Abstract
Objective
To determine whether changes in leisure time physical activity (LTPA) and body composition reflect concomitant changes in 400 m walk time.
Methods
Data were collected at the baseline and 48 month visits in Women on the Move through Activity and Nutrition Study. At baseline, participants (n=508) were randomized to the Lifestyle Intervention (LC) or Health Education (HE) group. The LC intervention focused on weight (7–10%) and waist circumference reduction through healthy lifestyle behavior change. Change in walk time over 48 months was the primary outcome. Secondary measures included change in LTPA and body composition measures including, body weight, BMI, waist circumference (WC), and dual energy x-ray absorptiometry-derived fat and lean mass.
Results
Increased LTPA and reductions in body weight, BMI, WC, and fat mass were associated with decreased walk time from baseline to 48 months (p<0.01). After stratification by group, LTPA was no longer significantly related to walk time in the HE group.
Conclusions
Increased LTPA and weight loss resulted in improved physical function, as measured by the 400 m walk, in a group of overweight, post-menopausal women. These findings support the utility of the 400 m walk to evaluate progress in physical activity or weight loss programs.
Keywords: body composition, walking, postmenopause
Introduction
Self-paced walking tests were developed to provide a familiar and acceptable method of estimating cardiorespiratory fitness and exercise tolerance in older adults1,2. The Long Distance Corridor Walk (LDCW) protocol was designed to build upon the strengths of previous time-based walks, but provide a more accurate estimate of cardiorespiratory fitness. In a 2001 study of older adults, Simonsick et al.1 showed that when compared to the six-minute walk, participants performed closer to maximal capacity when asked to walk a given distance [i.e., 400 meters (m)]. In a follow-up study that also included older adults, the 400 m walk was shown to be a valid estimate of measured maximal oxygen consumption (VO2max)2. In addition to providing a valid field estimate of cardiorespiratory fitness among older adults, the 400 m walk was also shown to be a valid estimate physical function3 and predict total mortality, cardiovascular disease (CVD), mobility limitation and disability4.
Although there is evidence to support that the 400 m walk is a useful estimate of cardiorespiratory fitness1,2, functional status3, and general health4,5 among older adults, the utility of this measure in younger populations is currently unknown. Results from two previous studies examining the 400 m walk in middle-aged women are promising6,7. In our 2007 study using baseline data from the Woman on the Move through Activity and Nutrition (WOMAN) Study, longer 400 m walk times were significantly associated with increased clinical and subclinical CVD risk6. In a 2010 validation study which also included middle-aged women, 400 m walk time was shown to be highly reproducible over a one-week interval, a valid estimate of measured VO2max, and significantly related to a comprehensive profile of physical activity and fitness measures7. Obesity has been shown to be associated with increased functional limitation and decreased physical performance8,9. Although the evidence is mounting supporting the role of the 400 m walk to provide an estimate of cardiorespiratory fitness in middle-aged women, it currently unknown whether it can also be used as a marker of physical function. Given that physical activity and body composition have been shown to be important predictors of physical function10, the objectives of this study were to examine whether changes in LTPA and body composition reflect concomitant changes in walk time over a 48 month period. Together with results of previous studies, these findings would clarify the utility of the 400 m walk in middle-aged women.
Methods
Design Overview
The WOMAN Study, a five year randomized clinical trial, was designed to evaluate whether a non-pharmacological lifestyle intervention focused on weight loss through dietary and physical activity changes would reduce measures of subclinical atherosclerosis among postmenopausal women aged 52–62 years11. Data were collected at baseline, 6, 18, 30, and 48 months; however, all measures relevant to these analyses were completed at baseline and study end.
Setting and Participants
Recruitment and data collection were conducted at the University of Pittsburgh in Pittsburgh, PA. Eligibility criteria for study enrollment included body mass index (BMI) between 25–39.9 kg/m2, waist circumference ≥ 80 cm, no diagnosed CVD, type 2 diabetes mellitus, and/or psychotic disorder, blood pressure ≤ 140/90 mmHg with or without antihypertensive therapy, and low density lipoprotein cholesterol (LDL-c) level between 100–160 mg/dL without lipid lowering therapy11,12. Women were primarily recruited through direct mailing from selected ZIP codes in Allegheny County, Pennsylvania from April 2002 to October 2003. All participants provided written informed consent and all protocols were approved by the institutional review board at the University of Pittsburgh.
