Abstract
The use of psychostimulants as an adjuvant therapy in treatment-resistant depression is not very common nowadays and has been the subject of much criticism. This article gives a brief review of the literature and reports on the findings from a retrospective study carried out in 65 depressed patients treated with psychostimulants (amphetamine and methylphenidate) in addition to conventional antidepressants. Thirty-eight out of 65 patients showed significant improvement, in particular with respect to energy mood, and psychomotor activity. The best response to psychostimulants was seen in inhibited types of depression and in combination with a tricyclic antidepressant. None of the patients developed drug dependency. The incidence of side effects was low, and agitation and restlessness improved with an additional short-term treatment with benzodiazepines. It is concluded that the rapid onset of action (2-3 hours) after administration may help cover the therapeutic latency period of conventional antidepressants and probably potentiates their effect. In view of their potential benefits in treatment-resistant depressive states, psychostimulants should be tried more often.
Keywords: psychostimulant, adjuvant therapy, treatment-resistant depression, combination with tricyclics, dependency, rapid onset, potentiation of antidepressant effect
Abstract
El uso de psicoestimulantes como fúrmacos potenciadores en el tratamiento de las depresiones resistentes no es muy frecuente en la actualidad y signe siendo motivo de críticas. Este artículo revisa parte de la lieratura y refiere los resultados de un estudio retrospectivo realizado en 65 paceientes con depresión que recibieron psicoestimulantes (anfetamina y metilfenidato) además de antidepresivos convencionales. Treinta y aocho pacentes mostraron una mejoría significativa de la energía, el ánimo y la actividad psicomotora. La mejor respuesta a los psicoestimulantes se observó en los pacentes con depresión inhubidu que recibieron tricídicos. Ninguno de los pacientes desarrolló una farmacodependencia. La incidencia de efectos adversos fue baja ; la agitación e inquietud se redujeron con benzodiazepinas utilizadas por poco tiempo. Se concluyyó que el rápido inicio de la acción de los psicoestimulantes (2 a 3 horas) luego de su administración, puede ayudar a cubrir el período de latencia terapéutica de los antidepresivos convencionales y probablemente potencie el efecto de estos últimos. Los psicoestimulantes debieran utilizarse con más frecuencia en el tratamineto de la depresión resistente considerando sus potenciales ventajas.
Abstract
L'utilisation des psychostimulants comme traitement adjuvant des dépressions résistantes n'est pas très fréquente de nos jours et a été largement critiquée. Cet article donne un aperçu rapide de la littérature et rapporte les résultats d'une étude rétrospective menée chez 65 patients dépressifs cotraités par psychostimulants (amphétamine et méthylphémidate) et antidépresseurs classiques. Trente-huit patients sur 65 ont montré une amélioration significative, en particulier, en ce qui concerne l'énergie, l'humeur et l'activité psychomotrice. La meilleure réponse aux psychostumulants a été notée pour les dépressions ralenties et en association avec un antidépresseur tricyclique. Aucun des patients n'a développé de phénomène de dépendance. La fréquence des effets secondaires était faible, et l'agitation et la nervosité ont été améliorées par une prescription de courte durée de benzodiazépines. En conclusion, la survenue rapide (2 à 3 heures) de l'effet après la prise pourrait aider à couvrir la période de latence thérapeutique des antidépresseurs classiques et, probablement, potentialiser leurs effets. Vu leurs bénéfices potentiels dans le traitement des dépressions résistantes, les psychostimulants devraient être plus fréquemment utilisés.
The use of psychostimulants in the therapy of treatment-resistant depression in addition to conventional antidepressants is not very common and has been criticized by some authors. In Germany, Austria, and Switzerland, depression is not a listed indication for the use of psychostimulants. In contrast, at the Zurich Psychiatric University Hospital, dextroamphetamine and ritalin have been used since the thirties to treat severe cases of treatment-resistant depression, especially in the presence of prominent fatigue and apathy, and psychostimulants are now well established as an adjuvant therapy. This article reviews the literature on the use of psychostimulants in treatment-resistant depression and discusses the findings relative to therapeutic efficacy, side effects, and frequency of dependency from a retrospective study carried out in 65 patients of our hospital treated with psychostimulants.
Review of the literature
Historical background
Amphetamine was first, synthesized in 1887, with the first significant, clinical investigations being performed in 1927.1 The drug was used as a bronchodilator in asthma, as an appetite suppressant, for narcolepsy, and, paradoxically, was discovered in the 1930s to alleviate the hyperactive syndrome in children.
