Abstract
Objective
To conduct a meta-analysis of the association between depression and medication adherence among patients with chronic diseases. Poor medication adherence may result in worse outcomes and higher costs than if patients fully adhere to their medication regimens.
Data Sources
We searched the PubMed and PsycINFO databases, conducted forward searches for articles that cited major review articles, and examined the reference lists of relevant articles.
Study Eligibility Criteria, Participants, and Interventions
We included studies on adults in the United States that reported bivariate relationships between depression and medication adherence. We excluded studies on special populations (e.g., substance abusers) that were not representative of the general adult population with chronic diseases, studies on certain diseases (e.g., HIV) that required special adherence protocols, and studies on interventions for medication adherence.
Study Appraisal and Synthesis Methods
Data abstracted included the study population, the protocol, measures of depression and adherence, and the quantitative association between depression and medication adherence. Synthesis of the data followed established statistical procedures for meta-analysis.
Results
The estimated odds of a depressed patient being non-adherent are 1.76 times the odds of a non-depressed patient, across 31 studies and 18,245 participants. The association was similar across disease types but was not as strong among studies that used pharmacy records compared to self-report and electronic cap measures.
Limitations
The meta-analysis results are correlations limiting causal inferences, and there is some heterogeneity among the studies in participant characteristics, diseases studied, and methods used.
Conclusions
This analysis provides evidence that depression is associated with poor adherence to medication across a range of chronic diseases, and we find a new potential effect of adherence measurement type on this relationship. Although this study cannot assess causality, it supports the importance that must be placed on depression in studies that assess adherence and attempt to improve it.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1704-y) contains supplementary material, which is available to authorized users.
KEY WORDS: depression, adherence, chronic disease, meta-analysis
INTRODUCTION
Poor adherence to prescribed medication is a well-known problem. Estimates for levels of medication adherence in chronic disease range from 20% to 80%, 1–3 and poor outcomes due to non-adherence are well documented and result in added health care costs in the United States. 4,5 Recent studies confirm that poor adherence is associated with higher costs across a range of diseases including heart failure, 6 osteoporosis, 7,8 Parkinson’s disease, 9 Crohn’s disease, 10 cardiovascular disease, 11 kidney transplant, 12 and diabetes. 13 Non-adherence has been associated with higher rates of mortality in cardiovascular disease and diabetes. 14–16 Despite the obvious nature of the medication adherence problem, interventions to improve adherence have not been overwhelmingly successful, in part because of the lack of understanding about true barriers to adherence. 17,18
Researchers report on a wide range of barriers to adherence, including health system, provider, and patient factors. 1,4,19–22 It has long been known that psychological distress can affect medical well being, 23 and the effect of depression on medication adherence may be one mechanism through which mood disorders affect health outcomes. Whether from lack of energy, motivation, social withdrawal, feelings of hopelessness, or changes in cognition and expectations about the benefits or harms of treatment, patients with depression have many risk factors that could contribute to non-adherence. Patients with depression may also have more difficulty with patient–provider communication and less satisfaction with their care 24.
Two prior meta-analyses examined the association between depression and adherence to treatment recommendations. 25,26 In a meta-analysis of studies from 1968 to 1998, DiMatteo et al. 25 included 12 studies of the association between depression and treatment adherence, but only five studies examined medication adherence with a total of 284 patients. In these five studies, the odds of non-adherence were threefold greater in depressed patients compared to non-depressed patients. 25 In a more recent meta-analysis, Gonzalez et al. 26 reviewed 47 studies on diabetes treatment adherence, but only 14 of the studies focused on medication adherence. The association between depression and medication adherence for those 14 studies was similar to that observed by DiMatteo et al.
Conclusions about the association between depression and medication adherence from these two earlier reviews are limited by the number of studies and the types of diseases included. First, there is a risk of publication bias when analyzing a small number of studies. For example, Gonzalez reported a small fail safe number (n = 24) for the medication adherence studies, suggesting that a relatively small number of unpublished studies with null results could change the outcome of the analysis. 27 Second, two common chronic conditions, hyperlipidemia and hypertension, were not included in either review. Third, the small number of studies precluded analysis of important potential moderators of the association such as disease type, measures of adherence (which are known to affect adherence rates 28,29), measures of depression, and sample size. Finally, the barriers influencing adherence to medication differ from those affecting adherence to other therapies such as diet and exercise, 30 and a focus specifically on medication-related adherence is warranted. To address these important issues, we reviewed the recent literature on the association between depression and medication adherence across a range of chronic diseases, performed a meta-analysis to evaluate the strength and direction of this association, and conducted a series of key moderation analyses.
METHODS
Data Sources
We followed the example of previous researchers to conduct our systematic review. 25,26 We searched the PubMed and PsycInfo databases for English-language articles published from 1998 to April, 2009. Dissertations, conference proceedings, and book chapters were excluded, and publication types of “letters,” “editorials,” and “comments” were omitted. Specific articles 22,31–33 were the basis of an additional forward search (i.e., articles citing the selected articles) and a related-article search in the PubMed database.
We searched PubMed and PsycInfo using synonyms for the following terms: adherence (e.g., compliance, non-adherence, and refusal), depression (e.g., depressive disorder and mental health), barriers (e.g., predictors, determinants, and factors), and medication (e.g., drugs, drug therapy, pharmaceutical, and prescription). The complete list of search terms and the search strategy are available online in Appendix 1.
Study Selection
We included observational studies that examined depression as a barrier to medication adherence among U.S. adults, including studies that described “predictors,” “facilitators,” or “determinants” of medication adherence and those studies that examined the “relationship” between specific barriers and adherence. We included only U.S.-based studies, since the effect of depression on adherence is likely influenced heavily by culture and other factors of the healthcare system, and we aimed to focus our results to be most applicable to the US. 34 We included only studies of adults over age 18, since adherence barriers for children can be very different from those of adults.
Studies testing an intervention for medication adherence were excluded, as they have been in prior reviews. 25 We also excluded studies that did not define adherence or specify its method of measurement. We excluded any studies focused specifically on people who were homeless or substance abusers, patients with schizophrenia or other psychotic disorders, tuberculosis, or HIV, and studies examining injectable medication, because of the unique circumstances that surround medication adherence for each of these populations. HIV regimens in particular have required an exceptionally high level of adherence (>95%) to be effective, 35,36 have a unique side effect profile, and are prescribed in unique settings, which makes them not comparable to regimens for other chronic diseases of interest to this study. We also excluded studies focusing solely on adherence to antidepressants.
The principal outcome of interest was medication adherence, which was defined as taking medication as prescribed by a health care provider. The types of non-adherence in the review included the following: (a) non-fulfillment (primary non-adherence), where patients do not fill prescriptions written by providers (b) non-persistence, where patients discontinue taking a prescribed medication without being advised to do so by a provider, and (c) non-conforming (our term for what is typically referred to as “non-adherence”), where patients fail to take medications as prescribed, for example, by skipping doses or taking doses at the wrong time. There is no gold standard for assessing medication adherence, so a variety of methods were accepted for this review. These methods ranged from self-report (e.g., questionnaires or interviews) to more objective measures such as electronic cap event monitoring and examination of pharmacy or medical records.
