Abstract
Background
This study examines the prevalence of physician-diagnosed respiratory conditions and mental health symptoms in firefighters and emergency medical service workers up to 9 years after rescue/recovery efforts at the World Trade Center (WTC).
Methods
We analyzed FDNY physician and self-reported diagnoses by WTC exposure and quintiles of pulmonary function (FEV1%predicted). We used screening instruments to assess probable PTSD and probable depression.
Results
FDNY physicians most commonly diagnosed asthma (8.8%) and sinusitis (9.7%). The highest prevalence of physician-diagnosed obstructive airway disease (OAD) was in the lowest FEV1%predicted quintile. Participants who arrived earliest on 9/11 were more likely to have physician-diagnosed asthma (OR=1.4). 7% had probable PTSD. 19.4% had probable depression.
Conclusions
Self-reported and physician-diagnosed respiratory conditions remain common, especially among those who arrived earliest at the WTC site. OAD was associated with the lowest pulmonary function. Since respiratory and mental health conditions remain prevalent, ongoing monitoring and treatment is important.
Keywords: World Trade Center, Respiratory Health, Mental Health, Occupational Medicine, Firefighters
Introduction
After the World Trade Center (WTC) disaster, a consistent picture of respiratory and mental health conditions has emerged in subsets of the estimated 91,000 rescue/recovery workers [Farfel, et al. 2008]. Respiratory health studies have concentrated on symptoms and occasionally pulmonary function tests, but few have examined physician diagnoses of respiratory conditions. Those that have examined diagnoses have concentrated on self-reported diagnoses rather than on actual physician diagnoses from medical records [MMWR 2002, Brackbill, et al. 2009, Prezant, et al. 2008, Wheeler, et al. 2007]. Mental health studies have primarily focused on post-traumatic stress disorder (PTSD), using validated screening tools to provide prevalence estimates, often ignoring other conditions such as depression. Most published studies have focused on the first 5 years post-9/11, a few have examined co-morbidity on a limited basis, and even fewer have examined co-morbidity, within mental health or between respiratory and mental health. The goal of this study is to describe these conditions as they currently exist, nearly ten years post-9/11, in the only WTC-exposed cohort without significant self-selection bias or longitudinal dropout.
The 14,500 employees of the Fire Department of New York (FDNY), consisting of emergency medical service (EMS) workers and firefighters, represent a sentinel population to assess WTC health effects: this group has known pre-9/11 health status, high WTC exposure, and excellent cohort retention with regular health monitoring of active and retired workers. We and others have documented post-9/11 declines in pulmonary function, airway hyper-reactivity, and both respiratory and PTSD symptoms up to eight years post 9/11 [Farfel, et al. 2008, MMWR 2002, Brackbill, et al. 2009, Prezant, et al. 2008, Wheeler, et al. 2007, Aldrich, et al. 2010, Banauch, et al. 2003, Berninger, et al. 2010, DiGrande, et al. 2011, Galea, et al. 2002, Galea, et al. 2003, Herbert, et al. 2006, Kelly, et al. 2007, Perrin, et al. 2007, Prezant, et al. 2002, Reibman, et al. 2009, Stellman, et al. 2008, Webber, et al. 2009, Weiden, et al. 2010].
Adverse outcomes closely track with surrogate exposure measures, especially acute exposure to the massive dust cloud during the morning of 9/11, and arrival in the first days after the towers fell [Prezant, et al. 2002], and to a lesser extent, with prolonged work at the site [Webber, et al. 2009], where workers continued to encounter airborne contaminants consisting of re-aerosolized particulate matter and combustion byproducts [Farfel, et al. 2008].
This study describes the current burden of post-9/11 respiratory conditions (physician diagnoses, symptoms and pulmonary function), and mental health conditions (probable PTSD and probable depression) and their co-morbidities.
Methods
Participants
The population consisted of 14,314 firefighters and EMS workers who were hired before July 25, 2002, the date the WTC site formally closed, and who first arrived at the WTC site within the first 2 weeks after 9/11. Subjects signed informed consent at the time of enrollment, which allowed analysis of their information for research. This study was approved by the Institutional Review Board of Montefiore Medical Center (#07-09-320, #02-02-041E). The current analysis excluded N=1,943 persons without a monitoring exam during the study period (9/11/2007-9/10/2010); N=399 women due to small numbers; N=242 fire marshals as their tasks/exposures were different; and N=787 who did not have spirometry within 90 days of their monitoring exam, leaving 10,943 in the analytic cohort. If persons had more than one exam during the study period (9/11/2007-9/10/2009), we used data from the most recent one.
Data Sources
Demographic data came from the FDNY employee database, spirometry data from the FDNY-WTC-PFT database, and physician diagnoses from the FDNY physician diagnosis database. Beginning in 1996, the FDNY Bureau of Health Services (FDNY-BHS) medical monitoring and treatment program was updated to include an electronic medical treatment record with ICD9 coded diagnoses and mandatory monitoring exams that included spirometry, every 12–18 months. Since 10/2001, FDNY-BHS monitoring exams include self-administered physical and mental health questionnaires from which we obtained WTC exposure, respiratory symptoms, self-reported diagnoses of respiratory conditions, probable PTSD, and probable depression.
WTC exposure status
Exposure to the WTC site is based on initial arrival time as follows: arriving on the morning of 9/11 (arrival group 1); arriving during the afternoon of 9/11 (arrival group 2); arriving on 9/12/2001, Day 2 (arrival group 3); or arriving any day between days 3 and 14 (arrival group 4) [Prezant, et al. 2002]. We also created a duration variable - a summation of each calendar month that an individual worked for at least one day at the site, from September 2001 through July 2002 [Webber, et al. 2009].
Tobacco smoking status
Tobacco smoking was defined as “ever” if the participant reported current or former smoking on any health questionnaire and ”never” smokers if participants consistently reported never smoking on all questionnaires.
Pulmonary Function Test
Spirometry was performed according to American Thoracic Society guidelines and quality assurance standards. Forced expiratory volume in 1 second (FEV1) percent predicted (FEV1%predicted) was calculated using NHANES III equations based on age at examination, height, gender, and race/ethnicity [Aldrich, et al. 2010]. We used the FEV1%predicted from the day of the monitoring visit when the questionnaire was completed; if spirometry was not available from the same date, we used the closest FEV1%predicted within 90 days of the study visit.
Self-Reported Diagnoses
Self-reported diagnoses include diagnoses made by any physician, FDNY or otherwise. Self-reported diagnoses of obstructive airways diseases (OAD) were based on responses to the following questions: “In the past 12 months, has a doctor or health professional told you that you have current asthma, chronic bronchitis, or COPD/emphysema?” Self-reported sinusitis was obtained through a similar question. Multiple answers were allowed.
