Abstract
Screening for preschizophrenia in the general population with the aim of preventing transition to full-blown illness is an epidemiological impossibility because a rare disease cannot be predicted. The lack of specificity resulting in abundance of false-positives can be remedied in part by using much more restrictive screening criteria that combine several indicators of risk for transition to schizophrenia. Raising the specificity (reducing the false-positives), however, can only be done at the expense of sensitivity (increasing the false-negatives). The most commonly used strategy to raise specificity is the sample enrichment strategy. This involves the creation of samples enriched with schizophrenia risk by selectively filtering at-risk people out over a range of consecutive referral processes starting in the general population, through to general practioners, mental health services, and the early detection clinic. However, improvements in specificity obtained by the sample enrichment strategy should not be attributed to the use of some predictive instrument that supposedly identifies high-risk individuals. The epidemiologically and ethically most viable way for screening and early detection is to selectively increase the permeability of the filters on the pathway to mental health care. This will occasion samples of help-seekers enriched with schizophrenia risk at the level of mental health services (thus reducing false-positives), while at the same time making an attempt to "attract" as many detectable schizophrenia prodromes as possible through the filters along the pathway to mental health care (thus reducing false-negatives). Early psychosis research has yielded some useful suggestions in that it is becoming increasingly clear that it is not just psychosis itself, but rather the clinical context of the psychotic experience that determines risk for transition to schizophrenia. Thus, risk for transition to full-blown psychotic disorder is to a large degree determined by size of psychosis "load," comorbid distress and depression, cannabis use, cognitive ability, and subjective reports of impairment and coping. Making a diagnosis of psychotic disorder is not an exact science: it involves an arbitrary cutoff imposed on dimensional variation of psychopathology and need for care over time. Gaining insight into the cognitive and biological factors that drive the dimensional variation, including therapeutic interventions, is arguably more useful than sterile dichotomous prediction models.
Keywords: prediction, screening, schizophrenia, psychotic disorder, specificity, sensitivity, sample enrichment strategy
Abstract
La selección de sujetos pre-esquizofrénicos en la población general con el objetivo de prevenir la transición hacia la enfermedad totalmente constituída constituye una imposibilidad epidemiológica dado que una enfermedad poco frecuente no se puede predecir. La falta de especificidad, que da origen a gran cantidad de falsos positivos, puede ser remediada en parte al utilizar criterios de selección mucho más restrictivos que combinen algunos indicadores de riesgo para la transición hacia la esquizofrenia. Sin embargo, el aumento de la especificidad (reducción de falsos positivos) sólo puede realizarse a expensas de la sensibilidad (aumento de falsos negativos). La estrategia más comúnmente utilizada para aumentar la especificidad es el enriquecimiento de la muestra. Esta implica la creación de muestras enriquecidas con pacientes con riesgo de esquizofrenia mediante la filtración selectiva de sujetos con riesgo a partir de una serie de procesos de derivación consecutiva que se inician en la población general, a través de médicos generales, servicios de salud mental y clínicas para la detección precoz. Sin embargo, un aumento en la especificidad obtenido mediante la estrategia de enriquecimiento de la muestra no debe ser atribuido al empleo de algún instrumento predictor que presuntamente identifique individuos con alto riesgo. La forma de selección y detección precoz epidemiológica y éticamente más viable, es el aumento selectivo de la permeabilidad de los filtros en el camino hacia la atención en salud mental. Esto generará muestras de buscadores de ayuda enriquecidas con pacientes con riesgo de esquizofrenia a nivel de los servicios de salud mental (reduciendo así los falsos positivos) y al mismo tiempo se intentará "atraer" en cuanto sea posible a pacientes con pródromos esquizofrénicos detectables mediante filtros a lo largo del camino hacia la atención en salud mental (reduciendo así los falsos negativos). La investigación en psicosis precoces ha entregado algunas sugerencias útiles que están siendo cada vez más claras en el sentido que no sólo la psicosis en sí misma, sino que el contexto clínico de la experiencia psicótica es el que determina el riesgo de la transición hacia la esquizofrenia. De este modo, el riesgo de transición hacia el trastorno psicótico totalmente constituído está determinado en gran medida por el peso de la “carga” psicótica, el distrés y la depresión comórbidos, el empleo de cannabis, la capacidad cognitiva y las expresiones subjetivas de deterioro y adaptación. La realización del diagnóstico de un trastorno psicótico no constituye una ciencia exacta, sino que implica la imposición de un límite arbitrario a las variaciones en las dimensiones psicopatológicas y la necesidad de evaluación a lo largo del tiempo. El progreso en la comprensión de los factores cognitivos y biológicos que llevan a la variación de las dimensiones, incluyendo las intervenciones terapéuticas, es discutiblemente más útil que los estériles modelos de predicción dicotómica
Abstract
Le dépistage d'état préschizophrénique dans la population générale dans le but d'empêcher le passage à la forme déclarée de la maladie est une impossibilité épidémiologique, parce qu'une maladie rare ne peut être anticipée. Le manque de spécificité dû à l'abondance des faux positifs peut être compensé en partie par des critères de dépistage plus restrictifs associant plusieurs indicateurs de risque pour le passage à la schizophrénie. L'augmentation de la spécificité (réduction des faux positifs) ne peut néanmoins se faire qu'aux dépens de la sensibilité (augmentation des faux négatifs). La méthode la plus répandue pour augmenter la spécificité est d'enrichir l'échantillon. Cela implique la création d'échantillons dans lesquels le risque schizophrénique est augmenté en filtrant sélectivement les individus à risque par une série d'orientations successives à partir de la population générale en passant par les médecins généralistes, les services de santé mentale et les services de détection clinique précoce. Néanmoins, ces améliorations de spécificité obtenues par cette méthode ne devraient pas être attribuées à l'utilisation de quelques instruments prédictifs supposés identifier les patients à haut risque. La méthode de dépistage et de détection précoce qui a le plus de chances de réussir épidémiologiquement et éthiquement est d'augmenter sélectivement la perméabilité des filtres sur le parcours vers les soins de santé mentale. Ceci produira des échantillons de demandeurs d'aide enrichis en risque schizophrénique dans les services de santé mentale (réduisant donc les faux positifs) en essayant d'attirer en même temps à travers ces filtres autant de prodromes schizophréniques que possible (réduisant donc les faux négatifs). La recherche de psychose précoce est à l'origine de quelques propositions utiles qui montrent de plus en plus clairement que ce n'est pas juste la psychose elle-même, mais le contexte clinique d'un épisode psychotique qui détermine le risque de passage à la schizophrénie. Le risque de passage à un état psychotique déclaré est donc largement déterminé par le poids de la «charge» psychotique, par l'existence d'une dépression et d'une souffrance comorbides, d'un usage de cannabis, par les capacités cognitives et les sentiments subjectifs exprimés de détérioration et de stratégies d'adaptation. Diagnostiquer un trouble psychotique ne relève pas d'une science exacte : cela implique une limite arbitraire imposée aux variations dimensionnelles en psychopathologie et la nécessité de soins au cours du temps. On peut dire qu'avancer dans la compréhension des facteurs biologiques et cognitifs qui commandent la variation dimensionnelle, y compris les interventions thérapeutiques, est sans doute plus utile que tes modèles stériles dichotomiques de prédiction.
he detection of psychotic disorder in the prodromal phases, coupled with specialized early interventions to prevent transition to overt psychotic disorder, has become the subject of an increasing amount of research and debate.1-8 Although this issue is by no means new,9,10 it is only in the last few years that the outlines of a consensus, based on quantitative arguments, are becoming discernible. These will be discussed in this article, using data from several population-based investigations to illustrate the quantitative arguments.
Is there a rationale for schizophrenia prevention in the first place?
