Abstract
Purpose
The aim of this study was to review autopsies to determine the pattern of deaths in females at Wesley Guild Hospital, Ilesa, Nigeria.
Methods
A 9-year retrospective study was done of all autopsies done on females in the Department of Morbid Anatomy and Forensic Medicine, Obafemi Awolowo University Teaching Hospitals Complex, Wesley Guild Hospital, Ilesa, Nigeria, from January 2002 to December 2010. Records of all autopsies done on females during the period were reviewed.
Results
During the study period 215 cases of female death were autopsied. The age range was 0–75 years (mean = 32.9). Deaths due to trauma were most common (57.2%), followed by obstetric deaths (15.8%). Deaths due to infections and cardiovascular diseases accounted for 13% and 5.6%, respectively. Injuries sustained from automobile accidents were responsible for 88.6% of all trauma deaths. Gunshot injuries accounted was 4.9% of these trauma deaths. The causes of death from automobile accidents included multiple injuries (49.5%), head injury (38.5%), and hypovolemia (8.3%). Obstetric deaths were predominantly due to uterine sepsis (51.5%) and hemorrhagic shock (39.4%). About 39% of deaths from infection were due to septicemia. Acute bacterial meningitis, acute lobar pneumonia, and malaria caused 23.1%, 15.4%, and 7.7% of deaths from infections, respectively. Four cases of sudden unnatural deaths (other than trauma) were recorded.
Conclusion
Trauma was the most common cause of death in women autopsied in our hospital, and automobile injuries were the most common causes of these trauma deaths. Obstetric deaths ranked second. Sepsis and hemorrhage were the most common causes of these obstetric deaths. Deaths from eclampsia were low. Requests for autopsies on women who died from cancer were few. There is a need for clinicians to ascertain the actual cause of death in women who die from cancer.
Keywords: females, mortality, autopsy
Introduction
Mortality in women has long been a source of concern to health policy makers and health organizations. Greater emphasis is generally on maternal mortality which has been linked to development indices and can be used to assess the level of development of countries. Although the rates of death in many age groups are not clearly known because of unavailability of data, the rate of maternal mortality has been well studied. The maternal mortality ratio in Nigeria is known to have been persistently greater than 1000 per 100,000 live births in the past decade. Various efforts have been made to improve the status of women and to reduce their mortality. These include education, empowerment, and health programs. One of the most-emphasized health programs is reduction in maternal mortality.1 Maternal mortality is mainly due to malaria in pregnancy, prolonged obstructed labor, obstetric hemorrhage, and sepsis.2–7
Deaths from trauma are also important in females. Road traffic accidents have been recognized as a major cause of death in developing countries. The leading causes of death in surgical wards at a teaching hospital in South-Eastern Nigeria were acute abdomen (22.2%), road traffic accident (18.14%), and malignancies (14.56%).8 Although death from road accidents is more common in men, women are significantly involved. Other trauma deaths that involve women include domestic violence, homicide, suicide, and fall from height.9
It is a known fact that death from infections is more common in developing than developed countries. Sani et al found infections to be the most common cause of death in the medical wards of a teaching hospital in Northern Nigeria.10 This can be due to malaria, human immunodeficiency virus, and bacterial infections. Other infections also cause death in varying proportions.
Death from cancer is also a major problem. Breast cancers, cancers of the cervix, and ovarian cancers are three of the most common cancers that particularly involve women. 11 Among 94 women who died in the gynecology ward of Lagos University Teaching Hospital from 2002 to 2007, 44.7% died from cervical cancer and 29.8% died from ovarian cancer.12 Breast cancer screening through mammography and fine needle aspiration cytology is being used for early detection. Cervical smear is also used for early detection of premalignant cervical lesions. Ovarian cancer is more difficult to detect because of its generally occult nature and poor accessibility of the ovaries for ease of screening.