Two researchers (WG, JG) independently reviewed all titles retrieved using the search strategies. Titles were excluded if it was clear that the topic was not relevant to the current review. Abstracts of the remaining articles were examined independently by the same two researchers for the inclusion criteria listed above, and full articles were retrieved for abstracts meeting the inclusion criteria. Data collected on the full articles (see data extraction below) were used to exclude articles that did not meet the study eligibility criteria. The two reviewers resolved differences between them by consensus.
Data Extraction
We developed a worksheet form to collect data from the articles based upon the objectives for the current review. Two authors (WG, JG) independently collected data from the studies and compared results. Discrepancies between the reviewers were resolved by discussing the relevant points with each other until a consensus was reached. We examined the data to identify duplicate studies in the review (i.e. comparing author names, study location, population characteristics, study dates, and sample sizes). We did not contact any authors for additional information.
The data collection form contained the following items: (a) study design (e.g., cross-sectional, prospective, or case control), (b) participant characteristics including percentage of males, seniors (65 and over), and ethnic/racial category, (c) study characteristics including study location, recruitment method, and sample size, (d) chronic disease studied, (e) medication adherence assessment type (non-fulfillment, non-persistence, non-conforming), and (f) method of medication adherence evaluation (self-report, pill count, electronic monitoring, pharmacy or medical records).
We collected data specific to depression from each study, including the instrument used to measure depression or depressive symptoms (e.g. Beck Depression Inventory), whether depression was assessed in the article using ICD-9 code or another tool to report a diagnosed condition versus measured using symptom scales, and assessment of comorbid conditions. In addition, we determined if the reliability and validity of the depression scale was documented in the article by the authors. Methodological quality of the articles was discussed, but no formal scales were used for assessment.
One author (JG) collected the specific variables required for the meta-analysis; this data was then checked by a statistical analyst. The data included the following: analysis types, number of participants, effect size (correlation coefficient, odds ratio, etc.), standard error, confidence interval, P-value, means or proportions of groups, and type of variables used to measure adherence and depression.
Statistical Analyses and Data Synthesis
Data extracted from studies that reported bivariate associations between depression and medication adherence were evaluated for pooling. We included multiple studies from a single article in the meta-analysis if the participant samples were collected independently. For studies that reported effect sizes for more than one measure of adherence or depression, we selected the one measure more likely to be objective (e.g., pharmacy records over self-report) or the one that used a continuous scale, which would provide more statistical power to detect effects than a scale that was dichotomized (e.g., adherent and non-adherent).
We followed methods previously used by DiMatteo et al. 25 and by Gonzalez et al. 26 to conduct the meta-analysis and used the correlation effect size (r). 27,37 In some cases, studies reported the correlation coefficient (r) between medication adherence and depression. When the effect size r was not reported, we calculated it from the t or χ2 statistics and odds ratios. 27 In studies reporting only the regression coefficient between medication adherence and depression, we used the formula suggested by Gonzalez et al. 26 and Peterson to calculate the effect size. 38 For one study, 39 simulation was used to generate r from the reported adherence rate (mean and standard deviation) for each level of depression score. Using the mean and standard deviation, we drew randomly from a normal distribution for the number of observations in each group to obtain an estimated adherence rate for all patients in the sample. 40 We then used the correlation between these estimates and depression level as the effect size. Results reported as non-significant (i.e. P > 0.05) were assigned a conservative estimate of an effect size of 0.
We calculated summary statistics, including median and mean effect size, for r using Fisher’s z transformation of r. The 31 studies were significantly heterogeneous (P < 0.01); thus we employed a random effects model to calculate the 95% confidence intervals for the weighted and unweighted mean effect sizes. Weighted and unweighted effect size d and an odds ratio are reported. 27,41 We calculated the risk difference and relative risk using the weighted effect size 42.
We performed random effect meta-regressions 43 to examine the effect of each covariate of interest on r. Covariates we examined included method of effect size calculation, sample size, disease type, depression as the focus of the study (versus an included covariate), medication adherence evaluation method and the use of a validated depression scale. In addition, we evaluated the selective publishing of significant results over non-significant results by calculating the overall “fail safe n” and tolerance level. 27 Stata 10.1 was used to conduct all analyses 44.
RESULTS
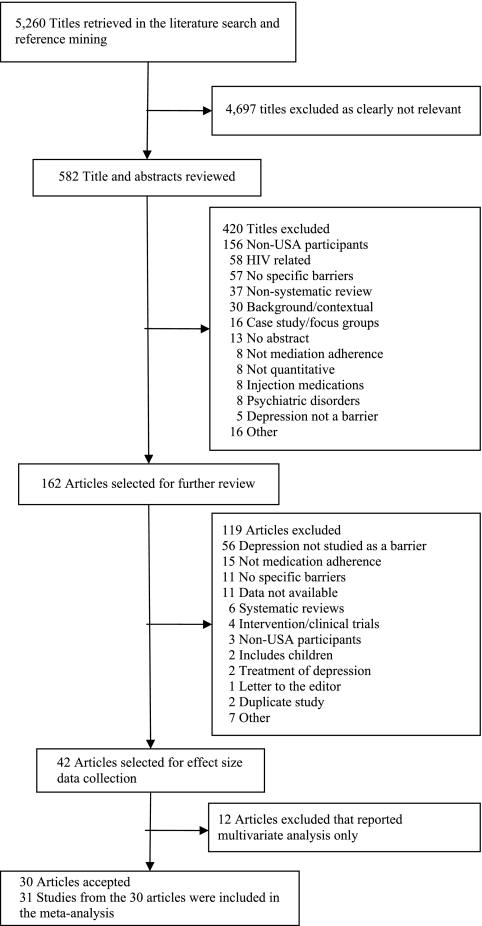
The literature search and reference mining returned 5,260 titles, and of these titles, we selected 582 for further review (see Fig. 1). One study from the DiMatteo et al. 25 review and four from the Gonzalez et al. 26 review met our inclusion criteria. A total of 42 articles met our eligibility requirements, but collection of effect size data determined that only 30 of the 42 articles included the bivariate association data required for pooling the results. Twenty-nine of the articles reported results for a single sample of participants, and one article 45 reported effect sizes for two independently collected samples. As a result, we analyzed 31 studies across the 30 articles.
Figure 1.
Flow diagram of study selection.
The studies covered a range of diseases, with coronary heart disease, diabetes, hyperlipidemia, and hypertension comprising the bulk of the studies (see Table 1). Appendix 2, available online, presents all the data collected from these studies. A negative effect size indicates that a higher level of depression or depressive symptoms is related to lower levels of medication adherence.
Table 1.
