Abstract
Context
Terminal hospitalizations are costly and often avoidable with appropriate advance care planning.
Objectives
This study examined the association between advance care planning, as measured by facility rate of do not resuscitate (DNR) orders in U.S. nursing homes (NHs) and changes in terminal hospitalization rates.
Methods
Retrospective cohort study of the changing prevalence of DNR orders in U.S. NHs. Using a fixed effect multivariate model, we examined whether increasing facility rate of DNR orders correlates with reductions in terminal hospitalizations in the last week of life, controlling for changes in facility characteristics (staffing, use of NP/PA, case mix of nursing residents, admission volume, racial composition, payer mix).
Results
The average facility rate of terminal hospitalizations was 15.5%, fluctuating between 1999 (15.0%) and 2007 (14.8%). NHs starting with low rates of DNR orders that increased their rates had fewer terminal hospital admissions in 2007 (11.2%) than facilities with continuously low DNR usage. Even after applying a multivariate fixed effect model, the effect of changes in facility DNR order rate on terminal hospitalization was −0.056 (95% confidence interval: −0.061, −0.050), indicating that for every 10% increase in DNR orders there was 0.56% decrease in terminal hospitalizations. This rate can be compared with the increase of 0.70% in the terminal hospitalization rate when an NH became disproportionately dependent on Medicaid funding or the 0.40% decrease in terminal hospitalization rate associated with adding a nurse practitioner to the clinical staff complement.
Conclusion
NHs that changed their culture of decision making by increasing their facility rate of DNR orders decreased their rate of terminal hospitalizations.
Keywords: Do not resuscitate, advance care planning, terminal hospitalizations
Introduction
Advance care planning has been promoted as means for persons to state their wishes in preparation for a future period of potential incompetence.1 This practice of educating patients about their condition and prognosis, ascertaining their preferences for care in the present and future, and formulating a plan of care is thought to lead to an ethically acceptable reduction in health care costs. Considerable resources, such as the mandates of the 1990 Patient Self-Determination Act (PSDA), have been devoted to educating the public about their right to participate in medical decisions and to complete written advance directives to legally state their wishes for either a proxy decision maker and/or provide specific instructions for medical care.
The outcomes of cardiopulmonary resuscitation in nursing homes (NHs) are poor and studies find that less than two in 100 NH residents have a successful resuscitation attempt.2-5 Often, advance care planning in the NH setting starts with a discussion and decision about resuscitation, with later dialogue focusing on restriction of other life-sustaining treatments. In our previous research, the facility rate of do not resuscitate (DNR) orders has been used as a measure of the decision-making culture of that NH facility. Previously, we noted that NHs with higher facility rates of DNR orders had lower rates of feeding tube use and hospitalization.6,7 In both of these studies, the facility rate of DNR orders was used as a marker of the culture of decision making or advance care planning, given the poor outcomes of resuscitation in the NH setting.
Only two studies have examined the changing rate of DNR orders. Both examined the changes post PSDA. Teno et al.8 found an increase in the rate of DNR orders in NH residents, whereas Baker et al. focused their study on hospitals in Ohio and did not find an increase in the rate of DNR orders.9 The goal of this article was to determine if the use of DNR orders in NHs had changed from 1999 to 2007 and to determine whether facility changes in the culture of decision making (as measured by the NH facility rate of DNR orders) were associated with a reduction in terminal hospitalizations for NH residents.
Methods
Study Population
All Medicare- and Medicaid-certified U.S. NHs are required to submit the minimum data set (MDS) resident assessment data, which contains information on DNR orders, orders to forgo hospitalizations, artificial hydration and nutrition, and data on the use of written advance directives. These data are collected at the time of admission, yearly, and when a change occurs in the status of the patient. We created two aggregated measures that differ on data sources. The first aggregated measure, the facility rate of DNR orders, used all MDS assessments closest to the first Thursday in April. For this aggregated measure, the NH must have had at least 25 NH residents. By statistical convention, 25 is chosen as the minimum number of subjects required to examine a facility rate. A second aggregated measure examined the facility rate of terminal hospitalizations for NH residents aged 66 years and older with Medicare insurance. The age 66 years was chosen so that there would be at least one year’s worth of data. For the second aggregated measure, we matched MDS and Medicare enrollment and inpatient hospitalization data. To calculate the facility rate of terminal hospitalizations, we required a minimum of 25 deaths of Medicare beneficiaries in a calendar year in which a person resided in an NH at least eight days prior to death. Both of these facility aggregate measures were examined from 1999 to 2007. This research project was approved by the Institutional Review Board of Brown University, Providence, RI, with waiver of informed consent.