Randomized Groups
In total, 508 eligible women were randomized to the health education (HE) or a lifestyle change (LC) group using a block randomized design. The intervention design of the WOMAN Study has been previously reported11,12. The HE (comparison) group received a core educational series of six lectures offered in year 1 and then quarterly thereafter. The intervention offered to the LC group built upon previous studies utilizing a non-pharmacological lifestyle approach, including the Women’s Healthy Lifestyle Project13 and Diabetes Prevention Program14. The lifestyle intervention was group-based and facilitated by a multidisciplinary team of nutritionists, exercise physiologists, and behavioral psychologists. The specific goals focused on weight and waist circumference reduction through dietary and physical activity changes. Participant contact was extensive and included 40 group visits during the first year and a minimum of 12 monthly visits in years 2 and 3. The lifestyle intervention was stopped at approximately 36 months due to lack of continued funding. Accordingly, results from baseline to 48 months post-randomization include a period of approximately 12 months where there was little or no intervention.
Study Measures
400 Meter Walk
The 400 m walk test requires participants to walk 10 laps along a hallway with cones set 20 m apart (40 m per lap) at a pace that could be maintained for the full 10 laps (i.e., usual pace). Heart rate (HR) was monitored with a Polar Pacer heart monitor (Model 60905; Woodbury, NY). Participants with elevated blood pressure (BP≥200/110) or resting HR (>110 or <40) or reporting exacerbation of chest pain, shortness of breath, or cardiac event or procedure within the past three months were excluded for safety reasons. The 400 m walk was stopped if the participant’s HR exceeded 135 beats per minute or if a participant reported chest pain or dyspnea during the test. HR was recorded in the seated position prior to the walk and standing at test completion and following 2 minutes of recovery. Systolic blood pressure (SBP) was measured while seated prior to the walk and standing at test completion. The entire protocol took approximately 8–10 minutes to administer.
Physical Activity
Physical activity was collected using the Modifiable Activity Questionnaire (MAQ), an interviewer-administered questionnaire, which assesses reported leisure and occupational activities over the past year15. Due to the limited reported occupational activity in the WOMAN Study population, only the LTPA estimate is reported16. LTPA was calculated as the product of the duration and frequency of 39 common activities (in hours per week), weighted by a standardized estimate of the metabolic equivalent (MET) of that activity17 and summed for all activities performed. Data were expressed as metabolic equivalent hours per week (MET·hr·wk−1). The MAQ has been previously shown to be a reliable15,18 and valid15,18,19 estimate of self-reported physical activity.
Body Composition
Height and weight measured with a stadiometer and calibrated balance beam scale, respectively; BMI was calculated by dividing the participant’s weight in kilograms by the square of her height in meters. Average waist circumference was measured at the navel (horizontal plane at the center of the navel) using a fiberglass retractable tape measure. A Hologic QDR 200 densiometer (Hologic; Waltham, MA) was used to ascertain whole body, trunk, and leg body fat and non-fat (i.e., lean) mass. The ratio of low (40 keV) and high energy (70 keV) attenuation is linearally related to the amount of fat in the soft tissue20. Using this ratio it is possible to discriminate fat from non-fat mass, thus providing a valid measure of body composition.
Other Relevant Variables
Age (years) and demographic factors including race/ethnicity, educational attainment, marital status, and health behavior information and hormone therapy use were collected using standardized questionnaires.
Statistical Methods
Univariate analyses were conducted on measured parameters, stratified by randomized group assignment. All continuous variables were assessed for normality. Normally distributed variables were summarized with mean and standard deviation, non-normal data with medians and interquartile range (IQR), and proportions were noted for categorical variables. Depending upon the characteristics of the variable, Student t-tests, Wilcoxon Rank Sum, or asymptotic or exact chi square (χ2) tests compared the equality of parameters between the HE and LC group. In all WOMAN Study participants, and then stratified by randomized group assignment, linear mixed models (i.e., repeated measures analysis of variance) were used to quantify the rate of increase or decrease in 400 m walk time per unit increase in self-reported leisure physical activity and traditional and DXA-derived body composition parameters after adjustment for age at 48 month visit and relevant activity or body composition level at baseline. Since obese individuals have more lean mass than normal weight individuals of the same height21, lean mass parameters were adjusted for BMI at the 48 month follow-up. In the stratified analyses, tests of equality between the two slopes were then computed to determine if measuring the rate of change in 400 m walk differed between randomized groups. The distribution of LTPA was positively skewed with several relatively large values; therefore, a square-root transformation was applied before analyses. The means were then back-transformed and presented in MET·hr·wk−1. Statistical analyses were generated on all available data using SAS/STAT software, Version 9.2 of the SAS System for Windows (Cary, NC).
