Abstract
Background
Previous research reported that childhood adversity predicts juvenile- but not adult-onset depression, but studies confounded potentially genuine differences in adversity with differences in the recency with which adversity was experienced. This paper took into account the recency of risk when testing for differences among child-, adolescent-, and young-adult-onset depressions.
Methods
Up to nine waves of data were used per subject from two cohorts of the Great Smoky Mountains Study (N = 1,004), covering children in the community ages 9–16, 19, and 21 years. Youth and one of their parents were interviewed using the Child and Adolescent Psychiatric Assessment between ages 9–16; these same youth were interviewed using the Young Adult Psychiatric Assessment at ages 19 and 21. The most common psychosocial risk factors for depression were assessed: poverty, life events, parental psychopathology, maltreatment, and family dysfunction.
Results
Consistent with previous research, most childhood psychosocial risk factors were more strongly associated with child-onset than with adolescent-/adult-onset depression. When potentially genuine risk differences among the depression-onset groups were disentangled from differences due to the recency of risk, child- and young adult-onset depression were no longer different from one another. Adolescent-onset depression was associated with few psychosocial risk factors.
Conclusions
There were no differences in putative risk factors between child- and young adult-onset depression when the recency of risk was taken into account. Adolescent-onset depression was associated with few psychosocial risk factors. It is possible that some adolescent-onset depression cases differ in terms of risk from child- and young adult-onset depression.
Do child-, adolescent-, and adult-onset depression have the same risk correlates and precursors (Kaufman et al., 2001)? The answer to this question is unclear. Neurobiological and treatment research has found that usually two, but not all three, of these depression onset-groups share common correlates (Kaufman et al., 2001), suggesting a complex picture of both shared and non-shared pathways to the onset of depression at different points in development. If developmental subtypes of depression differed in terms of risk, examining them separately for purposes of biosocial research, prevention, and intervention would be important, as has been shown by research on developmental subtypes of antisocial behaviors (for a review, see Moffitt et al., 2006).
Psychosocial Risk for Child-, Adolescent-, and Young Adult-Onset Depression
Juvenile-onset depression is associated with a range of early psychosocial risk factors, including childhood poverty (Gilman et al., 2003), life events (Jaffee et al., 2002), parental psychopathology (Jaffee et al., 2002), maltreatment (Hill et al., 2004, Jaffee et al., 2002) and family dysfunction (Hill et al., 2004). Indeed youth with early-onset depression appear to be characterized by pervasive dysfunction throughout life (Jaffee et al., 2002, Hill et al., 2004, see also Christie et al., 1988, Giaconia et al., 1994, Kasch and Klein, 1996, Kovacs, 1984, Rao et al., 1995, Weissman et al., 1999). In contrast, the childhood psychosocial risk factor profile for adult-onset depression has appeared to be “similar to that of the never-depressed” (Jaffee et al., 2002, p. 215, Hill et al., 2004). These findings have been interpreted as indicating that child- and adult-onset depressions are likely to be etiologically distinct.
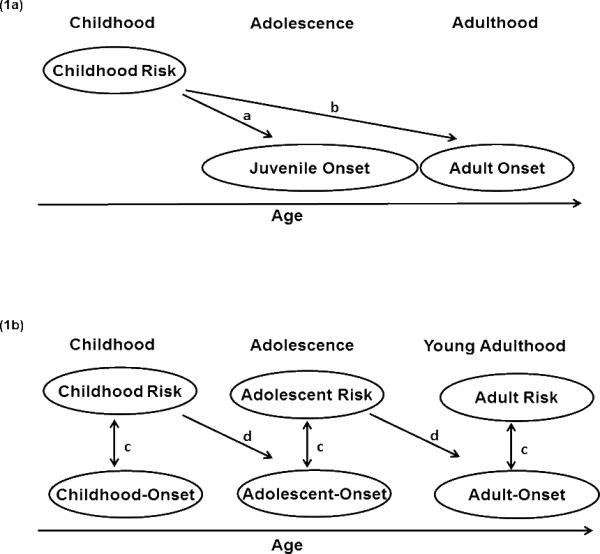
However, such a conclusion is premature because such apparent differences in risk might merely reflect differences in how recently risk factors were experienced. Risk factors in the key studies were typically assessed in childhood, but the depressogenic effects of adversities are strongest during the period immediately following their occurrence (e.g., Brown and Harris, 1978; Kessler et al., 1997), so perhaps we should not be surprised that childhood risk factors exerted most of their effects in childhood. Figure 1a illustrates that potentially genuine differences in risk were confounded with differences in the recency of risk occurrence, because the time elapsed between childhood risk and juvenile-onset depression (path “a”) was much less than the time elapsed between childhood risk and adult-onset depression (path “b”).
Figure 1.
Timing of risk in relation to depression onset. Figure 1a shows the design of previous studies, with childhood risk predicting juvenile- and adult-onset depressions. Figure 1b shows the design of the present study, with concurrent and antecedent risk predicting child-, adolescent-, and young adult-onset depressions.