NH Characteristics
NH characteristics were obtained from the Online Survey Certification and Reporting System (OSCAR) and by aggregating MDS resident records at the facility level. The Centers for Medicare & Medicaid Services requires each state to inspect participating NHs annually. The OSCAR database allowed us to obtain characteristics of the NH that included 1) registered nurse (RN) and licensed practical nurse (LPN) staffing; 2) certified nursing assistant (CNA) staffing; 3) use of a physician extender (e.g., nurse practitioner or physician assistant); and 4) the payer mix of self-pay, Medicare and Medicaid reimbursement sources. Facility aggregates of MDS data were used to characterize the changing case mix of the overall NH resident population. These were measured by Resource Utilization Groups (RUGs), the volume of NH admissions, the average age of residents, activities of daily living (ADL) scores using the 0–28-point scale, the percent of residents that were bedfast, the percent of residents walking independently, the percent of residents with advanced cognitive impairment as measured by a Cognitive Performance Score of 5 or 6, and the racial composition of NH residents as assessed by a nurse completing the MDS at the time of admission or annual assessments.
Statistical Analysis
Descriptive analysis was used to examine the temporal trend in rate of DNR orders, orders to forgo hospitalization, use of advance directives, and orders to forgo artificial hydration and nutrition. The change in facility DNR orders is described by reporting the distribution by year with the use of box plots. This was conducted among the 15,784 NHs that had at least 25 residents on the first Thursday of April. Two-hundred fifteen facilities were eliminated because of missing DNR orders and a further 2042 facilities were eliminated because they did not meet the inclusion criteria of having at least 25 residents.
We used descriptive univariate analyses and a fixed effect multivariate analysis to examine the association of the facility change in DNR orders and terminal hospitalizations among the 8583 NHs. For descriptive purposes, we examined the univariate associations of the rate of terminal hospitalizations in the last week of life with a characterization of the changing rates of NHs’ DNR order use between 1999 and 2007 in the following categories: 1) NHs that remained consistent in the lowest third of DNR order use in 1999 and 2007; 2) NHs that went from lower to middle third, but did not change by more than 15%; 3) NHs that went from lower to medium third, but improved by 15% or greater; 4) NHs that remained in the middle at both the time periods but did not drop by more than 15%; 5) NHs that remained in the middle third, but improved by at least 15%; 6) NHs that dropped from high to middle with decreases of at least 15%; 7) NHs that dropped to middle third, but did not decrease by more than 15%; 8) NHs that went from lowest to highest third in 2007; and 9) NHs that remained persistently highest third in both the time periods.
The association of the facility’s changing rate of DNR orders with terminal hospitalizations was examined using a multivariate fixed effect model, using longitudinal data for 8583 NHs with at least 25 deaths per year, in which the NH resident had resided in that NH within eight days of death. The data were adjusted for organizational characteristics and aggregate characteristics that changed over time. Unlike a random effect or a pooled least squares model, the fixed effect (within facility) model allows us to obtain unbiased estimates of the effect of the NH rate of DNR orders in the presence of unobserved time-invariant NH characteristics in influencing both terminal hospitalizations and the facility rate of DNR orders.10
Results
The temporal trends of DNR orders and other orders to forgo life-sustaining treatment were examined among all NH residents residing in NHs with at least 25 residents. Between 1999 and 2007, there were a total of 17,826 NHs submitting MDS data. Of these NHs, there were 15,784 NHs with at least 25 residents on the first Thursday in April of any given year.
