ABSTRACT
BACKGROUND
The use of online social networks (OSNs) among physicians and physicians-in-training, the extent of patient–doctor interactions within OSNs, and attitudes among these groups toward use of OSNs is not well described.
OBJECTIVE
To quantify the use of OSNs, patient interactions within OSNs, and attitudes toward OSNs among medical students (MS), resident physicians (RP), and practicing physicians (PP) in the United States.
DESIGN/SETTING
A random, stratified mail survey was sent to 1004 MS, 1004 RP, and 1004 PP between February and May 2010.
MEASUREMENTS
Percentage of respondents reporting OSN use, the nature and frequency of use; percentage of respondents reporting friend requests by patients or patients’ family members, frequency of these requests, and whether or not they were accepted; attitudes toward physician use of OSNs and online patient interactions.
RESULTS
The overall response rate was 16.0% (19.8% MS, 14.3% RP, 14.1% PP). 93.5% of MS, 79.4% of RP, and 41.6% of PP reported usage of OSNs. PP were more likely to report having visited the profile of a patient or patient’s family member (MS 2.3%, RP 3.9%, PP 15.5%), and were more likely to have received friend requests from patients or their family members (MS 1.2%, RP 7.8%, PP 34.5%). A majority did not think it ethically acceptable to interact with patients within OSNs for either social (68.3%) or patient-care (68.0%) reasons. Almost half of respondents (48.7%) were pessimistic about the potential for OSNs to improve patient–doctor communication, and a majority (79%) expressed concerns about maintaining patient confidentiality.
CONCLUSION
Personal OSN use among physicians and physicians-in-training mirrors that of the general population. Patient–doctor interactions take place within OSNs, and are more typically initiated by patients than by physicians or physicians-in-training. A majority of respondents view these online interactions as ethically problematic.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1761-2) contains supplementary material, which is available to authorized users.
KEY WORDS: doctor–patient relations, computer communication networks, professionalism, Internet, bioethics
INTRODUCTION
Online social networks (OSNs) are “spaces in the internet where users can create a profile and connect that profile to others (individuals or entities) to create a personal network.”1 There are multiple online social networks, but some of the most popular include Facebook, Twitter, MySpace, Friendster, and LinkedIn. Over the past several years, the rise in popularity of these networks has been dramatic. Facebook, the most popular online social network, boasts over 500 million users since its inception in 2004,2 and it recently surpassed Google as the most popular site on the internet.3 Among internet users aged 18–24, 75% of those online had profiles on OSNs as of 2008.1 The Pew Internet and American Life Project found that the use of social network sites among those age 18 or greater has increased from 8% of internet users in 2005 to 46% in 2009.4
OSNs are a new potential medium for interactions between physicians and patients that may present both opportunities and problems for patient–doctor communication.5 OSNs provide a forum within which a new form of purported professional indiscretions may take place, and a recent report suggested that OSNs have been a forum for lapses of professionalism among medical students.6 Among United States medical schools, 60% reported incidents of students posting unprofessional content online, and 38% of schools had developed disciplinary policies for handling inappropriate online content posted by students. Additionally, several recent reports have described patient–doctor interactions within OSNs.7–9 The ambiguous status of OSNs as they relate to medical interactions and the potential they present for altering fundamental aspects of the patient–doctor relationship have also prompted the formulation of proposed guidelines for physicians using OSNs.10,11
Currently, there are no studies that quantify the incidence of patient–doctor interactions within OSNs by practicing physicians and medical trainees. The goals of this study were to quantify the utilization patterns of OSNs by physicians, resident physicians, and medical students; to describe the frequency of patient–doctor interactions within these networks; and to evaluate attitudes toward such interactions among physicians and physicians-in-training.
METHODS
Study Sample
We conducted a random, stratified mail survey of a cohort of practicing physicians (PP), resident physicians (RP), and medical students (MS) in the United States. The source population list was obtained from a licensee of the American Medical Association (AMA) Masterfile (Direct Medical Data, Des Plaines, IL). The AMA Masterfile is recognized as one of the most complete source lists of licensed physicians and medical students in the United States. We utilized the mail survey format because the list of mailing addresses for potential participants is the most accurate and complete contact data contained in the AMA Masterfile. Additionally, we wanted to capture the attitudes of both users and nonusers of online technologies. Because the utilization rates of OSNs and patient interaction data for these populations has not been previously studied, there were no existing data with which to perform power calculations. Based upon previously published data regarding physician response rates to surveys,12 the expected response rate was 25%. It was felt that this would provide sufficient data for reasonable estimates of proportions, based on the survey responses. This study was approved by the joint Indiana University–Purdue University Indianapolis/Clarian Health System institutional review board.