We propose to test a “recency hypothesis” which posits that the lack of strong associations between childhood adversity and adult-onset depression occurs not because child- and adult-onset depressions genuinely differ in terms of risk, but because at every age the depressogenic effects of adversities are mostly time-limited. For example, family dysfunction might have depressogenic effects for a number of months or years, but not longer. Thus, if measured in childhood, it would be linked with child-, and perhaps with adolescent-onset depression (Hill et al., 2004), but not with young adult-onset depression. If measured in adolescence or young adulthood, family dysfunction would, however, be linked with adolescent- and perhaps with young adult-onset depression.
Studies have used cut-offs ranging from 14 to 20 years of age to distinguish between juvenile- and adult-onset depression (e.g., Jaffee et al., 2002, Hill et al., 2004, Gilman et al., 2003). Yet, the major increase in the prevalence of depression in females occurs around age 13 in Western populations (e.g., Angold et al., 2002), and research increasingly suggests that adolescent-onset depressions may constitute their own category (e.g., Copeland et al., 2009; Kaufman et al., 2001). Thus, placing adolescent-onset depressions with either the child- or with the adult-onset depressions could mask adversity-onset links.
The present study attempts to eliminate the confound between the recency and risk differences hypotheses by measuring the same psychosocial risk factors occurring concurrently with and antecedently to child-, adolescent-, and young adult-onset depressions (see Figure 1b). According to the recency hypothesis, the odds ratios for paths “c” should be similar in size to one another, as should the odds ratios for paths “d”. According to the risk differences hypothesis, odds ratios for paths “c” should differ in size from one another, as should the odds ratios for paths “d”.
METHODS
Sample and Procedures
The Great Smoky Mountains Study (GSMS) is a longitudinal study of the development of psychiatric disorders in youth (Costello et al., 1996, Costello et al., 2003). The accelerated cohort (Schaie, 1965), two-phase sampling design and measures are described in detail elsewhere (Costello et al., 1996). Briefly, a representative sample of 9-, 11-, and 13-year-olds in western North Carolina was selected using a household equal probability design. In the screening phase the primary caregiver completed a questionnaire containing items regarding behavioral disorders from the Child Behavior Checklist (Achenbach and Edelbrock, 1983). The interview phase included all children scoring above a pre-defined cut-off on this screen (designed to identify the most pathological 25% of the population), along with a 10% random sample of the remainder. All age-eligible American Indian children from the area were also recruited. Data were collected on one cohort at ages 9 and 10, two cohorts at ages 11, 12, and 13, and all three cohorts at ages 14, 15, 16, 19, and 21. Of the 1777 children recruited, 1420 agreed to participate (80%). Across waves, an average of 82% of possible interviews was completed (75% to 94%). The present study focuses on the two youngest GSMS cohorts (first assessed at ages 9 and 11, respectively; N = 1004), because childhood assessments were available for these two cohorts. Each subject was interviewed up to nine times. Before each interview began, parent and child signed informed consent/assent forms approved by the Institutional Review Boards of Duke University Medical Center and the Eastern Band of Cherokee Indians.
Measures
Psychiatric disorders were assessed using 1) the Child and Adolescent Psychiatric Assessment (CAPA, Angold and Costello, 2000, Angold and Costello, 1995) until age 16, and 2) the upward extension of the CAPA, the Young Adult Psychiatric Assessment (YAPA) at ages 19 and 21 (Angold et al., 1999). To minimize recall bias, the timeframe for determining the presence of most psychiatric symptoms is the 3 months immediately preceding the interview. Scoring programs for the CAPA and YAPA, written in SAS (SAS Institute, 2004), combined information about the date of onset, duration, and intensity of each symptom to create diagnoses according to the DSM-IV. A symptom was counted as present if reported by either parent or child until age 16 or by the young adult at ages 19+. The two-week test-retest reliability of CAPA diagnoses for 10 to 18 year-olds is comparable to that of other structured diagnostic interviews (Ks for individual disorders range from .56 to 1.0; Angold and Costello, 1995). Consistent with relevant previous research, we used age to distinguish among the depression onset groups (Hill et al., 2004; Jaffe et al., 2002). Using pubertal status to define these groups resulted in only minor changes. Child-onset depression was defined as first reported diagnosis between ages 9 to <13, adolescent-onset as first reported diagnosis between the ages of 13 to 16, and young adult-onset as first reported diagnosis at ages 19 or 21. We included major depression, dysthymia and depression NOS in our depression category. Table 1 describes the depression onset groups in terms of sex and specific depression diagnoses. Several subjects had multiple diagnoses of depression within one developmental period (e.g., depression NOS in one childhood year, and major depression in another childhood year).
Table 1.