Apart from the above-mentioned diseases, numerous conditions that affect men also affect women.13 Women die from conditions like diabetes mellitus, renal diseases, hypertension,14 and respiratory diseases. Mortality is sometimes higher in women. Desalu et al showed mortality to be higher in women than men with respiratory diseases.15
Deaths in females in some age groups do not significantly differ from those of males. For instance, in the pediatric age group both males and females die from childhood diseases. These diseases include measles, protein energy malnutrition, and respiratory tract infections.16 Congenital malformation also contributes significantly to perinatal deaths.17
The aim of this study was to review autopsies to determine the pattern of deaths in females at Wesley Guild Hospital, Ilesa, Nigeria.
Materials and methods
A 9-year retrospective study was undertaken of all autopsies done on females in the Department of Morbid Anatomy and Forensic Medicine, Obafemi Awolowo University Teaching Hospitals Complex, Wesley Guild Hospital, Ilesa, Nigeria, from January 2002 to December 2010. This hospital serves Ilesa and its surrounding communities in Osun State of South-Western Nigeria. Records of all autopsies done on females during the period were retrieved from the autopsy register of the department. For all cases, data on age and cause of death were extracted.
The causes of death were classified into trauma, obstetrics/gynecology, infection, cardiovascular, neonatal, sudden unexpected death (other than trauma), and cancer, gastrointestinal, renal, and unknown causes.
The data obtained were analyzed using Statistical Packaging for Social Sciences (SPSS Inc, Chicago, IL) version 15.0. Simple descriptive statistics were used.
Results
In total, 215 cases of female deaths were autopsied during the study period, accounting for 30.6% of all autopsies done during the study period. The mean age of all cases was 32.9 years (range 0–75 [Table 1]).
Table 1.
Background characteristics of the patients
| Autopsies (n) | 703 |
| Females (n) | 215 (30.6%) |
| Males (n) | 488 (69.4%) |
| Mean age of females (years) | 32.9 ± 17.9 |
| Age range (years) | 0–75 |
Deaths due to trauma were most common and accounted for 123 (57.2%) of all cases, followed by obstetric deaths, which accounted for 34 (15.8%) of all cases. Deaths due to infections and cardiovascular diseases accounted for 13% (28) and 5.6% (12), respectively. Other causes of death and their respective frequencies and percentages are shown in Table 2.
Table 2.
Causes of death and patient age groups
| 0–9 years | 10–19 years | 20–29 years | 30–39 years | 40–49 years | 50–59 years | 60–69 years | 70–79 years | Unknown years | Total years | |
|---|---|---|---|---|---|---|---|---|---|---|
| Trauma Frequency (% of trauma) | 12 (9.8%) | 6 (4.9%) | 27 (22.0%) | 18 (14.6%) | 26 (21.1%) | 18 (14.6%) | 9 (7.3%) | 6 (4.9%) | 1 (0.8%) | 123 (100.0%) |
| Cancer Frequency (% of cancer) | 0 (0.0%) | 0 (0.0%) | 1 (250.0%) | 1 (25.0%) | 0 (0.0%) | 1 (25.0%) | 1 (25.0%) | 0 (0.0%) | 0 (0.0%) | 4 (100.0%) |
| SUD Frequency (% of SUD) | 1 (25.0%) | 0 (0.0%) | 1 (25.0%) | 0 (0.0%) | 1 (25.0%) | 1 (25.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (100.0%) |
| GIT Frequency (% of GIT) | 0 (0%) | 1 (50.0%) | 1 (50.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100.0%) |
| Obstetric Frequency (% of obstetric) | 0 (0%) | 9 (26.5%) | 12 (35.3%) | 11 (32.4%) | 2 (5.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 34 (100.0%) |
| Infection Frequency (% of infection) | 6 (21.4%) | 4 (14.3%) | 11 (39.3%) | 2 (7.1%) | 3 (10.7%) | 0 (0%) | 2 (7.1%) | 0 (0%) | 0 (0%) | 28 (100.0%) |
| CVS Frequency (% of CVS) | 0 (0%) | 1 (8.3%) | 1 (8.3%) | 3 (25.0%) | 0 (0%) | 5 (41.7%) | 1 (8.3%) | 0 (0%) | 1 (8.3%) | 12 (100.0%) |
| Renal Frequency (% of renal) | 1 (100.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100.0%) |
| Neonatal Frequency (% of neonatal) | 5 (100.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 5 (100.0%) |
| Unknown Frequency (% of unknown) | 0 (0%) | 1 (50.0%) | 0 (0%) | 1 (50.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100.0%) |
| Total Frequency (% of total) | 25 (11.6%) | 22 (10.2%) | 54 (25.1%) | 36 (16.7%) | 32 (14.9%) | 25 (11.6%) | 13 (6.0%) | 6 (2.8%) | 2 (0.9%) | 215 (100.0%) |
Abbreviations: SUD, sudden unexpected death; GIT, gastrointestinal tract; CVS, cardiovascular system.