Results
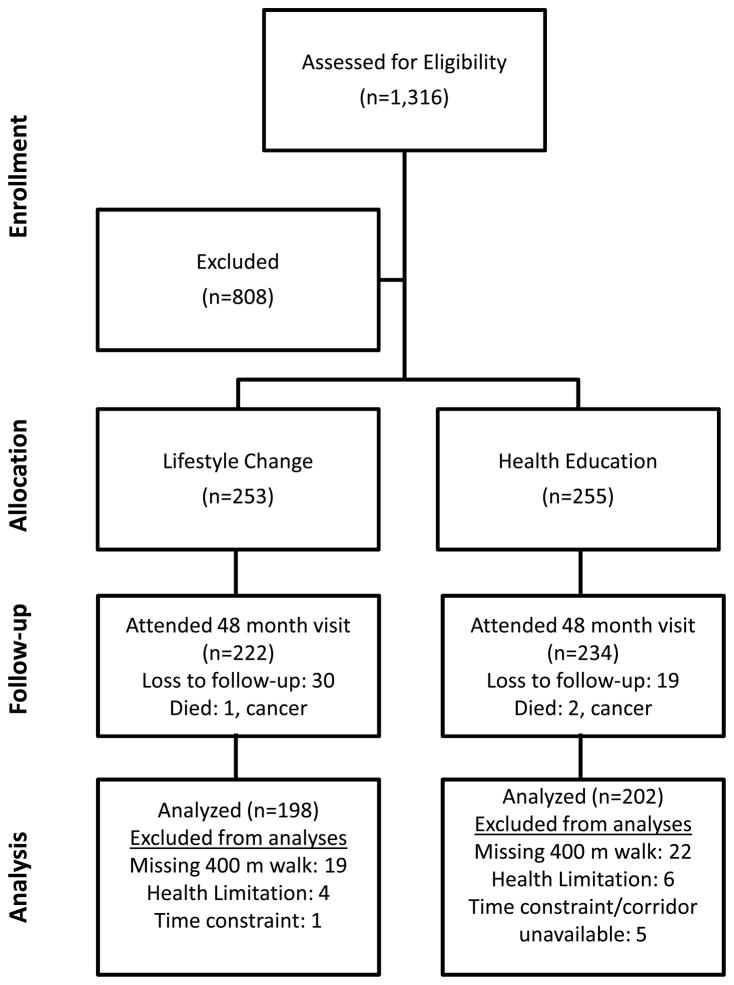
Of the 508 WOMAN Study participants randomized at baseline, 502 (98.8%) and 399 (78.5%) women completed the 400 m walk at the baseline and the 48 month follow-up visits, respectively (Figure 1). Of the 454 participants who completed at least part of the 48 month visit, 39 (8.6%) had missing 400 m walk data due to an undocumented reason, 6 (1.3%) did not complete the 400 m walk due to personal time constraints or unavailability of the corridor, and 10 (2.2%) did not complete the walk due to a functional limitation, acute symptom (e.g., dizziness), or chronic condition (i.e., recent diagnosis of cardiac arrhythmia). There were no significant differences in participant characteristics or baseline levels of LTPA or BMI between those that completed and did not complete the 400 m walk at 48 months.
FIG. 1.
Flow diagram of participants’ progress through the phases of the Women on the Move Through Activity and Nutrition study randomized trial.
At baseline, there were also no significant differences in measured parameters between randomized groups (Table 1). However, at 48 months, the HE group had longer walk times, and greater body weight, BMI, WC, and trunk fat mass when compared to the LC group (all p<0.04). Also, the HE group had somewhat greater whole body fat, whole body lean mass, and left leg lean mass than the LC group (all p<0.10). In the LC group, 400 m walk time significantly decreased over 48 months (p=0.03), whereas no significant change in walk time was noted over that same time period in the HE group.
Table 1.
Demographic, movement, and body composition variables among Woman on the Move through Activity and Nutrition (WOMAN) Study participants, stratified by randomized group assignmenta,b.