The answer to this question is evident. If there is a way to prevent an illness that usually has a poor prognosis and starts in young adulthood, every effort should be made to put preventive measures into place. Work originating in Germany, the Netherlands, Norway, and elsewhere has suggested that a delay of about 1 year between the onset of positive psychotic symptoms and the initiation of treatment is not rare.11-13 From the patient's point of view this contributes not only to severe social stagnation and decline,14,15 but also to severe mental suffering, thus providing a powerful rationale for prompt treatment immediately after the onset of the first psychotic episode. Another rationale for rapidly commencing treatment is the possibility that the longer the duration of untreated psychosis (DUP), the less effective treatment will be in the long term.16,17 It is quite likely that part of the observed association between a longer DUP and neuropsychological deterioration is noncausal.18,19 However, the mere possibility that prolonged episodes of psychosis impact negatively on longer-term outcome justifies the need for increased vigilance on the part of the clinician to identify prodromal symptoms.20,21
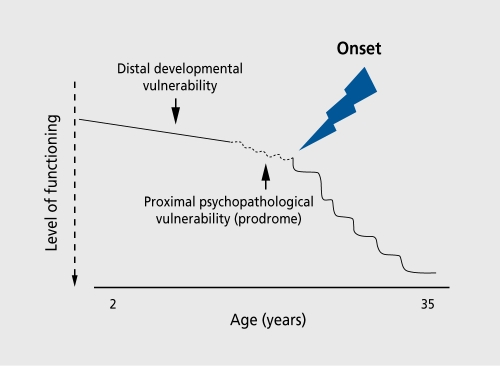
However, the concept of screening and prevention in schizophrenia hinges on schizophrenia somehow manifesting itself before the onset of the disease. Therefore, the rationale for schizophrenia prevention, in terms of feasibility needs to be demonstrated first. Evidence has come from two lines of research. The first focused more on the expression of nonpsychopathological vulnerability over the course of development, and the second more on the expression of subclinical psychotic phenomena proximal to illness onset (Figure 1).
Figure 1. Prepsychotic expression of illness.
Research on developmental vulnerabilities long before onset
The first line of research had its focus on the developmental trajectories of children destined later to develop schizophrenia, and established that there were small, but detectable, group differences between the preschizophrenia children and their peers in terms of motor, social, and cognitive development.22 Although the existence of such indicators of developmental vulnerability could in theory be used to initiate a selective prevention program, it soon became clear that although group differences were detectable between preschizophrenia children and their peers as early as 2 years of age, these differences were very small, with the great majority of preschizophrenia children scoring well within the normal range. This would make it all but impossible to predict prospectively, on the basis of such developmental indicators, if a child would develop schizophrenia.23 For example, if, in a cohort of 5000 children, 20 children (0.4%) out of a total of 30 destined to develop schizophrenia have a value on a motor development variable below 40 on a scale of 1 to 100, and the children share this feature on the developmental motor variable with 2000 (40%) other children in the cohort, it can be readily seen that - although significant- the predictive value of this score will be too low for the purpose of screening and prevention. The only way to remedy this situation is to introduce, with the wisdom of hindsight, some post hoc selection criterion24 that nevertheless would not have been available prospectively25
Research on mental state vulnerabilities close to onset
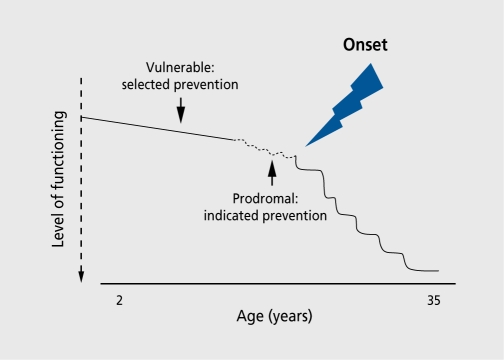
The second line of research should not be seen in isolation from the first, but a crucial difference is that the focus now is not so much on indicators of vulnerability expressed in parameters of motor, social, or cognitive development, but on parameters related to mental state and functioning in the period closer to the onset of the disorder, which, in the case of an actual illness onset, can retrospectively be labeled as prodromes of the illness. Careful follow-back studies of first-episode schizophrenia patients using instruments like the Interview for Retrospective Assessment of Schizophrenia (IRAOS)26 have established that the great majority of first-episode patients displayed evidence of signs and symptoms up to 6 years prior to onset of the psychotic disorder.27 Given the high rate of detectable prodromes in patients, the question arises of whether these prodromes could not have been used to identify individuals in the very early throes of psychosis, so that early treatment would have possibly aborted their further transition to full-blown psychotic disorder. In other words, if it is not possible to practice selective prevention in the developmental phase, would it be possible to practice indicated prevention in the prodromal phases Figure 2?
Figure 2. Prevention of full-blown psychotic disorder.
So chizophrenia has detectable prodromes, but how many - if any - prodrome-like mental states exist in the general population and must we distinguish between prevalence and incidence?
Prevalence of subclinical psychotic experiences
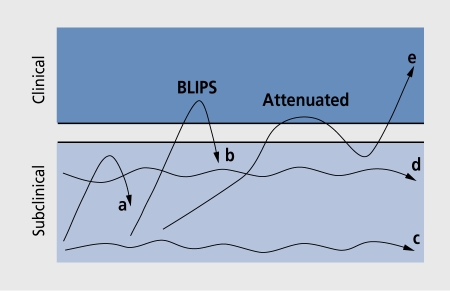
While it may well be possible to diagnose, with the wisdom of hindsight, the presence of prodromes in patients with established disease, the real issue is to try to turn things around and establish prospectively whether individuals with mental state experiences that resemble prodromes (if indeed such individuals exist at all in detectable quantities) will go on to develop schizophrenia in the future. From this prospective perspective, prodrome-like mental states can best be labeled as subclinical psychotic experiences instead of prodromes, as prodromes can only be diagnosed a posteriori, after the onset of the psychotic illness. A crucial question then becomes what the rate is of such subclinical psychotic experiences in these populations. We are particularly interested in subclinical positive psychotic experiences, as arguably these, in contrast to the very subtle, subclinical expression of experiences resembling negative symptoms or formal thought disorder, should also be measurable with reasonable accuracy in healthy populations. Indeed, key variables used in early identification and prevention of psychotic disorder are so-called attenuated, brief, or limited, psychotic symptoms, as well as schizotypal signs and symptoms (Figure 3). 28-35 Recent population-based research from the USA, France, the Netherlands, New Zealand, and Germany suggests that the lifetime prevalence of such subclinical psychotic experiences is very high.35-40 The data collected in the USA, New Zealand, Germany and the Netherlands are summarized together in Table I, as they used similar instruments across different age-groups and excluded psychotic phenomena due to drug use and physical illness. These studies show that the rate of subclinical psychosis is around 10% to 20%, depending on type of psychotic experience and age-group. The prevalence rate of psychotic experiences associated with distress is considerably lower at around 4%, although this figure is still much higher than the prevalence of nonaffective psychosis (less than 1%).
Figure 3. Course of subclinical psychosis. Person c has a stable low level and person d a stable higher level of subclinical psychosis. Persons a and b have unstable levels, but person a never crosses the clinical threshold, whereas person b does. Person e has unstable levels, develops an attenuated psychotic experience that initially resolves, but later results in full-blown psychotic disorder. The psychotic disorder of person e could possibly have been prevented by intervening in the attenuated stage. BLIPS, brief limited intermittent psychotic symptoms.
Table I. Lifetime prevalences of DIS/CIDI subclinical psychotic experiences expressed in percentages. DIS, Diagnostic Interview Schedule; CIDI, Composite International Diagnostic Interview.
| Country of study | No. of patients | Age (years) | Hallucinations | Delusions | Hallucinations and delusions | Remarks |
| USA36 | 810 | 18-64 | 11% | Rate for two or more | ||
| symptoms was 4.2% | ||||||
| New Zealand35 | 761 | 26 | 13% | 20% | - | |
| 761 | 11 | - | - | 14% | ||
| Germany38 | 2548 | 17-28 | 5% | 16% | 18% | Rate for two or more |
| symptoms was 7.3% | ||||||
| Netherlands39 | 7075 | 18-64 | 6% | 9% | 18% | Regardless of presence of distress |
| 7075 | 18-64 | 2% | 3% | 4% | With distress/help-seeking behavior |
Incidence of subclinical psychotic experiences
While the lifetime prevalence of subclinical experiences is important, the incidence is more relevant from the clinical viewpoint. Thus, trying to predict schizophrenia in somebody who had a psychotic experience 15 years ago is clinically less relevant than trying to predict schizophrenia in a person who, a week ago, had first-ever onset of a subclinical psychotic experience. It is perhaps surprising that, in spite of the fact that schizophrenia prevention is becoming increasingly more topical - even to the point of including individuals in randomized, controlled trials to prevent transition to full-blown psychotic disorder - virtually nothing is known about the epidemiological parameters of the mental state phenomena that are widely used to identify high-risk individuals. Only two studies, one in the USA41 and one in Europe,42 have attempted to quantify the incidence of psychotic experiences below the level of clinical disorder, both based on repeated measurements in a large general population sample. Given the fact that the incidence of schizophrenia as a clinical disorder is low at around 0.01% to 0.02%, the results of both studies are, similarly to the prevalence data shown above, in stark contrast, as the incidences found were 1% in the American study41 and 2% in the European study42 In other words, the incidence of subclinical psychosis is about 100 times more frequent than its clinical counterpart.
