Abstract
The diagnosis of Alzheimer's disease (AD) is a 2-stage process, in stage 1, the dementia syndrome, comprising neuropsychologic and neuropsychiatrie components together with deficits in activities of daily living, is differentiated on clinical grounds from a number of other conditions (delirium, concomitant physical illness, drug treatment normal memory loss, etc), in stage 2, the cause is determined, AD being the most common, followed by vascular dementia, Lewy-body dementia, frontal lobe dementia, and a host of so-called secondary causes. Although a mixed Alzheimer/vascular picture is common, gradual onset of multiple cognitive deficits is typical of AD, while abrupt onset, a fluctuating course, hypertension, and focal neurologic signs suggest vascular dementia, in Lewy-body dementia, memory loss may not be an early feature, and fluctuation can be marked by distressing psychotic symptoms and behavioral disturbance, investigations should be minimally invasive and relatively cheap, confined to routine blood tests, chest x-ray and/or electrocardiogram if clinically indicated, cardiologie or neurologic referral in the presence of cerebrovascular signs, and computed tomography if an intracranial lesion is suspected. Accurate diagnosis enables the clinician to outline the disease course to the family and inform them of genetic implications. Numerous instruments for assessing cognitive function, global status, psychiatric well-being, and activities of daily living are briefly reviewed.
Keywords: Alzheimer's disease, vascular dementia, Lewy-body dementia, diagnostic instrument, genetics
Abstract
El diagnóstico de la Enfermedad de Alzheimer (EA) es un proceso en dos etapas. En la primera etapa el síndrome demencial se traducirá clínicamente en compromiso neuropsicológico y neuropsiquiátrico junto a los déficits en las actividades de la vida diaria y es posible diferenciarlo -en sus manifestaciones clínicas- de muchas otras condiciones (delirium, enfermedades físicas concomitantes, tratamientos medicamentosos, pérdidas de memoria normales, etc.). En la segunda etapa es posible determinar su causa; la EA es la etiología más común, seguida por la demencia vascular, la demencia por cuerpos de Lewy, la demencia del lóbulo frontal y un conjunto de las así denominadas causas secundarias. Aunque es común encontrar un cuadro en que se mezcla la E.A con causas vasculares, lo más típico de la EA es la aparición gradual de los déficits cognitivos múltiples. En cambio, la instalación brusca de los síntomas, un curso fluctúante, hipertensión arterial y signos neurológicos focales son más sugerentes de una demencia vascular. En la demencia por cuerpos de Lewy la pérdida de memoria no aparece necesariamente en la primera etapa y puede haber fluctuationes, marcadas por síntomas psicóticos y trastornos de conducta. Las investigaciones deberían ser mínimamante invasoras y relativamente baratas, enfocadas a exámenes de laboratorio de rutina, radiografías de tórax y/o electrocardiograma si existe alguna indicación clínica. En caso de presentarse signos cerebrovasculares se solicitará la evaluación cardiológica o neurológica; la tomografía computarizada cerebral se solicitará ante la sospecha de una lesión intracraneal. Un diagnóstico preciso de EA habilita al clínico para delinear el curso de la enfermedad a los familiares e informarles acerca de las implicancia genéticas. Además se revisan brevemente diversos instrumentos para evaluar la función cognitiva, el estilo global, el bienestar psiquiátrico y las actividades de la vida diaria.
