Abstract
Background
Pediatric weight management clinics experience significant dropout, and few studies have investigated this problem. The objective of this study was to identify family and clinic characteristics associated with attrition from a tertiary care pediatric weight management clinic.
Methods
This was a prospective and retrospective clinical database study of a multidisciplinary clinic for obese children 2–18 years with a weight-related co-morbidity. All patients seen between November, 2007, and July, 2009, were included. Characteristics of Active and Inactive families were compared using chi-squared and t-tests, and logistic regression was used to identify independent correlates of program status. A one-page survey was mailed to all Inactive families.
Results
A total of 133 patients were seen during the study period. Their mean age was 12 years old, mean BMI was 38 kg/m2, 53% were female, 52% represented racial/ethnic minorities, and 50% were Medicaid recipients. In all, 32% dropped out of treatment. Inactive children had significantly lower BMI z-scores, were older, and were more likely to have poor school performance than active children. Similar results were found on regression analysis: Children with higher BMI z-scores, commercial insurance, average school performance, and a major weight-related co-morbidity were less likely to be inactive. The most common parent-reported reasons for dropping out were: Child not wanting to make changes, weight not improving, child desired to leave program, and program not meeting parent or child's expectations.
Conclusions
Attrition from pediatric weight management treatment is high, with age, weight, school performance, and health associated with dropout. Parents mostly reported child-related issues, including lack of weight loss, as reasons for dropout.
Introduction
Pediatric obesity is a pressing health issue for parents and pediatric care providers. Nationally representative data from 2007 to 2008 indicate that 16.9% of children and adolescents are obese, and 32% are either overweight or obese,1 a notable increase from earlier surveys.2 Recent expert recommendations, endorsed by leading child health organizations, outline a step-wise approach to treatment, which include multidisciplinary, tertiary care clinics.3–6 The demand for weight management clinics far exceed availability.7 However, attrition from such programs ranges from 37% to 73%.8–16
Few studies have investigated attrition from pediatric weight management.9,10,15–17 Only three multidisciplinary, tertiary care clinics have studied attrition from their programs,9,10,15,16 and a fourth analyzed attrition within a study of clinic outcomes.13 From these studies of similar programs, attrition rates range from 49% to 73%. Families reported that the clinic was “not what we are looking for,” or cited problems with their child missing too much school, inconvenient locations, issues with program content, scheduling conflicts, and difficulty with insurance coverage.8–10 Perceived lower quality of care by standardized assessment was associated with dropout, as was poorer caregiver-rated health status of child.10 Increased BMI, African-American race/ethnicity, Medicaid insurance status, single-parent household, older age, and children in poorer health have been inconsistently identified as predictors of attrition.9,10,13,15,16,18 The most recent Cochrane Systematic Review on pediatric obesity intervention trials reported 0% to 42% of participants being lost to follow-up.19 A review of attrition from pediatric weight management demonstrates comparable rates of dropout between trials and clinical programs, ranging from 12.5% to 50% in intensive interventions,20 including a trial that had to modify randomization after 83% dropped out of an intensive arm using structured meal planning.21 As in reports from clinical programs, few substantial differences were found between those dropping out of versus completing treatment.
Clinics can have a beneficial effect on the health and weight of obese children,12,13,21 but many of those presenting for treatment are dropping out. Reasons for this are difficult to pinpoint, as many factors must be addressed in a nonresearch–based clinic, such as characteristics of children and families, of the clinic itself, and the interactions between them. This can be further complicated by the cost of treatment. Insurance coverage of treatment is an important issue for weight management clinics22 and is cited by families as having an impact on their attrition and possible return to treatment.9,10 The expense of treatment in multidisciplinary clinics is likely due to uncovered services, such as those of counselors and dietitians. Although cost is an important consideration in evaluating attrition from treatment, it may cloud study of the problem, because cost would not indicate quality of treatment or predict the characteristics of a family likely to drop out. Cost may be prohibitive for some families to participate in treatment, even those with private, commercial insurance who have large co-payments and deductibles. Minimizing the impact of cost on treatment may provide a better opportunity to determine contributors to patient and family attrition.
Much remains unknown regarding attrition from weight management clinics, and thus, there are limited studies in which clinicians can draw upon to address this problem in their clinics. The primary aim of this study was to identify patient and family characteristics, including sociodemographic and health-related factors, associated with attrition from a weight management clinic that has minimized the cost to families by not charging for services outside of those covered by insurance plans. A secondary aim was to determine parent/caregiver reasons for initial dropout, focusing on programmatic and family issues. The overall goal of this project is to expand what is known about attrition from clinical weight management, to provide practical evidence for clinics to address this problem.