FDNY Physician Diagnoses
We reviewed the FDNY electronic medical record for diagnoses of any respiratory condition, to collect physician diagnoses of asthma, chronic bronchitis, COPD/emphysema, and sinusitis. To be used in our analyses, we required that a diagnosis be documented at least three times since 9/11 and at least one of these times during the study period (9/11/2007-9/10/2010). Multiple visits for the same diagnosis within a one month period were counted only once. Patients could have more than one diagnosis. We created an OAD category, consistent with the above requirements, which included at least one of the following diagnoses: asthma, chronic bronchitis, or COPD/emphysema. FDNY physicians receive instruction in diagnosing and treating respiratory diseases and are trained to use the same diagnostic criteria [Mannino 2003, Meltzer, et al. 2004]. Examining physicians select diagnoses after integrating the history, physical examination, spirometry, other pulmonary function testing, and chest imaging. For example, emphysema could be diagnosed if observed on chest CT imaging or pulmonary function testing but the diagnosis does not require that both criteria to be met. Asthma could be diagnosed if bronchodilator responsive (>12% and >200 ml increase in FEV-1), hyperreactive, or if there is a clear history of provocation that responds to bronchodilators. Chronic bronchitis is a clinical definition and does not require airflow obstruction.
Respiratory Symptoms
The questionnaire asked participants about respiratory symptoms in the last 12 months. For lower respiratory symptoms, answer choices included “no respiratory symptoms,” “wheezing,” “shortness of breath,” and “daily cough”; for upper respiratory symptoms, answers included “no nose or throat symptoms,” “nasal drip,” “nasal congestion.” Multiple answers were allowed.
Mental Health Symptoms
The self-administered mental health questionnaire included screening tools for PTSD and probable depression, which we required be completed within 90 days of the physical health questionnaire.
Probable PTSD
Probable PTSD was defined by the PTSD Checklist (PCL)-Civilian Version [Weathers, et al. 1993]. The PCL is a 17-item self-report survey corresponding to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for PTSD and linking symptoms to a specific traumatic experience (“the WTC attacks”). Symptoms were scored on a 5-point Likert scale and were grouped into three clusters: re-experiencing, avoidance, and hyper-arousal, and were assessed during the past 30 days. Individuals met the criteria for probable PTSD if they attained a summative score of 44 or greater (out of 85) [Blanchard, et al. 1996], and they fulfilled DSM-IV diagnostic criteria (affirming at least one re-experiencing symptom, at least three avoidance symptoms, and at least two hyper-arousal symptoms) [Blanchard, et al. 1994, Grubaugh, et al. 2005]. Combining the two criteria yielded a more conservative estimate of probable PTSD that has been used previously [Perrin, et al. 2007].
Probable Depression
Probable depression was measured using the Centers for Epidemiologic Studies Depression Scale (CES-D) with a cut-off of 16 and over. The CES-D screens for probable depression using 20 items rated on a 4-point scale [Radloff 1977].
Statistical Analysis
We examined factors such as arrival group in relation to FDNY physician diagnoses, self-reported diagnoses and current symptoms. Categorical variables were assessed using odds ratios (ORs) and 95% confidence intervals (95% CIs); continuous data were assessed using students T-tests. We ranked the measure of pulmonary function, FEV1%predicted at the time of the monitoring exam, and categorized values into quintiles for analysis of associations with variables including physician diagnoses and symptoms. Trends were tested using the Cochran-Armitage test. Spearman correlation coefficients were used to test the correlation between earlier and current FEV1%predicted values. We also used logistic regression models, adjusted for age on 9/11, retirement status, smoking and work duration to analyze the association between self-reported or FDNY physician diagnoses and early exposure to the WTC (arrival group 1). Data were analyzed using SAS, version 9.2 (SAS Institute, Cary, N.C.).
Results
Demographics
The analytic sample was composed of 9,715 (88.8%) male firefighters and 1,228 (11.2%) male EMS workers who took at least one physical health questionnaire during the study period. Most (67.8%) were between 25 and 44 years of age on 9/11, with a median age of 40.0 years. The majority of the cohort (60.6%) first arrived at the WTC site during the afternoon of 9/11 (arrival group 2) (Table I). 863 (7.9%) of the 10,943 were pre-9/11 FDNY retirees who returned to help with the rescue effort. The median age on 9/11 of the retirees was 52.0 years.
Table I.
Characteristics of the male study population who took at least one physical health questionnaire between 9/11/2007 and 9/10/2010
| Total Cohort | Fire | EMS | |
|---|---|---|---|
| N=10,943 | N=9,715 | N=1,228 | |
| Age on 9/11/01 | |||
| 18–24 | 198 (1.8%) | 138 (1.4%) | 60 (4.9%) |
| 25–44 | 7430 (67.9%) | 6469 (66.6%) | 961 (78.3%) |
| 45–64 | 3249 (29.7%) | 3043 (31.3%) | 206 (16.8%) |
| 65+ | 66 (0.6%) | 65 (0.7%) | 1 (0.1%) |
| Race | |||
| White | 9762 (89.2%) | 9117 (93.9%) | 645 (52.5%) |
| African American | 477 (4.4%) | 234 (2.4%) | 243 (19.8%) |
| Hispanic | 645 (5.9%) | 336 (3.5%) | 309 (25.2%) |
| Asian | 52 (0.5%) | 21 (0.2%) | 31 (2.5%) |
| Native American | 7 (0.1%) | 8 (0.1%) | 0 (0%) |
| Arrival Group* | |||
| 1 | 1686 (15.4%) | 1427 (14.7%) | 259 (21.1%) |
| 2 | 6634 (60.6%) | 5961 (61.4%) | 673 (54.8%) |
| 3 | 1431 (13.1%) | 1347 (13.9%) | 84 (6.8%) |
| 4 | 1192 (10.9%) | 980 (10.1%) | 212 (17.3%) |
| Duration of Exposure (median split)** | |||
| 1–3 Months | 4557 (50.6%) | 3931 (49.6%) | 626 (58.6%) |
| 4–11 Months | 4441 (49.4%) | 3999 (50.4%) | 442 (41.4%) |
| Duty Status | |||
| Active | 6385 (58.4%) | 5401 (55.6%) | 984 (80.1%) |
| Retired | 4558 (41.7%) | 4314 (44.4%) | 244 (19.9%) |
| Smoking Status‡ | |||
| Ever | 4308 (39.4%) | 3691 (38.0%) | 617 (50.3%) |
| Never | 6627 (60.6%) | 6018 (62.0%) | 609 (49.7%) |
| Total Surveys Taken | |||
| 1 | 2890 (26.4%) | 2743 (28.2%) | 147 (12.0%) |
| 2 | 4964 (45.4%) | 4637 (47.7%) | 327 (26.6%) |
| 3 | 3089 (28.2%) | 2335 (24.0%) | 754 (61.4%) |
Data are number (%).