Characteristics of the depression onset groups. The percentages for males and females refer to weighted percentages within the respective depression (or never-depressed) groups.
| Child-Onset First diagnosed at 9 to <13 | Adolescent-Onset First diagnosed at 13–16 | Adult-Onset First diagnosed at 19 or 21 | Never-Depressed | |
|---|---|---|---|---|
| Total N(%) | 46 (2.5) | 55 (5.6) | 44 (3.6) | 860 (88.3) |
| Males | 27 (58.8) | 24 (35.1) | 20 (40.6) | 497 (52.8) |
| Females | 19 (41.2) | 31 (64.9) | 24 (59.4) | 363 (47.2) |
| Odds Ratio M/F | 1.35 (0.53–3.47) | 0.49 (0.19–1.24) | 0.63 (0.22–1.80) | 1.55 (0.85–2.85) |
| Depressive Disorders | ||||
| Minor Depression | 42(2.3) | 50(5.5) | 34(2.5) | |
| Dysthymia | 4(0.2) | 15(1.6) | 17(1.7) | |
| Major Depression | 9(0.4) | 18(2.0) | 16(1.3) |
Other disorders were also assessed in the CAPA/YAPA. The unweighted Ns and weighted prevalence were 204 (11.6%) for childhood behavioral disorders, 99 (6.4%) for childhood anxiety disorders, 203 (18.8%) for adolescent behavioral disorders (including substance disorders), 48 (4.3%) for adolescent anxiety disorders, and 211 (27.7%) for young adult antisocial personality disorder and substance disorders, and 65 (9.3%) for young adult anxiety disorders.
Psychosocial risk factors were also collected in the CAPA and YAPA unless otherwise specified. Here, we included putative psychosocial risk domains that have been commonly identified for depression across development: poverty, stressful life events, parental psychopathology, maltreatment, and family dysfunction (Birmaher et al., 1996, Cicchetti and Toth, 1998, Goodyer, 2001, Harrington et al., 2006, Zalsman et al., 2006). Individual risk factors (e.g., low income, material hardship, and low education in the domain of poverty) were coded as 1 (present) if reported by either parent or child (CAPA), and as 0 when not present. During the adult assessments with the YAPA, the subject was the sole reporter of all risk factors. With the exception of lifetime parental psychopathology, all risk factors were assessed at the time of the interview (e.g., poverty) or over the preceding 3 months (e.g., life events), and were aggregated across childhood (i.e., any observation from ages 9 to <13), adolescence (i.e., any observation from ages 13 to 16), and young adulthood (e.g., any observation at ages 19 and 21). For example, if the subject had experienced material hardship at any assessment between the ages of 9 to <13, s/he received a 1 on the childhood version of material hardship. Because the timeframe for assessing depression was also the 3 months immediately preceding the interview, temporal overlap between childhood putative risk factors and depression onset in the same developmental period was possible (e.g., childhood risk and child-onset depression). Indeed, associations between risks and depression onset within the same developmental period can only establish putative risk factor status (Kraemer et al., 2001). To increase the parsimony of our analyses and our power to detect differences between the depression-onset groups, we created a sum score for each risk domain.
The poverty scale ranged from 0–3, summing low income, material hardship, and low education. Low income was coded when the household income was below the federal poverty level. Material hardship was coded when the family (CAPA) or the subject (YAPA) were unable to meet basic needs, having no health insurance, financial problems, residential instability, or no insurance for mental health or substance abuse care. Low education was coded when the subject's parents (CAPA) or the subject (YAPA) did not graduate from high school.
The loss and violence events scale ranged from 0–2, summing the occurrence of loss and violence events. Loss events included parental divorce/separation; death of a loved one, sibling, or peer; romantic breakup; breakup with or loss of best friend; pregnancy loss; and job loss (YAPA only). Violence events included death of a loved one by violence, war, terrorism, witness to a violent life event, and cause of death or severe harm. Details of the construction and psychometric testing of the Life Events section of the CAPA are contained elsewhere (Costello et al., 1998).
Lifetime parental psychopathology ranged from 0–3 and summed whether biological parents had ever sought or received treatment for mental health or drug problems, and whether the parent had been arrested and/or prosecuted for a crime since parent's age 18. (Arrests for DUI and/or drug related charges were not coded here). This risk factor was only assessed using a lifetime timeframe.
Maltreatment ranged from 0–2 and summed sexual abuse/violence (including rape) and physical abuse/captivity. In the YAPA, spousal abuse was included in the physical abuse variable. Finally, family dysfunction ranged from 0–3, and included parent-child conflict, interparental conflict, scapegoating (CAPA only), and subject's marital conflict (YAPA only). Parent-child conflict was coded when children scored in the top 25% of parent-child conflict within a given wave. Interparental conflict was coded when the relationship between parents was characterized by high conflict, poor communication, and/or violence. Scapegoating (parental differential treatment) was coded when children were regarded/treated more negatively by a parent compared to other children in the family. Subject's marital conflict was coded when subjects reported having conflict with a spouse.