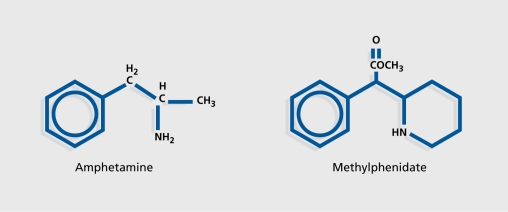
Since the 1930s, amphetamine and its derivatives methylphenidate and pemoline have been used in affective disorders, obsessive-compulsive disorders, and in schizophrenia (for a review see ref 2) (Figure 1.). However, in the 1950s, psychostimulants were replaced by the newly developed antidepressants. Their use was reduced still further in the 1960s, as these drugs were being increasingly abused.3,4 In recent years, the use of psychostimulants in psychiatry has been limited to the therapy of attention deficit, disorder (for a review see ref 5), refractory obesity, and narcolepsy. Most psychiatrists today are not familiar with the potential usefulness of psychostimulants in the therapy of treatmentresistant depression.
Figure 1. Structure of amphetamine and methylphenidate.
Pharmacology
Amphetamine increases the release of biogenic amines, exerts direct agonistic effects on presynaptic central receptors for 5-hydroxytryptamine (5-HT), and has a mild inhibiting effect, on monoamine oxidase.6,7 Thus, from a pharmacological viewpoint, psychostimulants complete and amplify the effect of conventional antidepressants8-14 and are assumed to increase the blood levels of certain antidepressants through their action on hepatic hydroxylation.13
Psychostimulants are rapidly absorbed following oral administration. At standard therapeutic doses (10 to 15 mg for amphetamine and 10 to 60 mg for methylphenidate), peak effects are found 2 to 3 hours after ingestion. Psychostimulants are metabolized by rapid oxidative dcamination to benzoic acid and hippuric acid.
Clinical effects
The greatest improvement reported following treatment with psychostimulants is in motor activity, mood, and psychomotor activity.15-17 An improvement in memory and concentration may be observed, in some cases accompanied by euphoria.18
The onset, of action of psychostimulants is usually observed clinically within 30 minutes to 1 or 2 hours following administration,19-23 and their effects last, about 4 hours.24
Patient response is heterogeneous, with variations in sensitivity due to individual differences in biological and genetic parameters.25 The use of psychostimulants must be carefully monitored.10 Patient response also depends on which type of psychostimulant, is administered, and if no therapeutic effect is observed with one drug, another one may prove effective. Furthermore, patient response to a given psychostimulant may vary from year to year.16 One feature of particular interest is that the response to amphetamines may be predictive of the therapeutic effect, of tricyclic drugs in depressed patients, since both types of drugs have similar mechanisms of action (rapid for the amphetamines, slower for the tricyclics) involving an increase in free norepinephrine levels.19 In contrast, the response to methylphenidate does not appear to be predictive of antidepressant efficacy.26
Side effects
At low doses (2-10 mg per day), amphetamine can induce sleep and libido disturbances as well as nausea, tremor, agitation, and restlessness.
At higher doses (30-60 mg per day), amphetamine may induce anxiety, psychoses, exhaustion symptoms with fatigue and drowsiness after the stimulation phase, prolonged depression, and prolonged hallucinosis27 whereby the individual continues to hallucinate after the drug has been metabolized.28
Extein29 described choreoathetosis after administration of psychostimulants in one patient, probably by potentiation of central dopaminergic activity. Because of the release of norepinephrine and dopamine induced by the psychostimulants, the appearance of stereotypic movements and tics is theoretically possible however, these have only been reported in animal experiments in the literature. Other possible yet rare side effects are hyperthermia and pulmonary hypertension7,30 and, even more rarely, cardiovascular shock and stroke.31 Natenshon24 and Ferguson and Funderburk32 did not observe any effect, on the cardiovascular system in their patients. They found neither advanced age nor cardiac disease to contraindicate the use of psychostimulants.
Wilbur33 noted declining efficacy of stimulants over time; most, other authors, however, reported no evidence of waning of effect in depressed patients treated with 5 to 60 mg methylphenidate for up to 1 year.24 Tolerance was seen only in relation to effects like hyperthermia, hypertonia, and anorexia, but not psychomotor stimulation.31,34,35
It should be stressed that the aforementioned side effects are observed not only in depressed patients, but also in patients treated with psychostimulants for other indications.
Development of dependency or tendency to abuse?
The possible development of dependency and a withdrawal syndrome after withdrawing amphetamines has been a controversial issue. Addiction was reported by Kramer et al3 and Edison,36 and a withdrawal syndrome characterized by apathy, decreased activity, and sleep disturbances with an increase in rapid eye movement (REM) sleep by Oswald and Thacore37 and Watson et al.38 Most studies, however, report, little or no dependence in depressed patients treated with amphetamines (see overview in refs 2 and 23). Psychostimulants may be withdrawn after several weeks of treatment without any danger of recurrence of depression.21 No tolerance or addiction has been reported to develop in geriatric patients. However, recurrence of mild depression, tiredness, and anxiety have been reported on stopping treatment with psychostimulants.39 Development of tolerance or abuse after patients are discharged from hospital is practically never reported.22,24,40
Dosage
The dosage of the psychostimulants must imperatively be individually adjusted. The daily doses usually recommended in treatment-resistant depressed patients range between 2.5 mg41 and 15 mg20 for amphetamine and between 10 and 60 mg for methylphenidate.42
Indications in depressive disorders
Some depressive disorders remain refractory to treatment despite intensive antidepressant therapy with adequate dosages and even combinations of antidepressants.43,44 These cases may benefit from adjuvant treatment with psychostimulants. The mood-elevating effects of the tricyclics, selective serotonin reuptake inhibitors (SSRIs), and monoamine oxidase inhibitors (MAOIs) usually only manifest, after 10 to 12 days. Side effects and drug interactions are quite common with these drugs. Although psychostimulants themselves are not as effective as conventional antidepressants,45,46 they have the dual advantage of a more rapid onset of action and of inducing a lower rate of adverse events.