Survey
The survey was designed by the study team based on the existing literature13 and guided by research questions. The survey instrument was then piloted among ten resident and practicing physicians, and underwent iterative revision by members of the study team.
The survey instrument examined four content areas: attitudes toward online social networks, personal utilization patterns of online social networks, patient interaction experiences within online social networks, and demographic data (the full survey is available as an appendix online). Most response options were categorical. Questions regarding physician attitudes toward OSNs and their role in the patient–doctor relationship utilized a 5-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree).
Demographic data collected included age, year of medical school graduation (or anticipated medical school graduation), medical specialty, self-reported practice type (academic, private practice, mixed), self-reported practice setting (urban, rural, suburban), and gender.
Utilization data included whether or not the respondent used or had ever used OSNs, the frequency of use, which OSNs were used, type of use (personal vs. professional), and privacy settings of respondents’ own personal OSN profile.
The survey was designed to assess experiences of online patient interactions. It included questions regarding whether or not participants had visited the personal OSN profile of a patient and the reason for any visits, and whether they had been aware of patients viewing their personal profile. Additionally, respondents were asked whether they had ever asked for or received friend requests from patients or a patient’s family member within OSNs, how frequently, and whether or not these requests were accepted.
Additional questions were designed to assess attitudes toward OSN use and patient interactions. Participants were asked to describe the extent of their agreement with statements describing attitudes toward the ethical acceptability of visiting patient profiles, interacting with patients as part of patient care, and interacting with patients for social reasons. These questions also assessed respondents’ views of the potential of OSNs to improve patient–doctor communication, and the perceived likelihood that OSNs could be utilized without compromising patient confidentiality.
Data Collection
The survey questionnaire was sent to study subjects along with an addressed, stamped envelope in three sequential mailings. Surveys were completed anonymously, but were coded in order to track responses. Data collection took place from February through May of 2010. No incentives were offered for survey completion.
Statistical Methods
All demographic variables and questionnaire responses were summarized by professional status (medical student, resident physician, or practicing physician) using descriptive statistics (mean and standard deviation for continuous measures; count and percent for categorical measures). Comparisons across groups were performed using analysis of variance (ANOVA) and Fisher’s exact tests. Pairwise comparisons between groups were also performed using Fisher’s exact tests, using the Bonferroni correction to adjust significance levels for multiple post hoc comparisons. For these comparisons, p values < 0.017 were considered significant. For the summary of age for both OSN users and non-users the mean and corresponding 95% confidence interval was calculated.
RESULTS
Respondent Characteristics
Surveys were sent to 1004 subjects within each of the three subgroups, for a total of 3012 subjects queried. Surveys returned as undeliverable were excluded from the analysis (59/1004 for MS, 87/1004 for RP, 30/1004 for PP). There were a total of 455 survey responses out of 2836 delivered surveys (16.0% response rate), with response rates for each subgroup as follows: 187/945 (19.8%) for MS, 131/917 (14.3%) for RP, and 137/974 (14.1%) for PP. Respondents’ demographic data are reported in Table 1.
Table 1.