Methods
Brenner FIT (Families In Training) Program
The Brenner FIT (Families In Training) Program is a multidisciplinary pediatric, family-based weight management clinic. The treatment team includes a pediatrician, dietitian, family counselor (licensed clinical social worker), and physical therapist. Children are seen by physician referral only. Brenner FIT accepts children aged 2–18 years who are obese (BMI ≥95th percentile for age and gender) with one or more obesity-related co-morbidities, including dyslipidemia, insulin resistance, fatty liver, orthopedic problems, pseudotumor cerebri, sleep apnea, or hypertension.
Physician services are billed to the child's insurance. Family counselor, dietitian, and physical therapy services are supported by institutional funding, philanthropy, and local charitable foundations. There are no additional costs to families aside from normal co-payments for physician services for those families with commercial insurance (Medicaid recipients have no co-payment), which occur four times over the year of treatment.
Height is measured three times with values averaged using a standing Seca® Model 240 wall stadiometer (Germany), weight measured with light clothes and no shoes on a Tanita WB 0110 Class III scale (Tokyo, Japan), and blood pressure obtained manually on a Welch–Allyn wall mounted sphygmomanometer with an appropriately sized cuff. All height, weight, and blood pressure measurements are performed by the physician in a standardized manner.
The Brenner FIT Program uses evidence- and expert opinion-based approaches to the treatment of pediatric obesity, focusing on behavior change in a family-centered setting.3,6 The treatment approach focuses on identifying unhealthy habits, then working with families to modify those habits using standard behavioral therapy approaches of self-monitoring, stimulus control, and goal setting.6,23 Motivational interviewing is used throughout to enable the family to set goals, address ambivalence to change, and keep discussions open and empathetic. All team members are trained by a certified Motivational Interviewing Network of Trainers counselor (MINT, www.motivationalinterview.org), and receive follow-up training once a year. Brenner FIT has adapted motivational interviewing, with the assistance of a MINT counselor, to use in families by a multidisciplinary team.24 Dietitians are certified by the American Dietetic Association in Childhood and Adolescent Weight Management (www.cdrnet.org/wtmgmt/childhoo.cfm), and they have established their role in a multidisciplinary team.25 Families receive training and support to implement behavior change, appropriately manage adverse reactions to lifestyle changes, and address psychosocial problems. No specific dietary intervention is employed beyond general recommendations for healthy eating (based on the US Department of Agriculture's Food Guide Pyramid, 2005). The clinic is held in the subspecialty clinics of Brenner Children's Hospital, a tertiary care pediatric hospital associated with Wake Forest University Baptist Medical Center, Winston-Salem, NC. The clinic features a large, family-friendly meeting room (bariatric couches, toys for younger children, readily available teaching materials, and a large video monitor for teaching), and a separate exam room with scale, stadiometer, and sphygmomanometer.
Treatment lasts 1 year, divided into three phases, each 4 months long. The initial visit is with the entire team, meeting all four members of the team (physician, family counselor, dietitian, physical therapist) at one time for 2 hours. This initial meeting consists of an in-depth assessment of: The child's health; family functioning, stressors, parenting practices, and child emotional and behavioral issues; dietary patterns, habits, and preferences; sedentary and physical activity levels; and overall motivation for changing health habits. The entire family, including siblings, is encouraged to attend this visit, although the child and parents typically attend. This visit also establishes the relationship between the team and the family and sets expectations for the family, including expected changes in weight and BMI, time commitment, and family participation in the program. The initial, intensive phase consists of biweekly visits with the team. The dietitian and family counselor are present for each of these visits, with the physical therapist participating if the child has musculoskeletal or activity issues, such as pain, muscle tightness, or severe cardiovascular deconditioning, or if treatment goals primarily focus on increasing physical activity. One of the primary means of behavior change is goal setting, with appropriate monitoring, or “tracking,” by the family at home. When families return to the clinic, these tracking records are used to gauge success and stimulate problem-solving discussions. The second phase consists of monthly visits with team members and features advanced goal setting and problem solving, primarily with the dietitian or family counselor. The final phase is individualized to the family, focusing on maintenance of habits modified for those successfully improving their weight status. For those not successful in weight management, the final phase entails problem solving around goals not achieved, or restructuring treatment plans to other health habits. Families see the physician every 4 months between phases to review laboratory studies, BMI, and overall progress.
After a year, families can continue with treatment or return to their primary care physician for further weight management. Referring physicians and primary care providers are updated on patient progress every 4 months and if the family ends treatment. Children who no longer meet the BMI criteria are instructed to follow up with their primary care provider.