Some individual risk factors were assessed in the CAPA, but not in the YAPA, because they were no longer relevant in young adulthood. For example, scapegoating (i.e., parental differential treatment of children in the home) was no longer coded in the young adult assessments, because many subjects no longer resided with parents and siblings. Other risk factors were only age-appropriate for young adults, including subject's job loss, and marital violence and conflict. Table 2 describes the depression onset groups in terms of (putative) risk factors. When identical risk domain scores across developmental periods were created or risk domain scores were standardized within developmental period, our overall findings did not change systematically.
Table 2.
Weighted means (standard deviations) of child, adolescent, and young adult risk factors by depression onset group.
| Psychosocial Risk Factors | Possible Range | Overall Mean N = 1004 | Child-Onset N = 46 | Adol.-Onset N = 55 | Adult-Onset N = 44 | Never-Depressed N = 859 |
|---|---|---|---|---|---|---|
| CHILDHOOD RISK | ||||||
| Poverty | 0–3 | 1.00(1.00) | 1.72(0.63) | 1.43(1.10) | 1.51(1.00) | 0.93(0.98) |
| Loss and Violence Events | 0–2 | 0.32(0.53) | 0.81(0.61) | 0.40(0.55) | 0.53(0.50) | 0.29(0.52) |
| Lifetime Parental Psychopathology | 0–3 | 0.99(0.90) | 1.73(0.73) | 1.19(0.99) | 1.00(0.49) | 0.95(0.91) |
| Maltreatment | 0–2 | 0.10(0.30) | 0.44(0.37) | 0.11(0.33) | 0.13(0.31) | 0.09(0.29) |
| Family Dysfunction | 0–3 | 0.87(0.83) | 1.48(0.66) | 0.80(0.73) | 1.01(0.73) | 0.85(0.84) |
| ADOLESCENT RISK | ||||||
| Poverty | 0–3 | 0.82(0.89) | 0.89(1.04) | 0.97(0.73) | 0.79(0.90) | |
| Loss and Violence Events | 0–2 | 0.46(0.62) | 0.55(0.68) | 0.78(0.68) | 0.43(0.61) | |
| Lifetime Parental Psychopathology | 0–3 | 1.09(0.85) | 1.38(1.03) | 1.18(0.51) | 1.05(0.85) | |
| Maltreatment | 0–2 | 0.19(0.39) | 0.51(0.51) | 0.20(0.37) | 0.15(0.36) | |
| Family Dysfunction | 0–3 | 0.80(0.80) | 1.28(0.85) | 1.44(0.96) | 0.72(0.75) | |
| YOUNG ADULT RISK | ||||||
| Poverty | 0–3 | 1.25(0.90) | 1.55(0.63) | 1.18(0.91) | ||
| Loss and Violence Events | 0–2 | 0.52(0.56) | 0.80(0.61) | 0.48(0.57) | ||
| Lifetime Parental Psychopathology | 0–3 | 1.10(0.81) | 1.49(0.72) | 1.05(0.81) | ||
| Maltreatment | 0–2 | 0.01(0.11) | 0.03(0.15) | 0.01(0.09) | ||
| Family Dysfunction | 0–3 | 0.24(0.46) | 0.63(0.60) | 0.20(0.45) |
1004 subjects had data on childhood (putative) risk factors. 877 subjects had data on adolescent (putative) risk factors, 837 had data on young adult putative risk factors.
Statistical Analyses
Weighted logistic regression models were estimated using generalized estimating equations (GEE) implemented by SAS PROC GENMOD. Robust (sandwich type) variance estimates adjusted the standard errors of the parameter estimates for the design effects. All analyses included sampling weights that were inversely proportional to selection probability; therefore, the results are representative of the population from which the sample was drawn. First, each depression onset group was examined separately, with child-onset versus never-depressed, adolescent-onset versus never-depressed, and young adult-onset versus never-depressed variables serving as outcome variables. Each (putative) risk factor sum score was examined individually for each depression onset group in univariate regression models. [Results for individual risk factors (as opposed to the sum scores) are available from the first author upon request]. Next, we also directly tested differences in the effect sizes of psychosocial risk factors among the depression onset groups. For example, we tested whether recent risk factors were more strongly associated with child- than with adolescent-onset depression. In order to test for these differences, we stacked childhood, adolescence, and young adulthood data, and tested interaction terms between risk factor sum scores and dummy variables indicating the timing of onset in the prediction of depression.
Because we conducted a large number of statistical tests, we focus on patterns of results rather than on single significant coefficients. We emphasize coefficients that are significant using two-tailed significance testing (i.e., at p < .05). However, considering that the hypotheses are directional in nature (i.e., higher levels of risk are associated with depression), coefficients significant at p < .10 are discussed when they are consistent with a larger pattern of significant results.