Arrival group 1 arrived to the WTC site on the morning of 9/11; Arrival group 2 arrived on the afternoon of 9/11; arrival group 3 arrived on 9/12/2001; arrival group 4 arrived between days 3 and 14 after 9/11.
Duration of exposure is available for 8,998 (82.2%).
Smoking status is available for 10,935 (99.9%).
Pre-9/11 Health Status
In order to be hired as an FDNY firefighter, candidates cannot have a history of OAD (asthma, COPD or emphysema). They are also required to have FEV1 of at least 80% of predicted. Since job-related physical stress is less severe for EMS workers, they can be hired with mild OAD if well-controlled on medication. For EMS, the minimum required FEV1 must be at least 70% of predicted. If we define abnormal spirometry as <70% predicted, post-hire (but pre-9/11), less than 1% of firefighters and 2.5% of EMS workers fell below this threshold level [Aldrich, et al. 2010]. We found that pre-9/11 and current FEV1%predicted values were highly correlated (R=0.8) and that the best predictor of current diagnosis was the current FEV1%predicted. Post-hire but pre-9/11, there were only 85 cases of asthma (0.8% of the cohort) and no cases of emphysema/COPD.
Self-reported Diagnosis of Respiratory Diseases
Table II shows self-reported diagnoses as reported on the most recent questionnaire. The most common diagnosis overall was sinusitis (1,894, 17.3%) followed by bronchitis (1,333, 12.2%). Of those with sinusitis, 40.9% (774) had an OAD, of whom 514 (66.4%) reported bronchitis. While rates varied slightly, the relative ranking of diagnoses did not vary by fire vs. EMS service. The prevalence of diagnoses, however, differed by arrival group, with 255 (14%) arrival group 1 respondents reporting a current physician diagnosis of asthma compared to 70 (5.9%) of arrival group 4 (OR=3.3; 95% CI=2.4–4.8). This pattern was similar across all diagnoses.
Table II.
Self-reported physician diagnoses from the most recent physical health survey (N=10,943)
| Sinusitis | Current Asthma | Bronchitis | COPD/Emphysema | Obstructive Airway Disease* | No Self-Reported Diagnoses | |
|---|---|---|---|---|---|---|
| Total | 1894 (17.3%) | 1014 (9.3%) | 1333 (12.2%) | 446 (4.1%) | 2153 (19.7%) | 7641 (69.8%) |
| Fire | 1651 (17.0%) | 918 (9.5%) | 1200 (12.4%) | 413 (4.3%) | 1941 (20.0%) | 6791 (69.9%) |
| EMS | 243 (19.8%) | 96 (7.8%) | 133 (10.8%) | 33 (2.7%) | 212 (17.3%) | 850 (69.2%) |
| Duty Status | ||||||
| Active | 993 (15.6%) | 195 (3.1%) | 745 (11.7%) | 55 (0.9%) | 881 (13.8%) | 4799 (75.2%) |
| Retired | 901 (19.6%) | 819 (18.0%) | 588 (12.9%) | 391 (8.6%) | 1272 (27.9%) | 2842 (62.4%) |
| Arrival Group** | ||||||
| 1 | 345 (20.5%) | 218 (12.9%) | 237 (14.1%) | 93 (5.5%) | 404 (24.0%) | 1090 (64.7%) |
| 2 | 1127 (17.0%) | 579 (8.7%) | 814 (12.3%) | 217 (3.3%) | 1267 (19.1%) | 4681 (70.6%) |
| 3 | 240 (16.8%) | 147 (10.3%) | 187 (13.1%) | 91 (6.4%) | 307 (21.5%) | 981 (68.6%) |
| 4 | 182 (15.3%) | 70 (5.9%) | 95 (8.0%) | 45 (3.8%) | 175 (14.7%) | 889 (74.6%) |
| Duration of Exposure (median split)† | ||||||
| 1–3 Months | 727 (16.0%) | 324 (7.1%) | 505 (11.1%) | 143 (3.1%) | 770 (16.9%) | 3306 (72.6%) |
| 4–11 Months | 845 (19.0%) | 412 (9.3%) | 618 (13.9%) | 165 (3.7%) | 932 (21.0%) | 3020 (68.0%) |
| Smoking Status‡ | ||||||
| Ever | 711 (16.5%) | 420 (9.8%) | 543 (12.6%) | 307 (7.1%) | 931 (21.6%) | 2965 (68.8%) |
| Never | 1183 (17.9%) | 593 (9.0%) | 788 (11.9%) | 138 (2.1%) | 1220 (18.4%) | 4670 (70.5%) |
Data are number (%). Percentages are row percents.
Diagnoses are not mutually exclusive and therefore row percentages can add up to greater than 100%.
Obstructive airway disease includes current asthma, bronchitis, and COPD/emphysema.
Arrival group 1 arrived to the WTC site on the morning of 9/11; Arrival group 2 arrived on the afternoon of 9/11; arrival group 3 arrived on 9/12/2001; arrival group 4 arrived between days 3 and 14 after 9/11.
Duration of exposure is available for 8,998 (82.2%).
Smoking status is available for 10,935 (99.9%).
After adjusting for smoking status, age on 9/11, arrival group and duration at the WTC site, retirees were 10.2 times (95% CI=8.3–12.4) more likely to have asthma, and 7.4 times (95% CI=5.3–10.5) more likely to have COPD/emphysema than actives.
We also observed a striking association between FEV1%predicted expressed by quintile distribution and self-reported diagnoses for OAD (Table III). Among firefighters, the lowest FEV1%predicted quintile represented: 41.1% (377) of those with asthma and 50.6% (209) of those with COPD/emphysema and the highest FEV1%predicted quintile represented 10.5% (96) of those with asthma and 6.8% (28) of those with COPD/emphysema. Conversely, of those not reporting any respiratory diagnosis, 23.5% (1,594) were in the highest FEV1%predicted group while 14.6% (994) were in the lowest. EMS workers followed a similar pattern.
Table III.