Table 1 characterizes the 15,784 NHs that met the cut-off of 25 NH residents. Additionally, Table 1 provides the characteristics of the NHs that submitted data in 1999 (n = 15,146) and 2007 (n = 14,854). Overall, the NHs were urban, for profit, and nearly one-half were part of a chain. About one in 10 (11.1%) were considered low resource secondary to enrolling a disproportionate number of patients that had only Medicaid insurance. Over time, the number of admissions, the use of nurse practitioners, and the RUG scores have increased. Additionally, there was a slight decrease in the number of NHs identifying as low resource facilities secondary to serving a disproportionate share of Medicaid-funded residents.
Table 1.
Characteristics of NHs and Change Between 1999 and 2007
| NH Characteristics | Overall (n = 15,784) |
NH in 1999 (n = 15,146) |
NH in 2007 (n = 14,854) |
|---|---|---|---|
| Urban location | 68.2 | 68.1 | 68.7 |
| For profit | 68.1 | 67.9 | 69.0 |
| Part of chain | 54.7 | 56.7 | 54.2 |
| Has dementia unit | 18.9 | 17.3 | 18.6 |
| Number of beds (mean, SD) | 109.7 (65.1) | 110.0 (66.8) | 110.1 (63.1) |
| Disproportionate share of Medicaid patients | 11.1 | 13.9 | 7.6 |
| Average age of NH residents in facility (mean, SD) | 80.8 (6.5) | 81.5 (6.1) | 80.4 (6.8) |
| Average ADL score (0–28, mean, SD) | 15.5 (3.1) | 15.2 (3.1) | 15.9 (3.0) |
| Percent of NH residents bedfast (mean, SD) | 5.2 (7.2) | 7.2 (8.3) | 4.3 (6.3) |
| Percent of NH residents walking independently (mean, SD) | 17.5 (14.4) | 20.0 (14.4) | 14.7 (13.7) |
| Percent of NH residents with advance cognitive impairment (mean, SD) | 20.0 (12.2) | 23.3 (12.2) | 16.7 (16.6) |
| Black NH residents (%, mean, SD) | 10.5 (18.0) | 9.6 (17.0) | 11.2 (18.4) |
| Hispanic NH residents (mean rate, SD) | 3.2 (9.3) | 2.6 (8.1) | 3.7 (10.1) |
| Nurse practitioner of physician assistant | 25.4 | 19.2 | 30.6 |
| RN staffing (mean hours per days per resident, SD) | 0.37 (0.50) | 0.43 (0.74) | 0.33 (0.46) |
| LPN staffing (mean hours per day, per resident, SD) | 0.74 (0.60) | 0.72 (0.79) | 0.81 (0.62) |
| CNA staffing (mean hours per days per resident, SD) | 2.2 (0.89) | 2.1 (1.2) | 2.2 (0.82) |
| Number of admissions (mean, SD) | 160.2 (164.3) | 138.4 (154.8) | 175.1 (168.1) |
| Resource utilization group (mean, SD) | 0.81 (0.10) | 0.78 (0.10) | 0.83 (0.10) |
Time Trend Change in the Rates of DNR Orders and Terminal Hospitalizations
Fig. 1 presents changes in the rate of DNR orders in the study’s facilities between 1999 and 2007. DNR orders showed a slight increase from 53.5 in 1999 to 55.5 in 2007. Among those residents with advanced cognitive impairment, the rate of DNR orders increased from 65.3% to 70.7%. There was no significant trend with do not hospitalize (DNH) orders, with rates in all years below 4%. Orders to forgo artificial hydration and nutrition remained unchanged at about 11%. Even among persons with advanced cognitive impairment, the rate of orders to forgo artificial hydration and nutrition changed only from 11.6% to 13.0%. Although there was no substantial change in overall facility DNR orders, individual NHs did demonstrate large changes and variations in their use of DNR orders. For example, 18.3% of facilities increased DNR orders by at least 15%, whereas 19.0% decreased their rate of DNR orders by the same margin.
Fig. 1.