Because their acute effects develop within less than a few hours,20 they may be used in combination with traditional antidepressants in order to cover the lattcr's therapeutic latency period and potentiate their effect.13,35 In a review of the literature, Chiarello and Cole2 showed that the majority of studies - even though some were methodologically unsatisfactory - reported beneficial effects following administration of psychostimulants in treatment-resistant depression.15,22,31,34,35,47-52 Nevertheless, no significant advantage of psychostimulants over placebo could be demonstrated in any of the placebocontrolled studies. Some authors have reported lack of effect, or even deterioration following the addition of psychostimulants.53-56
Beneficial effects have been described in particular in depression with marked apathy in elderly patients.32,52,57-60 Administration of psychostimulants appears to enhance the efficacy of concomitant (analytically orientated) psychotherapy in elderly patients by facilitating communication and cooperation through their mood-elevating effects.31
Psychostimulants are suggested to be of significant value in the management of depression in the elderly as well as in depressed patients with concomitant somatic disorders,14,21,22,60 and good results have been reported in the treatment of secondary depressions triggered by preexisting somatic diseases.4,21,40,61
Psychostimulants have been shown to be effective in patients with mild depressive symptoms in an outpatient setting.15,55,62
According to Rudolf,49,63 the addition of psychostimulants in patients with treatment-resistant depression receiving conventional antidepressants is superior to electroconvulsive therapy (ECT). Kerenyi et al15 reported methylphenidate to be useful in combination with ECT. Inhibited patients and depressed patients with bipolar disorder seemed to benefit, most, from adjuvant, treatment with psychostimulants.15 The response to psychostimulants in patients suffering from neurotic and agitated depression seems to be less satisfactory. Nevertheless, there is no contraindication to psychostimulants in agitated depression.64
The combination of psychostimulants with tricyclics and MAOIs has been a very controversial issue. Some authors have criticized the combination of psychostimulants and MAOIs on the basis of the possible development of an adrenergic crisis or the serotonin syndrome. The Physicians Desk Reference even warned against such drug combinations in 1983 because of the possibility of hypertensive crises, which, however, were found to be very rare.35
In contrast with the above reports, several series of open clinical trials showed the combination of psychostimulants and MAOIs to be safe (see review in refs 35, 65-67). More recently, authors such as Chiarello and Cole2 and Little68 have stressed the frequent, effectiveness of the combination of psychostimulants and MAOIs in treatment-resistant depression.
Findings from a retrospective study in §5 depressed patients
Subjects and methods
In a retrospective study, we evaluated all the medical records since the 1950s of patients at the Zurich Psychiatric Hospital who had received psychostimulants because of treatment-resistant depression (defined by Woggon44 as lack of improvement, despite treatment with at least two different antidepressants in adequate dosage for more than 4 weeks). A total of 65 patient records were analyzed (20 males and 45 females). The average age of male patients was 50 years, and that of female patients was 55 years. At the time of treatment, the patients were either hospitalized (inpatients) or undergoing ambulatory treatment as outpatients.
The patients who had received psychostimulants were identified from the hospital pharmacy records, which list the names of all patients having received drugs classified as narcotics. In earlier years, classifications of mental diseases such as the International Classification of Diseases (ICD) or Diagnostic and Statistical Manual of Mental Disorders (DSM) were not yet available, and diagnoses were descriptive only. Therefore, the classification in this retrospective study had to be done on a syndrome basis. The types of depression for which the patients had been treated with psychostimulants because of their refractory character were (in order of descending frequency): inhibited depression (50), anxious depression (39), agitated depression (21), depression with somatization (21), neurotic depression (20), bipolar disorder (16), and depressive states in schizoaffective disorders (4) with overlapping in symptomatology.
Because of the small number of subjects (65 patients, 17 treated with amphetamines, 35 with methylphenidate, and 13 treated with both amphetamines and methylphenidate), and because a separate statistical analysis of patients treated with amphetamines and those treated with methylphenidate failed to show any significant difference between both groups, it was decided to subsume treatment with amphetamines and with methylphenidate as “treatment with psychostimulants” for the purpose of the study.
The average total duration of psychopharmacological treatment (conventional antidepressants and psychostimulants) was 128 months (10 years, with a median of 84 months (7 years). Seventeen patients were treated with amphetamine, 35 with methylphenidate, and 13 with both amphetamine and methylphenidate, either concomitantly or one after the other.