Abstract
Le diagnostic de la maladie d'Alzheimer (MA) se fuit en deux étapes. En premier lieu, le diagnostic du syndrome de démence, avec ses deux composantes neuropsychologique et neuropsychiatrique, responsable de déficits dans les activités de la vie quotidienne, dont les caractéristiques cliniques permettent de le différencier d'autres pathologies (délire, maladie concomitante, intoxication médicamenteuse, perte de mémoire banale, etc.). La seconde étape est celle de la détermination de la cause, la plus fréquente étant la MA, suivie par la démence vasculaire, la maladie des corps de Lewy, la démence frontale et toute une série de causes dites secondaires. Bien qu'un tableau mixte Alzheimer/pathologie vasculaire soit fréquent, un début progressif marqué pur de multiples déficits cognitifs est caractéristique de la MA, alors qu'un début brusque, un déroulement fluctuant, une hypertension et des signes neurologiques focaux sont en faveur d'une démence vasculaire. Dans la démence des corps de Lewy, la perte de mémoire peut ne pas être précoce et les variations observées comportent des symptômes psychotiques sévères et des troubles du comportement. On se limitent pour les investigations et des examens peu invasifs et peu coûteux comme des examens sanguins courants, une radio pulmonaire et/ou un ECG selon la clinique, une consultation cardiologique ou neurologique en présence de signes cérébro-vasculaires et un scanner cérébral en cas de suspicion de lésions intrucrâniennes. Un diagnostic exact permet au médecin d'informer la famille du déroulement prévisible de la maladie et de ses implications génétiques. Nous passerons brièvement en revue les nombreux tests qui permettent d'évaluer la fonction cognitive, l'état général, l'état mental et les activités de la vie quotidienne.
Clinical assessment of dementia
The diagnosis of Alzheimer's disease (AD) is essentially a two-stage process. First, a diagnosis of dementia is made, the main conditions from which it should be differentiated being delirium, depression, concomitant physical illness, drug treatment, learning disability, the effects of a severely impoverished environment, and the normal memory loss that accompanies aging. Dementia is a clinical syndrome, and determining the cause of the syndrome is the second stage. The commonest cause is AD, followed by vascular dementia, Lewy-body dementia, and frontal lobe dementia. There are many so-called secondary causes of dementia, some of which are treatable. The clinical syndrome of dementia has three primary expressions. First, a neuropsychological element consisting of amnesia (loss of memory); aphasia (either a receptive aphasia or expressive aphasia, the latter being more apparent in conversation, and nominal aphasia tested by direct questioning of naming of objects); apraxia (the inability to carry out tasks despite intact sensory and motor nervous systems, manifest in dementia most usually by an inability to dress often described as putting on a shirt or coat back to front, or the inability to use a knife and fork correctly; and agnosia (the inability to recognize things such as one's own mirror reflection or a family member - remember this is different from forgetting the name of someone).
Second, a neuropsychiatrie component with associated symptoms such as psychiatric disturbances and behavioral disorders, which are present in a substantial proportion of patients. These symptoms have been described in a number of ways - noncognitive features, neuropsychiatrie features, and, more recently, behavioral and psychological symptoms of dementia (BPSD). The commonest are (approximate frequencies in brackets): depression (up to 66% at some point during their dementia); paranoid ideation (30%); misidentifications (20%, usually based on agnosia, often manifest as a failure to recognize others, sometimes coupled with the delusional belief that people or objects have been duplicated); hallucinations (15%, most commonly auditory, suspect an intercurrent delirium or Lewy-body dementia if persistent visual hallucinations are present); aggression (20%); and wandering (20%). Third, deficits in activities of daily living. Towards the later stages of dementia, these are manifest by obvious problems in dressing, eating, and going to the toilet (basic activities of daily living). In the early stages, they may manifest by a failure to wash or dress to a person's usual standard, and, in people living alone, self -neglect of the diet can lead to weight loss, while neglect of household tasks lead to comments about cleanliness of the house (instrumental activities of daily living).
| FEATURES OF DEMENTIA |
| • Neuropsychologic: amnesia, aphasia, apraxia, agnosia |
| • Neuropsychiatric: psychiatric disorders (eg, delusions, depression, hallucinations) behavioral disturbances (eg, aggression, agitation) |
| • Activities of daily living (basic and instrumental) |
This triad of presentation is common to all types of dementia, the differentiation being based on the clinical presentation, the presence of other features, and other aspects of the history and examination.