RESULTS
Replicating Previous Findings for Adult-Onset Depression
In order to replicate previous findings regarding adult-onset depression, we combined the adolescent- and young adult-onset groups into one group, a strategy used in previous research (see Figure 1a). Compared to the never-depressed, childhood poverty was the only childhood risk domain predicting adolescent-/adult-onset depression at p < .05 (OR = 1.65; 1.17–2.30, p < .01; see path “b” in Figure 1a). Thus, overall similarities in childhood psychosocial risk between the adult-onset depressed and the never-depressed were confirmed. To examine differences in childhood psychosocial risk between child- and adolescent-/adult-onset depression, we also tested interactions between risk factors and the timing of onset in the prediction of depression. Several factors were more predictive of child- than of adolescent-/adult-onset depression, including parental psychopathology (OR = 1.94; 1.09–3.46, p < .01 for the interaction term), maltreatment (OR = 8.55; 1.51–48.48, p < .05), and family dysfunction (OR = 2.36; 1.40–4.00, p < .05), but not childhood poverty and loss and violence events (OR = 1.21; 0.79–1.86, p > .10, and OR = 2.22; 0.77–6.37, p > .10, respectively). As in previous research, child- and adolescent-/adult-onset depression were mostly different in terms of childhood psychosocial risk, a finding previously interpreted as consistent with the risk differences hypothesis.
Recency versus Potentially Genuine Risk Differences
In order to disentangle differences in predictors among the depression onset groups caused by recency from potentially genuine risk differences, we first examined links between concurrent putative risk factors and the respective depression onsets (paths “c” in Figure 1b). Next we examined links between antecedent risk factors and depression onsets (i.e., childhood risk for adolescent-onset, and adolescent risk for young adult-onset depression; paths “d” in Figure 1b). All results are shown in Table 3.
Table 3.
Psychosocial risk factors predicting depression onset (compared to the never-depressed): Unadjusted odds ratios (95% CI),p-values.
| Risk Factors | Child-Onset | Adolescent-Onset | Young Adult-Onset | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Poverty | ||||||
| Childhood | 2.08 (1.62–2.69) | <.001 | 1.61 (1.04–2.49) | .03 a | 1.71 (1.06–2.76) | .03 |
| Adolescence | 1.12 (0.68–1.88) | .64 | 1.23 (0.84–1.81) | .28 | ||
| Young adulthood | 1.58 (1.10–2.28) | .01 a | ||||
| Loss and Violence Events | ||||||
| Childhood | 3.53 (1.49–8.35) | .004 | 1.43 (0.72–2.83) | .31 | 2.03 (1.03–4.03) | .04 |
| Adolescence | 1.35 (0.67–2.71) | .40 | 2.16 (1.02–4.58) | .04 | ||
| Young adulthood | 2.48 (0.91–6.77) | .08 a | ||||
| Lifetime Parental Psychopathology | ||||||
| Childhood | 2.31 (1.43–3.73) | .001 | 1.32 (0.84–2.06) | .23 | 1.06 (0.88–1.27) | .56 |
| Adolescence | 1.55 (0.86–2.78) | .15 | 1.20 (0.86–1.68) | .29 | ||
| Young adulthood | 1.96 (1.07–3.62) | .03 | ||||
| Maltreatment | ||||||
| Childhood | 9.28 (2.63–32.78) | .001 | 0.25 (0.03–2.14) | .20 | 2.95 (0.64–13.65) | .17 |
| Adolescence | 7.24 (1.71–30.62) | .007 | 1.65 (0.39–6.94) | .50 | ||
| Young adulthood | 3.36 (0.84–13.43) | .09 a | ||||
| Family Dysfunction | ||||||
| Childhood | 2.34 (1.54–3.54) | <.001 | 0.88 (0.58–1.35) | .55 | 1.25 (0.75–2.08) | .39 |
| Adolescence | 2.42 (1.39–4.20) | .002 | 3.02 (1.35–6.75) | .007 | ||
| Young Adulthood | 3.85 (1.66–8.94) | .002 | ||||
1004 subjects had data on childhood (putative) risk factors. 877 subjects had data on adolescent (putative) risk factors, 837 had data on young adult putative risk factors.
Odds ratios in bold were significant at p < .05. Odd ratios in bold and italics were significant at p < .10.
Shaded odds ratios represent associations between concurrent risk factors and depression onset.
No longer significant at p <.10 or less when comorbidity (i.e., concurrent anxiety and behavioral disorders) was taken into account.
Concurrent Putative Risk Factors
According to the recency hypothesis, concurrently assessed risk factors (paths “c” in Figure 1b, shown in the shaded cells of Table 3) should be similar in size for the three depression onset groups, and should have the strongest and most consistent links with depression onset. That is, childhood risk factors should have the strongest links with child-onset depression, adolescent risk factors should have the strongest links with adolescent-onset depression, and young adult risk factors should have the strongest links with young adult-onset depression.
The pattern of results suggest that, consistent with the recency hypothesis, all childhood putative risk factors were associated with child-onset depression, and young adult risk factors were associated with young adult-onset depression. Only adolescent maltreatment and family dysfunction (but not adolescent poverty, loss and violence events, and lifetime parental psychopathology) were associated with adolescent-onset depression.