Self-reported physician diagnoses from the most recent questionnaire associated with quintile of FEV1 %predicted (N=10,943)
| Quintile of FEV1% predicted | Sinusitis | Current Asthma | Bronchitis | COPD/Emphysema | Obstructive Airway Disease* | No Self-Reported Diagnoses |
|---|---|---|---|---|---|---|
| Fire | ||||||
| 20–82 | 312 (18.9%) | 377 (41.1%) | 288 (24.0%) | 209 (50.6%) | 595 (30.7%) | 994 (14.6%) |
| 83–89 | 324 (19.6%) | 194 (21.1%) | 203 (16.9%) | 81 (19.6%) | 360 (18.6%) | 1281 (18.9%) |
| 90–96 | 382 (23.1%) | 155 (16.9%) | 297 (24.8%) | 55 (13.3%) | 416 (21.4%) | 1528 (22.5%) |
| 97–103 | 303 (18.4%) | 96 (10.5%) | 216 (18.0%) | 40 (9.7%) | 302 (15.6%) | 1394 (20.5%) |
| 104–147 | 330 (20.0%) | 96 (10.5%) | 196 (16.3%) | 28 (6.8%) | 268 (13.8%) | 1594 (23.5%) |
| EMS | ||||||
| 20–82 | 87 (35.8%) | 54 (56.3%) | 64 (48.1%) | 25 (75.8%) | 104 (49.1%) | 284 (33.4%) |
| 83–89 | 48 (19.8%) | 14 (14.6%) | 18 (13.5%) | 3 (9.1%) | 34 (16.0%) | 166 (19.5%) |
| 90–96 | 55 (22.6%) | 10 (10.4%) | 21 (15.8%) | 2 (6.1%) | 31 (14.6%) | 163 (19.2%) |
| 97–103 | 32 (13.2%) | 12 (12.5%) | 23 (17.3%) | 1 (3.0%) | 31 (14.6%) | 131 (15.4%) |
| 104–147 | 21 (8.6%) | 6 (6.3%) | 7 (5.3%) | 2 (6.1%) | 12 (5.7%) | 106 (12.5%) |
Data are number (%). Percentages are column percents within service (Fire vs. EMS).
Diagnoses are not mutually exclusive.
Obstructive airway disease includes current asthma, bronchitis, and COPD/emphysema
FDNY Physician Diagnosed Respiratory Diseases
A total of 5,267 respondents (48.1%) had at least one visit to a FDNY physician for a respiratory problem, although most (2,994/5,267, 56.8%) did not meet our case criteria (Table IV). Asthma (963, 8.8%) and sinusitis (1065, 9.7%) were the most common FDNY-physician diagnoses. Those who had prolonged exposure to the WTC site, 4-11 months, were most commonly diagnosed with sinusitis (504, 11.4%) and bronchitis (457, 10.3%). There was a significantly higher prevalence of asthma among those in arrival group 1 (192, 11.4%) compared with those in arrival group 4 (61, 5.3%; OR=1.4, 95% CI=1.0-2.1). Retirees were again far more likely (OR=10.0; 95% CI=7.8-11.9) than actives to have asthma, after adjusting for smoking status, age on 9/11, arrival group and duration at the WTC site.
Table IV.
FDNY physician diagnosed respiratory conditions (N=10,943)
| Sinusitis | Asthma | Bronchitis | COPD/Emphysema | Obstructive Airway Disease* | No FDNY Diagnoses** | No Respiratory Visits to FDNY Physicians | |
|---|---|---|---|---|---|---|---|
| Total | 1065 (9.7%) | 963 (8.8%) | 903 (8.3%) | 55 (0.5%) | 1696 (15.5%) | 2994 (27.4%) | 5676 (51.9%) |
| Fire | 1041 (10.7%) | 911 (9.4%) | 890 (9.2%) | 51 (0.5%) | 1636 (16.8%) | 2825 (29.1%) | 4692 (48.3%) |
| EMS | 24 (2.0%) | 52 (4.2%) | 13 (1.1%) | 4 (0.3%) | 60 (4.9%) | 169 (13.8%) | 984 (80.1%) |
| Duty Status | |||||||
| Active | 595 (9.3%) | 169 (2.7%) | 589 (9.2%) | 10 (0.2%) | 691 (10.8%) | 1872 (29.3%) | 3431 (53.7%) |
| Retired | 470 (10.3%) | 794 (17.4%) | 314 (6.9%) | 45 (1.0%) | 1005 (22.1%) | 1122 (24.6%) | 2245 (49.3%) |
| Arrival Group† | |||||||
| 1 | 195 (11.6%) | 192 (11.4%) | 154 (9.1%) | 11 (0.7%) | 312 (18.5%) | 519 (30.8%) | 748 (44.4%) |
| 2 | 662 (10.0%) | 574 (8.7%) | 577 (8.7%) | 30 (0.5%) | 1041 (15.7%) | 1885 (28.4%) | 3362 (50.7%) |
| 3 | 137 (9.6%) | 134 (9.4%) | 113 (7.9%) | 13 (0.9%) | 226 (15.8%) | 333 (23.3%) | 797 (55.7%) |
| 4 | 71 (6.0%) | 63 (5.3%) | 59 (5.0%) | 1 (0.1%) | 117 (9.8%) | 257 (21.6%) | 769 (64.5%) |
| Duration of Exposure (median split)§ | |||||||
| 1–3 Months | 394 (8.7%) | 308 (6.8%) | 346 (7.6%) | 22 (0.5%) | 602 (13.2%) | 1188 (26.1%) | 2534 (55.6%) |
| 4–11 Months | 504 (11.4%) | 386 (8.7%) | 457 (10.3%) | 16 (0.4%) | 749 (16.9%) | 1282 (28.9%) | 2141 (48.2%) |
| Smoking Status | |||||||
| Ever | 387 (9.0%) | 413 (9.6%) | 310 (7.2%) | 46 (1.1%) | 674 (15.7%) | 1119 (26.0%) | 2324 (54.0%) |
| Never | 678 (10.2%) | 550 (8.3%) | 593 (9.0%) | 8 (0.1%) | 1021 (15.4%) | 1873 (28.3%) | 3347 (50.5%) |
Data are number (%). Percentages are row percents.
Diagnoses are not mutually exclusive and therefore row percentages can add up to greater than 100%.
Obstructive airway disease includes current asthma, bronchitis, and COPD/emphysema.
Had FDNY doctor visits but did not have at least three visits with same diagnosis.
Arrival group 1 arrived to the WTC site on the morning of 9/11; Arrival group 2 arrived on the afternoon of 9/11; arrival group 3 arrived on 9/12/2001; arrival group 4 arrived between days 3 and 14 after 9/11.
Duration of exposure is available for 8,998 (82.2%).
Smoking status is available for 10,935 (99.9%).
Similar to the pattern observed with self-reported diagnoses, the highest proportion of physician diagnosed OAD in firefighters was in the lowest FEV1%predicted quintile (Table V): 41.4% (377) of those with asthma and 22.4% (199) of those with bronchitis. These OAD diagnosis patterns were similar in EMS workers. Sinusitis, however, did not follow any obvious pattern (206, 19.8% in the lowest quintile vs. 190, 18.3% in the highest).