Respondent Characteristics
| Medical students (%) | Resident physicians (%) | Practicing Physicians (%) | All respondents (%) | |
|---|---|---|---|---|
| Number of respondents (response rate) | 187 (19.8) | 131 (14.3) | 137 (14.1) | 455 (16.0) |
| Primary practice type | N/A | |||
| Academic | 103 (81.8) | 16 (11.8) | 119 (44.4) | |
| Private practice | 4 (3.2) | 90 (66.2) | 94 (35.1) | |
| Mix private practice/academic | 13 (10.3) | 17 (12.5) | 30 (11.2) | |
| Other | 6 (4.8) | 13 (9.6) | 19 (7.0) | |
| Primary Practice Setting | N/A | |||
| Urban | 91 (71.7) | 48 (35.8) | 139 (51.9) | |
| Suburban | 31 (24.4) | 58 (43.3) | 89 (33.2) | |
| Rural | 5 (3.9) | 28 (20.9) | 33 (12.3) | |
| Average Years in practice | N/A | 2.6 | 22.8 | 13.0 |
| Gender | ||||
| Female | 99 (53.8) | 65 (50.4) | 56 (41.2) | 220 (48.4) |
| Male | 85 (46.2) | 64 (49.6) | 80 (58.8) | 229 (50.3) |
| Average age (SD) | 25.5 (2.7) | 30.2 (3.4) | 50.3 (12.7) | 34.1 (12.9) |
Usage Patterns
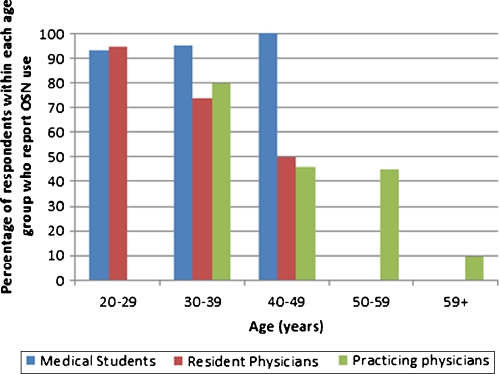
The utilization patterns of OSNs for each group of respondents are reported in Table 2. Medical students were more likely to report usage of OSNs than resident or practicing physicians (MS 93.5%, RP 79.4%, PP 41.6%; p <0.001 for all pairwise comparisons). Among all OSN users in this survey, Facebook was the most popular site (used by 99.4% of MS users, 96.2% of RP users, and 96.5% of PP users). Forty-six percent of MS, 50.0% of RP, and 50.9% of PP used more than one OSN. Medical students were more likely than practicing physicians to be daily users of OSNs (MS 46.6%, RP 38.8%, PP 24.6%; p = 0.003 for MS vs. PP). A majority of all three groups reported using OSNs for personal use only (MS 95.9%, RP 97.0%, PP 95.0%), and very few respondents used OSNs for professional purposes (MS 4.1%, RP 3.0%, PP 10.1%). Most respondents reported that their personal OSN privacy status was completely private (MS 63.2%, RP 68.4%, PP 48.1%). Less than half of respondents reported that their personal OSN profile contained only information they would be willing to share with patients (MS 42.4%, RP 41.4%, PP 49.1%). The plot of OSN usage by age, (Figure 1), shows OSN usage decreasing with increasing age in two of the three groups (RP and PP).
Table 2.
Usage Patterns of Online Social Networks
| Medical students (%) | Resident physicians (%) | Practicing physicians (%) | All respondents (%) | |
|---|---|---|---|---|
| Has respondent ever used social networking sites? | n = 186 | n = 131 | n = 137 | n = 454 |
| Yes | 174 (93.5) | 104 (79.4) | 57 (41.6) | 335 (73.8) |
| No | 12 (6.5) | 27 (20.6) | 80 (58.4) | 119 (26.2) |
| If respondent is a user, which OSNs do they use? | n = 174 | n = 104 | n = 57 | n = 335 |
| 173 (99.4) | 100 (96.2) | 55 (96.5) | 328 (97.9) | |
| 27 (15.5) | 10 (9.6) | 8 (14.0) | 45 (13.4) | |
| MySpace | 52 (29.9) | 31 (29.8) | 6 (10.5) | 89 (26.6) |
| Friendster | 13 (7.5) | 15 (14.4) | 1 (1.8) | 29 (8.7) |
| 20 (11.5) | 20 (19.2) | 20 (35.1) | 60 (17.9) | |
| Other | 5 (2.9) | 4 (3.8) | 3 (5.3) | 12 (3.6) |
| If respondent is a user, how often does respondent use OSNs? | n = 174 | n = 103 | n = 57 | n = 334 |
| Daily | 81 (46.6) | 40 (38.8) | 14 (24.6) | 135 (40.4) |
| Weekly | 70 (40.2) | 40 (38.8) | 21 (36.8) | 131 (39.2) |
| Type of utilization | n = 172 | n = 99 | n = 54 | n = 325 |
| Personal use | 165 (95.9) | 96 (97.0) | 48 (88.9) | 309 (95.1) |
| Personal and professional use | 7 (4.1) | 3 (3.0) | 4 (7.4) | 14 (4.3) |
| Professional use | 0 (0.0) | 0 (0.0) | 2 (3.7) | 2 (0.6) |
| Privacy status of personal OSN | n = 171 | n = 98 | n = 52 | n = 321 |
| Completely public | 1 (0.6) | 2 (2.0) | 2 (3.9) | 5 (1.6) |
| Limited public access | 58 (33.9) | 26 (26.5) | 23 (44.2) | 107 (33.3) |
| Completely private | 108 (63.2) | 67 (68.4) | 25 (48.1) | 200 (62.3) |