Because several concurrent putative risk factors were linked with child- and young adult-onset depression, but not with adolescent-onset depression, we tested for putative risk differences between adolescent-onset depression and the two other depression onset groups. For example, in order to examine whether concurrent poverty was indeed more strongly associated with child-than with adolescent-onset depression, we examined the interaction between poverty and timing of depression onset in the prediction of depression, essentially testing whether the odds ratios for concurrent risk factors reported in Table 3 differed between child- and adolescent-onset depression. Concurrent poverty was more strongly linked with child- than with adolescent-onset depression (OR = 1.82; 1.02–3.46, p < .01 for the interaction term). Similarly, concurrent loss and violence events were more strongly linked with child- than with adolescent-onset depression at the statistical trend level (OR = 2.75; 0.88–8.58, p < .10 for the interaction term). No other differences in concurrent risk between child- and adolescent-onset and adolescent- and young adult-onset depression were significant. Summarizing results regarding concurrent putative risk factors (paths “c” in Figure 1b), the child- and young-adult onset depression groups were similar in terms of concurrent psychosocial risk. Indeed, follow-up analyses did not identify significant differences in concurrent risk for child- versus adult-onset depression. Adolescent-onset depression, however, appeared to have some differences in risk from these groups.
Antecedent Risk Factors
According to the recency hypothesis, one would expect to see some modest associations between risk factors from a previous developmental period and depression onset. That is, some childhood risk factors may modestly predict adolescent-onset depression, and some adolescent risk factors may modestly predict young adult-onset depression (paths “d” in Figure 1b). Results showed that childhood poverty predicted adolescent-onset depression, and that adolescent loss and violence events and family dysfunction predicted young adult-onset depression (see Table 3). Analyses examining potential differences in risk (i.e., differences in odds ratios) in antecedent risk factors between adolescent- and young adult-onset depression showed that antecedent family dysfunction was more predictive of young adult- than of adolescent-onset depression (OR = 3.12; 1.42–7.29, p < .05). Summarizing results regarding antecedent risk factors, adolescent- and young adult-onset depression were mostly similar in terms of antecedent psychosocial risk.
Childhood Risk Factors and Young Adult-Onset Depression
Finally, the recency hypothesis would predict weak links between childhood risk factors and young adult-onset depression. In fact, most childhood risk factors did not predict young adult-onset depression, with the exceptions of childhood poverty, and childhood loss and violence events (see Table 3).
Follow-Up Analyses
In multivariate models we included corresponding risk factors from childhood and adolescence to predict adolescent-onset depression, and from childhood, adolescence and young adulthood to predict young adult-onset depression. Results showed that when concurrent risk factors were included, the previously significant corresponding risk factors from previous developmental periods continued to predict adolescent- and young-adult-onset depression with similar effect sizes. Thus, the effects of earlier risk factors were not mediated by identical later risk. In another set of multivariate analyses we controlled for concurrent comorbidity. For example, for adolescent-onset depression, we controlled for adolescent anxiety and behavioral disorders. Most associations remained significant (see coefficients marked with “a” in Table 3 for exceptions).
DISCUSSION
This is the first epidemiological study that focuses specifically on associations of psychosocial adversity with child-, adolescent-, and young adult-onset depression in order to disentangle differences due to recency from potentially genuine risk differences. We also employed age of onset cut-offs for child- and adolescent-onset depression that correspond with the points at which changes in the prevalence of major depression occur (e.g., Angold et al., 2002).
Consistent with previous research, most childhood psychosocial risk factors were more predictive of child-onset than of adolescent-/adult-onset depression. When we attempted to disentangle potentially genuine differences in risk from differences due to the recency with which risk factors had been experienced, our pattern of results was mostly consistent with the recency hypothesis, particularly, for child- and young adult-onset depression: All childhood putative risk factors were associated with child-onset depression; and corresponding young adult putative risk factors were associated with young adult-onset depression. Only two of five adolescent putative risk factors were linked with adolescent-onset depression. Overall, our findings showed that differences in childhood risk reported in previous studies mostly reflected differences in the recency with which the risk factors had been experienced rather than genuine risk differences.
A few noteworthy inconsistencies with the recency hypothesis emerged. First, childhood poverty had long-lasting effects, and did not differentiate child- from later-onset depression. This finding was not entirely surprising. In Jaffee and colleagues' work, childhood socioeconomic status did not differentiate between child- and adult-onset depression (Jaffee et al., 2002). In Gilman and colleagues' work, childhood low socioeconomic status also did not differentiate among child-, adolescent-, and adult-onset depression (Gilman et al., 2003). Our follow-up analyses that controlled for later corresponding risk factors showed that the pathway from childhood poverty to later depression onset was not explained by poverty in adolescence or in young adulthood. Childhood may be a sensitive period during which the experience of poverty creates lasting changes in the organism's stress response (Miller et al., 2009, Power et al., 1999, Danese et al., 2009), and, thus, vulnerability to depression. Second, childhood loss and violence events predicted young adult-onset depression. Although parental loss predicted juvenile-, but not adult-onset depression in a previous paper (Jaffee et al., 2002), others have written about the long-lasting mental health effects of childhood loss events (Brown and Harris, 1978).