What does “transition” from subclinical to clinical mean?
The high population prevalence and incidence rates of subclinical psychosis suggest that the psychosis phenotype exists in nature in a much more continuous state than the diagnostic manuals based on patients admitted to psychiatric hospitals would suggest.43,44 Early detection clinics report “high-risk” individuals having 50% transition rates to “psychotic disorder”45,46 over a 3- to 6-month period. However, making a diagnosis of psychotic disorder is not an exact science, it involves an arbitrary cutoff imposed on dimensional variations of psychopathology and the need for care over time. Gaining insight into the cognitive and biological factors that drive the dimensional variation, including therapeutic interventions, is arguably more useful than sterile dichotomous prediction models.
So, if the rate of subclinical psychosis is comparatively high, how predictable - if at all - is the transition to schizophrenia?
The significance of the high prevalence and incidence rates of subclinical psychotic experiences is that the ratio of subclinical/clinical is necessarily going to be very high: about 1:100 for incidence and about 1:20 for prevalence. In other words, for each 100 new onset cases of subclinical psychosis, only one case of nonaffective psychotic disorder is going to result: the predictive value is only 1%. Similarly, for each 20 individuals who have ever had a subclinical psychotic experience in their lives, only one is also going to have a lifetime diagnosis of nonaffective psychotic disorder: the diagnostic value is only 5%. In other words, if incident subclinical psychotic experiences were going to be used as a test to screen for incident psychotic disorder in the general population, 99% would be rated false-positive, and if prevalent subclinical psychotic experiences were going to be used as a test to screen for prevalent psychotic disorder, 95% would be rated falsepositive.
The diagnostic value and the predictive value of subclinical psychotic experiences in the general population studies have, until very recently, never been formally tested. In a European longitudinal, general population study, Hanssen et al47 assessed the diagnostic value of subclinical psychotic experiences by quantifying how many individuals with a lifetime subclinical psychotic experience also had a lifetime diagnosis of affective or nonaffective psychotic disorder. They found that the diagnostic value for any subclinical psychotic experience was 8%.47 The same authors assessed the 2-year predictive value of new onset subclinical psychotic experiences on later new onset of affective or nonaffective psychotic disorder and found that this also was 8% - as this was calculated over 2 years the 1-year predictive value would be 4%. This latter finding was somewhat surprising, as the predictive value of 4% is much higher than the expected 1% described above. The reason for the discrepancy was that affective and nonaffective psychotic disorder in this general population sample were combined into a single category with a higher rate than the traditional 0.01% to 0.02% schizophrenia incidence. In addition, the high incidence of psychotic disorder in general population studies, as opposed to treatment samples, is well known35,41 and can be taken to prove that case definition on the basis of treatment introduces a degree of treatment bias, also known as Berkson bias, in psychiatric incidence studies.48
Given predictive and diagnostic values of 4% to 8 %, how effective would prodromal intervention be if a treatment with a 50% success rate existed?
Let us very optimistically assume that, given the 4% predictive value described above, a treatment existed that could be applied in the prodromal phase and would abort transition to full-blown psychotic disorder in 50% of treated cases. If we wished to apply this treatment on the basis of a screening program for subclinical psychotic experiences in the general population, how many people who screened positive would need to be treated to prevent one case of psychotic disorder? This can be calculated quite simply as 0.04 (the predictive value) x 0.5 (the treatment success rate) =0.02 or, in other words, for every 100 cases who screened positive for subclinical psychosis and received treatment, 2 transitions would be prevented. In other words, the number needed to treat49 would be 50 and, more importantly, the number needed to inconvenience would be 49, ie, 49 individuals would needlessly receive treatment. Clearly, such figures indicate that early intervention in the general population is not feasible, at least not on the basis of the subclinical psychosis screening criterion. However, even if a screening criterion existed with a 25% predictive value, the number needed to inconvenience would still be 7 (Table II)- unacceptably high given the ethical rules surrounding screening in most countries50 and given the fact that antipsychotic treatments may not be without side effects.51-53
Table 2. The number of people screening positive for subclinical psychotic experiences who needed to be treated to prevent one case of full-blown psychotic disorder, as a function of the predictive value of the test and the success rate of the prodromal treatment in preventing transition to fullblown psychotic disorder.
| Predictive value (%) | Treatment success rate (%) | Number needed to treat | Number needed to inconvenience |
| 5 | 25 | 80 | 79 |
| 5 | 50 | 40 | 39 |
| 20 | 25 | 20 | 19 |
| 20 | 50 | 10 | 9 |
| 50 | 25 | 8 | 7 |
| 50 | 50 | 4 | 3 |
For screening and prevention of schizophrenia, not much can be done with predictive and diagnostic values of 4 of 8 %. Cans these values be improved?
The conclusion so far has been very simple: it is very difficult to predict or diagnose a rare disease in the general population on the basis of a test resembling some precursor phenomenon. Is it possible to improve on this state of affairs? The answer to this question is yes, and the strategy to follow is to change schizophrenia from a rare disease to a common disease: if instead of 1%, the prevalence of schizophrenia were 50%, the predictive value of any test, even pointing at random to a person with one's eyes closed, would be at least 50%, clearly a much more attractive situation epidemiological than the 8% probability reported above. As of course the incidence and prevalence of schizophrenia cannot be changed, some indirect manipulation must be employed in order to make the disease more “predictable.” Below, three possible strategies will be described.
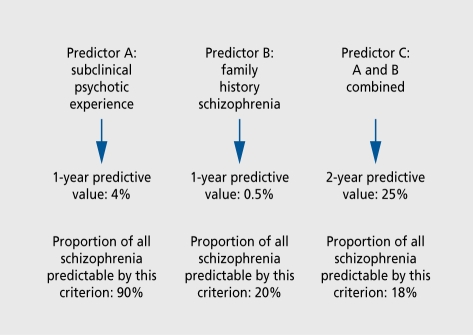
Raising the rate of schizophrenia by changing the context of risk
In the previous sections, the predictive and diagnostic values of a single predictor, subclinical psychotic experiences, were examined. However, if there are other predictors, and their effects are additive, the predictive value will increase accordingly, as illustrated in Figure 4. The problem with this strategy, however, is that although the combination of predictors into a single criterion will make schizophrenia more predictable, it will also apply to fewer patients (Figure 4). For example, if a family history of schizophrenia is used as an additional criterion for prediction, the maximum proportion of all future schizophrenia patients that can be predicted is 20%, as only 20% of all patients with schizophrenia have a positive family history. Therefore, the more predictors one combines, the greater the probability that a transition to psychotic disorder is going to take place in the near future, but also the greater the probability that this is not relevant for the bulk of schizophrenia cases that one is trying to prevent from occurring. In the case of a deadly disease for which a curative treatment existed in the prodromal phase, the strategy of combining predictors to enhance specificity at the expense of sensitivity would be disastrous, as one would need to reduce the number of false-negatives to an absolute minimum. However, in the case of schizophrenia, it could be argued that, given the fact that uncertainty exists about the type and effectiveness of treatments in the prodromal phase,54 and that the disease is not rapidly fatal, the goal should be to err on the side of reduction in false-positives rather than false-negatives, so as not to unnecessarily burden and/or stigmatize healthy individuals.
Figure 4. Making schizophrenia more predictable (but for fewer patients), Predictor A is the presence of subclinical psychotic experiences, which previous research has shown increased the 1 -year risk of schizophrenia by 4%. As the majority of patients with schizophrenia (around 90%) displayed such subclinical experiences as part of the prodrome, 90% of all schizophrenia should theoretically be predictable if this criterion were used. However, if a family history of schiozphrenia were used (predictor B), only 20% of all schizophrenia would be predictable, given that only 20% of patients have a family history, Therefore, although the application of predictor C (the combination of subclinical psychosis and a positive family history) greatly increased the 1-year predictive value, only a small proportion of all schizophrenia would be predictable with the criterion.