Prospective Database
Clinical databases can be a valuable tool in evaluating effectiveness in clinical practices where randomized trials are not appropriate.26 The Brenner FIT Program uses a prospective, clinical database to track outcomes and patient progress. Our database was expanded for this study and includes most clinical information gathered on the intake visit, including: Sociodemographics; physical measures and available laboratory studies; medical history; family assessment by counselor, including stressors (financial, relationship/marital, or medical); mental and behavioral health history of child and family; parent-reported school performance; family structure; insurance; weight management history; amount of sedentary activity; and physician assessment of weight-related co-morbidities. Follow-up data are entered every 4 months during the physician reassessment. Patients are considered Inactive if they: (1) Self-identified as dropping out of the program, or (2) missed or cancelled a visit and did not reschedule, despite two phone calls and a letter over a month requesting an appointment. If families notify the program of their intention to drop out, they are asked why; this is recorded in the database. If families cannot be contacted, they are deemed “lost to follow-up.”
The database was approved by the Wake Forest University Health Sciences Institutional Review Board.
Study Design
All patients (Active and Inactive) seen between November 7, 2007 (program initiation), and July 7, 2009, were included in this study and then followed for 4 months of treatment. Attrition was measured during the initial 4-month intensive phase of the program (eight total visits: Intake visit, six visits with treatment team, then review visit with physician).
A one-page survey was mailed to the parents/caregivers of all Inactive patients asking reasons for dropout. Response options were measured on a three-point Likert scale, and four open-response questions: (1) The most important reason for not returning to the program, (2) reasons for not returning, (3) what would help their family return, and (4) what would help their family stay in the program. They were also asked if they would like to return to the program. Surveys were anonymous and not linked to individual patients.
Data Analysis
Descriptive statistics were used to describe the sociodemographic, physical, and mental health characteristics of the population. Initial analyses were performed to identify significant relationships between potential predictor variables and the primary outcome program status (Active, Inactive). Chi-squared and Fisher exact tests were used to compare proportions of discrete variables between active and inactive participant groups. Means of continuous variables were compared with two-sample t-tests.
Multivariable logistic regression was used to identify independent correlates of program status, modeled as follows: Variables with potential associations identified in bivariable analysis (p<0.1); variables identified in similar studies; and those with clinical significance (age, race/ethnicity, gender) were further studied by logistic regression. Finally, linear regression was used when number of visits was the dependent variable.
All statistical analyses were performed using SAS Enterprise Guide© version 4 with SAS© version 9.1 (Cary, NC). This study was approved by the Wake Forest University School of Medicine Institutional Review Board.
Results
Study Participant Characteristics
During the study period, 133 patients and families were seen for initial evaluation. The mean patient age was 12 years, with slightly more girls than boys (Table 1). Slightly more than half were African American, Hispanic, or other (52%). “Other” included Asian, Southeast Asian, and Middle Eastern. Over half of the families had two caregivers in the home (both parents or parent/stepparent). Families, on average, lived approximately 30 min from the program site, with a range of 1.3–99 miles. Many families reported experiencing stressors in the family; 71% had at least one significant household stressor.
Table 1.
Characteristics of Children and Families Included in Study
| Variable | Total (N=133) |
|---|---|
| Mean age±SD, years | 12±3.4 |
| Gender, % (N) | |
| Female | 53% (70) |
| Male | 47% (73) |
| Race/ethnicity | |
| White | 48% (64) |
| African-American | 32% (43) |
| Hispanic | 14% (19) |
| Other | 5% (7) |
| Parent structure | |
| Dual parent | 58% (76) |
| Single parent | 36% (47) |
| Relative | 4% (5) |
| Divorced, joint placement | 1% (1) |
| Foster | 2% (3) |
| Other (group home) | 1% (1) |
| Family structure | |
| Number of adults in household, mean±SD | 1.8±0.6 |
| Number of children in household, mean±SD | 2.2±1 |
| Insurance | |
| Commercial | 46% (61) |
| Medicaid | 50% (66) |
| Other | 4% (5) |
| Distance of family home from clinic, miles±SD | 25±22 |
| Stressors present in family | |
| Medical (N=125) | 23% (29) |
| Financial (N=127) | 47% (60) |
| Relationship (N=127) | 48% (61) |
| Other (N=121) | 15% (18) |
| Parent mental health history | |
| Parent with history of mental health treatment (N=126) | 29% (36) |
| Parent presently in treatment (N=125) | 23% (29) |
| Child mental health history | |
| History of mental health treatment (N=132) | 30% (40) |
| Presently in treatment (N=132) | 18% (24) |
| Psychotropic medications (N=133) | 13% (17) |
| School and development | |
| Special education received in school | 17% (22) |
| Average or above average performance in school | 78% (101) |
| Developmental delay | 14% (19) |
| Weight status, mean±SD | |
| BMI, kg/m2 | 38±10 |
| BMI z-score | 2.617±0.474 |
| Fasting serum studies, mean±SD | |
| Insulin (N=82) | 34±31 |
| Total cholesterol (N=122) | 167±32 |
| LDL-C (N=118) | 102±27 |
| HDL-C (N=122) | 41±9 |
| Triglycerides (N=119) | 125±81 |
| Mean number of weight-related co-morbidities | 3.9±2 |
| Major weight-related co-morbidity* | 43% (57) |
| Asthma, present diagnosis | 26% (34) |
| Self-reported hours of sedentary activity, mean±SD | 4.4±2.6 |
| History of weight management attempt, parent | 42% (56) |
| History of weight management attempt, child | 36% (48) |
Type 2 diabetes, polycystic ovary syndrome, Blount disease, slipped capital femoral epiphysis, obstructive sleep apnea, pseudotumor cerebri, hypertension.