Clinical presentation of dementia
Patients with dementia tend to come to the attention of specialist services only when symptoms begin to interfere with their lives and are affecting everyday functioning. By then, the patient is often not able to provide an accurate history and may deny there is any problem. A history from an informant is essential. Dementia can have an apparent sudden onset, coinciding with the death of a spouse, a move from a familiar neighborhood, or a foreign holiday, but such an impression may have merely brought the condition to the notice of others or have precipitated a decline because of a sudden change in the environment. Support of the patient by a spouse or other carer can minimize problems that become evident to others only after a bereavement. A thorough history from an informant usually uncovers the truth. Failing cognitive function can be minimized by adherence to rigid routines, which are disrupted when the sufferer moves away from familiar surroundings.
| PRESENTATION OF DEMENTIA |
| • Often noticed by others |
| • Often precipitated by another event, eg, holiday or house move |
| • Death of a spouse may reveal previously unnoticed problems |
| • Informant history essential |
Symptoms of Alzheimer's disease
The first symptoms of AD are usually cognitive in nature, and memory impairment and disorientation in time and place are probably the commonest manifestations. Short-term memory is particularly impaired and the significance of such a change is sometimes not fully appreciated by families and others (including professionals), often being put down to a normal age-related decline. Changes in personality may, retrospectively-, be regarded as one of the earliest signs of dementia and are well documented in the later stages. Blessed et al1 described eleven types of personality change which are summarized below Consensus criteria for the diagnosis of Alzheimer's disease have been published and widely validated.2
| PERSONALITY CHANGES IN DEMENTIA |
| • Increased rigidity |
| • Increased egocentricity |
| • Impairment of regard for the feelings of others |
| • Coarsening of affect |
| • Impairment of emotional control |
| • Hilarity in inappropriate situations |
| • Diminished emotional responsiveness |
| • Sexual misdemeanor |
| • Hobbies relinquished |
| • Diminished initiative or growing apathy |
| • Purposeless hyperactivity |
Symptoms of vascular dementia
Differentiation between AD and vascular dementia can be difficult because the two conditions often coexist. The onset of vascular dementia is usually sudden and can sometimes follow a clearly definable cerebrovascular accident. The course is usually described as a stepwise progression with episodes of confusion with fluctuations in the degree of cognitive impairment.
| DIAGNOSTIC CRITERIA FOR DEMENTIA OF THE ALZHEIMER TYPE |
| • Development of multiple cognitive deficits with both: |
| • Memory impairment |
| • One or more of amnesia, apraxia, agnosia, |
| • Gradual onset of symptoms |
| • Symptoms interfere with work and social activities |
| • Absence of any other illness (systemic or cerebral) causing the dementia |
There is more lability of mood and a greater tendency towards depression and anxiety than is generally seen in AD. Very occasionally, small lacunar infarcts can be associated with gradual mental deterioration without focal signs. The patchy nature of the psychological deficits in contrast to the global impairment of AD is said to distinguish between the two types of dementia, with relative preservation of personality and insight in vascular dementia.
The key features that distinguish between AD and vascular dementia were described by Ilachinski3 and made up into a checklist from which a score (the Ischemic or Ilachinski score) is derived. The original score was based on features of vascular dementia in a textbook of psychiatry and studies of the cerebral blood flow in patients with dementia.
| FEATURES SUGGESTIVE OF VASCULAR DEMENTIA (NOTIONAL WEIGHTING IN BRACKETS) |
| • Abrupt onset (2) |
| • Stepwise deterioration (1) |
| • Fluctuating course (2) |
| • Nocturnal confusion (1) |
| • Preserved personality (1) |
| • Depression (1) |
| • Somatic complaints (1) |
| • Emotional incontinence (1) |
| • Hypertension (1) |
| • History of strokes (2) |
| • Associated atherosclerosis (1) |
| • Focal neurological signs (2) |
| • Focal neurological symptoms (2) |
| DIAGNOSTIC CRITERIA FOR VASCULAR DEMENTIA |
| • Presence of dementia |
| • Focal neurological signs and symptoms or neuroimaging evidence of cerebrovascular disease judged to be etiologically related to the dementia |
| • Symptoms not occurring in the course of delirium |
Patients from the initial study group were relatively young and more mildly affected by their illness than are patients seen in most old-age psychiatry services. A bimodal distribution of scores was found and suggested that patients with a score below 4 had a dementia of the Alzheimer type and those having a score of 7 or above a vascular dementia.