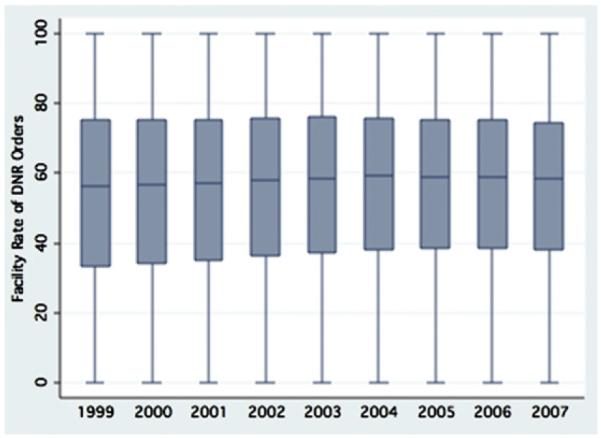
Change in the NH rate of DNR orders between 1999 and 2007.
Association of Facility Change in DNR Orders with Terminal Hospitalizations
The association of NH facility change in DNR orders with the facility rate of terminal hospitalizations was examined among NHs that had at least 25 deaths per year, with residents residing in the facility within eight days of death. There were 8583 NHs that met the study’s criteria. Excluded NHs were more likely to be located in rural areas (39.7% vs. 22.1%, P < 0.001) and they were less likely to be for profit (62.0% vs. 68.1%, P < 0.001) or a part of a chain of NHs (49.2% vs. 58.3%, P < 0.001). Additionally, these facilities had a smaller number of beds (mean of 69.2 vs. 135.1, P < 0.001). Fig. 2 examines the changing rate of terminal hospitalizations among those NHs that have at least 25 deaths a year. As can be seen, there was only a slight decrease in the rates of terminal hospitalization in the last week of life, going from 15.0% to 14.8%. Overall, approximately one in seven NH residents had a terminal hospitalization in the last seven days of life.
Fig. 2.
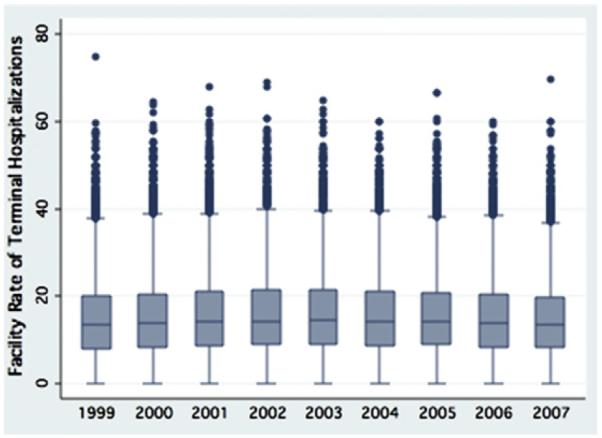
Change in the NH rate of terminal hospitalizations between 1999 and 2007.
Although the overall DNR order rate did not demonstrate a substantial change in the time period, individual NHs did change their rate of DNR orders. Examining those 7674 facilities meeting eligibility criteria and reporting data in 1999 and 2007, 1190 (15.5%) consistently remained in the highest third rate of DNR orders, whereas 549 (7.1%) facilities remained in the lowest third. Only 46 facilities improved from the lowest third in 1999 to the highest third in 2007. Most NHs (n = 2696, 35.1%) remained in the middle third, with changes of less than 15% in their rate of DNR use. Seven hundred seventy-two NHs (10%) started out in 1999 in the middle third and dropped by 15% points.
For descriptive purposes, we examined the univariate associations of the rate of terminal hospitalizations in the last week of life with characterization of the changing rates of NHs’ DNR order use between 1999 and 2007 in the following categories: 1) NHs that remained consistent in the lowest third of DNR order use in 1999 and 2007; 2) NHs that went from lower to middle third, but did not change by more than 15%; 3) NHs that went from lower to medium third, but improved by 15% or greater; 4) NHs that remained in the middle at both the time periods but did not drop by more than 15%; 5) NHs that remained in the middle third, but improved by at least 15%; 6) NHs that dropped from high to middle with decreases of at least 15%; 7) NHs that dropped to middle third, but did not decrease by more than 15%; 8) NHs that went from lowest to highest third in 2007; and 9) NHs that remained persistently higher third in both the time periods. Fig. 3 presents the rate of terminal hospitalizations, which ranges from 21.1% for those NHs remaining in the lowest third of DNR orders, to 10.2% in those NHs that remained in the highest rate of DNR orders. The rate of terminal hospitalizations for the 46 NHs that went from lowest to highest third of DNR orders was 11.2%. NHs that started in the middle third of the rate of DNR orders and decreased the number of DNR orders by at least 15% had a slightly higher rate of terminal hospitalization than those NHs that did not decrease by 15% (16.5% vs. 15.2%, respectively).