Regarding conventional antidepressant therapy, prior to receiving psychostimulant treatment, 3 patients had been administered one, 6 patients two, 10 patients three, 6 patients four, and 39 patients five or more antidepressants at various dosages. In 35 of the 65 patients, additional treatment modalities (such as sleep deprivation therapy, light, therapy, and ECT) had been used. Psychostimulants were given in combination with tricyclic antidepressants in 48 cases, with SSRTs in 35 cases, with MAOIs in 8 cases, with lithium in 35 cases, and with carbamazepine in 22 cases. (Some patients received two or more antidepressants and mood stabilizers, in combination with the psychostimulants.)
Dosage was titrated individually and modified during therapy. Patients treated with amphetamines received an average dosage of between 5 and 10 mg per day, the minimum being between 5 and 10 mg, and the maximum 20 mg per day. The average dosage of methylphenidate was 10 to 20 mg per day, with a minimum of 10 mg, and maximum of 40 mg per day. In 25 (out of 64) cases the dosage was increased, in 14 cases it remained unchanged, in 14 cases it was reduced, and in 11 cases it was discontinued. The average duration of psychostimulant therapy was 46 months (approximately 4 years) in the amphetamine group and 57 months (approximately 5 years) in the methylphenidate group. In most cases the treatment was continuous.
Patient characteristics arc summarized in Table I.
Table I. Retrospective study; patient characteristics (n=65).
| Amphetamine | Methylphenidate | Both | |
| Number of patients | 17 | 35 | 13 |
| Male (n) | 3 | 15 | 2 |
| Female (n) | 14 | 20 | 11 |
| Age in years (median) | 51 | 49 | 51 |
| Age of onset in years (median) | 37 | 37 | 37 |
| Benzodiazepines (n) | 21 | 36 | |
| Psychostimulant therpy in months (mendian) | 46 | 5 | 7 |
| Inhibited/anxious depression (n) | 11 | 25 | 7 |
| Agitated depression (n) | 6 | 10 | 6 |
Results
Thirty-eight patients improved on treatment with psychostimulants, whereas 26 remained unchanged or deteriorated.
It must be pointed out that no rating scales or self -rating scores had been used in the patients, since it was not common in the fifties or earlier to evaluate a patient's condition with scales. Patient, records therefore only allowed the course of the disease to be qualified as “better,” “unchanged,” or “worse.” In this way it could be shown that there was no significant differences between the different, age-groups in terms of outcome (chi-square test, and analysis of variance for nonparametric samples).
Because there was an overlap in the types of depression, we looked at the distribution of patients in terms of response to psychostimulant treatment with respect to syndrome (agitated depression and inhibited/anxious depression), and with respect to diagnosis (unipolar disorder and bipolar disorder) (Table II). The best response to psychostimulant, treatment was seen in the group of inhibited and anxious types of depression (27 out of 42 patients improved). In the group of patients with agitated depression, 11 out of 22 patients were improved. Finally, 8 out of 16 patients with bipolar depression were improved.
Table II. Effects curing treatment with psychostimulants (n=65).
| Better | Unchanged/Worse | Total | |
| Syndrome | |||
| Agitated | 11 | 11 | 22 |
| Inhibited/anxious | 27 | 15 | 42 |
| Diagnosis | |||
| Unipolar | 30 | 18 | 48 |
| Bipolar | 8 | 8 | 16 |
Looking now at improvement, in the course of depression according to the type of treatment the psychostimulant drug was added on to, improvement was noted in 6 out of 8 patients who were treated with a psychostimulant, and an MAOI, in 30 out of 48 patients treated with a psychostimulant and a tricyclic, in 21 out of 35 patients treated with a psychostimulant and an SSRI, in 21 out of 35 patients treated with a psychostimulant and lithium, and in 12 out of 22 patients treated with a psychostimulant, and carbamazepine.
Additional treatment with benzodiazepines was required in 21 out of 30 patients treated with amphetamines and in 36 out of 48 patients treated with methylphenidate (13 patients received both drugs).
Overall, the frequency of adverse events and side effects was higher in patients treated with methylphenidate than in patients treated with amphetamines. However, methylphenidate was prescribed in most cases to outpatients and at a relatively higher dosage. Side effects were reported in 51 out of 65 patients treated with psychostimulants, including nausea and headache in 32 patients, restlessness in 29 patients, agitation in 25 patients, sleep disturbances in 18 patients, and circulatory disorders in 6 patients. In all cases blood pressure remained unchanged before, during, and after treatment with psychostimulants.
It has to be taken into consideration, however, that it was not always possible to differentiate between the side effects attributable to the psychostimulants and those attributable to the antidepressants.
None of the depressed patients developed drug dependency or addictive behavior. To test for this possibility, psychostimulant, treatment was withdrawn, in most patients, at least once during the course of treatment for a period of 2 days, during which the patients experienced apathy and tiredness, but without, developing any craving for psychostimulant or signs of withdrawal.