Trauma was the most common cause of death for all age groups except age 10–19 years where obstetric causes accounted for 40.6% and trauma 27.3%. Most of these obstetric/gynecological deaths were due to uterine sepsis secondary to criminally induced abortion.
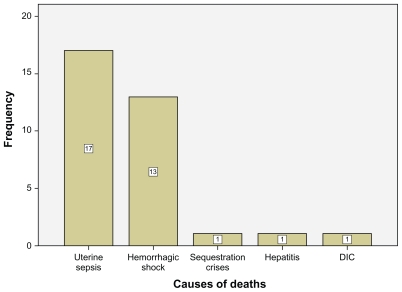
Injuries sustained from automobile accidents were responsible for 88.6% of all trauma deaths (Figure 1). Gunshot injuries accounted for 4.9% of these trauma deaths. Cases of assault (other than gunshot) and falls accounted for 5.7% and 0.8%, respectively. Most of the deaths from automobile accidents were as a result of multiple injuries sustained (49.5%). Head injury was the second most common cause of death following automobile accident and accounted for 38.5% of deaths. Other causes of death were hypovolemia, chest injuries, and severe burns, accounting for 8.3%, 2.8%, and 0.9%, respectively.
Figure 1.
Causes of trauma deaths in women.
Abbreviation: DIC, disseminated intravascular coagulopathy.
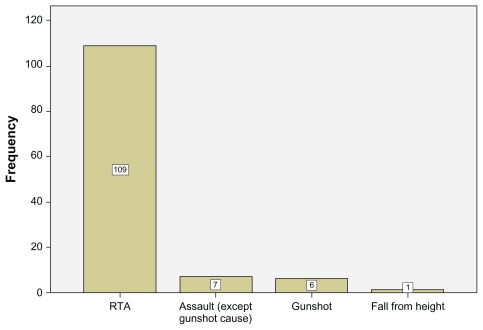
Uterine sepsis and hemorrhagic shock were the most common causes of obstetric deaths and accounted for 51.5% and 39.4% of all obstetric deaths, respectively (Figure 2). Analysis of the cases of uterine sepsis showed that 66.7% were due to induced abortion, 13.3% to intrauterine fetal death, 13.3% to puerperal sepsis, and 6.7% to chorioamnionitis. Fifty percent of deaths from obstetric hemorrhage were due to complications of induced abortion. Uterine rupture, abruptio placentae, and disseminated intravascular coagulopathy accounted for 35.7%, 7.1%, and 7.1%, respectively.
Figure 2.
Frequency and causes of obstetric deaths.
Indirect obstetric causes of death included viral hepatitis (3%) and sequestration crises (3%) due to sickle cell disease. All the cases of induced abortion were unbooked cases referred from private health facilities. All obstetric and gynecological deaths occurred between the ages 15 and 45 years. This age group accounted for 61.4% of all deaths. Table 3 shows causes of death in this age group. As shown in the table, trauma still remains the most common cause of death in this reproductive age group.
