analysis identified substantial differences in life expectancy when using familial income as a predictor.10
In summary, favorable economics have been linked to the risk of mortality after SCI in several studies using MSCIS data. However, studies using the CHART economic self-sufficiency score have low ceiling effects, as the highest group (scores 75–100) begins at 1.5 times the poverty-level. One study identified a significant relationship of familial income with life expectancy, but used a smaller data set derived from a single clinical setting.10 If a relationship between high income and mortality among persons with SCI can be validated using the larger MSCIS data, then we can not only improve the accuracy of life expectancy estimates but also provide additional evidence related to indirect benefits of interventions aimed at increasing the likelihood of employment for those who are capable of returning to work. Using household income, rather than CHART scores, will reduce the low ceiling effect and provide a more accurate assessment of the relationship between income and life expectancy.
Purpose
Our purpose was to utilize data from the MSCIS in the United States to evaluate the effect of education and 3 levels of household income on risk of mortality. We will use data on household income collected in the MSCIS starting in 1995 to address the relationship between income level and life expectancy in SCI.
METHODS
Participants
The NSCISC Database contains data reported from MSCIS rehabilitation hospitals around the United States since 1973. Institutional review board approval was obtained locally at each center prior to the collection of any data. Participants are recruited during acute care or inpatient rehabilitation after obtaining informed consent. Eligibility criteria for this study included being admitted to a MSCIS within 1 year of injury, having an SCI resulting from a traumatic event, residing within the geographic catchment area of the MSCIS, being discharged alive from rehabilitation with some residual neurologic deficit, and having data on household income collected at least once post-discharge beginning in 1995. Overall, 20 MSCIS hospitals located throughout the United States contributed data to this study.
Procedures
Data are collected on participants in the NSCISC Database during inpatient rehabilitation and at discharge, 1 year post-injury, 5 years post-injury, and at 5-year intervals thereafter. In addition, mortality was assessed annually through routine follow-up conducted by personnel at each MSCIS supplemented by searches of the SSDI and other on-line mortality databases such as obituary files and state death indexes, with the most recent searches conducted in March, 2009. The SSDI has been shown to have 94.2% sensitivity and 99.5% specificity in identifying mortality among persons in the NSCISC Database.11 Participants who were not found deceased were presumed to be alive, and their censoring date was the most recent of either the date of last contact or January 1, 2009. This results in a slight bias toward underestimating mortality among younger persons, females, African-Americans, and those who are not married since deaths among persons with these characteristics are the most likely not to be found in the SSDI.12
Measures
Beginning in November 1995 and terminating in 2006, annual household income level was measured at follow-up, and presented in the categories utilized in the BRFSS,13 a standardized instrument widely used by the Centers for Disease Control. These income levels were incorporated into the CHART economic self-sufficiency score.14 A cutoff score of $75,000 and greater was used to reflect high income, $25,000–74,999 middle income, and <$25,000 low income. Income is based on all sources from all members of the household, rather than the individual’s earnings alone (individual earnings data were not available). As we selected the first survey where income was measured, all measures used in this analysis come from that survey.
The CHART economic self-sufficiency score is a measure of economic hardship and accounts for household income while adjusting for out-of-pocket medical expenses and family size.14 While the scale is continuous (0–100), we categorized the levels by percentage above poverty, 0–50 represented at or below poverty level, 51–75 represents poverty-level to 50% above poverty level, and 76–100 represents 1.5 times poverty level and greater. Only post-injury household income was available.
Education was measured at the time of follow-up and was categorized as follows: less than a high school degree, high school degree or associate’s degree, and bachelor’s degree or more. Injury level was categorized as C1–C4, C5–C8, and non-cervical. Injury completeness was measured by either Frankel grade15 or AIS16 as the Frankel system was used until 1993, at which time it was switched to the AIS. Each Frankel grade was grouped with the corresponding AIS grade in our analyses. Other variables measured were gender, race, (African-American, other, white), current age, cause of injury, calendar year, and years since injury.