In the 38 patients who experienced a beneficial effect from treatment with psychostimulants, 35 patients reported an improvement, in energy, 26 in mood, 26 in motor activity, 15 in symptoms of psychomotor retardation, 11 in vigilance, and 7 in social interactions. Negative symptoms did not improve in the 4 patients with schizoaffective disorders.
Discussion
Our study highlights the benefit of the administration of psychostimulants in addition to conventional antidepressants in patients with treatment-resistant depression. These findings are concordant with those of the majority of open studies (see the review of the literature in the first part of this paper). There were no severe side effects and only a low incidence of mild and moderate side effects in the patient population we studied, in agreement with the findings described in the literature. Unlike Kramer et al3 and Edison,36 we found no evidence of drug dependency in our patients.
Some of our patients were suffering from concomitant. somatic illnesses. These patients probably benefited from the treatment, with psychostimulants, as reported by Woods et al22 in their sample of patients with depressive disorders secondary to somatic illnesses.
There were no severe cardiovascular disturbances in our patients.
In several studies in the literature, psychostimulants were used preferentially in elderly persons. In our study, both elderly and younger patients were treated with psychostimulants, with the same positive effect.
No psychoses (as opposed to Lucas and Weiss27) were observed in any of our patients treated with psychostimulants.
Some of the patients of our study (6 out of 8) responded positively to combined treatment with (reversible) MAO-A inhibitors (like moclobemide) and psychostimulants, even though this particular combination is regarded as controversial. The positive effect, of a combination of psychostimulants with tricyclic antidepressants (as recommended by Spencer69 and Woggon70) was confirmed in our study (30 of 48 patients treated with tricyclics and psychostimulants showed improvement). In agreement with Wharton et al13 and Feighner et al,35 we believe that combining a psychostimulant and a tricyclic antidepressant potentiates the action of the latter through an increase in the serum levels of its active metabolites. According to another hypothesis, the beneficial effect could be secondary to an increase in monoamine concentrations in the synaptic cleft.
In our experience, use of psychostimulants in agitated depression may be of benefit, although more rarely so than in inhibited depression, thus confirming the findings of Kerenyi.15 We also agree with Ward and Lampe64 that there is no contraindication to the use of psychostimulants in agitated depressed states. Like Wilbur,33 but in disagreement, with Wheatley,50 we have also used psychostimulants in neurotic depression, again with lower rates of success. Finally, we have found that treatment with psychostimulants in an outpatient clinical setting was possible without any problems in some of our patients, a finding in keeping with previous studies of Kerenyi,15 Rickels et al,62 and Mattes.55
Conclusions
Based on a retrospective study carried out in 65 patients suffering from treatment-resistant depression, we confirm that treatment with psychostimulants in addition to conventional antidepressants has a beneficial effect on the outcome of depression. Not all the patients in our study showed a significant improvement, but the majority (38 out of 65 patients) did. None of the patients developed drug dependency or withdrawal symptoms. The overall incidence and severity of side effects was low. In patients in whom agitation or restlessness developed, a dosage-reduction and/or additional short-term treatment with benzodiazepines proved consistently helpful. Apathy improved in a satisfactory way in most of the patients and in most, cases within the first hours following administration. The rapid onset of action of the psychostimulants has the advantage of covering the therapeutic latency period of conventional antidepressants and potentiating their effect. Psychostimulants should be preferably combined with tricyclic antidepressants. In some cases, an increase in dosage of conventional antidepressants can be avoided by taking advantage of the potentiating and additive effect, of the psychostimulants.
Although adjuvant therapy with psychostimulants in patients suffering from treatment-resistant depression has not yet become established in clinical practice, we believe that it should be tried more often in view of its potential benefits.
For relevant information concerning the review of literature I thank Dr Martin Preisig, from Lausanne
Contributor Information
Gabriele Stotz, Psychiatric University Hospital Munich, Germany.
Brigitte Woggon, Zurich University Psychiatric Hospital, Switzerland.
Jules Angst, Zurich University Psychiatric Hospital, Switzerland.