Raising the rate of schizophrenia by changing the quality of the subclinical psychosis
Although the majority of research efforts in the field of early identification and prevention made use of the presence of subclinical psychotic experiences (attenuated, brief, or otherwise subclinical psychotic experiences) to predict transition to full-blown psychotic disorder, work pertaining to the field of cognitive psychology predicts that the prognosis of subclinical psychosis also depends on associated features, such as the amount of subclinical psychosis, degree of associated distress, tendency to experience negative emotions (neuroticism) , comorbid depression, and coping.55-58
A recent series of publications pertaining to the Netherlands Mental Health Survey and Incidence Stduy (NEMESIS) clarified the issue of context of the subclinical psychotic experience in relation to the later onset of psychotic disorder. In this study a randomly selected general population cohort was interviewed with the Composite International Diagnostic Interview (CIDI)59 three times (T0 T1 and T2) over a period of 4 years, and individuals with suspected psychotic symptomatology were reinterviewed by clinicians over the telephone.39,44,60,61 Given the longitudinal design, it was possible to identify a group of individuals who at T0were free of any lifetime clinical or subclinical psychotic experiences and who at T1 had developed first-onset, incident subclinical psychotic experiences. The individuals with T1 incident psychosis were subsequently seen again at T2, 2 years later, and assessed for new onset of psychotic disorder. As reported above, the probability of developing a first-ever onset of psychotic disorder given the presence of a firstever onset of a subclinical psychotic experience 2 years earlier was 8%. However, this risk could be modified substantially depending on a range of characteristics associated with the subclinical experience (Table III). 2 For example, the number of incident subclinical psychotic experiences as well as their quality in terms of associated depression and distress or help-seeking behavior raised the predictive values considerably up to 500%, as did the presence of high levels of neuroticism, cannabis use, low cognitive ability, and subjective reports of impact on functioning (Table III).
Table III. Predictive value of incident subclinical psychotic experiences on incident affective and nonaffective psychotic disorder 2 years later as a function of associated characteristics of the predictor.42 CI, confidence interval. *These data were not reported in reference 42, but were analyzed specially for the purpose of this paper; for methods see reference 42. # A proxy measure of cognitive ability (educational attainment) was used.
| T1 predictor | 2-year predictive value for psychotic disorder | 95% CI |
| Subclinical psychotic experience | 8% | 6.8-8.4 |
| Subclinical psychotic experience + some degree of distress or help-seeking | 14% | 14.5-16.8 |
| associated with experience* | ||
| Subclinical psychotic experience + depressed mood | 15% | 13.6-15.8 |
| More than one subclinical psychotic experience | 21% | 19.8-22.3 |
| More than one subclinical psychotic experience with low mood | 40% | 38.5-41.5 |
| Subclinical psychotic experience and some degree of subjective impairment of functioning* | 16% | 14.5-16.8 |
| Subclinical psychotic experience and cannabis use* | 13% | 11.5-13.5 |
| Subclinical psychotic experience and lower cognitive ability*# | 13% | 11.5-13.5 |
| Subclinical psychotic experience and high neuroticism* | 12% | 11-13 |
Although these results may seem encouraging, a comparison with the data in Table II will make it clear that even these higher predictive values come nowhere near an acceptable trade off between successful abortions of transition to psychotic disorder and numbers needed to inconvenience. They nevertheless provide valuable clues to the dynamics of the onset of psychotic disorder, which may be useful, if not at the level of the general population, certainly at the level of mental health care.
Raising the rate of schizophrenia by sample enrichment strategies
The sample enrichment strategy basically consists of the creation of a sample with many people at risk by selectively filtering them out over a range of consecutive referral processes starting in the general population, through to general practioners (GPs) , mental health services, and the early detection clinic. The sample enrichment strategy is undoubtedly the most widely used approach in the early intervention literature, but possibly also the worst understood, in that the high predictive values obtained in sample enrichment studies are often wrongly attributed to some instrument with supposedly high predictive values, whereas in reality they are a function of the sample enrichment strategy itself. For example, several authors have suggested that the high “transition rate” to psychotic illness in individuals exhibiting psychosis-like symptoms is between 40% and 70%, thanks to the use of some prodromal-rating instrument,34,45,46,62,63 advocating the use of such instruments in order to reduce transition to full-blown illness. However, closer inspection of these data is required, as illustrated by the following example.
In a recent publication, Klosterkotter et al63 reported a follow-up study of 160 young individuals who were considered to be at risk of developing psychotic illness. The signs and symptoms used to predict transition to schizophrenia were from a list of “basic symptoms.”64 The presence of any of the baseline basic symptoms was used as a test to predict the onset of psychosis over a mean follow-up period of 9.6 years. The main results are presented in Table IV: the risk of developing schizophrenia, given the presence of a basic symptom described by Huber et al,64 was 77/110 (70%). Therefore, these data apparently predicted the onset of schizophrenia over a 9-year period with 70% accuracy! The question, however, is whether this high predictive accuracy can be completely attributed to these basic symptoms, or whether instead other factors are more important. In reality, only a minor proportion of the predictive value can be attributed to the basic symptoms, because most can be ascribed to the very high baseline rate of schizophrenia in this sample. As can be seen in Table IV, the final rate of schizophrenia in this sample was 79/160 (49%). The conclusion from this is that by chance alone, any subject in this study had a nearly 50% probability of developing schizophrenia anyway. In other words, the predictive value of any factor, whether it be basic symptoms, sex, color of the eyes, or any other random variable, would have been at least 50%. Thus, the role of the basic symptoms was to raise the predictive value modestly from 50% to 70%, not to fully cause a predictive value of 70%. Instead of the predictive value of basic symptoms, the real noteworthy element of the remarkable study by Klosterkotter et al63 lies in the fact that the authors succeeded in creating a series of sophisticated selection processes that led to a final enriched sample of individuals with a 50% probability of developing schizophrenia over the 9.6-year period. This selective enrichment process involved the existence of special interest groups at German university psychiatry departments, with an interest in young people who posed a challenge with regard to a possible diagnosis of schizophrenia. Such a center “attracts” a highly enriched sample of individuals at risk of schizophrenia through a series of selection processes, as illustrated in Table V Individuals in the general population developing illness behavior visit the GR The GP refers those with suspected severe mental disorder to the general mental health services. The general mental health services refer those with suspected schizophrenia onto the specialist university department. With each referral from one level to the next, a selection process takes place creating “enriched” samples that are progressively more likely to contain individuals who are likely to develop schizophrenia. Other groups wishing to replicate the German findings in their own setting, must therefore not only use the basic symptom scale, but, much more importantly, replicate exactly the same sample enrichment strategy to yield a sample with a 50% probability of developing schizophrenia. In addition, rather than a posteriori, any additional contribution of basic symptoms to the predictive value needs to be replicated prospectively in a fresh sample at the start of sampling enrichment procedure. If the results hold after these replications, the basic symptoms,64 or instruments used in Melbourne, Australia,46 or New Haven, Conn,45 may possibly be used to modestly raise the predictive value from 50% to 70% in samples enriched with schizophrenia risk. In Table V, the effect of using measures such as Basic Symptoms or other high-risk instruments at other levels in the sample enrichment procedure with more diluted samples and therefore lower rates of (future) schizophrenia is shown. The predictive values were calculated using the DIAGTEST procedure in the STATA statistical program, version 8,65 at various levels with their corresponding best estimate rates of schizophrenia. The DIAGTEST procedure in STATA provides the predictive values based on Bayes' theorem. As can be seen in Table IV in the general population, the basic symptoms would not yield a positive predictive value (PPV) of 70%, but of only 1.4%, and at other levels in the sample enrichment procedure the predictive values were also much lower.