| Baseline | 48 Month (mo) Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Lifestyle Change | n | Health Education | p value | n | Lifestyle Change | n | Health Education | p value | |
| Demographic Factors | ||||||||||
| Age, years | 253 | 56.9 (2.94) | 255 | 57.1 (2.94) | .34 | 222 | 60.8 (2.94) | 234 | 61.1 (2.94) | .30 |
| High School graduate, % | 252 | 98.8 | 255 | 98.4 | 1.0 | --- | --- | --- | --- | --- |
| Non-White, % | 253 | 10.3 | 255 | 13.3 | .29 | --- | --- | --- | --- | --- |
| Married, % | 253 | 68.8 | 255 | 66.3 | .55 | --- | --- | --- | --- | --- |
| Current smoker, % | 253 | 6.7 | 255 | 5.5 | .56 | --- | --- | --- | --- | --- |
| Hormone Therapy (HT) Group, % | --- | --- | --- | 221 | 232 | .20 | ||||
| HT at baseline and 48 mo | --- | --- | 37 | 16.7 | 40 | 17.2 | ||||
| Discontinued HT by 48 mo | --- | --- | 106 | 48.0 | 89 | 38.4 | ||||
| Started HT at 48 mo | --- | --- | 2 | 0.9 | 3 | 1.3 | ||||
| No HT at baseline or 48 mo | --- | --- | 76 | 34.4 | 100 | 43.1 | ||||
| Movement | ||||||||||
| Past Year Leisure Physical Activity, MET·hr·wk−1 | 250 | 11.1 (5.9, 20.2) | 250 | 11.5 (4.9, 21.2) | .67 | 217 | 11.6 (6.7, 21.9) | 230 | 12.1 (4.6, 20.0) | .20 |
| 400 m walk, sec | 249 | 311.6 (37.0) | 253 | 314.7 (37.0) | .34 | 198 | 308.7 (41.0) | 201 | 320.5 (41.0) | .004 |
| Body Composition | ||||||||||
| Traditional Measures | ||||||||||
| Body weight, lbs | 253 | 179.1 (25.3) | 255 | 181.3 (25.3) | .32 | 222 | 172.6 (26.9) | 232 | 180.6 (26.9) | .002 |
| Body mass index, kg/m2 | 253 | 30.6 (3.8) | 255 | 30.9 (3.8) | .29 | 222 | 29.5 (4.2) | 232 | 30.9 (4.2) | .0004 |
| Waist Circumference, cm | 253 | 105.5 (11.2) | 255 | 106.3 (11.2) | .42 | 221 | 98.3 (11.4) | 230 | 102.2 (11.4) | .0002 |
| DXA Measures | ||||||||||
| Fat Mass, kg | ||||||||||
| Whole Body | 246 | 33.1 (7.1) | 248 | 33.7 (7.1) | .40 | 207 | 32.7 (7.7) | 217 | 34.1 (7.7) | .06 |
| Trunk | 246 | 15.9 (3.9) | 248 | 16.2 (3.9) | .40 | 207 | 15.9 (4.4) | 217 | 16.7(4.4) | .04 |
| Right Leg | 246 | 6.1 (1.5) | 248 | 6.1 (1.5) | .71 | 207 | 6.1 (1.6) | 217 | 6.2 (1.6) | .41 |
| Left Leg | 246 | 5.9 (1.5) | 248 | 6.0 (1.5) | .54 | 207 | 5.7 (1.5) | 217 | 5.9 (1.5) | .23 |
| Lean Mass, kg | ||||||||||
| Whole Body | 246 | 46.6 (5.5) | 248 | 47.2 (5.5) | .26 | 207 | 45.6 (5.4) | 217 | 46.5 (5.4) | .07 |
| Trunk | 246 | 22.8 (2.8) | 248 | 23.2 (2.8) | .20 | 207 | 22.5 (2.8) | 217 | 22.9 (2.8) | .13 |
| Right Leg | 246 | 7.6 (1.1) | 248 | 7.7 (1.1) | .25 | 207 | 7.4 (1.1) | 217 | 7.6 (1.1) | .11 |
| Left Leg | 246 | 7.6 (1.1) | 248 | 7.7 (1.1) | .33 | 207 | 7.4 (1.1) | 217 | 7.5 (1.1) | .10 |
Data presented as mean (standard deviation), median (interquartile range), or percent.
Student t-test, wilcoxon rank sum, or chi square test used to compare data collected at baseline and 48 month follow-up visits between lifestyle change and health education groups.
All WOMAN Study Participants
After adjustment for age at 48 month visit and relevant baseline LTPA or body composition level, increased LTPA and reduced body weight, BMI, waist circumference, whole body, trunk, and lower leg fat mass were related to an decrease in walk time (Table 2). More specifically, a one MET·hr·wk−1 increase in LTPA was associated with a 3.16 second decrease in 400 m walk time from baseline to 48 months (p=.006). Further, a per unit increase in body weight (lbs), BMI (kg/m2), and waist circumference (cm) resulted in an increased walk time of 0.73, 4.56, and 1.31 seconds, respectively (all p<.001) over 48 months. Finally, a 1 kg increase in whole body, trunk, and right and left leg fat mass were all significantly associated with increases in walk time from baseline to 48 months [i.e., 2.22, 3.83, 10.88, and 11.96 seconds, respectively (all p<.001)]. Longitudinal relationships between lean mass parameters and walk time were not statistically significant.
Table 2.