Table V.
FDNY physician diagnosed respiratory conditions associated with quintile of FEV1 %predicted (N=10,943)
| Quintile of FEV1% predicted | Sinusitis | Asthma | Bronchitis | COPD/Emphysema | Obstructive Airway Disease* | No FDNY Diagnoses** | No Respiratory Visits to FDNY Physicians |
|---|---|---|---|---|---|---|---|
| Fire | |||||||
| 20–82 | 206 (19.8%) | 377 (41.4%) | 199 (22.4%) | 33 (64.7%) | 518 (31.7%) | 489 (17.3%) | 621 (13.2%) |
| 83–89 | 207 (19.9%) | 177 (19.4%) | 186 (20.9%) | 8 (15.7%) | 322 (19.7%) | 562 (19.9%) | 851 (18.1%) |
| 90–96 | 250 (24.0%) | 158 (17.3%) | 215 (24.2%) | 5 (9.8%) | 340 (20.8%) | 657 (23.3%) | 1047 (22.3%) |
| 97–103 | 188 (18.1%) | 104 (11.4%) | 162 (18.2%) | 2 (3.9%) | 249 (15.2%) | 563 (19.9%) | 974 (20.8%) |
| 104–147 | 190 (18.3%) | 95 (10.4%) | 128 (14.4%) | 3 (5.9%) | 207 (12.7%) | 554 (19.6%) | 1199 (25.6%) |
| EMS | |||||||
| 20–82 | 11 (45.8%) | 31 (59.6%) | 7 (53.9%) | 2 (50.0%) | 34 (56.7%) | 80 (47.3%) | 324 (32.9%) |
| 83–89 | 4 (16.7) | 5 (9.6%) | 2 (15.4%) | 1 (25.0%) | 7 (11.7%) | 39 (23.1%) | 184 (18.7%) |
| 90–96 | 6 (25.0%) | 8 (15.4%) | 2 (15.4%) | 1 (25.0%) | 10 (16.7%) | 25 (14.8%) | 198 (20.1%) |
| 97–103 | 2 (8.3%) | 5 (9.6%) | 2 (15.4%) | 0 (0%) | 6 (10.0%) | 19 (11.2%) | 154 (15.7%) |
| 104–147 | 1 (4.2%) | 3 (5.8%) | 0 (0%) | 0 (0%) | 3 (5.0%) | 6 (3.6%) | 124 (12.6%) |
Data are number (%). Percentages are column percents within service (Fire vs. EMS).
Diagnoses are not mutually exclusive.
Obstructive airway disease includes current asthma, bronchitis, and COPD/emphysema
Had FDNY doctor visits but did not have at least three visits with same diagnosis.
Respiratory Symptoms
Figure I shows respiratory symptoms by FEV1%predicted quintile. In those reporting cough, 27.8% (283) had a FEV1%predicted in the lowest quintile whereas only 16.9% (172) were in the highest FEV1%predicted quintile (OR=1.8; 95% CI=1.5–2.2). The same pattern holds for the other lower respiratory symptoms whereas, similar to physician diagnosed sinusitis, nasal congestion/drip was not associated with FEV1%predicted quintile.
Figure I. Percentage of most recent self-reported respiratory symptoms in quintiles of FEV1% among both firefighters and EMS workers (N=10,943).
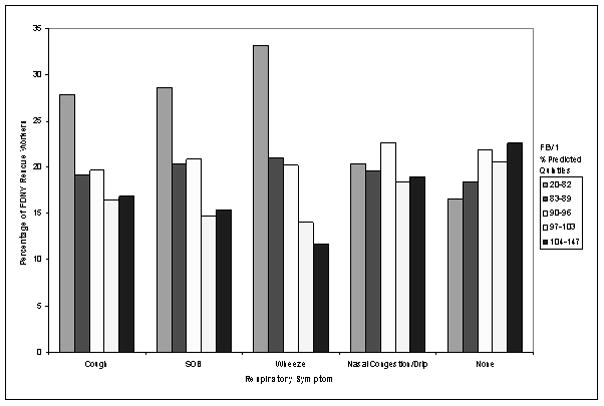
“None” means there were no reported respiratory symptoms (cough, SOB, wheeze, and nasal congestion/drip)
Probable PTSD and Probable Depression
10,867 (99.3%) participants took the FDNY mental health questionnaire within 90 days of their physical health survey and monitoring exam. At the time of the most recent questionnaire, 6.9% (752) of the population had probable PTSD (Table VI). There was no significant difference between firefighters and EMS workers in the prevalence of either probable PTSD or probable depression.
Table VI.
Probable PTSD and probable depression as reported on the most recent self-administered mental health questionnaire between 9/11/2007 and 9/10/2010 (N=10,867)§
| Probable PTSD | Probable Depression | Probable PTSD with Probable Depression | Below threshold for Probable PTSD or Probable Depression* | No Symptoms of Probable PTSD or Probable Depression** | |
|---|---|---|---|---|---|
| Total | 752 (6.9%) | 2106 (19.4%) | 715 (6.6%) | 7777 (71.6%) | 947 (8.7%) |
| Fire | 673 (7.0%) | 1879 (19.5%) | 641 (6.7%) | 6891 (71.5%) | 843 (8.7%) |
| EMS | 79 (6.5%) | 227 (18.6%) | 74 (6.1%) | 886 (72.5%) | 104 (8.5%) |
| Duty Status | |||||
| Active | 231 (3.6%) | 850 (13.4%) | 215 (3.4%) | 4812 (75.6%) | 688 (10.8%) |
| Retired | 521 (11.6%) | 1256 (27.9%) | 500 (11.1%) | 2965 (65.9%) | 259 (5.8%) |
| Arrival Group† | |||||
| 1 | 201 (12.0%) | 419 (25.1%) | 193 (11.6%) | 1132 (67.7%) | 112 (6.7%) |
| 2 | 413 (6.3%) | 1213 (18.4%) | 392 (6.0%) | 4755 (72.1%) | 603 (9.2%) |
| 3 | 85 (6.0%) | 296 (20.8%) | 82 (5.8%) | 1018 (71.5%) | 107 (7.5%) |
| 4 | 53 (4.5%) | 178 (15.1%) | 48 (4.1%) | 872 (73.9%) | 125 (10.6%) |
| Duration of Exposure (median split) †† | |||||
| 1–3 Months | 261 (5.8%) | 790 (17.4%) | 247 (5.5%) | 3296 (72.7%) | 435 (10.0%) |
| 4–11 Months | 322 (7.3%) | 880 (19.9%) | 305 (6.9%) | 3141 (71.2%) | 375 (8.5%) |
| Smoking Status‡ | |||||
| Ever | 307 (7.2%) | 914 (21.4%) | 295 (6.9%) | 3000 (70.3%) | 340 (8.0%) |
| Never | 444 (6.7%) | 1190 (18.1%) | 419 (6.4%) | 4771 (72.4%) | 607 (9.2%) |
Data are number (%). Percentages are row percentages.