Patients scoring between 4 and 7 were thought to have a mixed picture. The key features of vascular dementia are shown in Table I4-6 More recently, the validity of using the Ilachinski score to differentiate between vascular dementias and other types of dementias has been questioned. The Ilachinski score has been criticized as not being sufficiently sensitive. Moreover, higher scores on the Ilachinski do not mean that a diagnosis of vascular dementia is more likely, and the checklist does not take into account results from neuroradiological examinations. Infarctions are common in older people, including those with AD, and thus a mixed picture is common. The features that have been found to be most accurate in differentiating vascular- and Alzheimer-type dementia include neurological signs and symptoms, history of strokes, hypertension, and abrupt onset.7 There are two sets of diagnostic criteria for vascular dementia and these are summarized in Table I.
Table 1. Key features of vascular dementia (VaD) according to the criteria of ADDTC (Alzheimer's Disease Diagnostic and Treatment Centers) and NIND-AIREN (National Institute of Neurological Disorders and Stroke-Association Internationale pour la Recherche et l'Enseignement en Neurosciences). CT, computed tomography; CVD, cerebrovascular disease; MRI, magnetic resonance imaging; Tl, thallium. Adapted from ref 4: Amar K, Wilcock G, Scott M. The diagnosis of vascular dementia in the light of the new criteria. Age Ageing. 1996;25:51-55.
| Key features of VaD | ADDTC Criteria4 | NINDS-AIREN Criteria5 |
| Dementia definition | Global deterioration from previous level of function sufficient to interfere with the patient's life | Impairment of memory plus at least two other areas of cognitive domains (not due to the physical effects of stroke alone) sufficient to interfere with the patient's life |
| Probable VaD | Requires all of the following: | Requires all of the following: |
| 1. Dementia | 1. Dementia | |
| 2. Evidence of two or more strokes by | 2. CVD; focal signs on examination + evidence of relevant | |
| history, neurological signs, and/or | CVD by brain imaging (CT/MRI) | |
| neuroimaging, or a single stroke with a | 3. Relationship between the above two disorders, | |
| clear temporal relationship to the | manifested by one or more of the following: | |
| onset of dementia | • dementia onset within 3 months of a stroke | |
| 3. Evidence of at least one infarct | • abrupt deterioration in cognitive functions, | |
| outside the cerebellum by CT or Tl-weighted MRI | or fluctuating stepwise course | |
| Possible | 1. Dementia and | May be made in the presence of dementia and focal |
| 2. One or more of the following: | neurological signs in patients with: | |
| • History or evidence of a single stroke | 1 . No evidence of CVD on neuroimaging; or | |
| without a clear temporal relationship | 2. In the absence of clear temporal relationship between | |
| to dementia onset, or | stroke and dementia; or | |
| • Binswanger's disease that includes all the following: | 3. In patients with subtle onset and variable course of cognitive deficit and evidence of CVD | |
| (i) early onset of urinary incontinence or gait disturbance; | ||
| (ii) vascular risk factors; | ||
| (iii) extensive white matter changes on neuroimaging |
Symptoms of Lewy-body dementia
Lewy-body dementia is characterized by a fluctuating course with distressing psychotic symptoms and marked behavioral disturbance interspersed with periods of lucidity when the degree of cognitive impairment seems relatively- minor in relation to the severity of the behavioral disturbance. Consensus criteria have been agreed that incorporate these elements and are summarized below.8
| CLINICAL FEATURES OF LEWY-BODY DEMENTIA |
| • Progressive cognitive decline interfering with social or occupational functioning; memory loss may not be an early feature |
| • One or two features of: |
| - Fluctuating cognition with pronounced variation in attention and alertness |
| - Recurrent visual hallucinations |
| - Spontaneous motor features of parkinsonism |
Assessment of dementia
The aim of investigations is to establish a diagnosis and to detect the presence of coexisting disorders. An accurate diagnosis makes appropriate discussion of management and prognosis with the patient and their family. A diagnosis of AD will arouse anxieties in families about the genetic implications. Differentiating between AD and vascular dementia allows the clinician to give the family information about the course of the illness.