Longitudinal relationshipsa between 400 m walk time and leisure physical activity (LTPA)b and body composition parameters from baseline to the 48 month follow-up visit.
| n | Slope Estimate | Standard Error | p value | |
|---|---|---|---|---|
| Leisure Physical Activity, MET·hr·wk−1 | 384 | −3.16 | 1.16 | 0.006 |
| Body Composition | ||||
| Traditional Measures | ||||
| Body weight, lbs | 395 | 0.73 | 0.12 | <.001 |
| Body mass index, kg/m2 | 395 | 4.56 | 0.65 | <.001 |
| Waist Circumference, cm | 395 | 1.31 | 0.23 | <0.001 |
| DXA Measures | ||||
| Fat Mass, kg | ||||
| Whole Body | 364 | 2.22 | 0.37 | <0.001 |
| Trunk | 364 | 3.83 | 0.65 | <0.001 |
| Right Leg | 364 | 10.88 | 2.12 | <0.001 |
| Left Leg | 364 | 11.96 | 2.19 | <0.001 |
| Lean Mass, kg | ||||
| Whole Body | 364 | 0.81 | 0.93 | 0.38 |
| Trunk | 364 | 1.30 | 1.50 | 0.39 |
| Right Leg | 364 | −0.21 | 4.19 | 0.96 |
| Left Leg | 364 | −1.81 | 4.24 | 0.85 |
LTPA, body weight, BMI, waist circumference, and DXA-derived fat mass models adjusted for age at 48 month follow-up and relevant baseline value; DXA-derived lean mass models additionally adjusted for BMI at 48 month visit.
A square-root transformation was applied to Past Year Leisure Physical Activity. Data is back-transformed and presented as means.
Lifestyle Change vs. Health Education Group
After stratification by randomized group assignment, results were similar (Table 3). In the LC group, increased LTPA and decreased body weight, BMI, waist circumference, and whole body, trunk, and lower extremity fat mass were significantly associated with reductions in 400 m walk time from baseline to 48 months, after adjustment for age at 48 months and LTPA or relevant body composition level at baseline (all p<0.01). Similar to the unstratified results, no significant associations were noted between lean mass parameters and 400 m walk time from baseline to 48 month follow-up. In the HE group, results were again similar; however, longitudinal relationships between walk time and LTPA were not statistically significant (p=0.50). When examining the equality of the regression slopes between 400 m walk time and LTPA and body composition measures by randomized group assignment, significant slope differences were noted for LTPA only (p=.047).
Table 3.
Longitudinal relationshipsa between 400 m walk time and leisure physical activity (LTPA)b and body composition parameters from baseline to the 48 month follow-up visit, stratified by randomized group assignment.
| Lifestyle Change | Health Education | Test for equality of slope p value |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Slope Estimate | Standard Error | p value | n | Slope Estimate | Standard Error | p value | ||
| Leisure Physical Activity, MET·hr·wk−1 | 190 | −5.21 | 1.64 | .002 | 194 | −1.00 | 1.48 | 0.50 | 0.047 |
| Body Composition | |||||||||
| Traditional Measures | |||||||||
| Body weight, lbs | 196 | 0.69 | 0.15 | <.001 | 199 | 0.71 | 0.19 | <.001 | 0.95 |
| Body mass index, kg/m2 | 196 | 4.30 | 0.87 | <.001 | 199 | 4.60 | 1.08 | <.001 | 0.82 |
| Waist Circumference, cm | 196 | 1.22 | 0.29 | <.001 | 199 | 1.26 | 0.36 | 0.001 | 0.92 |
| DXA Measures | |||||||||
| Fat Mass, kg | |||||||||
| Whole Body | 181 | 2.00 | 0.49 | <.001 | 183 | 2.36 | 0.58 | <.001 | 0.63 |
| Trunk | 181 | 3.23 | 0.84 | <.001 | 183 | 4.45 | 1.05 | <.001 | 0.36 |
| Right Leg | 181 | 10.2 | 2.91 | <.001 | 183 | 10.9 | 3.09 | <.001 | 0.88 |
| Left Leg | 181 | 11.1 | 2.99 | <.001 | 183 | 12.2 | 3.20 | <.001 | 0.81 |
| Lean Mass, kg | |||||||||
| Whole Body | 181 | 1.04 | 1.28 | 0.42 | 183 | 0.36 | 1.23 | 0.77 | 0.68 |
| Trunk | 181 | 1.82 | 2.05 | 0.38 | 183 | 0.55 | 1.98 | 0.78 | 0.64 |
| Right Leg | 181 | −2.80 | 5.42 | 0.61 | 183 | 2.18 | 6.01 | 0.72 | 0.52 |
| Left Leg | 181 | −0.54 | 5.64 | 0.92 | 183 | −2.31 | 5.99 | 0.70 | 0.82 |
LTPA, body weight, BMI, waist circumference, and DXA-derived fat mass models adjusted for age at 48 month follow-up and relevant baseline value; DXA-derived lean mass models additionally adjusted for BMI at 48 month visit.