Fig. 3.
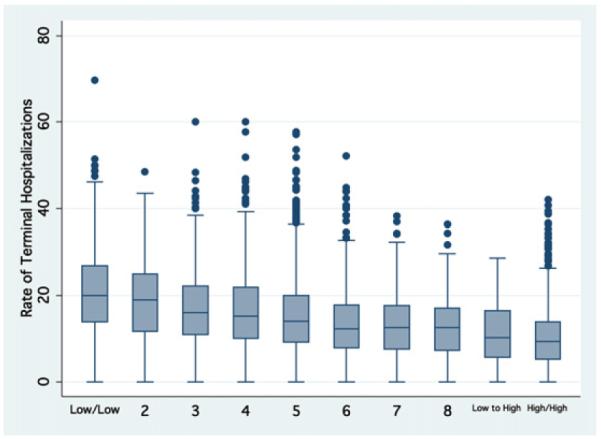
The association of facility rate of change in DNR orders with the rate of terminal hospitalizations. Figure examines the change in DNR orders between NHs in 1999 and 2007 based on the distribution of DNR and absolute change in DNR order with the rate of terminal hospitalizations in 2007. The rate of terminal hospitalizations ranged from 21.1% in NHs with the rate of DNR orders persistently in the lowest third to 10.2% in NHs persistently in the highest rate of DNR orders. The categories in figure from left to right are as follows: 1) NHs that remained consistent in the lowest third in 1999 and 2007; 2) NHs that went from lower to middle third, but did not change by 15%; 3) NH that went from lower to medium third, but improved by 15% or greater; 4) NH that remained in the middle at both the time periods but did not drop by 15%; 5) NH that remained in the middle third, but improved by 15%; 6) NH dropped from high to middle with a decrease by at least 15%; 7) NH dropped to middle third, but did not decrease by at least 15%; 8) NH that went from lowest to highest third in 2007; and 9) NHs remained persistently higher third in both the time periods.
To determine whether facility change in the ate of DNR orders was independently associated with the rate of terminal hospitalization, a fixed effect multivariate model that adjusted for changes in NH organizational characteristics, sociodemographic factors, and measures of disease severity was conducted with the NH as the unit of analysis. Table 2 presents the results of this analysis, revealing that for every 10% increase in the facility rate of DNR orders there was a 0.56% decrease in the rate of terminal hospitalizations. The addition of a nurse practitioner and/or physician extender was associated with a decrease in terminal hospitalizations. When an NH became a low resource facility secondary to becoming overly dependent on Medicaid payment, the result was a 0.70% increase in the rate of terminal hospitalizations.
Table 2.
Associations of Change in DNR Orders and Nursing Characteristics with Terminal Hospitalizations in the Last Week of Life Among NH Residents
| Change in Facility Rate or Characteristic | Coefficient | 95% Confidence Interval |
|---|---|---|
| Change in rate of DNR order per 10% | −0.56 | −0.50 to −0.61 |
| Hiring a nurse practitioner or physician assistant | −0.40 | −0.25 to −0.55 |
| Becoming an NH with disproportionate share of Medicaid patients | 0.70 | 0.41 to 1.0 |
*Results of multivariate fixed model that adjusted for changes in RN staffing, LPN staffing, nursing assistant staffing, the average case mix as measured by the RUGs, percentage of blacks, percentage of Hispanics, number of admissions, average age, average number of ADL deficiencies, percentage of person that are bedfast, and percentage of persons with advanced cognitive impairment.