| Don’t know | 2 (1.2) | 3 (3.1) | 0 (0.0) | 5 (1.6) |
| Other | 2 (1.2) | 0 (0.0) | 2 (3.9) | 4 (1.2) |
| I consider my social networking profile to be located in a public and openly viewable space. | n = 172 | n = 99 | n = 54 | n = 325 |
| Strongly agree/agree | 78 (45.3) | 37 (37.4) | 30 (55.6) | 145 (44.6) |
| Neutral | 11 (6.4) | 4 (4.0) | 4 (7.4) | 19 (5.8) |
| Strongly disagree/disagree | 82 (47.7) | 56 (56.6) | 20 (37.0) | 158 (48.6) |
| My online social networking profile contains only information that I would be willing to share with patients. | n = 172 | n = 99 | n = 53 | n = 324 |
| Strongly agree/agree | 73 (42.4) | 41 (41.4) | 26 (49.1) | 140 (43.2) |
| Neutral | 17 (9.9) | 3 (3.0) | 7 (13.2) | 27 (8.3) |
| Strongly disagree/disagree | 80 (46.5) | 55 (55.6) | 20 (37.7) | 155 (47.8) |
Figure 1.
Stratified OSN users by age.
Patient–doctor Interactions within Online Social Networks
Practicing physicians were more likely to report having patient interactions within OSNs than either medical students or resident physicians (Table 3). Specifically, they were more likely to have visited the profile of a patient or patient’s family member within an OSN than either MS or RP (MS 2.3%, RP 3.9%, PP 15. 5%; p < 0.001 for MS vs. PP, p = 0.014 for RP vs. PP). A larger proportion of PP reported being aware of a patient or patient’s family member visiting their own personal OSN profile (MS 1.2%, RP 8.3%, PP 28.1%; p = 0.006 for MS vs. RP, p < 0.001 for MS vs. PP, p = 0.002 for RP vs. PP).
Table 3.
Physician-patient Interactions within Online Social Networks
| Medical students (%) | Resident physicians (%) | Practicing physicians (%) | All respondents (%) | |
|---|---|---|---|---|
| Ever visited the profile of a patient or family member? | n = 174 | n = 103 | n = 58 | n = 335 |
| Yes | 4 (2.3) | 4 (3.9) | 9 (15.5) | 17 (5.1) |
| No | 170 (97.7) | 99 (96.1) | 49 (84.5) | 318 (94.9) |
| Ever been aware of a patient or family member visiting your personal site? | n = 168 | n = 97 | n = 57 | n = 322 |
| Yes | 2 (1.2) | 8 (8.2) | 16 (28.1) | 26 (8.1) |
| No | 166 (98.8) | 89 (91.8) | 41 (71.9) | 296 (91.9) |
| Ever received a “friend” request from a patient or patient’s family member? | n = 173 | n = 103 | n = 58 | n = 334 |
| Yes | 2 (1.2) | 8 (7.8) | 20 (34.5) | 30 (9.0) |
| No | 171 (98.8) | 95 (92.2) | 38 (65.5) | 304 (91.0) |
| Ever requested to be a “friend” with a patient or a patient’s family member? | n = 172 | n = 102 | n = 57 | n = 331 |
| Yes | 0 (0) | 1 (1.0) | 3 (5.3) | 4 (1.2) |
| No | 172 (100) | 101 (99) | 54 (94.7) | 327 (98.8) |
Significantly more practicing physicians reported receiving friend requests from patients or family members then either resident physicians or medical students (MS 1.2%, RP 7.8%, PP 34.5%; p = 0.007 for MS vs. RP, p < 0.001 for MS vs. PP and RP vs. PP). Of those who had received friend requests, 58% of practicing physicians reported that they always replied “no” to the request, and 42% replied that they accepted them on a case-by-case basis. For those resident physicians who had received friend requests, 57% reported that they never accepted friend requests from patients or their families, and 43% reported that they accepted them on a case-by-case basis. Among medical students who reported having received friend requests from patients or family members of patients, all reported accepting them on a case-by-case basis. No respondents from any group reported that they always accepted friend requests. Very few respondents reported ever requesting friendship of a patient or patient’s family member (MS 0%, RP 1.0%, PP 5.3%; p = 0.015 for MS vs. PP). Overall, patients were more likely to request friendship with physicians within OSNs than vice versa (patient-initiated request 9.0%, physician-initiated request 1.2%; p < 0.001).