A square-root transformation was applied to Past Year Leisure Physical Activity. Data is back-transformed and presented as means.
Discussion
To our knowledge, no previous study has examined the longitudinal relationships between 400 m walk and LTPA and body composition measures in a population sub-group other than older adults. In the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) study, a randomized controlled trial of a physical activity intervention compared with a successful aging intervention (i.e., comparison group) among older, sedentary adults, aged 70–89 years22, 400 m walk speed (m/sec), significantly decreased in the successful aging group after 12 months while remaining relatively stable in the physical activity group (p<.001)22. In the WOMAN Study, total walk time significantly decreased in the LC group over 48 months, while no differences in walk time were observed among participants randomized to the HE group. These findings suggest that among somewhat younger individuals, the weight loss and physical activity goals promoted in the LC group not only significantly decreased total walk time over 48 months, but may be important to attenuate declines in walking performance that are likely associated with the normal aging process.
In all WOMAN Study participants, increases in LTPA and decreases in body weight, BMI, WC, and DXA-derived fat mass were associated with shorter 400 m walk times over 48 months. Unfortunately, due to issues with data collinearities in the model (i.e., baseline body weight and age at 48 months), we were unable to determine whether the 400 m walk was more sensitive to weight loss than to change in LTPA. However, these results confirm two previous cross-sectional examination utilizing baseline data from middle-aged women6,7. In the WOMAN Study, self-report LTPA and pedometer steps significantly decreased (both p for trend <.01) and BMI and waist circumference significantly increased across increasing quartiles of walk time in early post-menopausal women (both p for trend <.0001)6. Similar relationships were observed in the PAW Study, a slightly younger sample of women representing pre- to post-menopause. After adjustment for age, 400 m walk time was inversely related to a multitude of self-report and direct physical activity measures (all p<0.05) and directly associated with WC and percent body fat as measured using bioelectrical impedance (both p<.0001)7. A direct relationship between walk time and BMI was also shown in a 2006 report by Newman et al, which utilized data in older adult participants (i.e., aged 70–79 years) from the Health Aging and Body Composition Study4. The results from the current study add to the previous studies by examining the longitudinal association between 400 m walk time in a younger cohort using a more detailed measure of body fat mass.
Elevated BMI has been shown to be related with increased self-reported functional limitation, decreased physical performance, and increased risk of functional decline8,9. In a study by Coakley et al10, BMI was shown to be the most important predictor of physical function and impaired ability to work and, after physical activity, the second most important predictor of vitality among 56,510 normal and overweight women aged 45 to 71 years enrolled in the Nurses’ Health Study (NHS). In a subsequent prospective study of the NHS cohort, weight gain over four years of observation was significantly associated with reduced physical functioning across all BMI categories among women aged 65 years or younger, with the most dramatic reductions shown in women who gained 9 kg or more. Similar findings were shown in older women (i.e., >65 years)23. Finally, participation in a 3 month weight loss intervention, that promoted weight loss through healthy dietary practices and increased physical activity, significantly increased physical performance (p=.026) as measured by a battery of basic physical tasks, including a 400 m walk24. Unfortunately, results were not shown for the 400 m walk only. In this study population, weight loss was associated with improvements in health-related quality of life25. The findings from the current study, support earlier studies and show that increased LTPA and weight loss resulted in improved physical function, as measured by the 400 m walk, in a group of overweight, post-menopausal women. Furthermore, improvements in walk time were not limited to LC participants, but rather were shown to be related to weight loss.
Interestingly, changes in DXA-derived lean mass variables from baseline to 48 month follow-up were not significantly related to changes in 400 m walk time in either the combined results or after stratification by randomized group assignment. These findings confirm earlier studies that examined associations between walking performance and lean mass. A study by Woo et al. 26, found that fat mass was a stronger determinant of six-meter walk time than appendicular muscle mass. Further, in the PAW Study, 400 m walk time was not shown to be significantly related to quadriceps and hamstring muscular strength and endurance as measured by an isokinetic dynometer in similarly aged women7.
There are several possible important clinical and research implications of the current investigation. The information gleaned from the 400 m walk could potentially be used by clinicians and researchers to provide a less invasive and valid estimate of cardiorespiratory fitness, which was demonstrated previously in PAW Study participants7. Since the only requirements for performing the test are adequate space to set up the course and a trained staff person to administer it, the 400 m walk could be particularly useful in medically underserved settings to supplement traditional health risk factor assessment and triage individuals for additional screening or intensive lifestyle intervention for chronic disease management. Further, as we have shown in the current study, the 400 m walk could be used as a direct measure to evaluate progress in lifestyle interventions or clinical weight loss programs.