Note: Rounding may lead to group totals being more than 100%.
SD, Standard deviation; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol.
Nearly a third of children had a history of mental health treatment (other than attention-deficit/hyperactivity disorder [ADHD]): 11% had depression, and 9% had some other form of mental illness, including anxiety, obsessive compulsive disorder, oppositional defiant disorder, and bipolar disorder. Nearly a third of parents/caregivers also had a history of mental health treatment, with depression the most common diagnosis. A total of 48% of parents reported cigarette use, 38% reported alcohol use (but not necessarily problematic use), and 7% used recreational drugs.
Children had a mean BMI of 38 kg/m2 (z-score of 2.617, 99th percentile). The average patient had nearly four weight-related co-morbidities, with almost half having a major or symptomatic weight-related co-morbidity. Those with a previous weight management attempt had primarily used either a commercial program (17%) or a specific diet (17%). Only 6% had attempted an exercise program or joined a gym. Only 2 children had taken prescription medication or herbal supplements for treatment of obesity.
Attrition
In all, 42 patients dropped out in the first 4 months of treatment (32%), a similar range to other comparable clinical programs that have reported attrition (Table 2). Inactive patients were significantly older than Active patients, but there were no differences by race/ethnicity or other sociodemographic factors, although this may have been influenced by the sample size (Table 3). Active and inactive groups did differ in health characteristics (Table 4). A child and parent history of mental health treatment approached significance (p=0.07 and 0.08, respectively), with the Inactive group having a higher proportion of mental health treatment. Inactive patients had significantly lower BMI z-scores than Active patients. Parent-reported school performance was also significantly associated with attrition, with Inactive patients more likely to have below-average school performance.
Table 2.
Attrition Rates in Tertiary Care, Multidisciplinary Pediatric Weight Management Clinics
| N | Attrition Rate | Attrition Parameters | |
|---|---|---|---|
| Barlow (9) | 157 | 61% | ≤2 visits in monthly clinic |
| Cote (10), Zeller (16) | 120, 212 | 55% | Failure to complete initial 12- to 16-week phase of program, weekly visits |
| Skelton (13) | 248 | 73% | ≤4 visits to program over 9–12 months of monthly clinic |
| Tershakovec (15) | 518 | 49% | ≤2 visits to monthly clinic |
| Brenner FIT | 133 | 32% | Failure to complete initial 4 months of program, biweekly visits |
Table 3.
Family Sociodemographic Characteristics, by Attrition Status at 4 Months of Treatment
| Variable | Active (N=91) | Inactive (N=42) | p |
|---|---|---|---|
| Mean age±SD, years | 11±3.7 | 13±2.5 | 0.004 |
| Gender, % (N) | |||
| Female | 54% (49) | 50% (21) | NS |
| Male | 46% (42) | 50% (21) | |
| Race | |||
| White | 48% (44) | 48% (20) | NS |
| African-American | 26% (24) | 45% (19) | NS |
| Hispanic | 18% (16) | 7% (3) | NS |
| Parent structure | |||
| Dual parent household | 60% (55) | 50% (21) | NS |
| Single parent household | 40% (36) | ||
| Insurance | |||
| Commercial | 51% (46) | 36% (15) | NS |
| Medicaid | 47% (42) | 57% (24) | |
| Other | 2% (2) | 7% (3) | |
| Distance from program, miles | 25.5±21.1 | 24.5±24.1 | NS |
SD, Standard deviation; NS, not significant at the level of p<0.05.
Table 4.