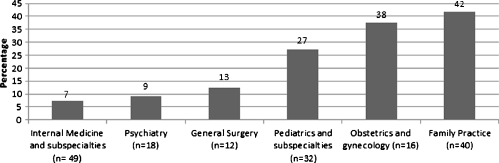
Data for patient-initiated friend requests categorized by specialty is reported in Figure 2. Forty two percent of family practitioners who use OSNs, 38% of obstetricians who use OSNs, and 27% of pediatricians who use OSNs had received friend requests from either a patient or a patient’s family member.
Figure 2.
Percentage of users who had received friend requests by specialty.*The following specialties had no users receive patient or family friend requests: anesthesiology, emergency medicine, surgical subspecialties, radiology, dermatology, pathology.
Attitudes Toward OSNs
All survey respondents, whether or not they reported using OSNs, were asked questions about their attitudes toward physician use of OSNs (Table 4). There were no statistically significant differences among the three groups for any of the responses. More than half of the respondents (57.9%) found it ethically unacceptable to visit the profiles of patients on OSNs. Additionally, a majority did not agree that it was ethically acceptable to interact with patients on OSNs, either for social (68.3%) or patient-care (68.0%) reasons. Almost half of respondents (48.7%) reported that they did not think OSNs had potential for improving patient–doctor communication; 26.4% of respondents agreed that OSNs did have potential to improve patient–doctor communication; and 20.5% of respondents were neutral on this question. A majority of respondents (79.0%) did not think that communication with patients within OSNs could be safely accomplished without compromising patient confidentiality.
Table 4.
Attitudes Toward Online Social Networks
| Medical Students (%) | Resident Physicians (%) | Practicing Physicians (%) | All respondents (%) | |
|---|---|---|---|---|
| It is ethically acceptable for physicians to visit the online profiles of patients within personal online social networking sites. | n = 186 | n = 131 | n = 137 | N = 454 |
| Strongly agree/agree | 44 (23.7) | 25 (19.1) | 30 (21.9) | 99 (21.8) |
| Neutral | 35 (18.8) | 18 (13.7) | 26 (19.0) | 79 (17.4) |
| Strongly disagree/disagree | 103 (55.4) | 86 (65.6) | 74 (54.0) | 263 (57.9) |
| It is ethically acceptable for physicians to interact (e.g. exchange personal tmessages) with patients within personal online social networking sites for social reasons. | n = 186 | n = 131 | n = 137 | N = 454 |
| Strongly agree/agree | 36 (19.4) | 16 (12.2) | 21 (15.3) | 73 (16.1) |
| Neutral | 31 (16.7) | 16 (12.2) | 15 (11.0) | 62 (13.7) |
| Strongly disagree/disagree | 117 (62.9) | 97 (74.0) | 96 (70.1) | 310 (68.3) |
| It is ethically acceptable for physicians to interact with patients within online social networking sites as part of patient care. | n = 186 | n = 131 | n = 136 | N = 453 |
| Strongly agree/agree | 37 (19.9) | 29 (22.1) | 22 (16.2) | 88 (19.4) |
| Neutral | 22 (11.8) | 17 (13.0) | 6 (4.4) | 45 (9.9) |
| Strongly disagree/disagree | 121 (65.0) | 85 (64.9) | 102 (74.5) | 308 (68.0) |
| Online social networking sites have potential for improving doctor-patient communication. | n = 186 | n = 131 | n = 137 | N = 454 |
| Strongly agree/agree | 52 (28.0) | 39 (29.8) | 29 (21.2) | 120 (26.4) |
| Neutral | 40 (21.5) | 31 (23.7) | 22 (16.1) | 93 (20.5) |
| Strongly disagree/disagree | 85 (45.7) | 59 (45.0) | 77 (56.2) | 221 (48.7) |
| Communication with patients within online social networking sites can be safely accomplished without compromising patient confidentiality. | n = 186 | n = 131 | n = 136 | N = 453 |
| Strongly agree/agree | 24 (12.9) | 18 (13.7) | 8 (5.9) | 50 (11.0) |
| Neutral | 20 (10.8) | 13 (9.9) | 13 (9.6) | 46 (10.2) |
| Strongly disagree/disagree | 127 (68.3) | 94 (74.0) | 100 (73.0) | 321 (70.9) |
DISCUSSION
The meteoric increase in the use of online social networks has led to a great deal of media and other coverage of the ways in which such online tools are changing human interaction, and several have focused on patient–doctor interactions.14–16 These anecdotal reports tend to speculate as to the frequency with which these exchanges are taking place and the positive and negative consequences of such interactions. Several published case reports have described patient–doctor interactions within OSNs in the medical literature.7–9,17 To our knowledge, this is the first attempt to quantify on a national level physician and medical student use of OSNs and patient interactions therein. Although the sample size was low and limits the generalizability of findings, it provides novel information about the use of OSNs by medical professionals.
