Abstract
The persistence of attention deficit hyperactivity disorder (ADHD) into adolescence and adulthood has now been accepted as a clinical entity. The rate of prevalence among adults is assumed to be from 2% to 4%. With increasing age, a symptom change has to be considered; disturbance of attention becomes more prominent, whereas hyperactivity often diminishes or changes to inactivity. Neuroimaging studies show a high striatal dopamine transporter (DAT) availability in most adults with ADHD; this can be reduced by stimulants. Nicotine seems to have a stimulant-like action on the DAT. In most adults with ADHD, therapy has to be multimodal, combining psychotherapy and medication. Methylphenidate is the first-line drug in adult ADHD; further options are amphetamine and noradrenaline reuptake inhibitors. Nonresponders to methylphenidate seem to have no elevated DAT availability prior to therapy. Combination with other psychiatric disorders occurs frequently in adults with ADHD; in these patients additional pharmacological treatment with special regard to the comorbid disease is recommended.
Keywords: attention deficit hyperactivity disorder, adolescence, adulthood, brain imaging techniques, single photon emission computed tomography, dopamine transporter, nicotine, diagnosis, therapy, methylphenidate
Abstract
Hoy, se acepta que el trastorno de hiperactividad con déficit de atención (THDA) puede persistir como entidad clínica hasta la adolescencia y vida adulta. La tasa de prevalencia entre los adultos varía entre el 2% y el 4%, Con el envejecimiento se produce un cambio sintomático; el trastorno de atención se agudiza, mientras que la hiperactividad suele disminuir o se torna en inactividad. Los estudios de neuroimagen revelan una gran disponibilidad del transportador de dopamina del estriado (DAT) entre la mayoría de los adultos con THDA; los estimulantes reducen su concentración. Al parecer, la nicotina estimula el DAT. El tratamiento de la mayoría de los adultos con THDA es multimodal - combinación de psicoterapia y medicación. El metilfenidato es el farmaco preferido para el THDA del adulto; otras posibilidades son la anfetamina y los inhibidores de la recaptación de noradrenalina. Al parecer, las personas que no responden al metilfenidato no muestran una disponibilidad elevada de DAT antes del tratamiento. Los adultos con THDA suelen padecer otros trastornos psiquiátricos; se recomienda un tratamiento farmacológico adicional de estos pacientes, prestando especial atención a la enfermedad asociada.
Abstract
La persistance d'un trouble d'hyperactivité et d'un déficit de l'attention à l'adolescence et à l'âge adulte (HADA) est maintenant acceptée en tant qu'entité clinique. La prévalence chez les adultes est estimée entre 2 et 4 %. Il faut tenir compte des symptômes qui se modifient avec l'âge: le trouble de l'attention s'aggrave alors que souvent l'hyperactivité diminue ou se mue en inactivité. Les études de neuro-imagerie montrent une présence striatale élevée du transporteur de la dopamine (TD) chez la plupart des adultes atteints de HADA, qui peut être diminuée par des stimulants, La nicotine semble avoir la même action sur le TD que les stimulants. Chez la plupart des adultes souffrant de HADA, le traitement doit être multimodal, associant psychothérapie et médicaments. Le methylphenidate est le traitement de première intention chez l'adulte souffrant de HADA ; les autres choix sont les amphétamines et les inhibiteurs de la recapture de la noradrenaline. Le taux de TD avant le traitement ne semble pas élevé chez les nonrépondeurs au methylphenidate. D'autres troubles psychiatriques sont souvent associés au HADA chez l'adulte ; chez ces patients il est recommandé de traiter le trouble comorbide.