The most important investigation is obtaining a full history from the patient together with further information from suitable informants such as family members, and will include the family doctor who is an essential source of information about the patient's family history, past medical and personal history, premorbid personality, social circumstances, and dynamics of family relationships.
Discussion with a reliable informant will quickly establish the onset and duration of the presenting problem. Difficulties with memory and changes in personality are universal. Problems encountered with hobbies, such as following a complicated knitting pattern or playing bridge, may be the first change noted. Knowledge of the course of the illness is important in distinguishing vascular dementia from AD. Evidence of psychotic symptoms such as hallucinations or delusions can be obtained from family members.
Examination of the mental state will show evidence of any self-neglect, physical illness may be apparent, and disinhibited or inappropriate behavior as might agitation or retardation indicating depression. Guarded or hostile behavior may indicate underlying paranoid ideas. Poor attention span (indicating clouding of consciousness) can be apparent and helpful in differentiating delirium from dementia.
The patient's speech will reveal evidence of aphasia or dysarthria. Abnormalities of speech seen in advanced dementia include perseveration (the patient continues to give the answer to the previous question in response to new questions), palilalia (when the last word of a question is repeated with increasing frequency), logoclonia (when the last syllable is repeated), and logorrhea (a meaningless outpouring of words). The patient may echo the examiner's speech (echolalia) or actions (echopraxia). The content of thought is often impoverished in dementia, but careful questioning will reveal the presence of delusions or depressive ideas and the patient may elaborate on psychotic experiences. Affective symptoms are often found in association with dementia and may be the presenting feature - agitation, anxiety, irritability are pointers. Disorders of perception occur frequently in people with dementia, and features suggestive of visual or auditory- hallucinations will be apparent from the history - it is not uncommon to see a person hallucinating in the presence of the examiner. Specific questioning will reveal psychotic symptoms such as paranoid ideas or misidentifications.
| MAIN FEATURES OF MENTAL STATE EXAMINATION |
| • Observe for agitation, retardation, self-neglect |
| • Enquire about symptoms of depression |
| • Enquire about psychotic symptoms |
| • Observe any obvious manifestations of physical illness |
| • Carry out cognitive function tests |
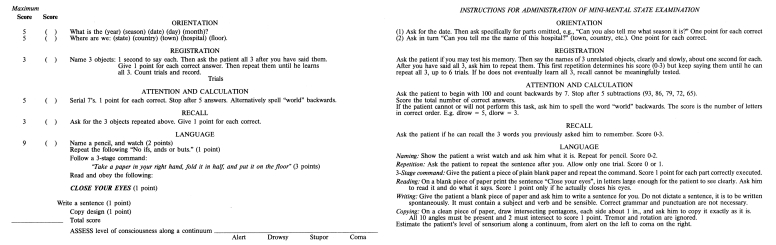
Assessment of cognitive function is greatly aided by using a standard test such as the Mini-Mental State Examination (MMSE).9 The MMSE is scored out of 30 points, of which 10 are given for orientation in time and place and the remainder for tests of attention, registration, recall, language, manipulating information, and praxis. It has been suggested that a cutoff of 23 or 24 on the MMSE is a satisfactory - discriminator between cognitive dysfunction and normality. The MMSE is a useful screening instrument in clinical assessment, but is not a substitute for a full history and mental state examination.(Figure 1). The MMSE is a useful screen in patients referred with a possible dementia. It is quick and easy to complete and sensitive to changes over time, with an expected decline of approximately 3 points each year in a patient with AD.
Figure 1. Mini-Mental State (M.F. Folstein). Reproduced from ref 9: Folstein MF, Folstein SE, McHugh PR. Mini-Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psych/atr fies. 1975;12:189-198. Copyright (c) 1975, Elsevier Science Ltd.