Our findings demonstrate that physicians and physicians-in-training use OSNs as much or more often than the general population. Additionally, medical students and resident physicians are more likely to use OSNs than practicing physicians, although this may simply be artifact of the lower age among students and resident physicians. The frequency of patient–doctor interactions among practicing physicians is noteworthy. And finally, most physicians and physicians-in-training think it ethically unacceptable to interact with patients on OSNs, and are doubtful that such interactions could occur without compromising patient confidentiality.
Several recent studies have attempted to quantify medical student and resident use of OSNs. Thompson et al. describe that 44.5% of medical students and resident physicians at a single public medical school and its affiliated hospital use OSNs.13 MacDonald et al. reported that 65% of recent medical school graduates in New Zealand reported using Facebook.18 Most recently, Moubarak et al. reported that 73% of residents and fellows utilize Facebook.9 Findings from the present study suggest that a significantly higher proportion of U.S. medical students (94%) report using OSNs for personal use than is suggested by these prior studies, although the percentage of resident users of OSNs (79.4%) is comparable to the Moubarak data.9 There are at least three possible explanations for the higher rates of use reported in this study. First, as noted above, the low response rate of our study leaves a potential for selection bias which may have skewed the responses in favor of users. However, both of the comparative studies were carried out in 2008, and usage of OSNs was likely less common at that time. Data from the Pew Internet & American Life Project demonstrate that usage of OSNs grew from 61% of aged 18–29 internet users in 2008 to 83% of internet users in January, 2010.4,19 Additionally, both of these studies estimated usage rates by cross-referencing class lists with Facebook pages, leaving the possibility that usage rates were underestimated.
The difference among the specialties with regards to the percentage of users who had received friend requests is interesting. Those specialties that are seen as having a more longitudinal interaction with patients, often revolving around the care of children (FP, OB/GYN, and pediatrics), were those with the most friend requests. While the low response rate precluded a comparison between the different specialties regarding their attitudes toward these interactions, this finding generates questions regarding whether or not there are differences in each of these specialties’ attitudes toward patient interactions within OSNs.
Several commentators have written from a theoretical perspective about the effects of the Internet and Web 2.0 technologies on the medical profession. For the most part, these have focused on the preponderance of easily searchable data on the Internet,20 professionalism,21 and the posting of potentially inappropriate material on various types of Web 2.0 formats, including YouTube,22 weblogs,23 and Twitter.24 The structure of OSNs are such that they can dramatically blur the line between public and private spaces.25 The relatively permanent nature of postings on such sites means that the control over information dissemination, once posted, differs significantly from a fleeting and local interaction within the hospital or outpatient office. Our study raises further questions about the nature of patient–doctor boundaries in the digital age. Physical disconnection may allow patients to pursue virtual dual relationships with their physicians more readily than they would pursue real ones. The fact that 34% of practicing physicians in our sample report having received friend requests from patients supports the idea that many patients feel comfortable approaching with their physicians within OSNs.
Even among this self-selected sample of physician users of OSN’s, our data suggest that most physicians do not feel comfortable interacting with patients within OSNs. While over one-third of practicing physicians had received a friend request from a patient, only 1.2% of respondents had initiated a friend request. Additionally, a substantial majority of physicians see patient interactions within OSNs, for any reason, as ethically unacceptable. Respondents also tended to be negative regarding the potential for OSNs to improve patient–doctor communication, and a great majority thought that interactions with patients in these venues posed significant risks to patient confidentiality.
Although a majority of respondents did not view patient–doctor interactions within OSNs as ethically acceptable, just over a third of respondents were either neutral or thought these interactions were ethically appropriate, and almost half (46.9%) were either neutral or thought that OSNs had potential for improving patient–doctor communication. This range of attitudes toward acceptability of these interactions highlights a lack of consensus regarding the normative stance that physicians and physicians-in-training hold toward such contact.