Analysis
For this analysis, the first annual evaluation containing valid income data was selected as the baseline from which subsequent mortality would be determined. Therefore, although participants might have been injured as early as 1973, no participant was enrolled in this study until November 1995. Any time post-injury that occurred before the measurement of household income was excluded from the analysis to avoid the bias that would occur by including that experience without also including patients who died before income data could be collected. The range of baseline annual evaluations used in this study (which equates to the first time household income was measured for each participant) was from first anniversary of injury to the 30th anniversary of injury. Only persons at least 18 years old at the time of baseline follow-up were included (those under 18 were not asked about household income and could not be included). Ventilator-dependent persons were also excluded due to the small sample size of such individuals. This resulted in a final sample size of 8,027 persons. All participants from the earlier studies by Krause et al5 and Strauss et al6 were included in these analyses, with additional data collected from new participants as well as longer follow-up of original participants. The number of participants increased 35.0% over the Krause et al5 study and 9.5% over the Strauss et al study.6
We used the first income assessment, as only 41.8% of participants had income data on more than one occasion. Of those with data on more than one occasion, 71.6% remained in the identical income category and 97.5% of these reported either the same income or changed by only one category. Among those whose income changed over time, 16.7% increased (1.4% by two categories) and 11.8% decreased (1.1% by two categories). Therefore, given the assessments were 5 years apart and the limited data on income change, there were not sufficient years of follow-up to include the second assessment.
We used logistic regression analysis with person-years data to assess the relationship between income and mortality. A person-year data set was constructed in which each person contributed one observation for each year of follow-up with the outcome of that year being either survival to the end of the year or death during the year. Therefore, a person enrolled in 1998 who died during the 7th follow-up year would contribute one observation each for years 1998 through 2003 with the outcome being categorized as alive, and one observation for 2004 with the outcome being categorized as deceased.
The person-year statistical method is longitudinal in nature and will produce results similar to those of a Cox proportional hazards model, with the difference decreasing as the unit of time decreases (from years to months to days). However, the person-year logistic regression approach has the advantage of more easily distinguishing the effects of current age, time post-injury and calendar year than a Cox model. Moreover, using person-years facilitates the calculation of life expectancy that is technically more cumbersome with a Cox model. This method has been used in previous studies of mortality after SCI.17
All potential risk factors were entered into the logistic regression model with backward elimination of those factors that were not statistically significant. Collinearity was assessed by examination of correlation coefficients among all the potential risk factors. No meaningful problems of multicollinearity were detected.
Biographic (age, gender, race) and injury characteristics (injury level and completeness, etiology) were included in the final model, along with household income and education. Years post-injury and calendar year were not significantly associated with the odds of dying, so these two factors were not included in the final regression model. Interaction terms were tested in the multivariable model, between the primary independent variable (income) and all other independent variables, and between SCI level and AIS/Frankel grade. There were no significant interactions with income, but the interaction between SCI level and AIS/Frankel grade was significant, and thus included in the final model. Previous research9 has shown mortality is similar for persons who are ambulatory or have AIS D injuries, regardless of injury level, so inclusion of an interaction term eliminates the effect of injury level on mortality for persons with AIS D injuries. An additional model was run with identical factors as shown above using the CHART economic self-sufficiency score with cutoffs previously used in the studies by Krause et al5 and Strauss et al6 in place of income.
Hosmer-Lemeshow and global χ2 tests were used to assess goodness-of-fit of the model.18 The C-statistic, measuring area under the Receiver Operating Characteristic curve, was used to assess discriminatory ability.18 Odds ratios with 95% CIs were calculated. Using the logistic regression model and statistical methods described previously, we calculated differences in life expectancy by income level for a 25- and 50-year-old white man with an AIS A injury resulting from a motor vehicle crash.19 For each example we also varied the level of injury (C4, C6, T7).