Attention deficit/hyperactivity disorder (ADHD) is the most common psychiatric disorder of childhood. In recent years there has been growing evidence that in many patients the disorder persists into adulthood. Meanwhile, adult ADHD has been recognized in the literature as a valid clinical entity, affecting as many as 2% to 4% of adults.1
Symptomatology and diagnosis
The core symptoms of ADHD are inattention, hyperactivity, and impulsivity.2 In most descriptions of ADHD in the 1980s and the early 1990s, it seemed that hyperactivity had to be present in every case as a striking symptom, but with growing knowledge of ADHD it became evident that not all patients-in particular girls-present hyperactivity. Since 1994, with the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM IV)3 three types of ADHD have been differentiated:
Combined type (6 or more symptoms of hyperactivity/impulsivity as well as of inattention);
Inattentive type (6 or more symptoms of inattention);
Hyperactive/impulsive type (6 or more symptoms of hyperactivity/impulsivity).
A change in symptoms with increasing age is characteristic of ADHD. After puberty, hyperactivity often changes to inactivity; therefore, ADHD often is not accepted as a diagnosis in adults. Impulsivity normally lessens with age. Adults with ADHD seem to have a problem with willpower: activity can be overexerted, but if a task is not attractive to the person, this results in a lack of effort. Or, inattention can change to hyperfocussing, when the person is attracted by a task.
With adults, differing patterns of comorbidity and symptom heterogeneity pose new conceptual, diagnostic, and treatment challenges. While core symptoms are often overt problems in children, in adults subtler executive dysfunction appears. Even though the growing consensus is that ADHD is a disorder of executive functions (EF), the details of the EF/ADHD connection remain unclear and may be far more complex in adults.4
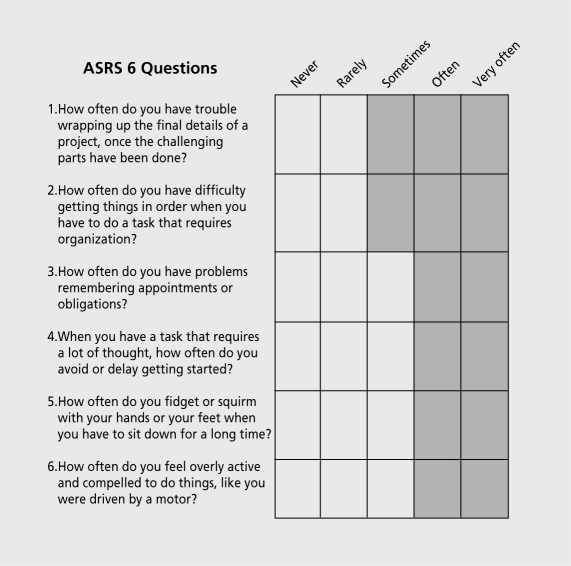
In Table I examples are given for the changes of the 18 DSM-IV symptoms from childhood to adulthood. The 6-question Adult Self-Report Scale -V1.1 (ASRS - V 1.1) Screener (http://www.hcp.med.harvard.edu/ncs/fpdir/adhd) is a subset of the WHO'S 18-question Adult Self- Report Scale - V1.1 (ASRS - V1.1) Symptom Checklist. The patient should fill in checkmarks. Four or more checkmarks in the darkly shaded areas may indicate that the symptoms are consistent with adult ADHD (Figure 1).
Figure 1. Adult Self-Report Scale (ASRS) Screener: 4 or more check-marks in the shaded areas may indicate symptoms of adult ADHD. ADHD, attention deficit hyperactivity disorder.
TABLE I. Comparison of ADHD symptoms in adulthood according to ASRS (http://www.med.nyu.edu/psych/assets/adhdscreen18.pdf.) in the left column and in childhood according to DSM-IV3 in the right column. ADHD, attention deficit hyperactivity disorder.