Physical and Mental Health Characteristics of Families, by Attrition Status at 4 Months of Treatment
| Variable | Active (N=91) | Inactive (N=42) | p |
|---|---|---|---|
| Stressor present in family | 71% (65) | 71% (30) | NS |
| Parent mental health history | |||
| Parent with history of mental health treatment (N=126) | 23% (20) | 40% (16) | 0.082 |
| Parent presently in treatment (N=125) | 19% (16) | 33% (13) | NS |
| Child mental health history | |||
| History of mental health treatment (N=132) | 25% (23) | 42% (17) | 0.069 |
| Presently in treatment (N=132) | 17% (15) | 22% (9) | NS |
| Psychotropic medications (N=133) | 12% (11) | 14% (6) | NS |
| School and development | |||
| Special education received in school | 14% (12) | 24% (10) | NS |
| Average or above average performance in school | 84% (74) | 64% (27) | 0.02 |
| Developmental Delay | 13% (12) | 17% (7) | NS |
| Weight status, mean±SD | |||
| BMI, kg/m2 | 37.8±10.7 | 38.5±8.7 | NS |
| BMI z-score | 2.663±0.526 | 2.515±0.317 | 0.047 |
| Systolic blood pressure, mean±SD, mmHg | 118±11 | 122±11 | 0.051 |
| Diastolic blood pressure | 70±11 | 72±8 | NS |
| Fasting serum studies, mean±SD | |||
| Insulin (N=82) | 32.8±33.5 | 37.3±23.9 | NS |
| Total cholesterol (N=122) | 166.9±34.3 | 166.2±26 | NS |
| LDL-C (N=118) | 101.8±28.4 | 102.6±24.6 | NS |
| HDL-C (N=122) | 39.8±9.2 | 43.6±9.6 | 0.038 |
| Triglycerides (N=119) | 130.2±82.1 | 112.8±79.6 | NS |
| Mean number of weight-related co-morbidities | 3.9±2 | 4.1±1.9 | NS |
| Major | 60% (34) | 40% (23) | 0.089 |
| Asthma, present diagnosis | 23% (21) | 31% (13) | NS |
| Self-reported hours of sedentary activity, mean±SD | 4.1±2.6 | 4.8±2.6 | NS |
| History of weight management, parent | 43% (39) | 41% (17) | NS |
| History of weight management, child | 32% (29) | 45% (19) | NS |
NS, Not significant at the level of p<0.1; SD, standard deviation; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Regression Analysis
Variables with potential association (p<0.1) with Inactive status in bivariable or unadjusted analysis were included in the model (age, child with history of mental health treatment, parent with history of mental health treatment, school performance, BMI z-score, systolic blood pressure, presence of major weight-related co-morbidity). Also, variables identified in similar studies (insurance, race/ethnicity, single-parent household), and with a high likelihood of significance (gender, distance from treatment program) were included. High-density lipoprotein cholesterol (HDL-C) was removed from the model due to missing data and being unlikely to have clinical significance, despite having significance in bivariable analysis.
After logistic regression of the full model, systolic blood pressure, single-parent household, and child with a history of mental health treatment had the highest p values and very wide confidence intervals (CIs), reflecting an excessive number of variables in the model. Upon removing those variables, we achieved an improved fit by diagnostic testing, finding BMI z-score (odds ratio [OR] estimate 0.143, 95% CI 0.033, 0.621), commercial insurance (0.032, 95% CI 0.002, 0.583), average school performance (0.046, 95% CI 0.001, 4.865), and the presence of a weight-related co-morbidity (0.358, 95% CI 0.135, 0.945) to be significant (p<0.05). Similar to bivariate analysis, those with a higher BMI z-score had lower odds of being inactive, as did those with commercial insurance coverage, average school performance, and a major weight-related co-morbidity.
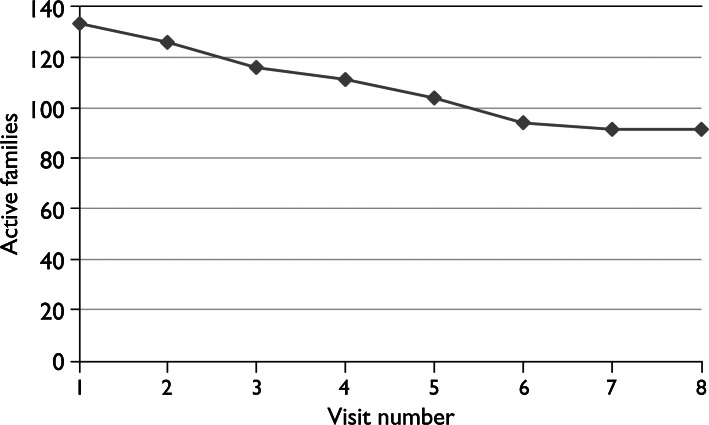
Duration of Program Participation
Inactive participants had a mean of 3.3±1.6 visits before dropping out. Five percent (n=7) never returned after the intake visit. The distribution of visits in the Inactive group was fairly even, with 52% of dropouts by the 4th visit, and 93% by the 5th visit (Figure 1). Exploratory analysis was performed on the number of visits before dropout and likely predictive variables using the same model as for Active/Inactive groups. There were no significant associations between number of visits and candidate variables by linear regression, nor were there differences in early (3 visits or less) or late (4 or more visits) dropouts by comparative tests or logistic regression.