A physical examination should be carried out with specific reference to the central nervous system. High blood pressure and focal neurological signs indicate vascular disease. Assessment of vision and hearing is important as impairments may exaggerate cognitive dysfunction. With regard to investigations, there are some that most doctors would recognize as being essential and others that depend on personal experience and, to a certain extent, local availability. Debate surrounds which screening tests are necessary, and some people argue that the low yield of treatable causes of dementia makes such tests superfluous. Investigations that are most useful are minimally invasive and relatively cheap. A standard screen would include full blood count, erythrocyte sedimentation rate, serum B12 and folate, urea and electrolytes, liver function tests, thyroid function tests, and, if there are atypical or unusual features, serological tests for syphilis. More detailed investigation by a cardiologist or physician may be indicated in patients with cere-brovascular disease in order to try and prevent further strokes. Chest x-ray and an electrocardiogram are indicated if suggested by abnormalities on clinical examination. Lumbar puncture is rarely carried out, but is indicated if there is any evidence of infection or encephalitis. Computed tomography scanning is the radiological investigation of choice to exclude intracranial lesions, with magnetic resonance imaging indicated for a more detailed assessment of cerebral structures. Single photon emission computed tomography can reveal deficits in blood flow and is particularly helpful in diagnosing frontal lobe dementia. Electroencephalography is sensitive to the confirmation of the diagnosis of delirium.
| USEFUL INFORMATION FROM AN INFORMANT REGARDING DEMENTIA |
| • Onset of illness: gradual or sudden |
| • First symptoms |
| • Amount of social support |
| • Presence of psychotic symptoms |
| ASSESSMENT INSTRUMENTS USEFUL IN DEMENTIA |
| • Cognitive function |
| - Mini-Mental State Examination (MMSE) |
| - Clock Drawing Test |
| • Global assessment |
| - Clinical Dementia Rating |
| - Global Deterioration Scale |
| • Psychiatric symptoms |
| - Cornell Scale for Depression in Dementia |
| - Neuropsychiatrie Inventory |
| • Activities of daily living |
| - Bristol Activities of Daily Living scale |
| - Disability Assessment of Dementia |
Assessment instruments for dementia
A number of different instruments have been developed to assess various aspects of dementia. A selection is summarized below, with a more extensive range available in Burns et al.10
Cognitive function
Mini-Mental State Examination (MMSE) 9: this is the most widely used test of cognitive function. It is scored out of 30, and tests the domains of orientation, language, writing, memory, and praxis. It is reproduced in Table II.
-
Standardized Mini-Mental State Examination (SMMSE)11: this is a standardized version of the Mini-Mental State Examination, which comes with complete rating instructions leading to slightly improved validity.
Abbreviated Mental Test Score (AMTS)12 this is a much briefer screening tool, scored out of 10, which tests only orientation and memory.
Alzheimer's Disease Assessment Scale (ADAS)13: this is now a standard cognitive scale used in drug trials. It assesses a number of cognitive functions including memory, language, and practice, and also has a section devoted to noncognitive features.
Clock Drawing Test (CDT)14-16: this is a relatively new development, is very easy to administer, and is very popular in primary care because of its simplicity.
Global measures
Clinical Dementia Rating (CDR)17,18: this is probably the most widely used global scale to give an overall severity rating in dementia, ranging from 0 (none), 0.5 (questionable dementia), through mild and moderate to severe dementia. Each is rated in 6 domains: memory, orientation, judgement and problem solving, community affairs, home and hobbies, and personal care.
Global Deterioration Scale (CDS)19: this consists of the description of 7 stages of dementia from 1 (normal) to 7, where all verbal ability is lost. The scale has been used extensively and validated with postmortem findings.
Psychopathology
Cornell Scale for Depression in Dementia (CSDD)20: this is a 19-item scale, which specifically assesses depression in people with dementia in 5 main domains: moodrelated signs, behavioral disturbance, physical signs, cyclic functions, and ideation disturbance. A mixture of informant-rated and observational ratings makes it ideal for the assessment in patients with cognitive impairment where information from the patient might not always be available. A score of 8 or above suggests significant depressive symptoms.
BEHAV-AD21: this is a 25-item scale, which measures many of the psychiatric symptoms and behavioral disturbances associated with dementia. They are rated on a 3 -point scale, and a second part of the scale is a global rating of the severity of the symptoms, the BEHAV-AD is particularly useful in the assessement of patients in drug trials.