Number of Articles Listed by Disease Studied
| Disease | Number of Articles* | References |
|---|---|---|
| Anticoagulation therapy | 1 | [62] |
| Asthma | 3 | [31, 63, 64] |
| Coronary Heart Disease | 4 | [46, 65–67] |
| Diabetes | 6 | [68–73] |
| Glaucoma | 1 | [39] |
| Heart failure | 1 | [74] |
| Hemodialysis/Kidney transplant | 1 | [75] |
| Hyperlipidemia/ Hypertension | 8 | [76–83] |
| Systemic Lupus Erythematosus | 1 | [45] |
| Multiple Diseases or Not Specified | 4 | [22, 84–86] |
* One article included two independent studies for a total of 31 studies across the 30 articles
Measures of adherence included self-report for 17 studies, electronic caps for eight studies, and pharmacy records for six studies. The association between depression and adherence was the focus of seven studies, and the remaining 24 studies focused on other barriers to adherence including depression as a potential confounder. Measures of depression included self-report scales for 28 studies and depression diagnosis on a medical chart for three studies. Among the instruments used to assess depression and depressive symptoms, the Center for Epidemiological Studies Depression Scale (CES-D) was the most common (eight studies), the Patient Health Questionnaire (PHQ) was second (six studies), the Beck Depression Inventory (BDI) was third (four studies) with the remaining studies using nine different scales. The study sample sizes ranged from 47 to 8,406, and the total number of participants included in this meta-analysis was 18,245.
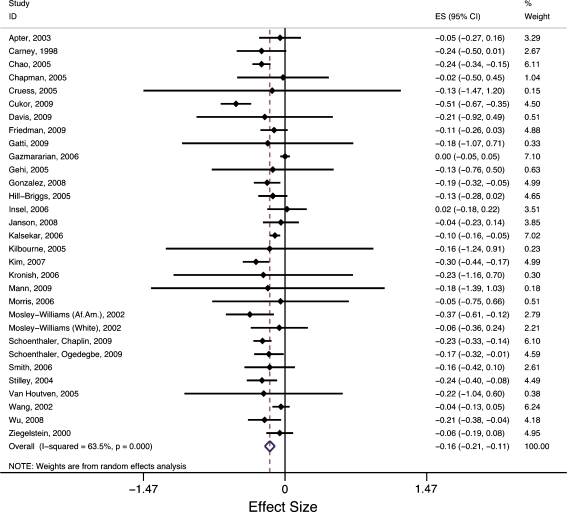
The results of the meta-analysis presented in Table 2 show a significant association between depression and medication adherence. While the weighted mean effect is of modest size, it is negative and achieves statistical significance (r = −0.16, 95% CI −0.20,−0.11, P < 0.001). The estimated odds of a depressed patient being non-adherent are 1.76 times that of the odds of a non-depressed patient (weighted mean odds ratio). This corresponds to a risk difference in non-adherence between depressed and non-depressed patients of 16%. Figure 2 shows a forest plot of z-transformed correlation effect sizes with a graphic representation of the weighted confidence intervals for each study. The random effects pooled value is shown at the bottom of the figure.
Table 3.
Appendix 2. Selected Articles on the Association between Depression and Adherence to Medication Therapies
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
|---|---|---|---|---|---|---|---|---|---|
| Apter et al. 2003 [63] | Asthma | Observational cohort 2000–2002 | Enrolled: 88 Responding at f/u: 85 | Multiple clinic: University of Pennsylvania | Convenience sample | Electronic monitoring: Prescribed doses taken within specified period | 20-item Center for Epidemiological Studies Depression Scale (CES-D), cutoff >=16 | −0.05 (−0.27, 0.16) | Depression was not significantly associated with adherence in bivariate analysis (OR = 0.99, 95% CI 0.95–1.03, P= 0.50). Thus, it was not included in the multivariate model. |
| Carney et al. 1998 [66] | Coronary Heart Disease | Observational cohort Dates not available | Enrolled: 78 Responding at f/u: 62 | Single clinic/ hospital/ pharmacy | Convenience sample | Electronic monitoring: Prescribed doses taken within specified period | Beck depression inventory | −0.24 (−0.50,0.01) | Multivariate analysis was not reported in this study. |
| Chao et al. 2005 [70] | Diabetes | Cross-sectional 2003–2003 | Enrolled: 445 | Health plan: Midwestern United States | Random sample via mailings | Morisky and Horne scales | Patient Health Questionnaire (PHQ-8) | −0.24 (−0.34,−0.15) | In structural equation modeling, no direct effect was found between depressive symptoms and adherence (Beta = −0.04), although the relationship may be mediated through perceived barriers to medication use, perceived side-effects, and self-efficacy. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Chapman et al. 2005 [78] | Hyperlipidemia Hypertension | Retrospective cohort 1997–2001 | Enrolled: 8,406 | Health plan | All new patients with disease from study site | Proportion of days covered | Depression diagnosis in chart | −0.02 (−0.50, 0.45) | Depression diagnosis was not associated with adherence in a multivariate model (OR = 0.94; 95% CI 0.78,1.13; P=.51) after adjusting for demographics, comorbidity, and history of health services use. |
| Cruess et al. 2009 [62] | Anticoagulation therapy | Prospective cohort Dates not available | Enrolled: 156 | Multiple clinics: Pennsylvania | All patients with disease from study site | Electronic monitoring: Prescribed doses taken with specified period | Millon Behavioral Medicine Diagnostic depression subscale | −0.13 (−1.47, 1.20) | Depression diagnosis was not significant in a logistic regression model (OR = 0.006; 95% CI −0.018,0.03; P = .64) after adjusting for demographics, indication for warfarin, and clinic site. |
| Cukor et al. 2009 [75] | Kidney transplant, Hemodialysis | Cross-sectional Dates not available | Enrolled: 159 | Single clinic/ hospital/ pharmacy: New York | Convenience sample | Medication TherapyAdherence Scale | Beck Depression Inventory (BDI) | −0.51 (−0.67, −0.35) | In a multiple regression model, depression was significantly associated with adherence (beta = −.287, P<.01) after adjusting for demographics, mode of treatment, and locus of control. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Davis et al. 2009 [86] | Diabetes, Hypertension, Seizures | Cross-sectional Dates not available | Enrolled: 472 | Single clinic/hospital/ pharmacy | Convenience sample | Self report, 2 items | Brief Symptom Index of Depression 7 items | −0.21 (−0.92, 0.49) | Depression was significantly associated with lower adherence in a multivariate model (OR = 2.83; 95% CI 1.63, 4.91; P < .001) after adjusting for demographics and drug/alcohol use. |
| Friedman et al. 2009 [39] | Glaucoma | Observational cohort 2006–2007 | Enrolled: 282 Responding at f/u: 196 | Multiple sites | All non-surgical patients with disease from study site | Travatan Dosing Aid: Prescribed doses taken with specified period, Cutoff: 75% | 10-item Center for Epidemiological Studies Short Depression scale | −0.11 (−0.26, 0.03) | Depression was not significant in the multivariate model. |