Figure 1.
Active families by visit number (N=133).
Parent/Caregiver Reasons for Attrition
Only 9 of the 42 families who dropped out informed the program they were doing so at the time of dropout. Of the 9, 4 cited they were dissatisfied with the program; 2 reported the distance traveled to the program was too great, 2 indicated that the child was not participating in treatment, and 1 did not provide a reason. A total of 33 (79% of Inactive patients) did not return for an appointment and did not respond to requests (two phone calls, letter) to reschedule.
Of the 42 Inactive families, 23 (55%) returned a completed survey (Table 5). Issues related to expectations and satisfaction were reported most frequently as contributing “a lot” or “a little” to the family not returning: “My child's weight was not getting better” (64%), “program did not meet my expectations” (48%), “program did not meet my child's expectations” (52%), and “my child wanted to leave the program” (41%). A total of 64% of respondents said “my child was not ready to make changes,” but only 19% noted that the family was not ready to make changes. Programmatic issues (e.g., insurance, cost, too much time, distance, and appointment times) were less frequently noted as reasons for dropout, although a third of respondents reported problems with transportation contributed “a lot.” In addition 41% noted too much missed school, with an equal number reporting too much missed work, although this was reported as less problematic. When asked the most important reasons for not returning, responses were “my child was not ready to make changes” (n=7) and “my child's weight was not getting better” (n=6). Only half of respondents answered the questions, “What could Brenner FIT do to help your family return to the program?” and “What could Brenner FIT do to help your family stay in the program.” There were no commonalities or patterns in these responses.
Table 5.
Parent-Reported Reasons for Dropout (N=23)
| A Lot (%) | A Little (%) | Not At All (%) | |
|---|---|---|---|
| My child was not ready to make changes | 36 | 27 | 36 |
| My child's weight was not getting better | 36 | 27 | 36 |
| Program did not meet my child's expectations | 22 | 30 | 48 |
| Program did not meet my expectations | 17 | 30 | 52 |
| My child wanted to leave the program | 18 | 23 | 59 |
| My child was missing too much school | 14 | 27 | 59 |
| Parents/caregivers missing too much work | 18 | 23 | 59 |
| Program too far away from our home | 14 | 23 | 64 |
| Program costs too much money (i.e., parking, travel, co-pays for insurance) | 14 | 23 | 64 |
| Problems with transportation | 32 | 5 | 64 |
| Program took too much time | 5 | 27 | 68 |
| Appointments not at convenient times | 5 | 27 | 68 |
| Visits to program not frequent enough | 0 | 27 | 73 |
| Family crisis and had to stop | 14 | 9 | 77 |
| Program not what we were looking for | 9 | 13 | 78 |
| My family was not ready to make changes | 0 | 19 | 81 |
| Difficulty with insurance coverage | 0 | 9 | 91 |
Note: Rounding may lead to group totals being more or less than 100%.
Discussion
This report of an intensive multidisciplinary pediatric weight management clinic highlights several important issues in the treatment of pediatric obesity. Children referred for weight management often have significant health issues. This population nearly met the criteria for morbid obesity (BMI≥40 kg/m2) in adults despite being only 12 years of age. Most families reported a major stressor in the family. A quarter of parent/caregivers reported mental health issues, and nearly a third of children had a history of mental health treatment. Even with cost to families being minimized, a third of families dropped out during the initial, intensive phase of treatment.
The attrition rate, and associated variables, was similar to other programs (Table 2). While overall there were few major differences between Active and Inactive groups, our cohort had some similarities to the few others series reported. Aside from obesity levels and attrition, African-American race/ethnicity was predictive in other studies,15,16,18 as was insurance16 and poorer physical and mental health status of the child.9,10,16 Our study demonstrated that more obese children with weight-related health issues were less likely to be Inactive, which could be viewed as positive, suggesting that more severely affected children remained in treatment. Our findings implied that children with Medicaid insurance coverage and poor school performance were more likely to drop out, similar to the other studies discussed. Interestingly, this severely obese and diverse population, many of whom reported mental health issues, being from single-parent households, and having to travel for 30 min or more to the clinic, remained engaged in treatment more than reported in the literature (Table 2). The lack of a difference in racial/ethnic makeup between the groups (despite having no team member of color), suggests that a multidisciplinary, family-centered approach may prevent higher rates of attrition15,16,18 Other clinics have reported families of older children being more likely to drop out of treatment,16 which is consistent with adolescents gaining independence and playing a greater role in decision making. Cost was not identified as a major contributor to dropout, likely due to Brenner FIT minimizing family expenses in treatment. We believe this allowed us to better identify family and clinic contributors to attrition.