Third, all differences among the depression onset groups involved adolescent-onset depression, suggesting that there could be some genuine differences in risk between adolescent-onset depression and the other onset groups. Alternative pathways to adolescent-onset depression, particularly for females, have been suggested, including low birth weight (Costello et al., 2007), early pubertal timing (Copeland et al., 2010), increases in pubertal hormones (Angold et al., 2003), and biopsychosocial and cognitive interactions (e.g., Ge et al., 2001, Susman, 1997).
Limitations and Directions for Future Research
First, the study's focus was limited to psychosocial risk factors, but findings have important implications for gene-environment interaction research. For example, taking into account developmental nuances of environmental risk such as their timing in relation to depression onset may be important for increasing rates of replications in G X E research involving 5-HTTLPR (Canli and Lesch, 2007). Second, our assessments began at age 9, but we will have missed cases with depression onset before age 9, depression onset in the 9 months of the year that the CAPA/YAPA interviews did not cover, and depression onset during years when interviews were not conducted. Third, the depression onset groups were relatively small, limiting our statistical power. We also did not distinguish between juvenile-onset groups with recurrence versus those without recurrence, however, previous work had found few early adversity differences between such groups (Jaffee et al., 2002). Fourth, our last available age for this study was 21, so findings may be specific to the narrow young adult age range assessed here.
Fifth, several of our risk factors were assessed concurrently with depression, and therefore could be indicative only of “putative” risk similarities and differences among depression onset groups. We also did not assess risk factors antecedent to child-onset depression. Sixth, our findings are not informative with respect to causal chains leading to the onset of depression. Risk factors can also be heterogeneous in terms of their developmental history, and future research should examine interactions between risk factors at different developmental periods in the prediction of depression onset. Finally, in order to capture each risk domain in the most age-appropriate, developmentally valid way, some individual risk factors included in each risk domain varied somewhat between childhood/adolescence and young adulthood. These slight changes in the composition of risk domains could allow for an alternative interpretation of findings: That apparent similarities in associations between child/adolescent and young adult risk factors nevertheless disguise potential risk differences. Additional analyses showed, however, that when risk factors were forced to be identical across developmental periods or when risk factors were standardized within each developmental period, the overall findings did not change.
These limitations were balanced by the prospective longitudinal design of our study, and the reliability of CAPA and YAPA symptom assessment. Furthermore, they were not unique to our study. Indeed, the only other prospective longitudinal study of depression onset groups assessed depression at only six waves per subject, starting at age 10, and interviewed participants every 2, 3, or 5 years, using 12-month time frames for symptoms assessments (Jaffee et al., 2002). Future prospective longitudinal studies should aim for continuous coverage of depression onset data. This would determine whether findings are specific to depression onset at particular ages, and not just to any diagnosis of depression at these ages.
Despite these limitations, our study shows that when potentially genuine risk differences were disentangled from differences in the recency of risk, the number of putative psychosocial risk differences among developmentally defined depression onset groups is relatively small. Although distinguishing among developmental subtypes has been useful for other disorders (Moffitt et al., 2008), our findings suggest that assuming distinctions between child- and young adult-onset depression based on differences in psychosocial risk factors is unwarranted. Differences between adolescent-onset depression and the two other depression-onset groups may be consistent with studies showing that adolescent-onset depression is predicted by biological factors.
ACKNOWLEDGEMENTS
The work presented here was supported by the National Institute of Mental Health (MH63970, MH63671, MH48085), the National Institute on Drug Abuse (DA/MH11301), and the William T Grant Foundation.
All authors had full access to all in this study and Dr. Shanahan takes responsibility for the integrity of the data, and the accuracy of the data analysis.
Footnotes
No authors have any conflicts of interest to report.