Table 3.
Causes of death in age group 15–45 years
| Causes of death | Frequency | % |
|---|---|---|
| Trauma | 70 | 53.1 |
| Obstetric | 34 | 25.8 |
| Infection | 18 | 13.6 |
| CVS | 5 | 3.8 |
| Cancer | 2 | 1.5 |
| SUD | 2 | 1.5 |
| GIT | 1 | 0.8 |
| Total | 132 | 100.0 |
Abbreviations: SUD, sudden unexpected death; GIT, gastrointestinal tract; CVS, cardiovascular system.
About 39% of deaths from infection were due to septicemia. Acute pyogenic meningitis, lobar pneumonia, and malaria caused 23.1%, 15.4%, and 7.7% of infective deaths, respectively. Infective gastroenteritis, tuberculosis, and typhoid fever caused 3.8% each.
Four cases of sudden unnatural deaths (other than trauma) were recorded. Electrocution caused 2 of these deaths while drug poisoning and drowning caused 1 death each.
Five neonatal deaths were autopsied during the period of study, 4 deaths from malignant tumors and 2 from gastrointestinal diseases (excluding infections). Of the 5 neonatal deaths, 2 were due to congenital malformations. The 2 cases of deaths from gastrointestinal diseases were due to perforated duodenal ulcer and intussusception.
Binary logistic regression analysis shows that the age groups 10–19 and 40–49 years have, respectively, positive and negative predictive values for trauma death (odds ratio [OR] 0.244, P = 0.003 and OR 3.842, P = 0.001, respectively). The only significant predictor for cardiovascular deaths was age group 40–49 years (OR 6.536, P < 0.003).
Obstetric deaths were significant in age groups 10–19 and 30–39 years (OR 4.652, P < 0.001, and OR 2.984, P < 0.01, respectively). None of the age groups had a significant association with other causes of death.
Discussion
The Wesley Guild Hospital Ilesa, Obafemi Awolowo University Teaching Hospital Complex is a tertiary health center that caters for the health needs of the people of Ijesha and its environs. The Ijesha zone of the Ife-Ijesa senatorial district of Osun State Nigeria has a population of 620,000 people (2006 Nigeria population census), 50% of the population being females. The hospital is located in the South-Western part of Nigeria and deaths that are certified or that occur in this hospital are routinely autopsied if they fall into certain categories, which include all maternal mortalities, automobile accident fatalities, deaths within 24 hours of admission, clinician requests, and other coroner cases.
The autopsy rate of approximately 100 per year is quite low, though more deaths would have occurred during the period. The acceptance of autopsy by the populace is not too encouraging.18,19
Deaths from trauma were overwhelmingly the most common (Table 1). Trauma deaths were more common than the obstetric deaths. Most of these trauma deaths were due to automobile accidents. Although these may not be the exact situation in the population, many hospital-based data may be reflective of the statistics in the population.13 This result shows that preventive efforts geared towards reduction of deaths in women should include reduction of trauma as well as obstetric deaths. Much emphasis had been placed on reduction of maternal mortality; policy makers should now consider how to further reduce automobile fatalities among women and also the general populace. Thirteen women were found to have died as a result of assault, 6 of which were gunshot injuries sustained during communal clashes.
The second most common cause of deaths in females is obstetric death. Many studies have shown the relatively high maternal mortality rate in Nigeria.2–7 Maternal deaths have remained high despite many efforts in reducing it.5 A more concerted effort is needed in the implementation of already existing policies on reduction of maternal mortality.
This study has also shown that uterine sepsis was the most common cause of maternal death. This is similar to the report by Nwagha et al,5 but slightly differs from reports by Mairiga et al4 and Agan et al7 who found sepsis to be less prominent. Many of the cases handled by the obstetricians at the study center are cases referred from private hospitals. Some of these cases may have been mismanaged before being referred to the hospital, which may be partly responsible for the many deaths from infections. It is very important for the attending physician and health personnel to maintain strict asepsis in all procedures, including during labor and delivery. Rational and prompt use of potent antibiotics in suspected cases of sepsis is advocated.