| Gatti et al. 2009 [84] | Hypertension, Hyperlipidemia, Diabetes, Other | Cross-sectional June – Oct 2006 | Enrolled: 281 Responding at f/u: 275 | Multiple pharmacies: Atlanta, Georgia | Systematic Convenience Sample | Morisky-8 Item Medication Adherence Scale | 1-question from 12-item Medical Outcomes Survey (MOS SF-12) | −0.18 (−1.07, 0.71) | Depressive symptoms were not associated with adherence in multivariate analysis adjusting for health literacy and beliefs about medication. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Gazmararian et al. 2006 [87] | Coronary Heart Disease Diabetes Hyperlipidemia Hypertension | Observational cohort Dates not available | Enrolled: 1,540 | Multiple sites: Ohio, Texas, and Florida | All patients with disease from study site | Cumulative medication gap based upon pharmacy claims, Cutoff: 80% | Self-report | 0.00 (−0.05, 0.05) | Depression was not associated with medication adherence in bivariate analysis and was not included in the multivariate model. |
| Gehi et al. 2005 [65] | Coronary Heart Disease | Cross-sectional 2000–2002 | Enrolled: 940 | Multiple sites in California | All patients with disease from study site | Self report using 3 questions | Patient Health Questionnaire (PHQ-9) | −0.13 (−0.76, 0.50) | Depression was associated with not taking medication as prescribed (OR = 2.2, 95% CI: 1.2–3.9) after adjusting for demographics, medical history, medication use and cardiac function. |
| Gonzalez et al. 2008 [69] | Diabetes | Observational cohort 2001– 2003 | Enrolled: 208 | Two clinics in Massachusetts | All patients with disease from study site | Self-Report of prescribed doses taken in the past 7 days, Cutoff: 100% | 10-item Harvard Department of Psychiatry/National Depression Screening Day Scale (HANDS) | −0.19 (−0.32, −0.05) | Depression was associated with non-adherence (OR = 1.08; 95% CI 1.001–1.16) after controlling for demographics, comobidity, and baseline self-care. |
| Hill-Briggs et al. 2005 [71] | Diabetes | Cross-sectional 1995–1997 | Enrolled: 172 | African Americans from multiple clinics: Johns Hopkins, Maryland | Participants in clinical trial | Modified Morisky | 20-item Center for Epidemiological Studies Depression Scale (CES-D) | −0.13 (−0.28, 0.02) | Multivariate analysis of depression and adherence was not performed. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Insel et al. 2006 [83] | Hyperlipidemia, Hypertension, Arthritis | Observational cohort Dates not available | Enrolled: 100 | Community sample | Convenience sample | Proportion of days covered using medication monitoring caps. | 30-item Geriatric Depression Scale (GDS) | 0.02 (−0.18, 0.22) | Depression was not associated with medication adherence scores in multivariate regression after controlling for demographics, illness severity, and executive functioning. |
| Janson et al. 2008 [31] | Asthma | Observational cohort 2000–2003 | Enrolled: 113 | Multiple clinic: Northern California | Convenience sample | Self-report prescribed doses taken with specified period, Cutoff: 50% | 20-item Center for Epidemiological Studies Depression Scale (CES-D), cutoff> = 16 | −0.04 (−0.23, 0.14) | Depression was not associated with medication adherence in bivariate analysis and was not included in the multivariate model. |
| Kalsekar et al. 2006 [72] | Diabetes | Observational cohort 1998–2001 | Invited: 1,326 | State: West Virginia Medicaid | All patients with disease from study site | Medication possession ratio | Depression diagnosis in chart | −0.10 (−0.16, −0.05) | Depression was associated with non-adherence (beta=−0.057, P = 0.019) after adjusting for demographics, comorbidity, provider interactions, treatment complexity, and diabetes severity. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Kilbourne et al. 2005 [73] | Diabetes | Observational cohort 2000–2001 | Enrolled: 203 Responding at f/u: 196 | Single clinic/ hospital/ pharmacy: VA | All patients with disease from study site | Electronic medication monitoring 30 days and prescription refill data | Patient Health Questionnaire (PHQ-9) | −0.16 (−1.24, 0.91) | Depression was associated with 20% fewer days with adequate medication coverage based on pharmacy fill data (beta= −20, 95% CI −40, −1) after adjusting for demographics, cognitive impairment, binge drinking, and number of medications. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Kim et al. 2007 [79] | Hypertension | Cross-sectional 2003–2004 | Enrolled: 208 | Community sample from Baltimore- Washington area | Participants in clinical trial | Modified Hill-Bone Compliance Scale | 21-item Kim depression Scale for Korean Americans (KDSKA) | −0.30 (−0.44, −0.17) | There was no significant relationship between depression and intentional (OR 1.012, 95% CI 0.95, 1.07) or non-intentional (OR 1.02, 95% CI 0.97, 1.07) non-adherence after adjusting for demographics, comorbid conditions, adverse effects, social support, satisfaction with care, and high blood pressure knowledge, beliefs and self-efficacy. |
| Kronish et al. 2006 [46] | Coronary Heart Disease | Observational cohort 2003–2005 | Enrolled: 560 Responding at f/u: 492 | Three sites in New Jersey, New York, and Connecticut. | All patients with disease from study site | Validated scale: Morisky | Beck Depression Inventory (BDI) | −0.23 (−1.16, 0.70) | Patients with persistent depression after 3 months were significantly less likely to report taking medications as prescribed (OR 0.50, 95% CI 0.27, 0.95) after adjusting for demographics and comorbidity. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Mann et al. 2009 [68] | Diabetes | Cross-sectional 2007–2007 | Enrolled: 151 | Single clinic/ hospital/ pharmacy: New York City | Convenience sample | Morisky scale | Patient Health Questionnaire (PHQ-9), cutoff ≥ 10 | −0.18 (−1.39, 1.03) | Depression was non-significant and dropped from the multivariate model in stepwise elimination. |
| Morris et al. 2006 [80] | Hypertension | Cross-sectional 2002–2003 | Enrolled: 492 | Single clinic/ hospital/ pharmacy: Indiana | Participants in clinical trial | 1. Prescription Claims: Medication possession ratio 2. Morisky scale (modified) | Patient Health Questionnaire (PHQ-8), cutoff ≥ 10 | −0.05 (−0.75, 0.66) | Depression was not significantly associated with refill adherence (OR 0.94, 95% CI 0.63, 1.40) after adjusting for age, marital status, and race. Depression was, however, associated with self-reported adherence (OR 0.48, 95% CI 0.32, 0.72). |