Relative mean differences in life expectancy were calculated as a function of the 3 income levels using expanded examples from the Krause et al5 and Strauss et al6 studies, with the base case being white, male, motor vehicle crash injury etiology, AIS A injury, and having a high school degree. The RMD was calculated as the difference between 2 life expectancies divided by their average [RMD=(A–B)/((A+B)/2)]. Separate calculations were made as a function of 3 different injury levels (C4, C6, and T7) and the same 2 age groups used in the previous studies (i.e., 25 years old, 50 years old). Estimates were also derived from the model using the CHART economic self-sufficiency score. RMDs were calculated using low income or CHART economic self-sufficiency score as the reference (i.e., middle vs. low or high vs. low income or CHART economic self-sufficiency scores), and the differences were interpreted as the percentage of increase in life expectancy for each level of income or CHART economic self-sufficiency score. We used 3 levels of the CHART economic self-sufficiency score, rather than treating it continuously, to be fully consistent with how this variable was treated in the preliminary studies of economics and life expectancy and because scores in excess of 100 cannot occur regardless of the actual income level.5–6
RESULTS
Of the 8,027 participants, there were 1,036 deaths occurring during the 57,947 person-years of follow-up. The mean length of time between injury date and study enrollment (collection of income data) was 7.7 (8.0) years. Of participants, 79.4% were male, 72.2% were white, 50.3% had a cervical injury, and 49.7% were complete injuries. There were differences in the mortality rate between income levels, with persons who reported a lower income having a higher mortality rate (Table 1). There were also significant differences in gender, race, etiology, SCI level, AIS/Frankel grade, age, and education. Education and income were correlated; however, each variable contributed to the final model, thus they both were included.
Table 1.
Characteristics of participants by mortality status.
| Patient Characteristic | Mortality | Person Years | Mortality Rate* |
|---|---|---|---|
| Gender | |||
| Female | 187 | 11899 | 15.72 |
| Male | 849 | 45012 | 18.86 |
| Race | |||
| White | 780 | 42613 | 18.30 |
| Black | 183 | 8970 | 20.40 |
| Other | 73 | 5328 | 13.70 |
| Etiology | |||
| MVC/Fl/Sp† | 796 | 44639 | 17.83 |
| Violence | 114 | 4451 | 25.61 |
| Other | 126 | 7821 | 16.11 |
| SCI Level | |||
| C1–C4 | 219 | 8940 | 24.50 |
| C5–C8 | 415 | 48909 | 21.95 |
| Non-cervical | 402 | 29062 | 13.83 |
| AIS/Frankel | |||
| A | 582 | 28362 | 20.52 |
| B | 127 | 6948 | 18.28 |
| C | 125 | 6710 | 18.62 |
| D/E | 202 | 14891 | 13.57 |
| Income | |||
| < $25,000 | 640 | 28463 | 22.49 |
| $25,000–$74,000 | 329 | 20834 | 15.79 |
| $75,000 + | 67 | 7614 | 8.80 |
| Education | |||
| Bachelors + | 167 | 13380 | 12.48 |
| High School/Associates | 648 | 35032 | 18.50 |
| < High School | 221 | 8499 | 26.00 |
| Current Year | |||
| 2005–2006 | 47 | 2711 | 17.34 |
| 2000–2004 | 306 | 16131 | 18.97 |
| 1995–1999 | 683 | 38069 | 17.94 |
| Years post-injury | |||
| 2 | 55 | 4307 | 12.77 |
| 3–4 | 93 | 5853 | 15.89 |
| 5–9 | 254 | 13593 | 18.69 |
| 10–19 | 311 | 18459 | 16.85 |
| 20–29 | 284 | 13273 | 21.40 |
| 30+ | 39 | 1429 | 27.29 |
per 1,000 person years
MVC/Fl/Sp =motor vehicle crash/fall/sports
Results of the multivariable logistic regression model are shown in Table 2. After inclusion of all variables from Table 1 and the interaction term between SCI level and AIS/Frankel grade, only etiology became non-significant. Both education and income remained significantly associated with mortality. Persons with low income (<$25,000) had 2.31 times the odds of mortality of persons with high income. Also, persons in the middle income category had 1.61 times the odds of mortality as the highest income group. Increasing education level was associated with lower odds of mortality, where persons with a bachelor’s degree or higher had 0.56 times the odds of mortality and persons with a high school or associate’s degree had 0.81 times the odds of mortality of persons with less than a high school degree.
Table 2.