Worthy of note is the predominance of obstetric death in the age group 10–19 years. Most of these cases were due to criminally induced abortion. Associated complications include sepsis, uterine perforation with gut evisceration, and shock. There is a need for increased education on adolescent sexuality and prevention of unwanted pregnancies.
Hemorrhagic shock is the second most common cause of maternal death and this corroborates many reports of it being a major problem.2–7 There is a need for more prompt identification of imminent shock and management of shock by the health care givers. Many of the cases were referrals from private facilities. Death from hemorrhagic shock is preventable. With adequate prevention and management, this cause of death in women can almost be completely eliminated. Eclampsia seems to be a relatively rare cause of death in this hospital and may be due to adequate management by the attending obstetricians.
Deaths of women from malignant tumors are known to be a problem worldwide.11 The fact that only 4 cases, representing 0.9% of all cases, were recorded in this study is most likely not representative of the proportion of cancer deaths. It probably signifies the very low number of requests for autopsy in deaths from cancer. It is necessary to educate clinicians on the need to know the actual cause of death in individuals with cancer. Some deaths could have been due to oncotherapy, effects of the tumor, or failure to provide adequate supportive and resuscitative management. The definite cause of death can best be known after an autopsy.
The neonatal mortality rate in developing countries, including Nigeria, is quite high.20 The rate of autopsy for neonatal deaths in our environment is very low. This is well demonstrated in this study in which only 2.3% of the autopsies were neonatal deaths. The time of grief around this period makes obtaining consent from the bereaved parents very difficult. This may have accounted for the dismally low rate of autopsy for this group of patients.
Conclusion
In conclusion, trauma was the most common cause of death in women autopsied in our hospital, and automobile accident was the most common cause of trauma death. Obstetric death was the second most common cause of mortality in women. Sepsis and hemorrhage, which are preventable, are still the most common causes of obstetric death in our hospital. Requests for autopsies on women who died from cancer were few. There is a need for clinicians to ascertain the actual cause of death in women who die from cancers.
Footnotes
Disclosure
The authors declare no conflicts of interest in relation to this paper.
References
- 1.Okaro JM, Iyoke CA. The Society of Gynecology and Obstetrics of Nigeria (SOGON) plan for sustainable reduction in maternal mortality: a review. Afr J Reprod Health. 2010;14(2):139–147. [PubMed] [Google Scholar]
- 2.Kullima AA, Kawuwa MB, Audu BM, Geidam AD, Mairiga AG. Trends in maternal mortality in a tertiary institution in Northern Nigeria. Ann Afr Med. 2009;8(4):221–224. doi: 10.4103/1596-3519.59575. [DOI] [PubMed] [Google Scholar]
- 3.Ikpeze OC. Pattern of morbidity and mortality following illegal termination of pregnancy at Nnewi, Nigeria. J Obstet Gynecol. 2000;20(1):55–57. doi: 10.1080/01443610063471. [DOI] [PubMed] [Google Scholar]
- 4.Mairiga AG, Saleh W. Maternal mortality at the State Specialist Hospital Bauchi, Northern Nigeria. East Afr Med J. 2009;86(1):25–30. doi: 10.4314/eamj.v86i1.46924. [DOI] [PubMed] [Google Scholar]