A surprising finding was that the Active group was more obese than the Inactive group. Other clinics have found a higher BMI associated with dropout.9,11,16,18 The reason for larger children being more likely to remain in treatment is not known, but it could be those with higher body weights may have greater reason for participation. Less obese children and their families may have experienced quicker success and believed they could manage weight issues on their own. A strong association with Active status was average or above average performance in school. Despite having no significant differences between groups by developmental delay or receipt of special education, poorer school performance may represent other troubles in the child that could diminish the family's ability to participate in an intensive weight management clinic.
Our study had limitations. Although we lacked a comparison group in this study, participant characteristics may be informative to those approaching childhood obesity in a family-centered manner. Many of the variables explored, such as family stressors and child school performance, were based on family report to clinical questions, even though they are part of a standardized interview. The team uses well-defined protocols, but treatment approaches are tailored to the patient and family, so our findings may not apply to all obesity treatment programs. Medicaid insurance was used as a marker for socioeconomic status and may not accurately reflect the financial or educational status of patients and families. A component of this study is prospective, because data are entered into the database continuously during treatment and the status of patients tracked closely. However, we also gathered data retrospectively. Clinical databases can be a valuable tool in evaluating clinical effectiveness and outcomes.26 In the case of weight management, databases can be useful in measuring the dissemination of clinical trials performed in homogeneous populations.27–29 Finally, the relatively small sample size limits our ability to identify correlates of attrition, as does the short-term follow-up.
Unique among other reports from weight management clinics, in our study clinic costs were billed to insurance only. Families with commercial insurance were responsible for co-payments to see the physician twice during the study (initial and eighth visit), and few families reported costs or difficulties with insurance as reasons for attrition. These findings indicate financial issues related to participating in clinic were likely minimized in this study, allowing for a “cleaner” evaluation of attrition.
Attrition increases the difficulty of determining treatment effectiveness, as lack of success appears to contribute to dropout. The study of predictors of attrition—especially among families at increased risk of dropout—may reveal better treatment approaches designed to engage and retain families. Furthermore, exploring what aspects of a treatment program contribute to dropout, such as inconvenient appointment times, could improve both programs and outcomes. Finally, child and family expectations of treatment, shown here to be an important component of dissatisfaction, deserve further focus as a means to improve adherence to treatment regimens. In particular, parents report child-focused areas contributing to dropout, such as lack of success in weight management and child not wanting to return. In a family-based program, the role of the child in treatment may need to be better defined. Parent-only treatment has shown promise in improving weight status, and could impact attrition.30,31 Alternatively, because older children appear more likely to drop out, designing interventions to better engage children, possibly using peer support, may keep them better engaged in treatment. The present study adds to the small body of literature in this area, providing additional evidence upon which to address this important problem.
Conclusion
Attrition from pediatric weight management programs is high and needs further investigation. While family-focused treatment appears to reduce attrition rates, identifying children and families at risk of dropout may allow tailored interventions that better meet such families' needs. Furthermore, identifying treatment program characteristics that contribute to dissatisfaction and attrition could result in improved retention of participants. These findings may improve both pediatric weight management attrition and outcomes, and may apply to other areas of health.
Acknowledgments
Dr. Skelton was supported in part by a grant from The Duke Endowment (No. 6110-SP) and by NICHD/NIH Mentored Patient-Oriented Research Career Development Award (K23 HD061597).
The authors would like to thank Karen Klein (Research Support Core, Office of Research, Wake Forest University Health Sciences) for her assistance in editing this manuscript, and Megan Bennett Irby (Brenner FIT Program) for her assistance in the conduct of the study.
Author Disclosure Statement
No financial disclosures were reported by the authors of this paper.