Crude and adjusted odds ratios for mortality.
| Patient Characteristic | Crude | Adjusted* | Adjusted** |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | |||
| Gender (vs. Female) | |||
| Male | 1.20 (1.02–1.41) | 1.24 (1.05–1.46) | 1.25 (1.05–1.48) |
| Race (vs. Other) | |||
| White | 1.35 (1.05–1.70) | 1.32 (1.00–1.74) | 1.40 (1.07–1.83) |
| Black | 1.49 (1.13–1.96) | 1.45 (1.24–1.87) | 1.24 (0.92–1.67) |
| Etiology (vs. MVC/FL/Sp†) | |||
| Violence | 0.90 (0.75–1.09) | 1.11 (0.90–1.37) | 1.12 (0.89–1.40) |
| Other | 1.44 (1.18–1.75) | 1.20 (0.97–1.47) | 1.22 (0.98–1.51) |
| Age (vs. 18–34) | |||
| 35–39 | 1.77 (1.34–2.34) | 1.80 (1.36–2.39) | 1.78 (1.33–2.39) |
| 40–44 | 2.16 (1.66–2.80) | 2.27 (1.74–2.95) | 2.24 (1.71–2.95) |
| 45–49 | 2.83 (2.20–3.64) | 3.10 (2.40–4.00) | 3.13 (2.40–4.09) |
| 50–54 | 3.57 (2.75–4.63) | 4.18 (3.21–5.44) | 4.06 (3.08–5.36) |
| 55–59 | 4.13 (3.12–5.47) | 5.27 (3.96–7.01) | 5.33 (3.95–7.18) |
| 60–64 | 4.49 (3.28–6.14) | 5.82 (4.22–8.01) | 6.02 (4.32–8.39) |
| 65–69 | 7.44 (5.50–10.05) | 9.98 (7.33–13.60) | 10.51 (7.62–14.50) |
| 70–74 | 10.75 (7.78–14.67) | 15.14 (10.98–20.86) | 13.44 (9.50–19.02) |
| 75–79 | 15.11 (10.66–21.42) | 25.28 (17.57–36.37) | 25.45 (17.42–37.18) |
| 80+ | 19.14 (13.18–27.82) | 35.16 (23.70–52.14) | 32.85 (21.61–49.94) |
| SCI Level (vs. Non-cervical) | |||
| C1–C4 | 1.77 (1.50–2.09) | 2.52 (2.09–3.06) | 2.56 (2.09–3.12) |
| C5–C8 | 1.59 (1.38–1.82) | 2.05 (1.74–2.41) | 2.14 (1.81–2.54) |
| AIS/Frankel (vs. D/E) | |||
| A | 1.51 (1.29–1.78) | 1.81 (1.37–2.37) | 1.70 (1.28–2.26) |
| B | 1.35 (1.08–1.69) | 1.30 (0.94–1.80) | 1.27 (0.91–1.78) |
| C | 1.37 (1.10–1.72) | 1.08 (0.78–1.49) | 1.01 (0.72–1.41) |
| Income (vs. $75,000 +) | |||
| < $25,000 | 2.56 (1.98–3.29) | 2.31 (1.76–3.02) | 1.63 (1.39–1.91) |
| $25,000–$74,000 | 1.79 (1.38–2.34) | 1.61 (1.23–2.12) | 1.29 1.06–1.57) |
| Education (vs. < High School) | |||
| Bachelors + | 0.48 (0.39–0.59) | 0.56 (0.45–0.71) | 0.49 (0.39–0.62) |
| High School/Associates | 0.71 (0.61–0.83) | 0.81 (0.69–0.96) | 0.81 (0.68–0.97) |
| AIS D*SCI Level | |||
| C1–C4 + AIS D | 0.34 (0.22–0.52) | 0.32 (0.25–0.41) | |
| C5–C8 + AIS D | 0.61 (0.43–0.88) | 0.58 (0.40–0.84) | |
Hosmer-Lemeshow; χ2 = 9.78; DF = 8; p = 0.28; C-statistic=0.75; variables adjusted for all other variables in the table
MVC/Fl/Sp =motor vehicle crash/fall/sports
Results from the CHART Model
Table 3 summarizes change in life expectancy (calculated using the results from the logistic regression model) and RMD between the income categories and between the CHART economic self-sufficiency scores. For each of the 6 examples, the increase in life expectancy between the highest income category (over $75,000 per year) and the low income category (less than $25,000 per year) was more than double that of the difference between the middle income ($24,999–$75,000 per year) and low income groups. For instance, at age 50 for those with a C4 injury level, there was a 2.6 year increase in life expectancy between the lowest and middle categories (RMD=23.6%), whereas there was a 6.5 year increase in life expectancy between the lowest and highest category (RMD =50.2%). The increase in life expectancy between low income to high income (6.5 years) represents a 150% increase in change in life expectancy compared with the difference between low income to middle income (2.6 years), whereas 100% would be expected if the relationship between categories was linear. Similarly, using the same C4 example, only at age 25, increases in life expectancy were 4.2 and 10.2 years between low to middle income and low to high income (a 142% increase in change in life expectancy where 100% would be expected).