| Mosley-Williams et al. 2002 [45] | Systemic Lupus Erythematosus | Cross-sectional Dates not available | Enrolled: 68 | Multiple clinics: African American women | Random sample | Self Report: frequency of failing to take medications when prescribed during the past year (5-point likert) | 20-item Center for Epidemiological Studies Depression Scale (CES-D) | −0.37 (−0.61, −0.12) | Multivariate analysis of depression and adherence was not performed. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Mosley-Williams et al. 2002 [45] | Systemic Lupus Erythematosus | Cross-sectional Dates not available | Enrolled: 54 | Multiple clinics: Caucasian Women | Random sample | Self Report: frequency of failing to take medications when prescribed during the past year (5-point Likert) | 20-item Center for Epidemiological Studies Depression Scale (CES-D) | −0.06 (−0.36, 0.24) | Multivariate analysis of depression and adherence was not performed. |
| Schoenthaler Chaplin, et al. 2009 [76] | Hypertension | Cross-sectional Dates not available | Enrolled: 439 | Multiple clinics: New York City | All patients with disease from study site | Morisky scale | Patient Health Questionnaire (PHQ-9) | −0.23 (−0.33, −0.14) | Depressive symptoms were significantly associated with lower medication adherence (β = −0.18, P = 0.001) after adjusting for age, gender, education, income, comorbidity, provider degree, and provider communication. |
| Schoenthaler Ogedegbe, et al. 2009 [77] | Hypertension | Observational cohort Dates not available | Enrolled: 190 Responding at FU: 167 | Multiple clinics: New York City | All patients with disease from study site | Morisky scale | 20-item Center for Epidemiological Studies Depression Scale (CES-D), cutoff ≥ 16 | −0.17 (−0.32, −0.01) | Medication adherence at 3-month follow-up was not associated with baseline depressive symptoms (beta = 0.010, P=.087 after adjusting for the mediating effects of self-efficacy. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Smith et al. 2006 [64] | Asthma | Observational cohort 2001–2002 | Enrolled: 82 Responding at f/u: 59 | Single clinic/ hospital/ pharmacy: Baltimore | Consecutive patients | Electronic monitoring: Prescribed doses taken within 2-week period. | 11-item Center for Epidemiologic Studies-Depression (CES-D) scale, cutoff ≥ 10 | −0.16 (−0.42, 0.10) | Depressive symptoms were significantly associated with adherence to asthma therapy (beta=−0.016, P = 0.028) after controlling for age, gender, and education. |
| Stilley et al. 2004 [82] | Hyperlipidemia | Observational cohort 1992–1995 | Enrolled: 158 | Community Sample: Southwest Pennsylvania | Volunteers, response to ads | Electronic monitoring: Percent days compliant | Hamilton Depression Scale | −0.24 (−0.40, −0.08) | Depression was not examined as an independent predictor in multivariate analysis. Psychologic distress (anxiety or depression) was not associated in fully adjusted models with adherence that controlled for personality, intelligence, mental flexibility and verbal learning. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Van Houtven et al. 2005 [85] | Not specified | Cross-sectional 2002 | Enrolled: 545 | Community Sample: Durham County | Random sample | Self Report: “During the past 12 months, did you either delay or not get a prescription that a doctor or provider prescribed for you?” | PRIME-MD 1000 Depression Measure | −0.22 (−1.04, 0.60) | Feeling down or depressed was significantly associated with delaying or not getting a prescription (OR = 2.71; 95%CI: 1.58, 4.66) after adjusting for demographics, economic constraints, self-reported health, and perceived discrimination. |
| Wang et al. 2002 [81] | Hypertension | Cross-sectional 1996 | Enrolled: 496 | Multiple clinics: Boston | Random sample | Prescription claims: Proportion of days covered | Brief Symptom Inventory Depression Subscale | −0.04 (−0.13, 0.05) | Depressive symptom severity was associated with non-adherence (OR = 0.93; 95%CI: 0.87, 0.99 for every point increase in the 14-point depression score) after adjusting for demographics, site of treatment, the use of thiazide diuretics, locus of control, and the presence of comorbid medical conditions. |
| Citation | Disease Studied | Study Design & Dates | Number of Participants | Patients | Sample Description | Measure of Adherence | Measure of Depression | Bivariate Effect Size (95% CI) | Multivariate Regression Key Findings |
| Wu et al. 2008 [74] | Heart failure | Observational cohort Dates not available | Enrolled: 134 | Multiple clinics: Kentucky | Convenience sample | Electronic monitoring: Proportion of days correct number of doses taken. | Patient Health Questionnaire (PHQ-9) | −0.21 (−0.38, −0.04) | Depression was not significantly associated with adherence measured as the percentage of correct doses taken per day (beta = 0.028, P = 0.790) after adjustment for demographics including SES, comorbidity, treatment variables, and relationship with provider. |
| Ziegelstein et al. 2000 [67] | Coronary Heart Disease (Post Myocardial Infarction | Observational cohort Dates not available | Enrolled: 276 Responding at f/u: 204 | Single clinic/ hospital/ pharmacy: Maryland | Consecutive patients | Medical Outcomes Study Adherence Specific Scale | Beck Depression Inventory: cutoff ≥ 10 | −0.06 (−0.19,−.08) | Results for multivariate analyses were not provided. |
Table 2.
Summary of Meta-Analysis Results
| Item | N | Heterogeneity Test (Q) | Median r | Mean r Un-weighted (95% CI) | Mean r Weighted (95% CI) | Cohen d | Odds Ratio (95% CI) | Risk Difference (%) | Relative Risk |
|---|---|---|---|---|---|---|---|---|---|
| All studies | 31 | P < 0.01 | −0.16 | −0.16 (−0.47,0.19) P = 0.373 | −0.16 (−0.20,−0.11) P < 0.001 | −0.32, −0.31 | 1.76 (1.33,2.57) | 16 | 1.33 |
| By Disease:* | |||||||||
| Diabetes | 6 | P= 0.22 | −0.17 | −0.17 (−0.74,0.56) P = 0.682 | −0.16 (−0.22,−0.10) P < 0.001 | −0.34, −0.32 | 1.73 (1.24,2.87) | 16 | 1.32 |
| Hyperlipidemia/ Hypertension | 8 | P = 0.01 | –0.11 | −0.13 (−0.68,0.51) P = 0.715 | −0.16 (−0.25,−0.07) P < 0.001 | −0.26,−0.32 | 1.79 (1.28,2.51) | 16 | 1.34 |
| Other diseases | 17 | P < 0.01 | −0.16 | −0.17 (−0.57,0.29) P = 0.479 | −0.16 (−0.25,–0.06) P = 0.001 | −0.35,−0.32 | 1.80 (1.26,2.57) | 16 | 1.34 |
* Notes: There were no significant differences in the weighted mean correlation coefficient (r) among the three categories of diseases. Abbreviations: r is the correlation coefficient (not the z transformed r); 95%CI is the 95% confidence interval; N is the number of studies; Cohen d estimate is reported for the unweighted and weighted effect sizes, respectively
Figure 2.
Forest Plot of Z-transformed Correlations. ES = Effect Size (z-transformed correlation) with 95% confidence interval.
Risk of Bias across Studies
The fail safe n for the weighted mean effect size is 1,613, indicating that 1,613 unpublished or unfound studies with non-significant findings (i.e. P > 0.05) would be required to bring our effect to a non-significant level of P = 0.05. This is almost 10 times the tolerance level of 165 studies 27.