A further clinical implication is the use of improved physical function as a motivational construct when counseling patients about weight loss and physical activity. Patient-centered care emphasizes placing equal weight on measures such as functional status, pain scores, and health-related quality of life when considering treatment outcomes and health care quality27–29. Additionally, patients and research participants cite improved physical function and energy levels as motivators in adopting or adhering to a weight loss or exercise program30,31. Therefore, for some patients, improved mobility may be an equally or more attractive reason to consider participating in healthy lifestyle programs than improvements in clinical measurements, such as LDL-c levels.
There are limitations to consider when interpreting the results of the current investigation. First, the study population consisted of a relatively homogeneous population which may limit the generalizability of the findings to more diverse clinical populations. Second, the walk time estimate could have been affected if participants had a gait abnormality, slowed down or took a wider step in order to navigate around the cones set up at the opposite ends of the corridor. Also, walking performance could have been influenced by individual-level differences in comprehending the instructions given prior to test initiation. However, attempts were made to reduce such bias by following a standardized protocol that was delivered by a core group of well-trained clinical research staff. Finally, in the WOMAN Study the formal lifestyle intervention ended approximately 36 months post-randomization. Twelve months of little or no intervention could have greatly impacted our ability to examine randomized group differences from baseline to 48 months, which would likely bias our results towards a null association. However, significant differences in the longitudinal relationship between LTPA and walk time between randomized groups were still observed after a significant period of no intervention. Furthermore, at intermediate follow-up visits, the LC group had significantly greater reductions in weight and waist circumference and increases in LTPA when compared to the HE group12,32.
Conclusion
The findings from the current study add to previous work exploring the psychometric properties and potential utility of the 400 m walk in middle-aged women7. In the current study, weight loss and positive healthy behavior change resulted in improved physical function, as measured by the 400 m walk. These findings clarify the value of the 400 m walk as a supplemental measure to evaluate progress in non-pharmacological lifestyle interventions or general weight loss programs. Finally, these results support future research examining the function of the 400 m walk in population sub-groups other than older adults.
Acknowledgments
The authors would like to acknowledge the 508 dedicated WOMAN study participants and the contributions of the WOMAN study staff. This research was funded by National Heart, Lung, and Blood contract R01-HL-66468.
Footnotes
Conflict of Interest/Financial Disclosure: None
References
- 1.Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: the Health ABC Long Distance Corridor Walk. J Am Geriatr Soc. 2001 Nov;49(11):1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- 2.Simonsick EM, Fan E, Fleg JL. Estimating cardiorespiratory fitness in well-functioning older adults: treadmill validation of the long distance corridor walk. J Am Geriatr Soc. 2006 Jan;54(1):127–132. doi: 10.1111/j.1532-5415.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- 3.Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2001 Oct;56(10):M644–649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 4.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. Jama. 2006 May 3;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 5.Newman AB, Haggerty CL, Kritchevsky SB, Nevitt MC, Simonsick EM. Walking performance and cardiovascular response: associations with age and morbidity--the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):715–720. doi: 10.1093/gerona/58.8.m715. [DOI] [PubMed] [Google Scholar]
- 6.Pettee KK, Larouere BM, Kriska AM, et al. Associations among walking performance, physical activity, and subclinical cardiovascular disease. Prev Cardiol. 2007 Summer;10(3):134–140. doi: 10.1111/j.1520-037x.2007.06173.x. [DOI] [PubMed] [Google Scholar]
- 7.Pettee Gabriel KK, Rankin RL, Lee CD, Charlton ME, Swan PD, Ainsworth BE. Test-Retest Reliability and Validity of the 400 Meter Walk Test in Healthy, Middle-Aged Women. Journal of Physical Activity and Health. doi: 10.1123/jpah.7.5.649. in press. [DOI] [PubMed] [Google Scholar]
- 8.Apovian CM, Frey CM, Wood GC, Rogers JZ, Still CD, Jensen GL. Body mass index and physical function in older women. Obes Res. 2002 Aug;10(8):740–747. doi: 10.1038/oby.2002.101. [DOI] [PubMed] [Google Scholar]