Table 3.
Absolute differences in life expectancies using the multivariable logistic regression model.
| Level | Income | CHART | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Middle-Low | High-Low | Middle-Low | High-Low | ||||||
| Difference | RMD | Difference | RMD | Difference | RMD | Difference | RMD | ||
| Age 50* | C4 | 2.6 | 23.6% | 6.5 | 50.2% | 1.6 | 16.3% | 3.4 | 31.8% |
| Age 50* | C6 | 2.7 | 21.5% | 6.8 | 46.6% | 1.7 | 15.4% | 3.7 | 30.7% |
| Age 50* | T7 | 3.4 | 18.3% | 8.2 | 39.0% | 2.1 | 12.2% | 4.6 | 24.9% |
| Age 25* | C4 | 4.2 | 16.7% | 10.2 | 36.3% | 2.8 | 12.1% | 5.8 | 23.5% |
| Age 25* | C6 | 4.3 | 15.6% | 10.5 | 34.1% | 2.8 | 11.1% | 5.9 | 22.0% |
| Age 25* | T7 | 4.7 | 12.8% | 11.1 | 27.8% | 3.2 | 9.2% | 6.5 | 17.8% |
Low Income=<$25,000, Middle Income=$25,000–74,999, High Income=>$75,000
Low Chart=0–50, Middle Chart=51–75, High Chart=76–100
White, male, motor vehicle crash etiology, AIS A, high school degree
Figure 1 directly compares the RMD using income and CHART economic self-sufficiency scores. This illustrates overall greater differences in RMD as a function of household income compared with the CHART economic self-sufficiency score.
Figure 1.
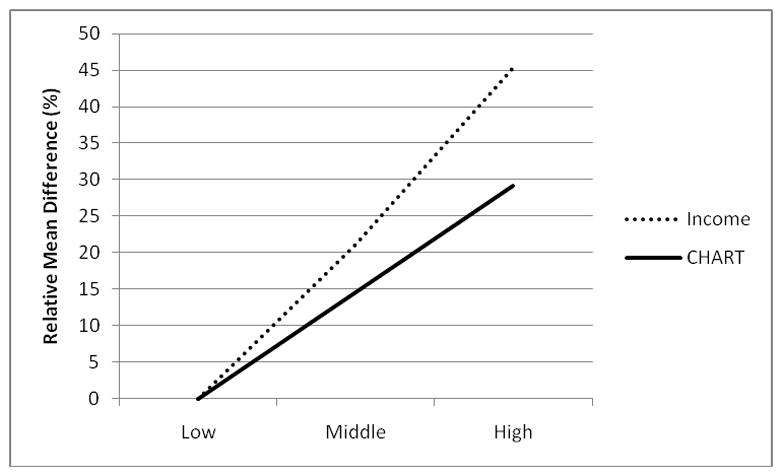
RMD in life expectancy as a function of family income and the economic subscale of the CHART
DISCUSSION
The results establish the importance of income as a predictor of long-term mortality and life expectancy after SCI among those persons who have already survived several years after injury. In general, these findings are consistent with previous studies using this database, as they also reaffirm the importance of injury severity and chronologic age with mortality.5–6 We found a clear gradation in survival based on an income effect (high, middle, low) on mortality. The effects were stronger by virtue of using household income rather than the CHART economic self-sufficiency score.5–6
Previous studies utilizing data from the MSCIS included a number of predictor variables in addition to economics (e.g., health status). Inclusion of these additional predictor variables made it impossible to directly compare the added predictive value of using household income in this study. Instead of attempting these direct comparisons, we included separate analyses of both income and CHART economic self-sufficiency scores in relation to life expectancy. Our findings suggest household income was more strongly associated with life expectancy than was the CHART economic self-sufficiency score (as used in earlier studies).5–6 When we isolated the effects of favorable economics, as defined by differences in life expectancy estimates between low and high income groups (using the example of C6 tetraplegia), there was a 34.1% RMD in life expectancy between low and high income groups for the 25-year old example, but only a 22% RMD between low and high CHART scores. For the 50-year-old example, the RMD was 46.6% between high and low income groups, compared with only 30.7% when using CHART economic self-sufficiency scores. Therefore, by virtue of using the CHART economic self-sufficiency score, earlier studies almost certainly underestimated the importance of favorable economics in relation to life expectancy. Our findings are also consistent with another recent study of household income and life expectancy among 1361 participants with SCI, finding nearly identical odds ratios between low and high income (2.40 compared with 2.31 in the current study) and between middle and high income (1.58 compared with 1.61 in the current study).10