REFERENCES
- 1.Leake CD. The Amphetamines, Their Actions and Uses. Springfield, III: Thomas, CQ. 1958 [Google Scholar]
- 2.Chiarello RJ., Cole JO. The use of psychostimulants in general psychiatry. A reconsideration. Arch Gen Psychiatry. 1987;44:286–295. doi: 10.1001/archpsyc.1987.01800150110013. [DOI] [PubMed] [Google Scholar]
- 3.Kramer JC., Fischman VS., Littlefield DC. Amphetamine abuse. JAMA. 1967;201:305–309. doi: 10.1001/jama.201.5.305. [DOI] [PubMed] [Google Scholar]
- 4.Ayd FJ. Psychostimulant therapy for depressed medically ill patients. PsychiatrAnn. 1985;15:462–465. [Google Scholar]
- 5.Trott GE. Das Hyperkinetische Syndrom des Kindes- und Jugenda Iters. Therapeutische Mogiichkeiten und deren Evaluation [Hyperkinetic Syndrome in Children and Youths. Therapeutic Possibilities and Their Evaluation]. (Thesis). Wurzburg, Germany; 1991 [Google Scholar]
- 6.Goodman LS., Gilman AG. The Pharmacological Basis of Therapeutics. 8th ed. New York, NY: McGraw-Hill Companies, Inc; 1990 [Google Scholar]
- 7.Forth H., Henschler D., Rummel W. Allgemeine und Spezielle Pharmakologie und Toxikologie. 4th ed. Mannheim, Germany: Bibliographisches Institut-Wissenschaftsverlag; 1983 [Google Scholar]
- 8.Sulser F., Owens ML., Dingell JV. On the mechanism of amphetamine potentiation by desipramine. Life Sci. 1966;5:2005–2010. [Google Scholar]
- 9.Dingell JV., Owens ML., Norvich MR., Sulser F. On the role of norepinephrine biosynthesis in the central action of amphetamine. Life Sci. 1967;6:1155–1162. doi: 10.1016/0024-3205(67)90197-x. [DOI] [PubMed] [Google Scholar]
- 10.Ban TA. The use of the amphetamines in adult psychiatry. Semin Psychiatry. 1969;1:129–143. [Google Scholar]
- 11.Perel JM., Black N., Wharton RN., Malitz S. Inhibition of imipramine metabolism by methylphenidate. Fed Proc. 1969;28:418. [Google Scholar]
- 12.van Praag HM., Schut T., Bosma E., van den Bergh RA. A comparative study of the therapeutic effects of some 4-chlorinated amphetamine derivatives in depressive patients . Psychopharmacologia. 1971;20:66–76. doi: 10.1007/BF00404060. [DOI] [PubMed] [Google Scholar]
- 13.Wharton RN., Perel JM., Dayton PG., Malitz S. A potential clinical use for methylphenidate with tricyclic antidepressants. Am J Psychiatry. 1971;127:1619–1625. doi: 10.1176/ajp.127.12.1619. [DOI] [PubMed] [Google Scholar]
- 14.Naor S., Talmon Y. Combined tricyclic antidepressants and Ritalin in elderly dépressives [in Hebrew]. Harefuah. 1992;123:251–252,307. [PubMed] [Google Scholar]
- 15.Kerenyi AB., Koranyi EK., Sarwer-Foner GJ. Depressive states and drugs. III. Use of methylphenidate (Ritalin) in open psychiatric settings and in office practice. Can Med Assoc J. 1960;83:1249–1254. [PMC free article] [PubMed] [Google Scholar]
- 16.Cameron JS., Specht PG., Wendt GR. Effects of amphetamines on moods, emotions and motivations. J Psychol. 1965;61:93–121. doi: 10.1080/00223980.1965.10544801. [DOI] [PubMed] [Google Scholar]
- 17.Murray JB. Psychophysiological effects of methylphenidate (Ritalin). Psychol Rep. 1987;61:315–336. doi: 10.2466/pr0.1987.61.1.315. [DOI] [PubMed] [Google Scholar]
- 18.Smith RC., Davis JM. Comparative effects of d-amphetamine, l-amphetamine and methylphenidate on mood in man. Psychopharmacology. 1977;53:1–12. doi: 10.1007/BF00426687. [DOI] [PubMed] [Google Scholar]
- 19.Fawcett J., Siomopoulos V. Dextroamphetamine response as a possible predictor of improvement with tricyclic therapy in depression. Arch Gen Psychiatry. 1971;25:247–255. [Google Scholar]
- 20.Kiloh LG., Neilson M., Andrews G. Response of depressed patients to methylamphetamine. Br J Psychiatry. 1974;125:496–499. doi: 10.1192/bjp.125.5.496. [DOI] [PubMed] [Google Scholar]
- 21.Fisch RZ. Methylphenidate for medical in-patients . Int J Psychiatry Med. 1985-1986;15:75–79. doi: 10.2190/fnld-htdm-9lp1-x3y3. [DOI] [PubMed] [Google Scholar]
- 22. Woods SW., Tesar GE., Murray GB., Cassem NH. Psychostimulant treatment of depressive disorders secondary to medical illness. J Clin Psychiatry. 1986;47:12–15. [PubMed] [Google Scholar]
- 23.Satel SL., Nelson C. Stimulants in the treatment of depression: a critical overview. J Clin Psychiatry. 1989;50:241–249. [PubMed] [Google Scholar]