References
- 1.Ogden CL. Carroll MD. Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Troiano RP. Flegal KM. Overweight children and adolescents: Description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 3.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 4.Davis MM. Gance-Cleveland B. Hassink S, et al. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 5.Krebs NF. Himes JH. Jacobson D, et al. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S193–228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 6.Spear BA. Barlow SE. Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 7.Barlow SE. Trowbridge FL. Klish WJ, et al. Treatment of child and adolescent obesity: Reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110:229–235. [PubMed] [Google Scholar]
- 8.Kitscha CE. Brunet K. Farmer A, et al. Reasons for non-return to a pediatric weight management program. Can J Diet Pract Res. 2009;70:89–94. doi: 10.3148/70.2.2009.89. [DOI] [PubMed] [Google Scholar]
- 9.Barlow SE. Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr (Phila) 2006;45:355–360. doi: 10.1177/000992280604500408. [DOI] [PubMed] [Google Scholar]
- 10.Cote MP. Byczkowski T. Kotagal U, et al. Service quality and attrition: An examination of a pediatric obesity program. Int J Qual Health Care. 2004;16:165–173. doi: 10.1093/intqhc/mzh015. [DOI] [PubMed] [Google Scholar]
- 11.Denzer C. Reithofer E. Wabitsch M, et al. The outcome of childhood obesity management depends highly upon patient compliance. Eur J Pediatr. 2004;163:99–104. doi: 10.1007/s00431-003-1376-7. [DOI] [PubMed] [Google Scholar]
- 12.Kirk S. Zeller M. Claytor R, et al. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13:876–882. doi: 10.1038/oby.2005.101. [DOI] [PubMed] [Google Scholar]
- 13.Skelton JA. Demattia LG. Flores G. A pediatric weight management program for high-risk populations: A preliminary analysis. Obesity. 2008;16:1698–1701. doi: 10.1038/oby.2008.243. [DOI] [PubMed] [Google Scholar]
- 14.Sothern MS. Schumacher H. von Almen TK, et al. Committed to kids: An integrated, 4-level team approach to weight management in adolescents. J Am Diet Assoc. 2002;102:S81–S85. doi: 10.1016/s0002-8223(02)90429-3. [DOI] [PubMed] [Google Scholar]
- 15.Tershakovec AM. Kuppler K. Ethnicity, insurance type, and follow-up in a pediatric weight management program. Obes Res. 2003;11:17–20. doi: 10.1038/oby.2003.4. [DOI] [PubMed] [Google Scholar]
- 16.Zeller M. Kirk S. Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Grossi E. Dalle Grave R. Mannucci E, et al. Complexity of attrition in the treatment of obesity: Clues from a structured telephone interview. Int J Obes. 2006;30:1132–1137. doi: 10.1038/sj.ijo.0803244. [DOI] [PubMed] [Google Scholar]
- 18.Heinberg LJ. Kutchman EM. Lawhun SA, et al. Parent involvement is associated with early success in obesity treatment. Clin Pediatr. 2009;49:457–465. doi: 10.1177/0009922809337531. [DOI] [PubMed] [Google Scholar]
- 19.Oude Luttikhuis H. Baur L. Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Skelton JA. Beech BM. Attrition in pediatric weight management: A review of the literature and new directions. Obes Rev. 2011;12:e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Savoye M. Shaw M. Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA. 2007;297:2697–2704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 22.Tershakovec AM. Watson MH. Wenner WJ, Jr., et al. Insurance reimbursement for the treatment of obesity in children. J Pediatr. 1999;134:573–578. doi: 10.1016/s0022-3476(99)70243-x. [DOI] [PubMed] [Google Scholar]
- 23.De Santis-Moniaci D. Altshuler L. Comprehensive behavioral treatment of overweight and the pediatric practice. Pediatr Ann. 2007;36:102–108. doi: 10.3928/0090-4481-20070201-09. [DOI] [PubMed] [Google Scholar]
- 24.Irby M. Kaplan S. Garner-Edwards D, et al. Motivational interviewing in a family-based pediatric obesity program: A case study. Fam Syst Health. 2010;28:236–46. doi: 10.1037/a0020101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross MM. Kolbash S. Cohen GM, et al. Multidisciplinary treatment of pediatric obesity: Nutrition evaluation and management. Nutr Clin Pract. 2010;25:327–234. doi: 10.1177/0884533610373771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Padkin A. Rowan K. Black N. Using high quality clinical databases to complement the results of randomised controlled trials: The case of recombinant human activated protein C. BMJ. 2001;323:923–926. doi: 10.1136/bmj.323.7318.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Epstein LH. Paluch RA. Roemmich JN, et al. Family-based obesity treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychol. 2007;26:381–391. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Epstein LH. Valoski A. Wing RR, et al. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264:2519–2523. [PubMed] [Google Scholar]
- 29.Epstein LH. Valoski A. Wing RR, et al. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373–383. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- 30.Golan M. Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004;62:39–50. doi: 10.1111/j.1753-4887.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 31.Golan M. Crow S. Targeting parents exclusively in the treatment of childhood obesity: Long-term results. Obes Res. 2004;12:357–361. doi: 10.1038/oby.2004.45. [DOI] [PubMed] [Google Scholar]