Since this survey was completed, the AMA has issued a policy statement entitled, “Professionalism in the use of social media.”11 This statement gives guidance regarding physician privacy, maintaining appropriate boundaries with patients within OSNs, the potential for real-life consequences regarding online professional lapses, and the responsibility to report unprofessional online actions of fellow physicians. Our study underscores the importance of these guidelines and demonstrates the need to separate personal use of OSNs from professional obligations and fiduciary duties. Given the frequency with which practicing physicians experience patient interactions within OSNs and the fact that there are a plurality of views regarding the ethical standing of such exchanges, there are three tangible recommendations for clinicians from our study. First, clinicians who utilize OSNs for interaction with patients should clearly delineate their professional from their social “digital footprint.”26 For this group, consistency in the policy toward these interactions will be imperative in order to avoid the impression of favoritism amongst patients. Second, clinicians who maintain a personal presence in OSNs should be cognizant that it is a forum for potential patient interaction and lapses in professional integrity.6 Finally, for those who feel compelled to share access with patients, closely policing one’s privacy status and profile content is imperative.
There are several limitations to this study. First, it is common that surveys of medical professionals frequently yield low response rates,12,27 and, as noted above, the response rate in this study significantly limits the generalizability of study findings. This limitation exposes the results to the possibility of self-selection bias. That is, users of OSNs may have responded to the survey at a higher rate than those who do not use them out of interest in the topic. This is especially possible given the remarkably high usage rates of medical student respondents. However, the usage rates of practicing physicians and training physicians are consistent with data from other recent polling.9,19 Additionally, the lack of literature and previous studies of this topic meant that a validated survey tool did not previously exist, and had to be created in order to study this topic in this population. Because the survey tool did not undergo formal psychometric validation, we cannot be absolutely sure of the validity and reliability of the findings.
This study generates several questions that are worthy of further evaluation. First, replication of these results within a study with a more robust response rate will help in determining the generalizability of the results. Second, understanding how patients feel about physician interactions within OSNs would complement these findings and may help physicians to understand patients’ motivations behind these interactions. Additionally, study of any negative consequences that may have come from such interactions would provide outcomes data to help justify any substantive normative attitudes toward these interactions.
In summary, data from this study support and add to the growing literature suggesting that OSNs create a new forum for potential dual relationships between physicians, medical students and patients. OSNs may lead to new kinds of patient–doctor interactions, raising questions about appropriate professional boundaries.6,18,20,22,28 Physicians and physicians-in-training descriptively hold a variety of views regarding the ethical acceptability of such interactions, and the normative stance by medical professionals toward these interactions remains to be codified.17 The nature of professional boundaries in the digital age is worthy of further reflection and investigation.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(PDF 500 kb)
Acknowledgements
The authors would like to thank the Methodist Health Foundation, the Richard M. Fairbanks Foundation, and the IU Health Values Fund for their support and funding of this study. The authors would also like to thank Mrs. Amy Chamness-Douthit for her tireless work in coordinating the survey responses and data.
Conflicts of Interest None Disclosed.
References
- 1.Lenhart A (2009) Adults and Social Network Websites. http://pewinternet.org/Reports/2009/Adults-and-Social-Network-Websites.aspx?r=1. Accessed May 3, 2011.
- 2.Facebook (2010) Press Room-Statistics. http://www.Facebook.com/press/info.php?statistics. Accessed May 3, 2011.
- 3.Hitwise (2010) Top 20 sites and engines. http://www.hitwise.com/us/datacenter/main/dashboard-10133.html. Accessed May 3, 2011.
- 4.Lenhart A (2009) The Democratization of Online Social Networks: A look at the change in demographics of social network users over time. Pew Internet & American Life Project. http://pewinternet.org/Presentations/2009/41--The-Democratization-of-Online-Social-Networks.aspx. Accessed May 3, 2011.