We performed meta-regressions to evaluate potential moderators of the association between depression and medication adherence. The type of medication adherence measure had a statistically significant effect on the mean effect size such that studies using pharmacy records for obtaining medication adherence had a significantly smaller effect size than those studies using self-report (respectively, r = −0.05, r = −0.21; P = 0.006). The mean effect size for studies using electronic monitoring devices was not significantly different from those using self-report (r = −0.14; P= 0.24).
A number of other factors were not statistically significant predictors of the effect size across the studies. Diseases were grouped into three categories to increase the power to observe differences among the disease types (see Table 2). Diabetes was included as a unique category, hypertension and hyperlipidemia were combined as a category because they were often studied together, and the remaining studies were combined as a reference or baseline category. No statistically significant differences were observed among the categories: diabetes (six studies; r = −0.17; P = 0.91), hyperlipidemia and hypertension (eight studies; r = −0.16; P = 0.98), and other diseases (17 studies; r = −0.16; reference). There were no statistically significant differences in effect sizes among the types of bivariate analyses used across the studies. Sample size was not a statistically significant predictor of effect size (P = 0.21). There was not a statistically significant difference whether a validated depression scale was used or not (r = −0.18 and −0.05 respectively; P = 0.08) or if depression was the primary focus of the study or not (r = −0.15 and r = −0.16, respectively; P = 0.77).
DISCUSSION
To our knowledge, this systematic review and meta-analysis is the first to focus specifically on the association between depression and medication adherence, analyze a sufficient number of studies to safely address the risk of publication bias, include studies of hypertension and hyperlipidemia, and investigate important potential moderators of the association. We found that depressed patients had 1.76 times the odds of being non-adherent compared to patients who were not depressed, across 31 studies and 18,245 participants.
These results were moderated by the method of adherence measurement. We found that using pharmacy records to assess medication adherence resulted in a significantly smaller correlation coefficient between depression and adherence compared to using self-report methods. The reason for this difference is not clear. Some have suggested that patients with depression may be more likely to self-report higher non-adherence than those without depression, in the setting of similar levels of actual medication-taking. 46,47 It is possible that pharmacy claims, which are objective measures of prescription filling, would not be subject to this reporting bias, although our analysis did not find any difference in the effect of depression between electronic monitoring studies and self-report. While pharmacy claims measure only the quantity of medications dispensed, it is also possible that self-reported adherence would capture other behaviors which may not be visible to claims and may be more susceptible to the effects of depression, such as incorrectly-timed doses or not ingesting filled medications. The variable concordance between the different measures of medication adherence, 28,48 and the heterogeneity of outcome measurement in these studies makes it difficult to draw firm conclusions; nonetheless, this finding suggests that future research in this area would benefit from including multiple methods of assessing adherence.
Other potential moderators did not reach statistical significance, including study size, depression assessment method, statistical methodology, or importantly, disease category (diabetes, hyperlipidemia/hypertension, and other). The consistent effect size across disease categories suggests that depression’s effects on adherence could be independent of each chronic disease’s treatment characteristics; while we are not able to draw definitive conclusions about how this finding might affect future research or interventions, lessons learned about the role of depression in adherence in diabetes, for example, could be applied to other chronic conditions.
The association between depression and medication adherence has important implications for clinical practice and quality of care for chronic diseases. Depression, as a diagnosis and as a set of symptoms, is extremely common in the US, with a 12-month national prevalence of approximately 6% and a lifetime prevalence of 13-16%. 49,50 Depression is common among those over age 65, who bear the burden of chronic diseases for which medication adherence is critical, 51 and there is evidence that depression is associated with adverse outcomes for several diseases, including coronary heart disease and diabetes. 52,53 Identifying depressed patients as being at high risk for medication non-adherence should be standard of care after decades of research. Alternatively, because the direction of the effect is not totally clear, medication non-adherence may be a marker for depression; suspected patient non-adherence would thus be an opportunity to screen for and discuss depression, which may be undiagnosed.
It is important to remember that depression is just one barrier known to affect medication adherence. Well-documented barriers include dose complexity and cost sharing. 54–56 Other barriers with research support include beliefs about medications, social support, side effects, and provider factors, among others. 57 Clinicians should be mindful of these barriers and be aware of recent reviews on interventions that may help improve adherence. 17,18,58,59 We are unable to comment on barriers to adherence for diseases excluded from this review such as HIV, although it should be noted that prior reviews have found depression to be a barrier to antiretroviral adherence 60,61.
There are several possible limitations in this study. First, meta-analysis results are correlational, providing limited opportunities to assess causality or identify confounders that could explain the apparent association between depression and poor adherence. A second limitation is the heterogeneity among the studies of assessment methodologies, participant characteristics, comparison groups, and statistical analyses methods. For example, patients with hypertension and hyperlipidemia constituted a large portion of the participants in the studies. Fortunately, however, our findings are supported by prior meta-analyses and our statistical methods partially account for the heterogeneity. A third limitation is the possibility of publication bias. In the current study, however, the number of unpublished studies with null effect would have to be quite large to change the outcome. The two largest included studies, in fact, found null effects, and yet the meta-analysis overall found a strong relationship between depression and adherence. Finally, it is possible that we missed some studies that have been published on medication adherence due to our selection of search terms.
CONCLUSIONS
This study confirms prior meta-analyses that show a statistically significant association between depression and medication adherence. More importantly, in two new findings, we show that depressed patients being treated for hypertension and/or hyperlipidemia are just as likely to be non-adherent as those being treated for diabetes or other chronic diseases, and that the observed relationship between depression and adherence may be different depending on the method of adherence measurement. Despite this new knowledge, the fundamental question remains whether treating depression can improve adherence. Several clinical trials are under way to address this important question. Regardless of the results of these trials, it is clear that clinicians should be asking about medication adherence in those with depression and should be asking about depression in those who are not adhering to their medications.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
This research was supported by the Agency for Healthcare Research and Quality (AHRQ: T32 HS00046-14), a VA HSR&D Career Development Award to Dr. Gellad (CDA 09-207), and by Mehlman Vogel Castagnetti.
Conflicts of Interest None disclosed.