REFERENCES
- Achenbach TM, Edelbrock C. Manual for the child behavior checklist and revised child behavior profile. Queen City Printers; Burlington, VT: 1983. [Google Scholar]
- Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1995;25:755–762. doi: 10.1017/s0033291700034991. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- Angold A, Cox A, Prendergast M, Rutter M, Simonoff E, Costello EJ, Asher BH. The Young Adult Psychiatric Assessment (YAPA) Duke University Medical Center; Durham, NC: 1999. [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: Effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Angold A, Worthman C, Costello EJ, Hayward C. Gender differences at puberty. Cambridge University Press; New York, NY US: 2003. Puberty and depression. [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA. Childhood and adolescent depression: A review of the past 10 years, Part I. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. The social origins of depression: A study of psychiatric disorder in women. Free Press; New York, NY: 1978. [Google Scholar]
- Canli T, Lesch KP. Long story short: the serotonin transporter in emotion regulation and social cognition. Nature Neuroscience. 2007;10:1103–1109. doi: 10.1038/nn1964. [DOI] [PubMed] [Google Scholar]
- Christie KA, Burke JD, Regier DA, Rae DS. Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. The American Journal of Psychiatry. 1988;145:971–975. doi: 10.1176/ajp.145.8.971. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. The development of depression in children and adolescents. American Psychologist. 1998;53:221–241. doi: 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Miller S, Costello EJ, Angold A, Maughan B. Outcomes of early pubertal timing in young women: A prospective population-based study. The American Journal of Psychiatry. 2010;167:1218–1225. doi: 10.1176/appi.ajp.2010.09081190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of youth: Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A, March J, Fairbank J. Life events and post-traumatic stress: The development of a new measure for children and adolescents. Psychological Medicine. 1998;28:1275–1288. doi: 10.1017/s0033291798007569. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Worthman C, Erkanli A, Angold A. Prediction from low birth weight to female adolescent depression: A test of competing hypotheses. Archives of General Psychiatry. 2007;64:343–350. doi: 10.1001/archpsyc.64.3.338. [DOI] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, Poulton R, Caspi A. Adverse childhood experiences and adult risk factors for age-related disease. Archives of Pediatric and Adolescent Medicine. 2009;163:1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH., JR Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B. Ages of onset of psychiatric disorders in a community population of older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:706–717. doi: 10.1097/00004583-199406000-00012. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Socio-economic status, family disruption and residential stability in childhood: Relation to onset, recurrence and remission of major depression. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2003;33:1341–1355. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- Goodyer IM. The depressed child and adolescent. 2nd ed. Cambridge University Press; New York, NY US: 2001. Life events: Their nature and effects. [Google Scholar]
- Harrington R, Gillberg C, Steinhausen H. A clinician's handbook of child and adolescent psychiatry. Cambridge University Press; New York, NY US: 2006. Affective disorders. [Google Scholar]
- Hill J, Pickles A, Rollinson L, Davies R, Byatt M. Juvenile- versus adult-onset depression: Multiple differences imply different pathways. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2004;34:1483–1493. doi: 10.1017/s0033291704002843. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Kasch KL, Klein DN. The relationship between age at onset and comorbidity in psychiatric disorders. Journal of Nervous and Mental Disease. 1996;184:703–707. doi: 10.1097/00005053-199611000-00008. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Martin A, King RA, Charney D. Are child-, adolescent-, and adult-onset depression one and the same disorder? Biological Psychiatry. 2001;49:980–1001. doi: 10.1016/s0006-3223(01)01127-1. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Feinberg TL, Crouse-Novac M, Paulauskas SL, Pollok M, Finkelstein R. Depressive disorders in childhood. II. A longitudinal study of the risk for a subsequent major depression. Archives of General Psychiatry. 1984;41:643–649. doi: 10.1001/archpsyc.1984.01790180013001. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. The American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, Cole S, Kobor MS. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. PNAS Proceedings of the National Academy of Sciences of the United States of America. 2009;106:14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, Slutske WS, Viding E. Research review: DSM-V conduct disorder: Research needs for an evidence base. Journal of Child Psychology and Psychiatry. 2008;49:3–33. doi: 10.1111/j.1469-7610.2007.01823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Cicchetti D, Cohen DJ. Developmental psychopathology, Vol 3: Risk, disorder, and adaptation. 2nd ed. John Wiley & Sons Inc.; Hoboken, NJ US: 2006. Life-course-persistent versus adolescence-limited antisocial behavior. [Google Scholar]
- Power C, Manor O, Matthews S. The duration and timing of exposure: Effects of socioeconomic environment on adult health. American Journal of Public Health. 1999;89:1059–1065. doi: 10.2105/ajph.89.7.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Ryan ND, Birmaher B, Dahl RE. Unipolar depression in adolescents: Clinical outcome in adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:566–578. doi: 10.1097/00004583-199505000-00009. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® Software. Version 9 Cary, NC: 2004. [Google Scholar]
- Schaie KW. A general model for the study of developmental problems. Psychological Bulletin. 1965;64:92–107. doi: 10.1037/h0022371. [DOI] [PubMed] [Google Scholar]
- Susman EJ. Modeling developmental complexity in adolescence: Hormones and behavior in context. Journal of Research on Adolescence. 1997;7:283–306. [Google Scholar]
- Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, Ryan ND, Dahl RE, Steinberg D. Children with prepubertal-onset major depressive disorder and anxiety grown up. Archives of General Psychiatry. 1999;56:794–801. doi: 10.1001/archpsyc.56.9.794. [DOI] [PubMed] [Google Scholar]
- Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: An overview epidemiology, clinical manifestation and risk factors. Child and Adolescent Psychiatric Clinics of North America. 2006;15:827–841. doi: 10.1016/j.chc.2006.05.002. [DOI] [PubMed] [Google Scholar]