Discussion
Terminal hospitalizations can be burden-some to dying patients and their families. Such hospitalizations may reflect inadequate advance care planning. In this study, we used NH prevalence of DNR orders as a marker for the facility’s culture of advance care planning. Multiple studies have found that the outcomes of resuscitation in the NH setting are poor, suggesting that resuscitation status should be assessed at the time of admission.2-5 We found that those NHs that increased their facility rate of DNR orders decreased their rate of terminal hospitalizations. These results support enhancing efforts to improve advance care planning in U.S. NHs.
Although there was an increase in the rate of DNR orders between 1990 and 1993 with the implementation of the PSDA,8 we observed just a slight increase in the rate of DNR orders from 1999 to 2007, the rate only increasing from 53.5% to 55.5%. The lack of significant change may reflect the shifting population of NHs. This is reflected in the rate of NH admissions increasing from 138.4 to 175.1 admissions. Indeed, even when restricting the change in DNR orders to persons with advanced cognitive impairment, there was only an increase of DNR orders of about 5% over the nine-year period. Despite the publication of several systematic reviews on the data regarding the effectiveness and morbidity associated with feeding tubes in persons with advanced dementia, the rate of orders to forgo feeding tubes only increased from 11.6% to 13.0%. These results suggest that there are important opportunities to improve advance care planning in U.S. NHs.
Almost 40% of NHs did change their practices in writing DNR orders, with a near equal amount increasing or decreasing their facility rate of DNR by 15%. As shown in Fig. 3, both the facility rate of DNR orders and the changing rate of DNR orders were associated with a change in the likelihood of terminal hospitalizations. It would be wrong to conclude that increasing rate of DNR orders directly causes a reduction in terminal hospitalizations. A DNR order does not provide information on a patient’s preference regarding terminal hospitalization. One should bear in mind while interpreting these results that we are using the facility rate of DNR orders as a measure of the NH culture of decision making. Those NHs that changed their culture of decision making, as measured by the use of DNR orders, reduced their rate of terminal hospitalizations. This association between increased facility rate of DNR orders and reduced terminal hospitalizations persisted even after adjusting for changes in NH organizational characteristics, NH resident sociodemographic characteristics, and aggregate disease severity of NH residents. Our findings are consistent with the results of randomized controlled trials to promote the use of written advance directives in the NH setting11 and efforts to promote the use of the Physician’s Orders for Life-Sustaining Treatment paradigm.12
The results indicate that NHs that have become low resource because of dependence on Medicaid payments (defined as 85% or more of reimbursements), rather than private pay or Medicare, have a higher facility rate of terminal hospitalizations. This study finds that facilities that become overly dependent on Medicaid have an increase in the rate of terminal hospitalizations by 0.7%. These findings are consistent with previous research reporting that such low resource NHs have poorer quality of care and higher likelihood of closure.13
Between 1999 and 2007, the use of nurse practitioners and physician assistants nearly doubled. Facilities that began to use nurse practitioners and/or physician assistants had a 0.4% decrease in the rate of terminal hospitalizations. Multiple studies have reported the association of an NH use of these health care providers with reduction in rates of hospitalizations.14-16
There are several limitations that need to be acknowledged in the interpretation of these findings. The MDS only collects data on the presence of order to forgo resuscitation and other forms of life-sustaining treatment. It should be noted that the MDS does not collect data on whether the process of DNR orders achieves the goals of shared decision making between the health care provider, the NH resident, if possible, and the family. However, our previous research suggests that facilities with higher rates of DNR orders had lower use of feeding tubes. It is possible that unmeasured factors resulted in a decrease in terminal hospitalizations. Our fixed effects model controls for persistent (time-invariant) unobserved NH factors influencing NH terminal hospitalizations and DNR order rates, but it cannot control for unobserved time-varying NH factors that we did not have measured. For the analysis that examined the association of facility changing rate of DNR order and terminal hospitalizations, only NH facilities with at least 25 Medicare deaths per year were included in the analysis. This resulted in the exclusion of smaller, rural NHs. Our results relied on data from 1999 to 2007. It is possible that there was a change that occurred after the end of our study period. Yet, this is the first national study to characterize the changing rate of DNR orders in a national sample of U.S. NHs for a nine-year period of time.