Although these findings suggest CHART economic self-sufficiency scores have a ceiling too low to fully tap the relationship between favorable economics and life expectancy, income scores also appear to have a ceiling effect, although not as great as the CHART economic self-sufficiency scores. This is reflected by the accelerating function between income and life expectancy, with a smaller RMD between low to mid-income levels compared with the RMD between mid-income and high income levels. In short, life expectancy of those with household income substantially higher than $75,000 may have still greater life expectancies, although there would be a point where we would anticipate this relationship would plateau. Recent estimates from the current population survey indicate that 37.0% of households in the general population have income of $75,000 or more per year.20 Our findings are also supported by studies of SES and life expectancy in the general population in the United States. These studies have found relationships between life expectancy and income, education,21–22 and also an index of deprivation.23
These findings have important implications for policy and practice, as education and income are variables that can become the focus of interventions to some degree. Policies that provide disincentives to return to work and obtaining earned income may inadvertently undermine longevity. We do not know the mechanisms by which income affects mortality, but a recently published extension to the theoretical risk model of mortality after SCI hypothesizes income is associated with both tangible and intangible benefits. The tangible benefits include access to resources and health care that can be used to reduce the likelihood of secondary conditions and obtain treatment when needed; whereas the less frequently discussed intangible benefits would include diminished stress that may otherwise result from unmet SCI needs. Using stress based neurobiologic theory, investigators have demonstrated relationships between socioeconomic status and multiple health outcomes within the general population.24
Limitations
There are several limitations that may bias estimates of life expectancy. First, there is considerable left censoring of the data (persons eligible for this study may have died before the study began), as participants were an average of 7.7 years post-injury at assessment. Therefore, substantial mortality occurred prior to the assessment of income and education. Second, the effect of injury severity on mortality will be underestimated because this effect is known to be greater in earlier years after injury (years that are differentially excluded from this sample). Third, some deaths likely occurred but went unreported due to the use of the SSDI, which was found to have only 92.4% sensitivity among deceased persons with SCI.11 Fourth, persons who are lost to follow-up are slightly more likely to be deceased than persons who are successfully followed, because being deceased is a reason why people cannot be found by data collectors. Fifth, there was an insufficient sample size above 80 years of age that precluded further modeling of the effect of age on mortality. The effect of this bias is to overestimate life expectancy in those who are most likely to still be alive to reach those ages (AIS D injuries, non-cervical injuries, and injuries at older ages). These sources of bias affect the accuracy of point estimates of life expectancy but should have only a small effect on the magnitude of differences between life expectancies based on income or CHART economic self-sufficiency scores.