Neuropsychiatrie Inventory (NPI)22: 12 behavioral areas are assessed in the NPI (delusions, hallucinations, agitation, depression, anxiety, euphoria, apathy, disinhibition, irritability, aberrant motor behavior, nighttime behaviors, and appetite/eating disorders), each of which is rated on a 4-point scale of frequency and 3-point scale of severity. Distress in carers is also measured.
MOUSEPAD23: this is based on the longer Present Behavioral Examination and measures a number of behavior and psychiatric symptoms, with particular reference to their development over the life of the dementia syndrome.
Functional ability
Bristol Activities of Daily Living Scale (DADLS)24: this is a 20-item scale rated on a 5-point severity looking at basic activities of daily living (eg, feeding, eating, and toileting) and instrumental activities of daily living (which refer to the performance of more complex tasks such as shopping, traveling, answering the telephone, and handling finances).
Interview for Deterioration in Daily living activities in Dementia (IDDD)25: this contains 33 self-care items rated on a 4-point scale and has been used extensively to assess the effects of drugs.
Disability Assessment for Dementia (DAD)26: a rating of activities of daily living in dementia separating them into the different areas of initiation, planning and organization, and affective performance; basic activities and instrumental of activities daily living are assessed.
Alzheimer's Disease Functional Assessment and Change Scale (ADFACS)27: this is an 18-item scale looking at a wide range of basic activities and instrumental activities of daily living.
Conclusion
The initial assessment and investigation of a person with dementia is particularly challenging and requires a systematic approach. It is a two-stage process, first with the diagnosis of dementia, and second discovering the cause of the dementia. Most information can be obtained by simple observation and examination of the mental state, and the major types of dementia can be delineated in this way. It is usually necessary to perform a number of relatively noninvasive investigations. There are a number of standard scales that can be used in the documentation of various features of dementia.
Selected abbreviations and acronyms
- ADAS
Alzheimer's Disease Assessment Scale
- ADFACS
Alzheimer's Disease Functional Assessment and Change Scale
- AMTS
Abbreviated Mental Test Score
- BADLS
Bristol Activities of Daily Living Scale
- BEHAV-AD
Behavioral symptoms in Alzheimer's disease (scale)
- CDR
Clinical Dementia Rating
- CDT
Clock Drawing Test
- CSDD
Cornell Score for Depression in Dementia
- DAD
Disability Assessment for Dementia
- GDS
Global Deterioration Scale
- IDDD
Interview for Deterioration in Daily living activities in Dementia
- MMSE
Mini-Mental State Examination
- MOUSEPAD
Manchester and Oxford Universities Scale for the Psychopathological Assessment of Dementia
- NPI
Neuropsychiatrie Inventory
- SMMSE
Standardized Mini-Mental State Examination
REFERENCES
- 1.Blessed G., Tomlinson B., Roth M. The association between quantitative measures of dementing and senile change in cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 2.McKhann G., Drachman D., Folstein M., Katzman R., Price D., Stadlan E. Clinical Diagnosis of Alzheimer's Disease: Report of the NINCDS-ADRDA workgroup under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 3.Hachinski VC., lliff LD., Zilkha E., et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32:632–637. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- 4.Amar K., Wilcock G., Scott M. The diagnosis of vascular dementia in the light of the new criteria. Age Ageing. 1996;25:51–55. doi: 10.1093/ageing/25.1.51. [DOI] [PubMed] [Google Scholar]
- 5.Chui H., Victoralt J., Margolan D. Criteria for the diagnosis of ischaemic vascular dementia proposed by the State of California Alzheimer's Disease Diagnostic and Treatment Centers. Neurology. 1992;42:473–480. doi: 10.1212/wnl.42.3.473. [DOI] [PubMed] [Google Scholar]