- 5.Hawn C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood) 2009;28(2):361–368. doi: 10.1377/hlthaff.28.2.361. [DOI] [PubMed] [Google Scholar]
- 6.Chretien KC, Greysen SR, Chretien JP, Kind T. Online posting of unprofessional content by medical students. JAMA. 2009;302(12):1309–1315. doi: 10.1001/jama.2009.1387. [DOI] [PubMed] [Google Scholar]
- 7.Lacson SM, Bradley C, Arkfeld DG. Facebook medicine. J Rheumatol. 2009;36(1):211. doi: 10.3899/jrheum.080750. [DOI] [PubMed] [Google Scholar]
- 8.Jain SH. Practicing medicine in the age of Facebook. N Engl J Med. 2009;361(7):649–651. doi: 10.1056/NEJMp0901277. [DOI] [PubMed] [Google Scholar]
- 9.Moubarak G, Guiot A, Benhamou Y, Benhamou A, Hariri S. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37(2):101–104. doi: 10.1136/jme.2010.036293. [DOI] [PubMed] [Google Scholar]
- 10.Guseh JS, 2nd, Brendel RW, Brendel DH. Medical professionalism in the age of online social networking. J Med Ethics. 2009;35(9):584–586. doi: 10.1136/jme.2009.029231. [DOI] [PubMed] [Google Scholar]
- 11.American Medical Association (2010) Professionalism in the use of social media. http://www.ama-assn.org/ama/pub/meeting/professionalism-social-media.shtml. Accessed May 3, 2011.
- 12.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/S0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 13.Thompson LA, Dawson K, Ferdig R, Black EW, Boyer J, Coutts J, Black NP. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954–957. doi: 10.1007/s11606-008-0538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fletcher D. Facebook. Time. 2010;175(21):32–38. [Google Scholar]
- 15.Foreman J (2010) You, your doctor, and the internet. Los Angeles Times, April 26, 2010. http://articles.latimes.com/2010/apr/26/health/la-he-Facebook-20100426. Accessed May 3, 2011.
- 16.Cohen E (2009) Should you "friend" your doctor on Facebook? http://www.cnn.com/2009/HEALTH/09/03/friending.your.doctor/index.html. Accessed May 3, 2011.
- 17.Grover M. Defining the patient-physician relationship in the era of Facebook. Acad Med. 2010;85(8):1262. doi: 10.1097/ACM.0b013e3181e5c0d2. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald J, Sohn S, Ellis P. Privacy, professionalism and Facebook: a dilemma for young doctors. Med Educ. 2010;44(8):805–813. doi: 10.1111/j.1365-2923.2010.03720.x. [DOI] [PubMed] [Google Scholar]
- 19.Pew Research Center’s Internet & American Life Project (2010) Online News Survey Dataset. http://pewinternet.org/Shared-Content/Data-Sets/2010/January-2010--Online-News.aspx. Accessed May 3, 2011.
- 20.Gorrindo T, Groves JE. Web searching for information about physicians. JAMA. 2008;300(2):213–215. doi: 10.1001/jama.2008.44. [DOI] [PubMed] [Google Scholar]
- 21.Greysen SR, Kind T, Chretien KC. Online professionalism and the mirror of social media. J Gen Intern Med. 2010;25(11):1227–1229. doi: 10.1007/s11606-010-1447-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farnan JM, Paro JA, Higa J, Edelson J, Arora VM. The YouTube generation: implications for medical professionalism. Perspect Biol Med. 2008;51(4):517–524. doi: 10.1353/pbm.0.0048. [DOI] [PubMed] [Google Scholar]
- 23.Lagu T, Kaufman EJ, Asch DA, Armstrong K. Content of weblogs written by health professionals. J Gen Intern Med. 2008;23(10):1642–1646. doi: 10.1007/s11606-008-0726-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chretien KC, Azar J, Kind T. Physicians on Twitter. JAMA. 2011;305(6):566–568. doi: 10.1001/jama.2011.68. [DOI] [PubMed] [Google Scholar]
- 25.Rosenblum D. What anyone can know - The privacy risks of social networking sites. Ieee Security & Privacy. 2007;5(3):40–49. doi: 10.1109/MSP.2007.75. [DOI] [Google Scholar]
- 26.Pew Research Center’s Internet & American Life Project (2008) Digital Footprints. http://www.pewinternet.org/Presentations/2008/Digital-Footprints.aspx. Accessed May 3, 2011.
- 27.Martin BC. Don’t survey physicians! Chicago: American Medical Association; 1974. [Google Scholar]
- 28.Gorrindo T, Gorrindo PC, Groves JE. Intersection of online social networking with medical professionalism: can medicine police the Facebook boom? J Gen Intern Med. 2008;23(12):2155. doi: 10.1007/s11606-008-0810-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(PDF 500 kb)