Probable PTSD and probable depression are not mutually exclusive.
Self-administered questionnaire data was available for 10,867 (99.3%).
This group has one or more symptoms of probable PTSD or depression.
This group has zero PTSD and zero depression symptoms.
Arrival group 1 arrived to the WTC site on the morning of 9/11; Arrival group 2 arrived on the afternoon of 9/11; arrival group 3 arrived on 9/12/2001; arrival group 4 arrived between days 3 and 14 after 9/11.
Duration of exposure is available for 8,998 (82.2%).
Current smoking status is available for 10,935 (99.9%).
In unadjusted analyses we found that those in arrival group 1 were 2.8 times (95% CI=2.0–3.8) more likely to have probable PTSD than those in arrival group 4. Those with probable PTSD were at the WTC site significantly longer (mean=4.6 months, SD=3.1) than those without probable PTSD (mean=4.1 months, SD=2.8; p=0.002). In multivariable logistic regression models, after adjustment for smoking status, age on 9/11, duration at the WTC site, and retirement, those with probable PTSD were 3.3 times (95% CI=2.3–4.9) more likely to have arrived at the WTC site on the morning of 9/11 (12.0% of arrival group 1 compared with 4.5% of arrival group 4). Participants with probable PTSD were 4.9 times (95% CI=4.0–6.0) more likely to be retired, after adjustment for smoking status, age at 9/11, arrival group, and duration at the site.
Nearly 20% (19.4%; N=2,106) of the population had probable depression (table VI). In unadjusted analyses we found that those with probable depression worked at the WTC site significantly longer (mean=4.4 months, SD=3.0) than those without probable depression (mean=4.1, SD=2.8, p=0.0006). In multivariable logistic regression models, after adjustment for smoking status, age on 9/11, duration at the WTC site, and retirement, those with probable depression were 2.2 times (95% CI=1.7–2.7) more likely to have arrived at the WTC site on the morning of 9/11 (25.1% of arrival group 1 compared with 15.1% of arrival group 4). Participants with probable depression were 3 times (95% CI=2.6–3.4) more likely to be retired, after adjustment for smoking status, age at 9/11, arrival group, and duration at the site.
Co-morbidity of mental health conditions was also common: of the 752 patients with probable PTSD, all but 37 (4.9%) also screened positive for probable depression (Table VI). Of the entire cohort, 715 (6.6%) screened positive for both probable PTSD and probable depression. Similarly, we found an association between co-morbidity and arrival group: 11.6% (193) of arrival group 1 had co-morbid probable PTSD and probable depression while only 4.1% (48) of arrival group 4 had both. Participants with both probable PTSD and probable depression were 5.1 times (95% CI=4.1–6.3) more likely to be retired, after adjustment for smoking status, age on 9/11, arrival group and duration at the WTC site.
There was also co-morbidity of mental health and respiratory conditions. 314 (41.8%) of those with probable PTSD also self-reported an OAD diagnosis. 698 (33.1%) of those with probable depression also self-reported an OAD diagnosis. 710 (33.3%) of those with probable PTSD or probable depression also self-reported an OAD diagnosis. Since there was high co-morbidity between depression and probable PTSD, of those with depression alone (without probable PTSD), 28.5% (396) self-reported an OAD diagnosis. Similar results were found when physician diagnoses from the medical record were used instead of self-reported diagnoses.
Discussion
This is the first study to describe the elevated prevalence of respiratory diagnoses, both FDNY-physician diagnosed and self-reported and probable PTSD and probable depression seven to nine years after working at the WTC site. As reported previously, prior to 9/11, firefighters in this cohort had excellent pulmonary function [Aldrich, et al. 2010] and rarely reported lower respiratory symptoms or disease [Webber, et al. 2009], consistent with our impression of a healthy workforce before 9/11 [Aldrich, et al. 2010, Kelly, et al. 2007, Webber, et al. 2009]. Seven to nine years later, we also found a high burden of current mental health symptoms, with almost 7% of the workforce reporting probable PTSD and 19.4% reporting probable depression. Particularly interesting is the burden of co-morbidity −95% of those with probable PTSD also screened positive for probable depression.
We have previously documented a decline in FEV1%predicted within 6 months of 9/11, with stabilization but little recovery over the next seven years [Aldrich, et al. 2010]. Other studies in WTC-exposed populations have similarly found abnormal spirometry [Herbert, et al. 2006], abnormal lung function [Prezant, et al. 2008, Aldrich, et al. 2010, Herbert, et al. 2006, Reibman, et al. 2009, Weiden, et al. 2010] and bronchial hyperreactivity after 9/11 [Banauch, et al. 2003, Prezant, et al. 2002]. The current study is the first to demonstrate that lower lung function is associated not only with WTC exposure and persistent respiratory symptoms, but also with actual physician diagnoses obtained directly from the FDNY medical chart, an association previously reported only for self-reported diagnoses of asthma [MMWR 2002, Brackbill, et al. 2009, Prezant, et al. 2008, Wheeler, et al. 2007]. This association is even more convincing as it was evident in participants with physician-diagnosed lower respiratory diseases, but not in those with upper respiratory disease. Further, the highest proportion of FDNY rescue workers with confirmed physician diagnosed asthma, bronchitis, and COPD/emphysema had the lowest FEV1%predicted levels indicating that persistent respiratory injury since exposure to the WTC had resulted in disease. We believe that the increase in respiratory diagnoses is not related to usual firefighting activities as pre-9/11 the prevalence of these conditions was low due to strict hiring criteria (especially in firefighters), decreasing structural fires over the last several decades [Fire Department of the City of New York 2009], and improved use of personal protective equipment. In addition, post-9/11 there has been dramatic reductions in smoking rates [Aldrich, et al. 2010].
We acknowledge that rates of some respiratory diseases increase with age [Lethbridge-Cejku, et al. 2006], but the rates that we found exceed those in the general population for individuals of similar age. Consistent with these high rates, we recently reported a four-fold increase in the number of disability retirements due to respiratory illness since 9/11 [Niles, et al. 2011]. Nearly all of the respiratory disability was due to OAD, with the majority due to asthma.
