A 54-year-old woman with a recent diagnosis of a large, surgically unresectable thymoma presented to the ER with shortness of breath, fever and a dry cough. Presenting chest x-ray showed bilateral infiltrates (Fig. 1). Four weeks previously she had received radiation therapy to the mediastinum along with chemotherapy. She was admitted to the hospital and started on broad spectrum antibiotics for presumed pneumonia. By hospital day four her oxygen requirements had worsened with an unchanged chest radiograph. A CT angiogram was performed and pulmonary embolism was excluded. The patient continued to deteriorate and was transferred to the intensive care unit. Steroids were initiated for possible radiation induced lung injury. Two days after the initiation of steroid treatment, a repeat chest radiograph showed drastic improvement of the bilateral infiltrates (Fig. 2). Radiation fields were compared with admission chest radiograph pulmonary infiltrates which correlated well (Fig. 3). Clinically, the radiographs and rapid improvement suggested a diagnosis of radiation pneumonitis, which occurs in 5-15% of patients who undergo radiation to the chest. Further investigation of her records showed that she received 28 radiation treatments delivered at 180cGy per fraction for a total dose of 5040cGy. Concurrent chemotherapy appears to increase risk of pneumonitis.1 The patient continued to rapidly improve and was discharged two days later.
Figure 1.
Presenting chest x-ray.
Figure 2.
Post-steroid treatment chest x-ray correspond to radiation fields.
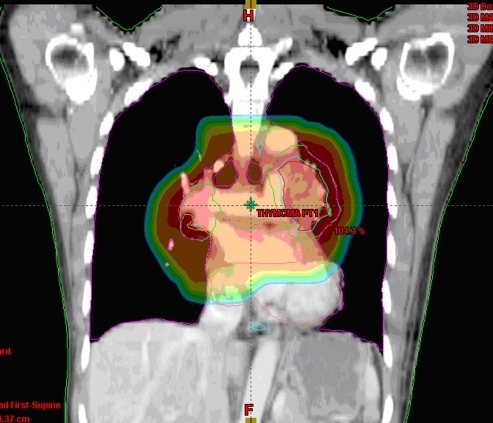
Figure 3.
Radiation fields corresponding with plain films.
Contributor Information
Von Ta, Phone: +1-916-2201566, FAX: +1-415-7757437, Email: tav@sutterhealth.org.
Paul Aronowitz, Phone: +1-415-6001133.
References
- 1.Chang, J. et al. Risk factors for Radiation Pneumonitis in Lung Cancer. Journal of Clinical Oncology. 2008 ASCO Annual Meeting Proceedings. 26, No 15 (May 20 Supplement):7573.