- 24.Natenshon AL. Clinical evaluation of Ritalin. Dis Nerv Syst. 1956;17:392–396. [Google Scholar]
- 25.Silberman EK., Reus VI., Jimerson DC., Lynott AM., Post RM. Heterogeneity of amphetamine. Am J Psychiatry. 1981;138:1302–1307. doi: 10.1176/ajp.138.10.1302. [DOI] [PubMed] [Google Scholar]
- 26.Little KY Amphetamine. Amphetamine, but not methylphenidate, predicts antidepressant efficacy. J Clin Psychopharmacoi. 1988;8:177–183. [PubMed] [Google Scholar]
- 27.Lucas AR., Weiss M. Methylphenidate hallucinosis. JAMA. 1971;217:1079–1081. [PubMed] [Google Scholar]
- 28.Smith DE., Fisher CM. An analysis of 310 cases of acute high-dose metamphetamine toxicity in Haight-Ashbury. Clin Toxicol. 1970;3:117–124. doi: 10.3109/15563657008990106. [DOI] [PubMed] [Google Scholar]
- 29.Extein I. Methylphenidate-induced choreoathetosis. Am J Psychiatry. 1978;135:252–253. doi: 10.1176/ajp.135.2.252. [DOI] [PubMed] [Google Scholar]
- 30.Wilson JD., Braunwald E., Isselbacher KJ., et al. Harrisons' Principles of Internal Medicine, 12th ed. New York, NY: McGraw-Hill Companies, Inc; 1991 [Google Scholar]
- 31.Jacobson A. The use of Ritalin in psychotherapy of depressions of the aged. Psychiatr Q. 1958;32:474–483. doi: 10.1007/BF01563517. [DOI] [PubMed] [Google Scholar]
- 32.Ferguson JT., Funderburk WH. Improving senile behavior with reserpine and Ritalin . JAMA. 1956;160:259. doi: 10.1001/jama.1956.02960390009003. [DOI] [PubMed] [Google Scholar]
- 33.Wilbur DL., McLean AR., Allen EV. Clinical observations on the effect of benzedrine sulfate. JAMA. 1937;109:549–554. [Google Scholar]
- 34.Elizur A., Wintner I., Davidson S. The clinical and psychological effects of pemoline in depressed patients. Int Pharmacopsychiatry. 1979;14:127–134. doi: 10.1159/000468371. [DOI] [PubMed] [Google Scholar]
- 35.Feighner JP., Herbstein J., Damlouji N. Combined MAOI, TCAand direct stimulant therapy of treatment-resistant depression . J Clin Psychiatry. 1985;46:206–209. [PubMed] [Google Scholar]
- 36.Edison GR. Amphetamines: a dangerous illusion. Ann int Med. 1971;74:605–610. doi: 10.7326/0003-4819-74-4-605. [DOI] [PubMed] [Google Scholar]
- 37.Oswald J., Thacore VR. Amphetamine and phenmetrazine addiction: physiological abnormalities in the abstinence syndrome. BMJ. 1963;issue 5354:427–431. doi: 10.1136/bmj.2.5354.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watson R., Hartmann E., Schildkraut JJ. Amphetamine withdrawal: affective state, sleep patterns and MHPG secretion. Am J Psychiatry. 1972;129:263–269. doi: 10.1176/ajp.129.3.263. [DOI] [PubMed] [Google Scholar]
- 39.Bare WW., Lin DVP. Stimulants for the aged. Long-term observations with methylphenidate-vitamine-homone combination. J Am Geriatr Soc. 1962;10:539–544. doi: 10.1111/j.1532-5415.1962.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 40.Fernandez F., Adams F., Holmes VF., Levy JK., Neidhart M. Methylphenidate for depressive disorders in cancer patients. Psychosomatics. 1987;28:455–461 . doi: 10.1016/S0033-3182(87)72476-1. [DOI] [PubMed] [Google Scholar]
- 41.Rudolf GdM. Amphetamine. Lancet. 1965;2:131. [Google Scholar]
- 42.Gerner RH. Systematic treatment approach t depression and treatment resistant de pression. Psychiatric Ann. 1983;13:37–49. [Google Scholar]
- 43.Woggon B. Somatische Therapien: Psychopharmakotherapie [Somatic Therapies: Psychopharmacotherapy]. In: Kisker KP, Lauter H, Meyer JE, Mûller C, Strômgren E, eds. Psychiatrie der Gegenwart . b:Affektive Psychosen. 1987:289. [Google Scholar]
- 44.Woggon B. Psychopharmakologische Behandlung therapieresistenter Depressionen [Psychopharmacological management of treatment-resistant depressions]. Fundam Psychiatrica. 1926;6:210–215. [Google Scholar]
- 45.Overall JE., Hollister LE., Pokorny AD., Casey JF., Katz G. Drug therapy in depressions. Clin Pharmacol Ther. 1961;3:16–22. doi: 10.1002/cpt19623116. [DOI] [PubMed] [Google Scholar]
- 46.Hare EH., Dominiak J., Sharpe L. Phenelzine and dexamphetamine in depressive illness. A comparative trial. BMJ. 1962;1:9–12. doi: 10.1136/bmj.1.5270.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myerson A., Boston MD. Effect of benzedrine sulfate on mood and fatigue in normal and in neurotic persons. Arch Neurol Psychiatry. 1936;36:816–822. [Google Scholar]