- 5.Nwagha UI, Nwachukwu D, Dim C, Ibekwe PC, Onyebuchi A. Maternal mortality trend in South East Nigeria: less than a decade to the millennium developmental goals. J Womens Health (Larchmt) 2010;19(2):323–327. doi: 10.1089/jwh.2008.1028. [DOI] [PubMed] [Google Scholar]
- 6.Onah HE, Okaro JM, Umeh U, Chigbu CO. Maternal mortality in health institutions with emergency obstetric care facilities in Enugu State, Nigeria. J Obstet Gynecol. 2005;25(6):569–574. doi: 10.1080/01443610500231484. [DOI] [PubMed] [Google Scholar]
- 7.Agan TU, Archibong EI, Ekabua JE, et al. Trends in maternal mortality at the University of Calabar Teaching Hospital, Nigeria, 1999–2009. Int J Womens Health. 2010;2:249–254. doi: 10.2147/ijwh.s11971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chukuezi AB, Nwosu JN. Mortality pattern in the surgical wards: a five year review at Federal Medical Centre, Owerri, Nigeria. Int J Surg. 2010;8(5):381–383. doi: 10.1016/j.ijsu.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Ekere AU, Yellowe BE, Umune S. Mortality patterns in the accident and emergency department of an urban hospital in Nigeria. Niger J Clin Pract. 2005;8(1):14–18. [PubMed] [Google Scholar]
- 10.Sani MU, Mohammed AZ, Bapp A, Borodo MM. A three-year review of mortality patterns in the medical wards of Aminu Kano Teaching Hospital, Kano, Nigeria. Niger Postgrad Med J. 2007;14(4):347–351. [PubMed] [Google Scholar]
- 11.Tavassoli FA, Devilee P, editors. World Health Organization Classification of Tumours Pathology and Genetics of Tumours of the Breast and Female Genital Organs. Lyon, France: IARC Press; 2003. [Google Scholar]
- 12.Anorlu RI, Obodo K, Makwe CC. Cancer mortality among patients admitted to gynecological wards at Lagos University Teaching Hospital, Nigeria. Int J Gynecol Obstet. 2010;110(3):268–269. doi: 10.1016/j.ijgo.2010.03.038. [DOI] [PubMed] [Google Scholar]
- 13.Adeolu AA, Arowolo OA, Alatise OI, et al. Pattern of death in a Nigerian teaching hospital; 3-decade analysis. Afr Health Sci. 2010;10(3):266–272. [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman JS, Rotimi CN, Brieger WR, et al. The mortality risk associated with hypertension: preliminary results of a prospective study in rural Nigeria. J Hum Hypertens. 1996;10(7):461–464. [PubMed] [Google Scholar]
- 15.Desalu OO, Oluwafemi JA, Ojo O. Respiratory diseases morbidity and mortality among adults attending a tertiary hospital in Nigeria. J Bras Pneumol. 2009;35(8):745–752. doi: 10.1590/s1806-37132009000800005. [DOI] [PubMed] [Google Scholar]
- 16.Aikhionbare HA, Yakubu AM, Naida AM. Mortality pattern in the Emergency Pediatric Unit of Ahmadu Bello University Teaching Hospital, Zaria, Nigeria. Cent Afr J Med. 1989;35(5):393–396. [PubMed] [Google Scholar]
- 17.Abudu OO, Uguru V, Olude O. Contribution of congenital malformation to perinatal mortality in Lagos, Nigeria. Int J Gynecol Obstet. 1988;27(1):63–67. doi: 10.1016/0020-7292(88)90089-6. [DOI] [PubMed] [Google Scholar]
- 18.Olasode BJ, Odesanmi W. The hospital autopsy – halting the decline. Niger Postgrad Med J. 1998;5(1):37–39. [Google Scholar]
- 19.Oluwasola AO, Fawole OI, Otegbayo JA, et al. Trends in clinical autopsy rate in a Nigerian tertiary hospital. Afr J Med Sci. 2007;36(3):267–272. [PubMed] [Google Scholar]
- 20.Omoigberale AI, Sadoh WE, Nwaneri DU. A 4 year review of neonatal outcome at the University of Benin Teaching Hospital, Benin City. Niger J Clin Pract. 2010;13(3):321–325. [PubMed] [Google Scholar]