Other equally important limitations of this study will offset the aforementioned biases thereby causing an underestimation of the magnitude of the relationship of income and life expectancy. First, education and income are based on self-report, and inaccurate reporting is a possibility. For example, some persons who had income might underreport it out of fear of losing benefits or being reported for tax purposes. Second, income and education may change over time, and measuring them only once will result in misclassification for some of the person-years. However, relatively few participants had income that changed more than one category over time (2.5%), so the effect of income change should be minimal. Third, there is an artificial ceiling on income level at greater than $75,000 per year, such that we cannot differentiate the effects of income near this level with those of substantially higher levels. The greater the degree of inaccurate reporting of income (either due to inaccurate reports per se or changes in income since assessment) and the extent to which income level beyond $75,000 is associated with further declines in mortality, the more likely life expectancy will be underestimated for those with the highest incomes. Fourth, those with missing income data who were excluded from this study had a slightly higher subsequent mortality rate than persons from whom income data were obtained. If these individuals were systematically from 1 income group, this would affect the strength of the relationship between income and mortality. Similarly, we did not identify the underlying factors or mechanisms by which income would be related to life expectancy (e.g. access to high-quality medical care). It is worth noting, however, that insurance status through worker’s compensation was not a significant predictor of mortality in this study.
Two other aspects of the study are noteworthy. Because of the relatively small number of ventilator-dependent persons, they could not be included in the study. Health and income are likely intricately related and both are predictive of mortality.5, 9 We did not utilize health or community integration as predictors, as was done in previous MSCIS studies, and we could not adjust for specific health-related behaviors and disease that track with income level. To the extent that higher income is related to better overall health and community integration, adjusting for those factors would reduce the apparent impact of income, as it did in previous MSCIS studies..
Future Research
A priority for additional research is to identify the mechanisms by which household income is related to mortality. Because of the importance of access to quality care, future research should consider direct measurement of this in relation to life expectancy. It is also important to determine whether different mechanisms relate to low and high income. From a methodologic standpoint, a direct follow-up of this cohort utilizing the NDI, along with the SSDI, would help to capture all cases of mortality and refine estimates of life expectancy. If income is related to the probability of deaths being identified by the SSDI, with higher incomes more likely to be detected because they are making social security payments, then the addition of the NDI will help to determine whether the strength of the relationship of income and mortality is actually greater. Additionally, the NDI can provide information regarding the causes of death, and further analyses can be done to look at the association of income with specific causes of death. Lastly, there must be a priority for intervention research to enhance longevity after SCI.
Conclusion
Although SCI is associated with an increased risk of mortality, life expectancy estimates vary substantially as a function of household income.
Acknowledgments
Sponsorship: The contents of this publication were developed under grants from the Department of Education, NIDRR grant numbers H133G030117 and H133N000005, and the National Institutes of Health, grant number 1R01 NS 48117-01. However, those contents do not necessarily represent the policy of the Department of Education or NIH, and you should not assume endorsement by the Federal Government.
I certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on me or on any organization with which I am associated AND, if applicable, I certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
List of Abbreviations
- AIS
American Spinal Injury Association Impairment Scale
- BRFSS
Behavioral Risk Factor Surveillance System
- CHART
Craig Handicap Assessment and Reporting Technique
- CI
confidence interval
- MSCIS
Model Spinal Cord Injury Systems
- NDI
National Death Index
- NSCISC
National Spinal Cord Injury Statistical Center
- OR
odds ratio
- RMD
relative mean difference
- SCI
spinal cord injury
- SSDI
Social Security Death Index
Footnotes
Reprints are not available from this author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Spinal Cord Injury Statistical Center (NSCISC) Annual Statistical Report. Birmingham, AL: University of Alabama; Jun, 2006. [Google Scholar]
- 2.DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation. 1999;80(11):1411–9. doi: 10.1016/s0003-9993(99)90252-6. [DOI] [PubMed] [Google Scholar]
- 3.Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2006;87:1079–85. doi: 10.1016/j.apmr.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 4.Krause JS. Secondary conditions and spinal cord injury: A model for prediction and prevention. Topics in Spinal Cord Injury Rehabilitation. 1996;2(2):217–27. [Google Scholar]
- 5.Krause JS, DeVivo MJ, Jackson AB. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Archives of Physical Medicine & Rehabilitation. 2004;85:1764–73. doi: 10.1016/j.apmr.2004.06.062. [DOI] [PubMed] [Google Scholar]
- 6.Strauss D, DeVivo M, Shavelle R, Brooks J, Paculdo D. Economic factors and longevity in spinal cord injury: a reappraisal. Archives of Physical Medicine & Rehabilitation. 2008;89(3):572–4. doi: 10.1016/j.apmr.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Krause JS. Accuracy of life expectancy estimates in life care plans: Consideration of non-biographical and injury related factors. Topics in Spinal Cord Injury Rehabilitation. 2002;7:59–68. [Google Scholar]
- 8.Krause JS, Carter RE. Risk of mortality after spinal cord injury: relationship with social support, education, and income. Spinal Cord. 2009;47(8):592–6. doi: 10.1038/sc.2009.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krause JS, Zhai Y, Saunders LL, Carter RE. Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil. 2009;90(10):1708–15. doi: 10.1016/j.apmr.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krause JS, Saunders LL. Life expectancy estimates in the life care plan: Accounting for economic factors. Journal of Life Care Planning. 2010;9(2):15–28. [PMC free article] [PubMed] [Google Scholar]
- 11.DeVivo MJ, Stover SL, Black KJ. Prognostic factors for 12-year survival after spinal cord injury. Arch Phys Med Rehabil. 1992;73(2):156–62. [PubMed] [Google Scholar]
- 12.DeVivo M, Underhill A, Fine P. Accuracy of world-wide-web searches for persons with traumatic brain injury. Brain Injury. 2004;18(11):1155–62. doi: 10.1080/02699050410001672323. [DOI] [PubMed] [Google Scholar]
- 13.Powell-Griner E, Anderson JE, Murphy W. State-and sex-specific prevalence of selected characteristics--behavioral risk factor surveillance system, 1994 and 1995. Morbity and Mortality Weekly Report CDC Surveill Summ. 1997;46(3):1–31. [PubMed] [Google Scholar]
- 14.Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. The Craig Handicap Assessment and Reporting Technique. Englewood, CO: Craig Hospital; 1992. [Google Scholar]
- 15.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–92. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 16.Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association Spinal Cord. 1997;35:266–74. doi: 10.1038/sj.sc.3100432. [DOI] [PubMed] [Google Scholar]
- 17.Strauss D, Shavelle R, DeVivo MJ, Day S. An analytic method for longitudinal mortality studies. Journal of Insurance Medicine. 2000;32:217–25. [PubMed] [Google Scholar]
- 18.Hosmer DW, Lemeshow S. Applied logistic regression. 2. New York, New York: John Wiley and Sons; 2000. [Google Scholar]
- 19.DeVivo MJ. Estimating life expectancy for use in determining lifetime costs of care. Topics in Spinal Cord Injury Rehabilitation. 2002;7(4):49–58. [Google Scholar]
- 20.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2007. 2008 [cited 2009 May 4]. Available from: URL: http://www.census.gov/prod/2008pubs/p60-235.pdf.
- 21.Rogot E, Sorlie PD, Johnson NJ. Life expectancy by employment status, income, and education in the National Longitudinal Mortality Study. Public Health Rep. 1992;107(4):457–61. [PMC free article] [PubMed] [Google Scholar]
- 22.Lin CC, Rogot E, Johnson NJ, Sorlie PD, Arias E. A further study of life expectancy by socioeconomic factors in the National Longitudinal Mortality Study. Ethn Dis. 2003;13(2):240–7. [PubMed] [Google Scholar]
- 23.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35(4):969–79. doi: 10.1093/ije/dyl083. [DOI] [PubMed] [Google Scholar]
- 24.Szanton SL, Gill JM, Allen JK. Allostatic load: a mechanism of socioeconomic health disparities? Biol Res Nurs. 2005;7(1):7–15. doi: 10.1177/1099800405278216. [DOI] [PMC free article] [PubMed] [Google Scholar]