References
- 1.DiMatteo MR. Variations in patients' adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 2.Adherence to long-term therapies: Evidence for action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 3.National Council on Patient Information and Education. Variations in patients' adherence to medical recommendations: A quantitative review of 50 years of research. Bethesda, MD; 2007. [DOI] [PubMed]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medial treatment outcomes: A meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Wu JR, Moser DK, Chung ML, Lennie TA. Objectively measured, but not self-reported, medication adherence independently predicts event-free survival in patients with heart failure. J Card Fail. 2008;14:203–10. doi: 10.1016/j.cardfail.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hiligsmann M, Rabenda V, Bruyere O, Reginster JY. The clinical and economic burden of non-adherence with oral bisphosphonates in osteoporotic patients. Health Policy. 2010;96:170–7. [DOI] [PubMed]
- 8.Hiligsmann M, Rabenda V, Gathon HJ, Ethgen O, Reginster JY. Potential clinical and economic impact of nonadherence with osteoporosis medications. Calcif Tissue Int. 2010;86:202–10. [DOI] [PubMed]
- 9.Davis KL, Edin HM, Allen JK. Prevalence and cost of medication nonadherence in Parkinson's disease: Evidence from administrative claims data. Mov Disord. 2010;25:474–80. [DOI] [PubMed]
- 10.Kane SV, Chao J, Mulani PM. Adherence to infliximab maintenance therapy and health care utilization and costs by Crohn's disease patients. Adv Ther. 2009;26:936–46. doi: 10.1007/s12325-009-0069-7. [DOI] [PubMed] [Google Scholar]
- 11.Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: A longitudinal analysis. Med Care. 2010;48:87–94. doi: 10.1097/MLR.0b013e3181c12e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinsky BW, Takemoto SK, Lentine KL, Burroughs TE, Schnitzler MA, Salvalaggio PR. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Am J Transplant. 2009;9:2597–606. doi: 10.1111/j.1600-6143.2009.02798.x. [DOI] [PubMed] [Google Scholar]
- 13.Breitscheidel L, Stamenitis S, Dippel FW, Schoffski O. Economic impact of compliance to treatment with antidiabetes medication in type 2 diabetes mellitus: A review paper. J Med Econ. 2010;13:8-15. [DOI] [PubMed]
- 14.McGinnis BD, Olson KL, Delate TM, Stolcpart RS. Statin adherence and mortality in patients enrolled in a secondary prevention program. Am J Manag Care. 2009;15:689–95. [PubMed] [Google Scholar]
- 15.Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–86. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 16.Ho PM, Magid DJ, Masoudi FA, McClure DL, Rumsfeld JS. Adherence to cardioprotective medications and mortality among patients with diabetes and ischemic heart disease. BMC Cardiovasc Disord. 2006;6:48. doi: 10.1186/1471-2261-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: A systematic review. Arch Intern Med. 2007;167:540–50. doi: 10.1001/archinte.167.6.540. [DOI] [PubMed] [Google Scholar]
- 18.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008 CD000011. [DOI] [PubMed]
- 19.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: A meta-analysis. Med Care. 2007;45:521–528. doi: 10.1097/MLR.0b013e318032937e. [DOI] [PubMed] [Google Scholar]
- 20.DiMatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Counsel Special Issue: Educating and Counseling Children about Physical Health. 2004;55:339–344. doi: 10.1016/j.pec.2003.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: A meta-analysis. Med Care. 2009;47:826–34. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gatti ME, Jacobson KL, Gazmararian JA, Schmotzer B, Kripalani S. Relationships between beliefs about medications and adherence. Am J Health Syst Pharm. 2009;66:657–64. doi: 10.2146/ajhp080064. [DOI] [PubMed] [Google Scholar]
- 23.Manning WG, Jr, Wells KB. The effects of psychological distress and psychological well-being on use of medical services. Med Care. 1992;30:541–53. doi: 10.1097/00005650-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Piette JD, Richardson C, Valenstein M. Addressing the needs of patients with multiple chronic illnesses: The case of diabetes and depression. Am J Manag Care. 2004;10:152–62. [PubMed] [Google Scholar]
- 25.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care. 2008;31:2398–403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenthal R. Meta-analytic procedures for social research. Applied social research methods series. London: Sage; 1984.
- 28.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: A summary of the literature. Med Care. 2004;42:649–52. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- 29.Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–74. doi: 10.1002/pds.1230. [DOI] [PubMed] [Google Scholar]
- 30.McHorney CA. The adherence estimator: A brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin. 2009;25:215–38. doi: 10.1185/03007990802619425. [DOI] [PubMed] [Google Scholar]
- 31.Janson SL, Earnest G, Wong KP, Blanc PD. Predictors of asthma medication nonadherence. Heart Lung. 2008;37:211–8. doi: 10.1016/j.hrtlng.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20:764–71. doi: 10.1016/S0149-2918(98)80139-2. [DOI] [PubMed] [Google Scholar]
- 33.Senior V, Marteau TM, Weinman J. Genetic Risk Assessment for FHTSG. Self-reported adherence to cholesterol-lowering medication in patients with familial hypercholesterolaemia: The role of illness perceptions. Cardiovasc Drugs Ther. 2004;18:475–81. doi: 10.1007/s10557-004-6225-z. [DOI] [PubMed] [Google Scholar]
- 34.Kleinman A. Culture and depression. N Engl J Med. 2004;351:951–3. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- 35.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 36.Mannheimer S, Friedland G, Matts J, Child C, Chesney M. The consistency of adherence to antiretroviral therapy predicts biologic outcomes for human immunodeficiency virus-infected persons in clinical trials. Clin Infect Dis. 2002;34:1115–21. doi: 10.1086/339074. [DOI] [PubMed] [Google Scholar]
- 37.Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego: Academic Press; 1985. pp. xxii–369. [Google Scholar]
- 38.Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. J Appl Psychol. 2005;90:175–181. doi: 10.1037/0021-9010.90.1.175. [DOI] [PubMed] [Google Scholar]
- 39.Friedman DS, Okeke CO, Jampel HD, et al. Risk factors for poor adherence to eyedrops in electronically monitored patients with glaucoma. Ophthalmology. 2009; 116:1097-105. [DOI] [PubMed]
- 40.Ross SM. Simulation. 4. Amsterdam: Elsevier Academic Press; 2006. pp. xiii–298 s. [Google Scholar]
- 41.Pearson K. Mathematical contributions to the theory of evolution. Vii, viii. Proceedings of the Royal Society. 1900; LXVI:140-164, 241-244.