Conclusion
Hospitalizations in the last week of life ought to reflect a decision-making process in which the competent NH resident or their surrogate decision maker is informed of their prognosis, and the risks and benefits of treatments. Our results found that NHs that changed their end-of-life decision-making culture by increasing their facility rate of DNR orders also reduced their rates of terminal hospitalizations in the last week of life. Additionally, this study finds relatively unchanged use of DNR orders, DNH orders, and orders to forgo artificial hydration and nutrition over a nine-year period. Future interventions are needed to focus on improving the use of advance care planning in the NH setting.
Disclosures and Acknowledgments
This work was supported in part by National Institute on Aging grant P01AG027296.
References
- 1.Teno JM, Nelson HL, Lynn J. Advance care planning. Priorities for ethical and empirical research. Hastings Cent Rep. 1994;24:S32–S36. [PubMed] [Google Scholar]
- 2.Benkendorf R, Swor RA, Jackson R, Rivera-Rivera EJ, Demrick A. Outcomes of cardiac arrest in the nursing home: destiny or futility? Prehosp Emerg Care. 1997;1:68–72. doi: 10.1080/10903129708958790. [DOI] [PubMed] [Google Scholar]
- 3.Murphy DJ, Murray AM, Robinson BE, Campion EW. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Intern Med. 1989;111:199–205. doi: 10.7326/0003-4819-111-3-199. [DOI] [PubMed] [Google Scholar]
- 4.Gordon M, Cheung M. Poor outcome of on-site CPR in a multi-level geriatric facility: three and a half years experience at the Baycrest Centre for Geriatric Care. J Am Geriatr Soc. 1993;41:163–166. doi: 10.1111/j.1532-5415.1993.tb02052.x. [DOI] [PubMed] [Google Scholar]
- 5.Shah MN, Fairbanks RJ, Lerner EB. Cardiac arrests in skilled nursing facilities: continuing room for improvement? J Am Med Dir Assoc. 2007;8(3 Suppl 2):e27–e31. doi: 10.1016/j.jamda.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Teno JM, Mitchell SL, Gozalo PL, et al. Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA. 2010;303:544–550. doi: 10.1001/jama.2010.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell SL, Teno JM, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA. 2003;290:73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 8.Teno JM, Branco KJ, Mor V, et al. Changes in advance care planning in nursing homes before and after the patient Self-Determination Act: report of a 10-state survey. J Am Geriatr Soc. 1997;45:939–944. doi: 10.1111/j.1532-5415.1997.tb02963.x. [DOI] [PubMed] [Google Scholar]
- 9.Baker DW, Einstadter D, Husak S, Cebul RD. Changes in the use of do-not-resuscitate orders after implementation of the Patient Self-Determination Act. J Gen Intern Med. 2003;18:343–349. doi: 10.1046/j.1525-1497.2003.20522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wooldridge JM. Econometric analysis of cross section and panel data. MIT Press; Cambridge, MA: 2002. [Google Scholar]
- 11.Molloy DW, Russo R, Pedlar D, Bedard M. Implementation of advance directives among community-dwelling veterans. Gerontologist. 2000;40:213–217. doi: 10.1093/geront/40.2.213. [DOI] [PubMed] [Google Scholar]
- 12.Tolle SW, Tilden VP, Nelson CA, Dunn PM. A prospective study of the efficacy of the physician order form for life-sustaining treatment. J Am Geriatr Soc. 1998;46:1097–1102. doi: 10.1111/j.1532-5415.1998.tb06647.x. [DOI] [PubMed] [Google Scholar]
- 13.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 15.Kane RL, Keckhafer G, Flood S, Bershadsky B, Siadaty MS. The effect of Evercare on hospital use. J Am Geriatr Soc. 2003;51:1427–1434. doi: 10.1046/j.1532-5415.2003.51461.x. [DOI] [PubMed] [Google Scholar]
- 16.Buchanan JL, Murkofsky RL, O’Malley AJ, et al. Nursing home capabilities and decisions to hospitalize: a survey of medical directors and directors of nursing. J Am Geriatr Soc. 2006;54:458–465. doi: 10.1111/j.1532-5415.2005.00620.x. [DOI] [PubMed] [Google Scholar]