Table IV. Predictive value of basic symptoms of schizophrenia in a 9.6-year follow-up of 160 young individuals.63 .
| Outcome | Total | |||
| Psychosis + | Psychosis - | |||
| Test | Symptom + | 77 | 33 | 110 |
| Symptom - | 2 | 48 | 50 | |
| Total | 79 | 81 |
Table V. Positive predictive value (PPV) of basic symptoms at different levels along the pathways of mental health care with varying schizophrenia prevalences. *These figures were reported by Klosterkotter et al, 2001,63 In the other rows, the PPV has been adjusted for the change in prevalence, all else remaining the same.
| Care pathway level | Prevalence of schizophrenia | PPV of basic symptoms64 |
| General population | 0.6% | 1.4% |
| Primary care | 2.0% | 4.7% |
| Mental health outpatients | 7.0% | 15.3% |
| Specialized university | 50%* | 70%* |
| department with special | ||
| interest in schizophrenia* |
Thus, reports of high PPVs in schizophrenia on the basis of mental states or other risk factors can be attributed to the high baseline rates of schizophrenia in the samples used, created through a series of selection procedures in the sampling process34,45,46,63 or, sometimes, the statistical62 procedure used.25,66 These selection procedures contribute to exciting and clinically relevant findings. However, almost invariably a large proportion of the predictive values are wrongly attributed to the various predictors used rather than to the selection procedures that resulted in higher prevalence or incidence rates of schizophrenia and hence a higher baseline predictive value. The consequence of this confusion is that clinicians attempting to use such findings in their practice may erroneously focus on the predictors rather than the sampling enrichment selection procedure itself. In addition, the high predictive values reported in the literature are often based on a posteriori optimization algorithms in the sample at the end of the sample enrichment filtering procedure. The correct procedure would be to demonstrate its validity a priori in a prospective investigation at the beginning of the sample enrichment procedure.
Of course, the sample enrichment strategy, similarly to the other strategies to raise the prevalence of schizophrenia that were discussed earlier, suffers from the limitation that only a tiny proportion of all detectable schizophrenia cases in the general population will be identified for early treatment in this way. The great majority of prodromal schizophrenia will never make it through the various selection procedures from the decision to visit the GP, subsequent GP referral to mental health outpatients, and from there to the specialized prodromal clinic- they will only come to the attention of mental health services after having developed the first acute psychotic episode, not before. Although it is true that prevention of even 1% of all transitions to schizophrenia would constitute an important result from the clinical viewpoint, one may nevertheless question whether specialized early intervention clinics can ever be made cost-effective, given competing demands for funding.67
Do people with preschizophrenia wish to be «detected»?
In the previous sections, it was demonstrated that screening at the level of the general population is not useful from a methodological viewpoint, as diagnostic and predictive values would remain too low. However, screening in the general population may also be ethically unsound as one may well violate the person's right “not to know” that one has (a risk for) a mental illness. This problem may be overcome by screening individuals who demonstrate subclinical psychotic experiences at the level of mental health outpatient services instead of the general population level. To screen at the mental health services' level would not only result in much higher predictive values as seen above, but would have the additional advantage that such individuals would already have acknowledged a need for help for a mental health problem. This strategy would result in less danger of stigmatization in the case of a false-positive test result or of violating the right “not to know” in the case of a true positive test result. In fact, the only way to go about screening for schizophrenia in not only a methodologically but also an ethically responsible fashion, would be to screen for schizophrenia in individuals who are already seeking mental health care: the prevalence of schizophrenia in this population is sufficiently high to make screening feasible and they would already have developed the hypothesis that they may need help for a problem to do with their mental health. Even then, however, there may be a risk that, as people become more focused on the culture of detection and prevention of schizophrenia, the cultural change itself would result in increasing numbers of people receiving (pre) schizophrenia diagnoses, similar to the recent fashionable reduction in the diagnostic threshold for attention deficit-hyperactivity disorder (ADHD) and autism spectrum disorder in children, and multiple personality disorder in adults.
So far, all we have seen are high-risk strategies that may prevent transition to full-blown psychotic disorder in an tiny proportion of all preventable schizophrenia: can't we do better than that?
The prevention paradox
The problem with the high-risk strategies described so far is what has been called the prevention paradox.68 At the heart of the paradox lies the observation that preventing a small number transitions to psychotic disorder is possible without being able to affect transition of the large number of all other preventable schizophrenia. In other words, the high-risk groups used for screening and prevention are not very representative of all preventable schizophrenia, and focusing on the low-risk groups would therefore have a much higher preventive yield.
The strategy to focus on everybody at risk, regardless of whether their risk is high or low, is a form of universal prevention or population prevention. An example of this type of intervention is to raise the price of alcoholic beverages to reduce traffic accidents. Raising the prices of alcohol reduces alcohol consumption in the whole population. Raising prices therefore affects not only the few problem drinkers, who are most at risk for traffic accidents, but also the much more prevalent group of moderate drinkers. Although the problem drinkers are more at risk of traffic accidents than the moderate drinkers, most alcohol-related accidents are not caused by the few problem drinkers, but by the much more prevalent group of moderate drinkers, whose individual risk may be lower than the problem drinkers, but whose impact on the total population rate of traffic accidents is higher simply because there are many more moderate drinkers than problem drinkers.
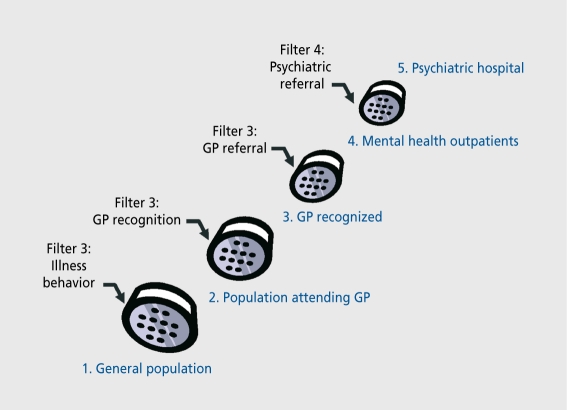
In the field of schizophrenia, the analogy with the alcohol paradigm lies in increasing the permeability of the “filters along the pathway to mental health care.”69 These “filters” refer to the hurdles that a prospective patient, with a newly developed psychotic illness, will encounter before coming into contact with a qualified mental health professional (Figure 5). The first filter on the pathway to mental health care is the development of awareness on the part of the patient and his or her family and friends that there are psychotic experiences resulting in behavior necessitating consultation with a health professional, who is usually the GP. The next filter is the ability of the GP to detect the early symptoms of psychotic illness, resulting in an accurate provisional diagnosis. The next filter comprises the GP's decision to refer the patient to the appropriate mental health services. Once in contact with the services, many patients with psychotic illness will pass the filter and move on to the next level, which is admission to hospital. If the permeability of the filters can be increased, the whole population, regardless of whether their risk for psychosis is high or low, will experience a greater accessibility to mental health services and therefore to the possibility of schizophrenia prevention.
Figure 5. Figure 5. Filter model of psychotic symptoms and psychotic disorder. GP, general practitioner. Reproduced from reference 69: Goldberg D, Huxley P. Mental Illness in the Community. London, UK: Tavistock Publications; 1980. Copyright © Tavistock Publications, 1980.
How the permeability of these filters can be influenced was demonstrated in a Norwegian study70,71 In this study an extensive public information campaign was conducted to educate the general population, schools, and health professionals alike, regarding the signs and symptoms associated with early psychosis and the long-term benefits of early referral, diagnosis, and treatment. An observation of this study was that, compared with the period prior to the campaign, the incidence of reported psychotic illness increased to approximately 40% with an associated reduction in the time taken for initiation of treatment or DLJP,70,71 suggesting that the campaign had caused a relatively large increase in the permeability of the filters along the mental health care pathway Similar improvements in mental health care have also been corroborated by an Australian study72 and a Canadian study73 The significance of these studies was to demonstrate that the filters could be made more permeable so that more early psychosis came earlier in contact with services.
The great advantage of the universal prevention approach is that it will make people come to mental health services rather than the other way round, reducing the inherent risk of stigmatization and falsely labeling individuals. Another advantage is that previous work has shown that individuals whose subjective subclinical experiences are not objectively recognized by the clinician nevertheless have a higher risk of transition to psychotic disorder74 - under the universal prevention strategy these individuals can also be encouraged to seek help at the level of mental health care more easily. However, the cost-effectiveness of these public health campaigns and the extent to which the patients referred were in the throws of a brief psychotic state that would have resolved naturally anyway remains to be elucidated. Another risk with this approach is that services will become flooded by individuals with all types of mental health complaints, many of which are not in need of treatment, let alone treatment in the context of schizophrenia prevention.