- 48.Dub LA., Lurie LA. Use of benzedrine in the depressed phase of the psychotic state. Ohio State Med J. 1939;35:39–45. [Google Scholar]
- 49.Rudolf GdM. The treatment of depression with desoxyephedrine (Methedrine). J Ment Sci. 1949;95:920–929. doi: 10.1192/bjp.95.401.920. [DOI] [PubMed] [Google Scholar]
- 50.Wheatley D. Amphetamines in general practice: their use in depression and anxiety . Semin Psychiatry. 1969;1:163–173. [Google Scholar]
- 51.Cookson J., Silverstone T. The effects of methylamphetamine on mood and appetite in depressed patients. Int Clin Psychopharmacoi. 1986;1:127–133. doi: 10.1097/00004850-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 52.Robin AA., Wisseberg S. Psychostimulants in psychiatry. Can J Psychiatry. 1990;35:3–10. doi: 10.1177/070674379003500102. [DOI] [PubMed] [Google Scholar]
- 53.Robin AA., Wiseberg S. A controlled trial of methylphenidate (Ritalin) in the treatment of depressive states. J Neurol Neurosurg Psychiatry. 1958;21:55–57. doi: 10.1136/jnnp.21.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hare EH., McCance C., McCormick WO. Imipramine and Drinamyl in depressive illness. BMJ. 1964;1:818–820. doi: 10.1136/bmj.1.5386.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mattes JA. Methylphenidate in mild depression: a double-blind controlled trial. J Clin Psychiatry. 1985;46:525–527. [PubMed] [Google Scholar]
- 56.Darvill FT., Woolley S. Double-blind evaluation of methylphenidate (Ritalin) hydrochloride. JAMA. 1959;169:1739. doi: 10.1001/jama.1959.03000320041011. [DOI] [PubMed] [Google Scholar]
- 57.Ferguson JT. Treatment of reserpine-induced depression with a new analeptic: phenilydate. Ann NY Acad Sci. 1955;61:101. doi: 10.1111/j.1749-6632.1955.tb42456.x. [DOI] [PubMed] [Google Scholar]
- 58.Dube AH., Osgood CK., Notkin H. The effects of an analeptic (Ritalin), an ataraxic (reserpine) and a placebo in senile states. J Chron Dis. 1957;5:220–234. doi: 10.1016/0021-9681(57)90137-6. [DOI] [PubMed] [Google Scholar]
- 59.Kaplitz SE. Withdrawn, apathetic geriatric patients responsive to methylphenidate. J Am Geriatr Soc. 1975;23:271–276. doi: 10.1111/j.1532-5415.1975.tb00317.x. [DOI] [PubMed] [Google Scholar]
- 60.Katon W., Raskind M. Treatment of depression in the medically ill elderly with methylphenidate . Am J Psychiatry. 1980;137:963–965. doi: 10.1176/ajp.137.8.963. [DOI] [PubMed] [Google Scholar]
- 61.Kaufmann MW., Murray GB., Cassem NH. Use of psychostimulants in medically ill patients. Psychosomatics. 1982;23:817–819. doi: 10.1016/S0033-3182(82)73080-4. [DOI] [PubMed] [Google Scholar]
- 62.Rickels K., Gingrich RL., McLaughlin FW., et al. Methylphenidate in mildly depressed outpatients. Clin Pharmacol Ther. 1972;13:595–601. doi: 10.1002/cpt1972134595. [DOI] [PubMed] [Google Scholar]
- 63.Rudolf GdM. The treatment of depression with methylamphetamine. J Ment Sci. 1956;4:358–363. doi: 10.1192/bjp.102.427.358. [DOI] [PubMed] [Google Scholar]
- 64.Ward NG., Lampe TH. Atrial of dextroamphetamine in patients with involutional agitated depression. J Clin Psychiatry. 1982;43:35–36. [PubMed] [Google Scholar]
- 65.Schuckit M., Robins E., Feighner J. Tricyclic antidepressants and monoamine oxidase inhibitors. Arch Gen Psychiatry. 1971;24:509–514. doi: 10.1001/archpsyc.1971.01750120025005. [DOI] [PubMed] [Google Scholar]
- 66.Robie TR., Flora A. Antidepressant chemotherapy, 1965. Rapid response to serotonin precursor potentiated by Ritalin. Psychosomatics. 1965;6:351–354. doi: 10.1016/s0033-3182(65)72255-x. [DOI] [PubMed] [Google Scholar]
- 67.White K., Simpson G. Combined MAOI-tricyclic antidepressant treatment. J Clin Psychopharmacoi. 1981;1:264–282. doi: 10.1097/00004714-198109000-00002. [DOI] [PubMed] [Google Scholar]
- 68.Little KY. d-Amphetamine versus methylphenidate: effects in depressed inpatients. J Clin Psychiatry. 1993;54:349–355. [PubMed] [Google Scholar]
- 69.Spencer S. Depression in general practice managment. BMJ. 1965;2:1052–1053. [PMC free article] [PubMed] [Google Scholar]
- 70.Woggon B. Gibt es Antidepressiva, die bei bestimmten Depressionen speziell indiziert sind? [Are there any antidepressant agents that are specially indicated in specific types of depression?] . Schweiz Med Wochenschr. 1993;123:1312–1319. [PubMed] [Google Scholar]