- 9.Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons. J Am Geriatr Soc. 2002 May;50(5):918–923. doi: 10.1046/j.1532-5415.2002.50220.x. [DOI] [PubMed] [Google Scholar]
- 10.Coakley EH, Kawachi I, Manson JE, Speizer FE, Willet WC, Colditz GA. Lower levels of physical functioning are associated with higher body weight among middle-aged and older women. Int J Obes Relat Metab Disord. 1998 Oct;22(10):958–965. doi: 10.1038/sj.ijo.0800698. [DOI] [PubMed] [Google Scholar]
- 11.Kuller LH, Kriska AM, Kinzel LS, et al. The clinical trial of Women On the Move through Activity and Nutrition (WOMAN) study. Contemp Clin Trials. 2007 Jul;28(4):370–381. doi: 10.1016/j.cct.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuller LH, Kinzel LS, Pettee KK, et al. Lifestyle Intervention and Coronary Heart Disease Risk Factor Changes over 18 Months in Postmenopausal Women: The Women On the Move through Activity and Nutrition (WOMAN Study) Clinical Trial. Journal of Women’s Health. 2006;15(8):964–976. doi: 10.1089/jwh.2006.15.962. [DOI] [PubMed] [Google Scholar]
- 13.Simkin-Silverman LR, Wing RR, Boraz MA, Kuller LH. Lifestyle intervention can prevent weight gain during menopause: results from a 5-year randomized clinical trial. Ann Behav Med. 2003 Dec;26(3):212–220. doi: 10.1207/S15324796ABM2603_06. [DOI] [PubMed] [Google Scholar]
- 14.The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002 Dec;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997 Jun;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- 16.Newman MA, Pettee KK, Storti KL, Richardson CR, Kuller LH, Kriska AM. Monthly variation in physical activity levels in postmenopausal women. Med Sci Sports Exerc. 2009 Feb;41(2):322–327. doi: 10.1249/MSS.0b013e3181864c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000 Sep;32(9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 18.Kriska AM, Knowler WC, LaPorte RE, et al. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990 Apr;13(4):401–411. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 19.Schulz LOHI, Smith CJ, Kriska AM, Ravussin E. Energy intake and physical activity in Pima Indians: comparison with energy expenditure measured by doubly-labeled water. Obes Res. 1994;2:541–548. doi: 10.1002/j.1550-8528.1994.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 20.Mazess RB, Barden HS, Bisek JP, Hanson J. Dual-energy x-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. The American journal of clinical nutrition. 1990 Jun;51(6):1106–1112. doi: 10.1093/ajcn/51.6.1106. [DOI] [PubMed] [Google Scholar]
- 21.Forbes GB. Lean body mass-body fat interrelationships in humans. Nutrition reviews. 1987 Aug;45(8):225–231. doi: 10.1111/j.1753-4887.1987.tb02684.x. [DOI] [PubMed] [Google Scholar]
- 22.Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006 Nov;61(11):1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 23.Fine JT, Colditz GA, Coakley EH, et al. A prospective study of weight change and health-related quality of life in women. Jama. 1999 Dec 8;282(22):2136–2142. doi: 10.1001/jama.282.22.2136. [DOI] [PubMed] [Google Scholar]
- 24.Jensen GL, Roy MA, Buchanan AE, Berg MB. Weight loss intervention for obese older women: improvements in performance and function. Obes Res. 2004 Nov;12(11):1814–1820. doi: 10.1038/oby.2004.225. [DOI] [PubMed] [Google Scholar]
- 25.Yankura DJ, Conroy MB, Hess R, Pettee KK, Kuller LH, Kriska AM. Weight regain and health-related quality of life in postmenopausal women. Obesity (Silver Spring, Md. 2008 Oct;16(10):2259–2265. doi: 10.1038/oby.2008.345. [DOI] [PubMed] [Google Scholar]
- 26.Woo J, Leung J, Kwok T. BMI, body composition, and physical functioning in older adults. Obesity (Silver Spring) 2007 Jul;15(7):1886–1894. doi: 10.1038/oby.2007.223. [DOI] [PubMed] [Google Scholar]
- 27.Stewart M. Towards a global definition of patient centred care. BMJ (Clinical research ed) 2001 Feb 24;322(7284):444–445. doi: 10.1136/bmj.322.7284.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Social science & medicine (1982) 2000 Oct;51(7):1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 29.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. The Journal of family practice. 2000 Sep;49(9):796–804. [PubMed] [Google Scholar]
- 30.Wilcox S, Richter DL, Henderson KA, Greaney ML, Ainsworth BE. Perceptions of physical activity and personal barriers and enablers in African-American women. Ethnicity & disease. 2002 Summer;12(3):353–362. [PubMed] [Google Scholar]
- 31.Conroy MB, Simkin-Silverman LR, Pettee KK, Hess R, Kuller LH, Kriska AM. Lapses and psychosocial factors related to physical activity in early postmenopause. Medicine and science in sports and exercise. 2007 Oct;39(10):1858–1866. doi: 10.1249/mss.0b013e318137388d. [DOI] [PubMed] [Google Scholar]
- 32.Pettee KK, Kriska AM, Conroy MB, et al. Discontinuing hormone replacement therapy: attenuating the effect on CVD risk with lifestyle changes. Am J Prev Med. 2007 Jun;32(6):483–489. doi: 10.1016/j.amepre.2007.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]