A more restrictive campaign approach would be to target general practices only Bak and colleagues75 described a much more limited information campaign among GPs who were offered a possibility of rapid, low-threshold referral service for patients with early psychosis in an urban setting. These authors also reported an increase in referrals compared with the precampaign period.
Another more restrictive approach would be to combine the universal with the high-risk sample enrichment strategy by making the filters more permeable, while at the same time putting restrictions into place so that only those who are most likely to carry schizophrenia risk would rise more easily through the filters on the pathway to mental health care and come into contact with a specialized early intervention clinic. This could be done, for example, by focusing community educational campaigns very restrictively on psychosis and its prodromes.
If rare disorders are so difficult to predict, why not make the process more efficient and use subclinical psychosis to predict psychotic disorders and also the much more prevalent nonpsychotic disorders?
The NEMESIS study demonstrated that the predictive value of subclinical psychotic experiences remains low even if affective and nonaffective psychotic disorders are combined into a single outcome category because of lack of specificity42 However, this very lack of specificity may be an advantage in public health terms, as it raises the possibility of strategies to predict and prevent a range of psychiatric disorders, not just schizophrenia.76 Thus, the predictive efficiency of subclinical psychosis may be enhanced considerably if it used to not only predict psychotic disorder, but also a range of other disorders such as depression and anxiety, which, according to recent research, are also moderately strongly comorbid with psychosis.77,78 Using the three interview waves (T0, T1, and T2) of the NEMESIS data discussed above, we calculated the predictive value of first-ever onset subclinical psychotic experiences at T1 on T2 incidence of Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R) depressive disorder, anxiety disorder, alcohol or drug misuse, and any nonpsychotic disorder, alone and in combination with T2 incident affective and nonaffective psychotic disorder. This revealed that predictive values for nonpsychotic disorder were lower than the 8% predictive value for psychotic disorder, with the exception of depression (predictive value: 13%). Combining psychotic and nonpsychotic disorder outcome categories only raised predictive values by a small amount (Table VI).
Table VI. Predictive values, using the three waves of the Netherlands Mental Health Survey and Incidence Study (NEMESIS) (T0, T1, and T2) of T1 incident subclinical psychotic experiences on T2 incident disorders. CI, confidence interval.
| T2 predicted outcome | Predictive value of T1 incident subclinical psychotic experiences (95% CI) |
| Psychotic disorder | 8% (6.8, 8.4) |
| Depressive disorder | 13% (11.6, 13.9) |
| Anxiety disorder | 4% (3.7, 5.0) |
| Alcohol/drug misuse disorder | 6% (5.4, 7.1) |
| Any nonpsychotic disorder | 7% (5.5, 7.4) |
| Combined depressive disorder | 15% (13.8, 16.0) |
| and psychotic disorder | |
| Combined anxiety disorder | 9% (7.6, 9.4) |
| and psychotic disorder | |
| Alcohol/drug misuse disorder | 10% (8.7, 10.5) |
| and psychotic disorder | |
| Any disorder | 7% (5.5, 7.4) |
Conclusion
The area of early intervention and prevention of psychotic illness is certainly exciting and brings a muchneeded focus to the underfunded mental health services for the severely mentally ill. On the other hand, a range of epidemiological and ethical issues remain to be addressed. Similarly, it has been pointed out that early detection and good early treatment need to go hand in hand,5 and unfortunately the evidence base for so-called phase-specific treatments at this time remains very limited, offering little guidance.54 Lastly, cost-effectiveness data remain wanting. Therefore, the following conclusions can be drawn:
Early detection clinics report “high-risk” individuals having 50% transition rates to “psychotic disorder” over a 3- to 6-month period. However, making a diagnosis of psychotic disorder is not an exact science: it involves an arbitrary cutoff imposed on dimensional variations of psychopathology and the need for care over time. Gaining insight into the cognitive and biological factors that drive the dimensional variation, including therapeutic Interventions, Is arguably more useful than sterile dlchotomous prediction models.
Screening In the general population for at-risk mental states Is useless: a rare disease such as schizophrenia cannot be predicted using prevalent predictors. In fact, depressive disorder can be better predicted by subclinical psychotic experiences than psychotic disorder itself (although for depression the predictive value also remains much too low to be useful for screening purposes).
Screening predictive values can be improved substantially by manipulating the sample rate of (future) schizophrenia, but the price to be paid is high as large numbers of false-negatives will be created, which will remain permanently “undetectable.” The sample enrichment strategy (creating samples with many people at risk by selectively filtering them out over a range of consecutive referral processes starting In the general population, through to GPs, mental health services, and the early detection clinic) Is the most commonly used strategy to Improve screening predictive values, but these Improvements are equally commonly wrongly attributed to the use of some predictive instrument that supposedly identifies high-risk individuals.
If one considers that cost-effectiveness considerations should not stand in the way of clinicians attempting to help people at risk of making the transition to psychotic disorder, the epidemiologically and ethically most viable way for screening and early detection is to selectively increase the permeability of the filters on the pathway to mental health care. This will occasion samples of help-seekers enriched with schizophrenia risk at the level of mental health services (reduction of false-positive rate), while at the same time making an attempt to “attract” as many detectable schizophrenia prodromes as possible through the filters along the pathway to mental health care (reduction of false-negative rate).
Although the feasibility usefulness, and cost-effectiveness of screening and early detection remains uncertain, clinicians continue to be regularly faced with the difficult decision of whether or not to treat an early psychosis-like state. Research in early psychosis has yielded some useful suggestions in that it is becoming increasingly clear that not just psychosis by itself, but rather the clinical context of the psychotic experience determines risk for transition to schizophrenia. Thus, risk for transition to full-blown psychotic disorder is to a large degree predicted by size of psychosis “load,” comorbid distress and depression, cannabis use, cognitive ability, and subjective reports of impairment and coping.
Contributor Information
Jim Van Os, Department of Psychiatry and Neuropsychology, South Limburg Mental Health Research and Teaching Network, European Graduate School of Neuroscience, Maastricht University, The Netherlands; Division of Psychological Medicine, Institute of Psychiatry, London, UK.
Philippe Delespaul, Department of Psychiatry and Neuropsychology, South Limburg Mental Health Research and Teaching Network, European Graduate School of Neuroscience, Maastricht University, The Netherlands.