- 42.Rosenthal R, Rosnow RL, Rubin DB. Contrasts and effect sizes in behavioral research: A correlational approach. New York: Cambridge University Press; 2000. [Google Scholar]
- 43.Berkey CS, Hoaglin DC, Mosteller F, Colditz GA. A random-effects regression model for meta-analysis. Stat Med. 1995;14:395–411. doi: 10.1002/sim.4780140406. [DOI] [PubMed] [Google Scholar]
- 44.Release 10. College Station: StataCorp LP; 2007. Stata statistical software. [Google Scholar]
- 45.Mosley-Williams A, Lumley MA, Gillis M, Leisen J, Guice D. Barriers to treatment adherence among African American and white women with systemic lupus erythematosus. Arthritis Rheum. 2002;47:630–8. doi: 10.1002/art.10790. [DOI] [PubMed] [Google Scholar]
- 46.Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med. 2006;21:1178–1183. doi: 10.1111/j.1525-1497.2006.00586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morgado A, Smith M, Lecrubier Y, Widlocher D. Depressed subjects unwittingly overreport poor social adjustment which they reappraise when recovered. J Nerv Ment Dis. 1991;179:614–9. doi: 10.1097/00005053-199110000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Steiner JF, Gardner EM. Assessing medication adherence from pharmacy records. Pharmacoepidemiology and Drug Safety. 2006;15:575–577. doi: 10.1002/pds.1259. [DOI] [Google Scholar]
- 49.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (ncs-r) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 50.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the national epidemiologic survey on alcoholism and related conditions. Arch Gen Psychiatr. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 51.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 52.Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 53.Hoen PW, Whooley MA, Martens EJ, Na B, Melle JP, Jonge P. Differential associations between specific depressive symptoms and cardiovascular prognosis in patients with stable coronary heart disease. J Am Coll Cardiol. 2010;56:838–44. doi: 10.1016/j.jacc.2010.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15:e22–33. [PubMed] [Google Scholar]
- 55.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. doi: 10.1016/S0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 56.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: Associations with medication and medical utilization and spending and health. JAMA. 2007;298:61–9. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gellad WF, Grenard JL, McGlynn EA. A framework for driving policy options. Santa Monica, CA: RAND Corp; 2009. A review of barriers to medication adherence. [Google Scholar]
- 58.Chapman RH, Ferrufino CP, Kowal SL, Classi P, Roberts CS. The cost and effectiveness of adherence-improving interventions for antihypertensive and lipid-lowering drugs*. Int J Clin Pract. 2010;64:169–81. doi: 10.1111/j.1742-1241.2009.02196.x. [DOI] [PubMed] [Google Scholar]
- 59.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: Scientific review. JAMA. 2002;288:2868–79. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- 60.Fogarty L, Roter D, Larson S, Burke J, Gillespie J, Levy R. Patient adherence to HIV medication regimens: A review of published and abstract reports. Patient Educ Couns. 2002;46:93–108. doi: 10.1016/S0738-3991(01)00219-1. [DOI] [PubMed] [Google Scholar]
- 61.Malta M, Magnanini MM, Strathdee SA, Bastos FI. Adherence to antiretroviral therapy among HIV-infected drug users: A meta-analysis. AIDS Behav. 2010;14:731–47. doi: 10.1007/s10461-008-9489-7. [DOI] [PubMed] [Google Scholar]
- 62.Cruess DG, Localio AR, Platt AB, et al. Patient attitudinal and behavioral factors associated with warfarin non-adherence at outpatient anticoagulation clinics. Int J Behav Med. 2010; 17:33–42. [DOI] [PMC free article] [PubMed]
- 63.Apter AJ, Boston RC, George M, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: It's not just black and white. J Allergy Clin Immunol. 2003;111:1219–26. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- 64.Smith A, Krishnan JA, Bilderback A, Riekert KA, Rand CS, Bartlett SJ. Depressive symptoms and adherence to asthma therapy after hospital discharge. Chest. 2006;130:1034–8. doi: 10.1378/chest.130.4.1034. [DOI] [PubMed] [Google Scholar]
- 65.Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: Findings from the heart and soul study. Arch Intern Med. 2005;165:2508–13. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carney RM, Freedland KE, Eisen SA, Rich MW, Skala JA, Jaffe AS. Adherence to a prophylactic medication regimen in patients with symptomatic versus asymptomatic ischemic heart disease. Behav Med. 1998;24:35–9. doi: 10.1080/08964289809596379. [DOI] [PubMed] [Google Scholar]
- 67.Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–23. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
- 68.Mann DM, Ponieman D, Leventhal H, Halm EA. Predictors of adherence to diabetes medications: The role of disease and medication beliefs. J Behav Med. 2009;32:278–84. [DOI] [PubMed]
- 69.Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with type 2 diabetes. Diabet Med. 2008;25:1102–7. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chao J, Nau DP, Aikens JE, Taylor SD. The mediating role of health beliefs in the relationship between depressive symptoms and medication adherence in persons with diabetes. Res Social Adm Pharm. 2005;1:508–25. doi: 10.1016/j.sapharm.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 71.Hill-Briggs F, Gary TL, Bone LR, Hill MN, Levine DM, Brancati FL. Medication adherence and diabetes control in urban african americans with type 2 diabetes. Health Psychol. 2005;24:349–57. doi: 10.1037/0278-6133.24.4.349. [DOI] [PubMed] [Google Scholar]
- 72.Kalsekar ID, Madhavan SS, Amonkar MM, et al. Depression in patients with type 2 diabetes: Impact on adherence to oral hypoglycemic agents. Ann Pharmacother. 2006;40:605–11. doi: 10.1345/aph.1G606. [DOI] [PubMed] [Google Scholar]
- 73.Kilbourne AM, Reynolds CF, 3rd, Good CB, Sereika SM, Justice AC, Fine MJ. How does depression influence diabetes medication adherence in older patients? Am J Geriatr Psychiatry. 2005;13:202–10. doi: 10.1176/appi.ajgp.13.3.202. [DOI] [PubMed] [Google Scholar]
- 74.Wu JR, Moser DK, Chung ML, Lennie TA. Predictors of medication adherence using a multidimensional adherence model in patients with heart failure. J Card Fail. 2008;14:603–14. doi: 10.1016/j.cardfail.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cukor D, Rosenthal DS, Jindal RM, Brown CD, Kimmel PL. Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients. Kidney Int. 2009; 75:1223–9. [DOI] [PubMed]
- 76.Schoenthaler A, Chaplin WF, Allegrante JP, et al. Provider communication effects medication adherence in hypertensive african americans. Patient Educ Couns. 2009;75:185–91. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schoenthaler A, Ogedegbe G, Allegrante JP. Self-efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive african americans. Health Educ Behav. 2009;36:127–37. doi: 10.1177/1090198107309459. [DOI] [PubMed] [Google Scholar]
- 78.Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165:1147–52. doi: 10.1001/archinte.165.10.1147. [DOI] [PubMed] [Google Scholar]
- 79.Kim EY, Han HR, Jeong S, et al. Does knowledge matter?: Intentional medication nonadherence among middle-aged korean americans with high blood pressure. J Cardiovasc Nurs. 2007;22:397–404. doi: 10.1097/01.JCN.0000287038.23186.bd. [DOI] [PubMed] [Google Scholar]
- 80.Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–92. doi: 10.1592/phco.26.4.483. [DOI] [PubMed] [Google Scholar]
- 81.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: The impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–11. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Stilley CS, Sereika S, Muldoon MF, Ryan CM, Dunbar-Jacob J. Psychological and cognitive function: Predictors of adherence with cholesterol lowering treatment. Ann Behav Med. 2004;27:117–24. doi: 10.1207/s15324796abm2702_6. [DOI] [PubMed] [Google Scholar]
- 83.Insel K, Morrow D, Brewer B, Figueredo A. Executive function, working memory, and medication adherence among older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61:P102–P107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- 84.Houtven CH, Voils CI, Oddone EZ, et al. Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J Gen Intern Med. 2005;20:578–583. doi: 10.1007/s11606-005-0104-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Davis DP, Jandrisevits MD, Iles S, Weber TR, Gallo LC. Demographic, socioeconomic, and psychological factors related to medication non-adherence among emergency department patients. J Emerg Med. Epub 2009 May 21. [DOI] [PubMed]
- 86.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: A focus on health literacy. J Gen Intern Med. 2006;21:1215–21. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.