Before 9/11, the prevalence of chronic sinusitis symptoms was low [Prezant, et al. 2008, Kelly, et al. 2007], becoming elevated post-9/11 [Prezant, et al. 2008, Herbert, et al. 2006, Kelly, et al. 2007, Reibman, et al. 2009]. The physician-diagnosed cases of chronic sinusitis in the current study provide important new information and show a continued association with WTC-exposure, but without an association with pulmonary function. Seven to nine years later, the persistence of an association between upper and lower respiratory disease and WTC-exposure reinforces the need for ongoing monitoring and treatment, as it is clear that many of these conditions now represent chronic disease.
Rates of self-reported diagnoses were consistently higher than for physician diagnoses. This discrepancy is not unexpected. Self-report includes diagnoses made by any physician, FDNY or otherwise. Our members have access to health care both at FDNY and elsewhere, whereas we only have access to the FDNY electronic medical record. Self-report may also include self-diagnoses even though the question specified a diagnosis made by a “doctor or healthcare professional”. However, for COPD/emphysema, the high rates of self-report as compared to FDNY physician diagnosis argue additionally for the over-diagnosis of this disease in the community due to a lack of clearly defined criteria [Mannino 2003].
Previous studies have shown an elevated risk for probable PTSD in this and other WTC-exposed populations [Berninger, et al. 2010, DiGrande, et al. 2011], which we confirm seven to nine years later. After the Oklahoma City bombing, PTSD among firefighters was found to be prevalent and associated with increased time spent at the disaster site [North, et al. 2002], which we also find in our cohort. Probable PTSD was not the only mental health condition found in our population: overall, one-fifth of this population screened positive for probable depression, which is higher than rates from previous screening studies of WTC-exposed populations [Galea, et al. 2002, Stellman, et al. 2008]. This finding is especially important given the time interval since 9/11 and is particularly striking in relation to the 12 month prevalence of depression in U.S. general adult population, which is 6.7% [Kessler, et al. 2005]. Other studies on male war veterans found high rates of depression related to war trauma 20 years after returning home, suggesting that depression may be a persistent problem after trauma [Ginzburg, et al. 2010]. Although probable PTSD and probable depression represent screening results and not clinician diagnoses, they have been validated in this [Chiu, et al. 2011, Chiu, et al. 2010] and other populations [Radloff 1977, Lewinsohn, et al. 1997]. Additionally, using these screening tools is consistent with other research done on mental health post-9/11 [Farfel, et al. 2008, Berninger, et al. 2010, DiGrande, et al. 2011, Stellman, et al. 2008]. It is important, however, to note the overlap between question content in the screening instruments for probable PTSD and probable depression. Therefore, while these conditions are elevated, the co-morbidity between these two mental health conditions may in part be artifactual.
In contrast, there is clear co-morbidity between respiratory and mental health conditions, with 314 (41.8%) of those with probable PTSD also reporting an OAD diagnosis and 698 (33.1%) of those with probable depression also reporting an OAD diagnosis. Five years post-9/11, Brackbill et al. has also reported high rates of co-morbidity between self-reported asthma and probable PTSD but associations with broader category of disease (OAD and depression) were not included [Brackbill, et al. 2009]. Mental health conditions are well-known to be associated with respiratory disease [Goodwin and Pine 2002], especially with the sensation of dyspnea. Therefore, we suggest that concurrent screening and treatment for mental and physical health conditions be done.
Study limitations include the lack of access to treatment data for both the respiratory and mental health conditions, which inhibits our ability to assess treatment effects. And, since our questionnaires collected information at the same time, we cannot comment on the temporal association between mental and physical health co-morbid diagnoses. Additionally, our duration variable is calculated by asking individuals if they spent at least one day at the WTC site in a given month. Therefore, we do not know the number of days an individual spent working at the WTC site.
In conclusion, this is the first study in a WTC-exposed population to analyze a wide-spectrum upper and lower respiratory diseases using actual physician diagnoses. The most common respiratory diagnoses were asthma, chronic bronchitis, and sinusitis. Seven to nine years later, reduced pulmonary function and WTC exposure were associated with lower respiratory disease while only exposure was associated with upper respiratory disease. Strengths of this study include minimal self-selection bias in the population studied and a healthy worker effect resulting in minimal respiratory disease prior to 9/11 [Aldrich, et al. 2010, Kelly, et al. 2007, Webber, et al. 2009]. The frequent associations between probable PTSD and probable depression underscore the need to treat these conditions together. Given that 9 years later, about 41% of FDNY firefighters and EMS workers report that they still suffer from at least one WTC-related physical or mental health condition, and that co-morbidity is present in about one-third of those with any physical or mental health condition, it is important that medical monitoring continue and that treatment be refocused with increased emphasis on comorbidities.
Acknowledgments
Grant Sponsor: National Institute of Occupational Safety and Health; Grant Number: 3U10-OH008242; 3U10-OH008243.
Grant Sponsor: National Institute of Health; Grant Number: K23HL08419; K24A1080298
This study was funded by the National Institute of Occupational Safety and Health (3U10-OH008242; 3U10-OH008243) and the National Institute of Health (K23HL08419; K24A1080298).