REFERENCES
- 1.McGorry PD., Yung AR., Phillips LJ. The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003;29:771–790. doi: 10.1093/oxfordjournals.schbul.a007046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warner R. Early intervention in schizophrenia: a critique. Epidemiol Psichiatr Soc. 2002;11:248–255. doi: 10.1017/s1121189x00005819. [DOI] [PubMed] [Google Scholar]
- 3.Cougnard A., Salmi LR., Verdoux H. A decade of debate on early intervention in psychosis: a systematic review of screening criteria. Schizophr Res. 2003;60:91–93. doi: 10.1016/s0920-9964(02)00202-5. [DOI] [PubMed] [Google Scholar]
- 4.Lencz T., Smith CW., Auther AM., Correll CU., Cornblatt BA. The assessment of “prodromal schizophrenia”: unresolved issues and future directions. Schizophr Bull. 2003;29:717–728. doi: 10.1093/oxfordjournals.schbul.a007041. [DOI] [PubMed] [Google Scholar]
- 5.Malla AM., Norman RM. Treating psychosis: is there more to early intervention than intervening early? Can J Psychiatry. 2001;46:645–648. doi: 10.1177/070674370104600710. [DOI] [PubMed] [Google Scholar]
- 6.McGIashan TH. Commentary: progress, issues, and implications of prodromal research: an inside view. Schizophr Bull. 2003;29:851–858. doi: 10.1093/oxfordjournals.schbul.a007051. [DOI] [PubMed] [Google Scholar]
- 7.Parnas J. From predisposition to psychosis: progression of symptoms in schizophrenia. Acta Psychiatr Scand Suppi. 1999;395:20–29. doi: 10.1111/j.1600-0447.1999.tb05979.x. [DOI] [PubMed] [Google Scholar]
- 8.Verdoux H. Have the times come for early intervention in psychosis? Acta Psychiatr Scand. 2001;103:321–322. doi: 10.1034/j.1600-0447.2001.00009.x. [DOI] [PubMed] [Google Scholar]
- 9.Offenkrantz WC., AIdrich CK. The early diagnosis of psychosis. Med Clin North Am. 1960;44:237–248. doi: 10.1016/s0025-7125(16)34069-x. [DOI] [PubMed] [Google Scholar]
- 10.Treuting TF. The early recognition of psychosis. Bull Tulane Univ Med Fac. 1953;13:33–36. [PubMed] [Google Scholar]
- 11.Hafner H., Riecher Rossler A., Maurer K., Fatkenheuer B., Loffler W. First onset and early symptomatology of schizophrenia. A chapter of epidemiological and neurobiological research into age and sex differences. Eur Arch Psychiatry Clin Neurosci. 1992;242:109–118. doi: 10.1007/BF02191557. [DOI] [PubMed] [Google Scholar]
- 12.Johannessen JO., Larsen TK., McGIashan T. Duration of untreated psychosis: an important target for intervention in schizophrenia? Nord J Psychiatry. 1999;53:275–283. [Google Scholar]
- 13.Larsen TK., McGIashan TH., Moe LC. First-episode schizophrenia: I. Early course parameters. Schizophr Bull, 1996;22:241–256. doi: 10.1093/schbul/22.2.241. [DOI] [PubMed] [Google Scholar]
- 14.Hafner H., Loffler W., Maurer K., Hambrecht M., an der Heiden W. Depression, negative symptoms, social stagnation and social decline in the early course of schizophrenia. Acta Psychiatr Scand. 1999;100:105–118. doi: 10.1111/j.1600-0447.1999.tb10831.x. [DOI] [PubMed] [Google Scholar]
- 15.Hafner H., Nowotny B. Epidemiology of early-onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1995;245:80–92. doi: 10.1007/BF02190734. [DOI] [PubMed] [Google Scholar]
- 16.Crow TJ., MacMillan JF., Johnson AL., Johnstone EC. A randomised controlled trial of prophylactic neuroleptic treatment. Br J Psychiatry. 1986;148:120–127. doi: 10.1192/bjp.148.2.120. [DOI] [PubMed] [Google Scholar]
- 17.Loebel AD., Lieberman JA., Alvir JM., Mayerhoff DI., Geisler SH., Szymanski SR. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 1992;149:1183–1188. doi: 10.1176/ajp.149.9.1183. [DOI] [PubMed] [Google Scholar]
- 18.Verdoux H., Bergey C., Assens F., et al. Prediction of duration of psychosis before first admission. Eur Psychiatry. 1998;13:346–352. doi: 10.1016/S0924-9338(99)80701-9. [DOI] [PubMed] [Google Scholar]
- 19.Verdoux H., Liraud F., Bergey C., Assens F., Abalan F., Van Os J. Is the association between duration of untreated psychosis and outcome confounded? A 2-year follow-up study of first-admitted patients. Schizophr Res. 2001;49:231–241. doi: 10.1016/s0920-9964(00)00072-4. [DOI] [PubMed] [Google Scholar]
- 20.Norman RM., Malla AK. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol Med. 2001;31:381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 21.Norman RM., Malla AK., Verdi MB., Hassall LD., Fazekas C. Understanding delay in treatment for first-episode psychosis. Psychol Med. 2004;4:255–266. doi: 10.1017/s0033291703001119. [DOI] [PubMed] [Google Scholar]
- 22.Jones P., Rodgers B., Murray R., Marmot M. Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet. 1994;344:1398–1402. doi: 10.1016/s0140-6736(94)90569-x. [DOI] [PubMed] [Google Scholar]
- 23.Isohanni M., Isohanni I., Koponen H., et al. Developmental precursors of psychosis. Curr Psychiatry Rep. 2004;6:168–175. doi: 10.1007/s11920-004-0061-5. [DOI] [PubMed] [Google Scholar]
- 24.Reichenberg A., Rabinowitz J., Weiser M., Mark M., Kaplan Z., Davidson M. Premorbid functioning in a national population of male twins discordant for psychoses. Am J Psychiatry. 2000;157:1514–1516. doi: 10.1176/appi.ajp.157.9.1514. [DOI] [PubMed] [Google Scholar]
- 25.Jones PB., Van Os J. Commentary: Behavioural and intellectual functioning in Israeli adolescent boys predicted psychiatric hospital admission for schizophrenia. Evidence-Based Ment Health. 2000;3:89. [Google Scholar]
- 26.Hafner H., Riecher-Rossler A., Hambrecht M., et al. IRAOS: an instrument for the assessment of onset and early course of schizophrenia. Schizophr Res. 1992;6:209–223. doi: 10.1016/0920-9964(92)90004-o. [DOI] [PubMed] [Google Scholar]
- 27.Hafner H., Maurer K., Loffler W., Riecher-Rossler A. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993;162:80–86. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- 28.Carr V., Halpin S., Lau N., O'Brien S., Beckmann J., Lewin T. A risk factor screening and assessment protocol for schizophrenia and related psychosis. Aust N Z J Psychiatry. 2000;34(suppI):S170–S180. doi: 10.1080/000486700240. [DOI] [PubMed] [Google Scholar]
- 29.Chapman LJ., Chapman JP., Kwapil TR., Eckblad M., Zinser MC. Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol. 1994;103:171–183. doi: 10.1037//0021-843x.103.2.171. [DOI] [PubMed] [Google Scholar]
- 30.Chapman LJ., Edell WS., Chapman JP. Physical anhedonia, perceptual aberration, and psychosis proneness. Schizophr Bull. 1980;6:639–653. doi: 10.1093/schbul/6.4.639. [DOI] [PubMed] [Google Scholar]
- 31.Jenner JA., Van De Willige G. HIT, hallucination focused integrative treatment as early intervention in psychotic adolescents with auditory hallucinations: a pilot study. Acta Psychiatr Scand. 2001;103:148–152. doi: 10.1034/j.1600-0447.2001.00189.x. [DOI] [PubMed] [Google Scholar]
- 32.Kwapil TR., Miller MB., Zinser MC., Chapman J., Chapman LJ. Magical ideation and social anhedonia as predictors of psychosis proneness: a partial replication. J Abnorm Psychol. 1997;106:491–495. doi: 10.1037//0021-843x.106.3.491. [DOI] [PubMed] [Google Scholar]
- 33.McGorry PD. The nature of schizophrenia: signposts to prevention. Aust N I J Psychiatry. 2000;34(suppI):S14–S21. doi: 10.1080/000486700217. [DOI] [PubMed] [Google Scholar]
- 34.Phillips LJ., Yung AR., McGorry PD. Identification of young people at risk of psychosis: validation of Personal Assessment and Crisis Evaluation Clinic intake criteria. Aust N 1 J Psychiatry. 2000;34(suppI):S164–S169. doi: 10.1080/000486700239. [DOI] [PubMed] [Google Scholar]
- 35.Poulton R., Caspi A., Moffitt TE., Cannon M., Murray R., Harrington H. Children's self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 36.Eaton WW., Romanoski A., Anthony JC., Nestadt G. Screening for psychosis in the general population with a self-report interview. J Nerv Ment Dis. 1991;179:689–693. doi: 10.1097/00005053-199111000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Kendler KS., Gallagher TJ., Abelson JM., Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–1031. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 38.Spauwen J., Krabbendam L., Lieb R., Wittchen HU., Van Os J. Sex differences in psychosis: normal or pathological? Schizophr Res. 2003;62:45–49. doi: 10.1016/s0920-9964(03)00063-x. [DOI] [PubMed] [Google Scholar]