- 6.Roman G., Tatemichi T., Erkinjuntti T., et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250–260. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 7.Burns A., Howard R., Pettit W. A Medical Companion. Oxford, UK: Blackwell Science; 1995 [Google Scholar]
- 8.McKeith IG., Galasko D., Kosaka K., et al. Consensus guidelines for the clinical and pathologie diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996;47:1113–1124. doi: 10.1212/wnl.47.5.1113. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF., Folstein SE., McHugh PR. Mini-Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Burns A., Lawlor B., Craig S. Assessment Scales in Old Age Psychiatry. London, UK: Martin Dunitz; 1999 [Google Scholar]
- 11.Molloy D., Alemayehu E., Roberts R. Reliability of a standardized Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. Am J Psychiatry. 1991;148:102–105. doi: 10.1176/ajp.148.1.102. [DOI] [PubMed] [Google Scholar]
- 12.Hodkinson HM. Evaluation of a mental test score or assessment of mental impairment in the elderly. Age Ageing. 1972;1:233–238. doi: 10.1093/ageing/1.4.233. [DOI] [PubMed] [Google Scholar]
- 13.Rosen WG., Mohs RC., Davis KL. A new rating scale for Alzheimer's disease. Am J Psychiatry. 1984;141:1356–1364. doi: 10.1176/ajp.141.11.1356. [DOI] [PubMed] [Google Scholar]
- 14.Brodaty H., Moore CM. The Clock Drawing Test for dementia of the Alzheimer's type: a comparison of three scoring methods in memory disorders clinic. Int J Geriatr Psychiatry. 1997;12:619–627. [PubMed] [Google Scholar]
- 15.Shulman K., Shedletsky R., Silver I. The challenge of time. Clock drawing and cognitive function in elderly. Int J Geriatr Psychiatry. 1986;1:135–140. [Google Scholar]
- 16.Sunderland T., Hill J., Mellow A., et al. Clock drawing in Alzheimer's disease. J Am Geriatr Soc. 1989;37:725–729. doi: 10.1111/j.1532-5415.1989.tb02233.x. [DOI] [PubMed] [Google Scholar]
- 17.Hughes C., Berg L., Danzec RW., Coban L., Martin R. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;145:66–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 18.Morris J. The CDR: current version and scoring rules. Neurology. 1993;43:2412–2413. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 19.Reisberg B., Ferris SH., DeLeon MJ., Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139:1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 20.Alexopolous G., Abrams R., Young R., Shamoian C. Cornell Scale for Depression in Dementia. Biol Psychiatry. 1998;23:271–284. doi: 10.1016/0006-3223(88)90038-8. [DOI] [PubMed] [Google Scholar]
- 21.Reisberg B., Borenstein J., Salob SP., Ferns SH., Franssen E., Georgotas A. Behavioural Symptoms in Alzheimer's disease. Phenomenology and treatment. J Clin Psychiatry. 1987;48(suppl 5):9–15. [PubMed] [Google Scholar]
- 22.Cummings JL., Mega M., Gray K., Rosenberg-Thompson S., Carusi DA., Gornbein J. The Neuropsychiatrie Inventory - comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–2314. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 23.Allen NHP., Goredon S., Hope T., Burns A. Manchester and Oxford Universities Scale for the Psychopathological Assessment of Dementia (MOUSEPAD). Br J Psychiatry. 1996;169:293–307. doi: 10.1192/bjp.169.3.293. [DOI] [PubMed] [Google Scholar]
- 24.Bucks R., Ashworth D., Wilcock G., Siegfrid K. Assessment of activities of daily living in dementia. Age Ageing. 1996;25:113–120. doi: 10.1093/ageing/25.2.113. [DOI] [PubMed] [Google Scholar]
- 25.Teunisse S., Derix MMA., Van Crevel H. Assessing the severity of dementia - patient and caregiver. Arch Neurol. 1991;48:274–277. doi: 10.1001/archneur.1991.00530150042015. [DOI] [PubMed] [Google Scholar]
- 26.Galineas I., et al. Development of a functional measure for persons with Alzheimer's disease. Am J Occup Ther. 1999 doi: 10.5014/ajot.53.5.471. [DOI] [PubMed] [Google Scholar]
- 27.Galasko D., Bennett D., Sanor M., et al. An inventory to assess activities of daily living for clinical trials in Alzheimer's disease. Alzheimer Dis Assoc Disord. 1997;11(suppl 2):S33–39. [PubMed] [Google Scholar]