References
- Farfel M, DiGrande L, Brackbill R, Prann A, Cone J, Friedman S, Walker DJ, Pezeshki G, Thomas P, Galea S, Williamson D, Frieden TR, Thorpe L. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health. 2008;85:880–909. doi: 10.1007/s11524-008-9317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MMWR. Self-reported increase in asthma severity after the September 11 attacks on the World Trade Center--Manhattaan, New York, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:781–784. [PubMed] [Google Scholar]
- Brackbill RM, Hadler JL, DiGrande L, Ekenga CC, Farfel MR, Friedman S, Perlman SE, Stellman SD, Walker DJ, Wu D, Yu S, Thorpe LE. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302:502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower respiratory diseases after occupational and environmental disasters. Mt Sinai J Med. 2008;75:89–100. doi: 10.1002/msj.20028. [DOI] [PubMed] [Google Scholar]
- Wheeler K, McKelvey W, Thorpe L, Perrin M, Cone J, Kass D, Farfel M, Thomas P, Brackbill R. Asthma diagnosed after 11 September 2001 among rescue and recovery workers: findings from the World Trade Center Health Registry. Environ Health Perspect. 2007;115:1584–1590. doi: 10.1289/ehp.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldrich TK, Gustave J, Hall CB, Cohen HW, Webber MP, Zeig-Owens R, Cosenza K, Christodoulou V, Glass L, Al-Othman F, Weiden MD, Kelly KJ, Prezant DJ. Lung function in rescue workers at the World Trade Center after 7 years. N Engl J Med. 2010;362:1263–1272. doi: 10.1056/NEJMoa0910087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banauch GI, Alleyne D, Sanchez R, Olender K, Cohen HW, Weiden M, Kelly KJ, Prezant DJ. Persistent hyperreactivity and reactive airway dysfunction in firefighters at the World Trade Center. Am J Respir Crit Care Med. 2003;168:54–62. doi: 10.1164/rccm.200211-1329OC. [DOI] [PubMed] [Google Scholar]
- Berninger A, Webber MP, Cohen HW, Gustave J, Lee R, Niles JK, Chiu S, Zeig-Owens R, Soo J, Kelly K, Prezant DJ. Trends of elevated PTSD risk in firefighters exposed to the World Trade Center disaster: 2001–2005. Public Health Rep. 2010;125:556–566. doi: 10.1177/003335491012500411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. Am J Epidemiol. 2011;173:271–281. doi: 10.1093/aje/kwq372. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346:982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, Bucuvalas M, Kilpatrick D. Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. Am J Epidemiol. 2003;158:514–524. doi: 10.1093/aje/kwg187. [DOI] [PubMed] [Google Scholar]
- Herbert R, Moline J, Skloot G, Metzger K, Baron S, Luft B, Markowitz S, Udasin I, Harrison D, Stein D, Todd A, Enright P, Stellman JM, Landrigan PJ, Levin SM. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114:1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly K, Niles J, McLaughlin MT, Carroll S, Corrigan M, Al-Othman F, Prezant D. World Trade Center Health Impacts on FDNY Rescue Workers, A Six-Year Assessment: September 2001-September 2007. Fire Department; City of New York: 2007. [Google Scholar]
- Perrin MA, DiGrande L, Wheeler K, Thorpe L, Farfel M, Brackbill R. Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am J Psychiatry. 2007;164:1385–1394. doi: 10.1176/appi.ajp.2007.06101645. [DOI] [PubMed] [Google Scholar]
- Prezant DJ, Weiden M, Banauch GI, McGuinness G, Rom WN, Aldrich TK, Kelly KJ. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med. 2002;347:806–815. doi: 10.1056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- Reibman J, Liu M, Cheng Q, Liautaud S, Rogers L, Lau S, Berger KI, Goldring RM, Marmor M, Fernandez-Beros ME, Tonorezos ES, Caplan-Shaw CE, Gonzalez J, Filner J, Walter D, Kyng K, Rom WN. Characteristics of a residential and working community with diverse exposure to World Trade Center dust, gas, and fumes. J Occup Environ Med. 2009;51:534–541. doi: 10.1097/JOM.0b013e3181a0365b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellman JM, Smith RP, Katz CL, Sharma V, Charney DS, Herbert R, Moline J, Luft BJ, Markowitz S, Udasin I, Harrison D, Baron S, Landrigan PJ, Levin SM, Southwick S. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116:1248–1253. doi: 10.1289/ehp.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber MP, Gustave J, Lee R, Niles JK, Kelly K, Cohen HW, Prezant DJ. Trends in respiratory symptoms of firefighters exposed to the world trade center disaster: 2001–2005. Environ Health Perspect. 2009;117:975–980. doi: 10.1289/ehp.0800291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiden MD, Ferrier N, Nolan A, Rom WN, Comfort A, Gustave J, Zeig-Owens R, Zheng S, Goldring RM, Berger KI, Cosenza K, Lee R, Webber MP, Kelly KJ, Aldrich TK, Prezant DJ. Obstructive airways disease with air trapping among firefighters exposed to World Trade Center dust. Chest. 2010;137:566–574. doi: 10.1378/chest.09-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannino DM. Chronic obstructive pulmonary disease: definition and epidemiology. Respir Care. 2003;48:1185–1191. discussion 1191–1183. [PubMed] [Google Scholar]
- Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, Bachert C, Baraniuk J, Baroody FM, Benninger MS, Brook I, Chowdhury BA, Druce HM, Durham S, Ferguson B, Gwaltney JM, Kaliner M, Kennedy DW, Lund V, Naclerio R, Pawankar R, Piccirillo JF, Rohane P, Simon R, Slavin RG, Togias A, Wald ER, Zinreich SJ. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114:155–212. doi: 10.1016/j.jaci.2004.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist (PCL): Realiability, validity, and diagnostic utility. Annual Meeting of the International Society of Traumatic Stress Studies; San Antonio, Texas. 1993. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. Psychological morbidity associated with motor vehicle accidents. Behav Res Ther. 1994;32:283–290. doi: 10.1016/0005-7967(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Grubaugh AL, Magruder KM, Waldrop AE, Elhai JD, Knapp RG, Frueh BC. Subthreshold PTSD in primary care: prevalence, psychiatric disorders, healthcare use, and functional status. J Nerv Ment Dis. 2005;193:658–664. doi: 10.1097/01.nmd.0000180740.02644.ab. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Fire Department of the City of New York. FDNY Annual Report 2008–2009. New York City: 2009. [Google Scholar]
- Lethbridge-Cejku M, Rose D, Vickerie J. Vital Health Statistics. 2006. Summary health statistics for U.S. adults: National Health Interview Survey, 2004. [PubMed] [Google Scholar]
- Niles JK, Webber MP, Gustave J, Zeig-Owens R, Lee R, Glass L, Weiden MD, Kelly KJ, Prezant DJ. The impact of the world trade center attack on FDNY firefighter retirement, disabilities, and pension benefits. Am J Ind Med. 2011 doi: 10.1002/ajim.20965. [DOI] [PubMed] [Google Scholar]
- North CS, Tivis L, McMillen JC, Pfefferbaum B, Spitznagel EL, Cox J, Nixon S, Bunch KP, Smith EM. Psychiatric disorders in rescue workers after the Oklahoma City bombing. Am J Psychiatry. 2002;159:857–859. doi: 10.1176/appi.ajp.159.5.857. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord. 2010;123:249–257. doi: 10.1016/j.jad.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Chiu S, Webber MP, Zeig-Owens R, Gustave J, Lee R, Kelly KJ, Rizzotto L, McWilliams R, Schorr JK, North CS, Prezant DJ. Performance characteristics of the PTSD Checklist in retired firefighters exposed to the World Trade Center disaster. Ann Clin Psychiatry. 2011;23:95–104. [PubMed] [Google Scholar]
- Chiu S, Webber MP, Zeig-Owens R, Gustave J, Lee R, Kelly KJ, Rizzotto L, Prezant DJ. Validation of the Center for Epidemiologic Studies Depression Scale in screening for major depressive disorder among retired firefighters exposed to the World Trade Center disaster. J Affect Disord. 2010;121:212–219. doi: 10.1016/j.jad.2009.05.028. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Pine DS. Respiratory disease and panic attacks among adults in the United States. Chest. 2002;122:645–650. doi: 10.1378/chest.122.2.645. [DOI] [PubMed] [Google Scholar]