- 39.Van Os J., Hanssen M., Bjjl RV., Ravelli A. Straus (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 40.Verdoux H., Maurice-Tison S., Gay B., Van Os J., Salamon R., Bourgeois ML. A survey of delusional ideation in primary-care patients. Psychol Med. 1998;28:127–134. doi: 10.1017/s0033291797005667. [DOI] [PubMed] [Google Scholar]
- 41.Tien AY., Eaton WW. Psychopathologic precursors and sociodemographic risk factors for the schizophrenia syndrome. Arch Gen Psychiatry. 1992;49:37–46. doi: 10.1001/archpsyc.1992.01820010037005. [DOI] [PubMed] [Google Scholar]
- 42.Hanssen M., Bak M., Bjjl R., VoIIebergh W., Van Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2004. In press. doi: 10.1348/014466505X29611. [DOI] [PubMed] [Google Scholar]
- 43.Johns LC., Van Os J. The continuity of psychotic experiences in the general population. Clin Psychol Rev. 2001;21:1125–1141. doi: 10.1016/s0272-7358(01)00103-9. [DOI] [PubMed] [Google Scholar]
- 44.Van Os J., Hanssen M., Bjjl RV., VoIIebergh W. Prevalence of psychotic disorder and community level of psychotic symptoms: an urban-rural comparison. Arch Gen Psychiatry. 2001;58:663–668. doi: 10.1001/archpsyc.58.7.663. [DOI] [PubMed] [Google Scholar]
- 45.Miller TJ., McGIashan TH., Rosen JL., et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 46.Yung AR., Phillips LJ., Yuen HP., et al. Psychosis prediction: 12-month follow-up of a high-risk (“prodromal”) group. Schizophr Res. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- 47.Hanssen MS., Bjjl RV., VoIIebergh W., Van Os J. Self-reported psychotic experiences in the general population: a valid screening tool for DSM-III-R psychotic disorders? Acta Psychiatr Scand. 2003;107:369–377. doi: 10.1034/j.1600-0447.2003.00058.x. [DOI] [PubMed] [Google Scholar]
- 48.Marie N., Myin-Germeys I., Delespaul P., De Graaf R., VoIIebergh W., Van Os J. Is our concept of schizophrenia influenced by Berkson's bias? Social Psychiatry Psychiatr Epidemiol. 2004;39:600–605. doi: 10.1007/s00127-004-0803-z. [DOI] [PubMed] [Google Scholar]
- 49.Sackett DL., Richardson WS., Rosenberg W., Haynes RB. Evidence-Based Medicine. New York, NY: Churchill Livingstone; 1997 [Google Scholar]
- 50.Hennekens CH., Buring JE. Screening. In: Hennekens CH, Buring JE, eds. Epidemiology in Medicine. Toronto, Canada: Little, Brown and Company; 1987 [Google Scholar]
- 51.Bentall RP., Morrison AP. More harm than good: the case against using antipsychotic drugs to prevent severe mental illness. J Ment Health. 2002;11:351–356. [Google Scholar]
- 52.McGuire PK. Prodromal intervention: the need for evaluation. A reply to Bentall and Morrison. J Ment Health. 2002;114:469–470. [Google Scholar]
- 53.Warner R. Fact versus fantasy: a reply to Bentall and Morrison. J Ment Health. 2003;12:351–357. [Google Scholar]
- 54.Marshall M., Lockwood A. Early intervention for psychosis. Cochrane Database Syst Rev. 2004:CD004718. doi: 10.1002/14651858.CD004718. [DOI] [PubMed] [Google Scholar]
- 55.Bak M., Myin-Germeys I., Hanssen M., et al. When does experience of psychosis result in a need for care? A prospective general population study. Schizophr Bull. 2003;29:349–358. doi: 10.1093/oxfordjournals.schbul.a007010. [DOI] [PubMed] [Google Scholar]
- 56.Garety PA., Kuipers E., Fowler D., Freeman D., Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 57.Krabbendam L., Janssen I., Bak M., Bjjl RV., de Graff R., Van Os J. Neuroticism and low self-esteem as risk factors for psychosis. Social Psychiatry Psychiatr Epidemiol. 2002;37:1–6. doi: 10.1007/s127-002-8207-y. [DOI] [PubMed] [Google Scholar]
- 58.Krabbendam L., Myin-Germeys I., Hanssen M., De Graaf R., VoIIebergh W., Bak M., Van Os J. Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. Br J Clin Psychol. 2004. In press doi: 10.1348/014466504X19767. [DOI] [PubMed] [Google Scholar]
- 59.Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 60.Van Os J., Bak M., Hanssen M., Bjjl RV., de Graaf R., Verdoux H. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol. 2002;156:319–327. doi: 10.1093/aje/kwf043. [DOI] [PubMed] [Google Scholar]
- 61.Van Os J., Hanssen M., Bak M., Bjjl RV., VoIIebergh W. Do urbanicity and familial liability coparticipate in causing psychosis? Am J Psychiatry. 2003;160:477–482. doi: 10.1176/appi.ajp.160.3.477. [DOI] [PubMed] [Google Scholar]
- 62.Davidson M., Reichenberg A., Rabinowitz J., Weiser M., Kaplan Z., Mark M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry. 1999;56:1328–1335. doi: 10.1176/ajp.156.9.1328. [DOI] [PubMed] [Google Scholar]
- 63.Klosterkotter J., Hellmich M., Steinmeyer EM., Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry. 2001;58:158–164. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- 64.Huber G. [Prodromal symptoms in schizophrenia]. Fortsch Neurol Psychiatr. 1995;63:131–138. doi: 10.1055/s-2007-996611. [DOI] [PubMed] [Google Scholar]
- 65.StataCorp STATA Statistical Software: Release 8.0. Texas: College Station; 2002 [Google Scholar]
- 66.Van Os J., Takei N., Verdoux H., Delespaul P. Early detection of schizophrenia [letter]. Br J Psychiatry. 1997;170:579. doi: 10.1192/bjp.170.6.579a. [DOI] [PubMed] [Google Scholar]
- 67.Kuipers E., HoIIoway F., Rabe-Hesketh S., Tennakoon L. An RCT of early intervention in psychosis: Croydon Outreach and Assertive Support Team (COAST). Soc Psychiatry Psychiatr Epidemiol. 2004;39:358–363. doi: 10.1007/s00127-004-0754-4. [DOI] [PubMed] [Google Scholar]
- 68.Rose G. The Strategy of Prevention. Oxford, UK: Oxford Medical Publications;1992 [Google Scholar]
- 69.Goldberg D., Huxley P. Mental Illness in the Community. London, UK: Tavistock Publications; 1980 [Google Scholar]
- 70.Johannessen JO. Early intervention and prevention in schizophrenia experiences from a study in Stavanger, Norway. Seishin Shinkeigaku Zasshi Psychiatr Neurol Jpn. 1998;100:511–522. [PubMed] [Google Scholar]
- 71.Johannessen JO., McGIashan TH., Larsen TK., et al. Early detection strategies for untreated first-episode psychosis. Schizophr Res. 2001;51:39–46. doi: 10.1016/s0920-9964(01)00237-7. [DOI] [PubMed] [Google Scholar]
- 72.Carbone S., Harrigan S., McGorry PD., Curry C., EIkins K. Duration of untreated psychosis and 12-month outcome in first-episode psychosis: the impact of treatment approach [see comments]. Acta Psychiatr Scand. 1999;100:96–104. doi: 10.1111/j.1600-0447.1999.tb10830.x. [DOI] [PubMed] [Google Scholar]
- 73.Malla A., Norman R., McLean T., Scholten D., Townsend L. A Canadian programme for early intervention in non-affective psychotic disorders. Aust N Z J Psychiatry. 2003;37:407–413. doi: 10.1046/j.1440-1614.2003.01194.x. [DOI] [PubMed] [Google Scholar]
- 74.Bak M., Delespaul P., Hanssen M., de Graaf R., VoIIebergh W., van Os J. How false are “false” positive psychotic symptoms? Schizophr Res. 2003;62:187–189. doi: 10.1016/s0920-9964(02)00336-5. [DOI] [PubMed] [Google Scholar]
- 75.Bak M., Radstake S., Van Os J. Consultatie aan huisartsen ter detectie van zorgvermjjdende mensen met een psychose. Maandblad Geestelijke Volksgezondheid. 1999;54:1281–1289. [Google Scholar]
- 76.Jones PB., Tarrant CJ. Developmental precursors and biological markers for schizophrenia and affective disorders: specificity and public health implications. Eur Arch Psychiatry Clin Neurosci. 2000;250:286–291. doi: 10.1007/s004060070003. [DOI] [PubMed] [Google Scholar]
- 77.Hanssen M., Peeters F., Krabbendam L., Radstake S., Verdoux H., Van Os J. How psychotic are individuals with non-psychotic disorders? Social Psychiatry Psychiatr Epidemiol. 2003;38:149–154. doi: 10.1007/s00127-003-0622-7. [DOI] [PubMed] [Google Scholar]
- 78.Van Os J., Verdoux H., Maurice-Tison S., et al. Self-reported psychosis-like symptoms and the continuum of psychosis. Social Psychiatry Psychiatr Epidemiol. 1999;34:459–463. doi: 10.1007/s001270050220. [DOI] [PubMed] [Google Scholar]