| 1. How often do you have trouble wrapping up the final details of | Often does not follow through on instructions and fails to finish |
| a project, once the challenging parts have been done? | schoolwork, chores, or duties in the workplace (and due to |
| oppositional behavior or failure to understand instructions) | |
| 2. How often do you have difficulty getting things in order when | Often has difficulty organizing tasks and activities |
| you have to do a task that requires organization? | |
| 3. How often do you have problems remembering appointments | is often forgetful in daily activities |
| or obligations? | |
| 4. When you have a task that requires a lot of thought, how often | Often avoids, dislikes, or is reluctant to engage in tasks that require |
| do you avoid or delay getting started? | sustained mental effort {such as schoolwork or homework) |
| 5. How often do you fidget or squirm with your hands or feet | Often fidgets with hands or feet or squirms in seat |
| when you have to sit down for a long time? | |
| 6. How often do you feel overly active and compelled to do things. | Is often "on the go" or often acts as if "driven by a motor" |
| like you were driven by a motor? | |
| 7. How often do you make careless mistakes when you have to | Often fails to give close attention to details or makes careless |
| work on a boring or difficult project? | mistakes in schoolwork. work, or other activities |
| 8. How often do you have difficulty keeping your attention when | Often has difficulty sustaining attention in tasks or play activities |
| you are doing boring or repetitive work? | |
| 9. How often do you have difficulty concentrating on what people | Often does not seem to listen when spoken to directly |
| say to you, even when they are speaking to you directly? | |
| 10. How often do you misplace or have difficulty finding things at | Often loses things necessary for tasks or activities (eg, toys. |
| home or at work? | school assignments, pencils, books, or tools) |
| 11. How often are you distracted by activity or noise around you? | Is often easily distracted by extraneous stimuli |
| 12. How often do you leave your seat in meetings or other | Often leaves seat in classroom or in other situations in which |
| situations in which you are expected to remain seated? | remaining seated is expected |
| 13. How often do you fee! restless or fidgety? | Often runs about or climbs excessively in situations in which it is |
| inappropriate (in adolescents or adults, may be limited to subjective | |
| feelings of restlessness) | |
| 14. How often do you have difficulty unwinding and relaxing | Often has difficulty playing or engaging in leisure activities quietly |
| when you have time to yourself? | |
| 15. How often do you find yourself talking too much when you | Often talks excessively |
| are in social situations? | |
| 16. When you're in a conversation, how often do you find yourself | Often blurts out answers before questions have been completed |
| finishing the sentences of the people you are talking to, before | |
| they can finish them themselves? | |
| 17. How often do you have difficulty waiting your turn in situations | Often has difficulty awaiting turn |
| when turn taking is required? | |
| 18. How often do you interrupt others when they are busy? | Often interrupts or intrudes on others (eg, butts into conversations |
| or games) |
Wender developed a set of characteristics to specify both childhood criteria and current ADHD symptoms.5 He pointed out affective lability, which is not mentioned in DSM-IV, as a frequent symptom in adult ADHD.
Prevalence of AI adulthood
The prevalence of ADHD in children according to DSM-IV criteria varies from 2.4% to 19.8%.6 Concerning persistence into adulthood, most authors describe a rate of about 50%. The largest follow-up study, which investigated 197 Chinese children after 15 years, showed a rate of persistence of 70%:7,8 Generally, the degree of prevalence (1 % to 6% in adults) depends on the view of the reporter in the initial assessment. Most instruments consist of some form of self-report, and in adulthood it is often not possible to ask information of parents or persons with a close relationship to the patient. Patients with ADHD are often not aware of their symptoms, or do not report the severity of symptoms.
Neurobiological basis of ADHD
Current interest in the neurobiological basis of ADHD originally commenced in the 1970s. Neurochemical, neurophysiological, and radiological attributes were noted, proving, in particular, abnormalities in the dopaminergic and noradrenergic system. Genetic investigations showed increased evidence that genetic components were present in most cases of ADHD, which is now seen as the psychiatric disease with the highest heritability.9
Neuroimaging studies with magnetic resonance imaging (MRI), photon-emission tomography (PET), and single photon-emission computed tomography (SPECT) suggest involvement of striatal structures in ADHD.10-13 Molecular genetic studies described an involvement of a polymorphism of the dopamine transporter (DAT) 1 gene in ADHD (eg, a higher rate of homozygosity of the 10-repeat allele in the 3 'untranslated region of exon 15 of the DAT gene on chromosome 5p15.3).14-19
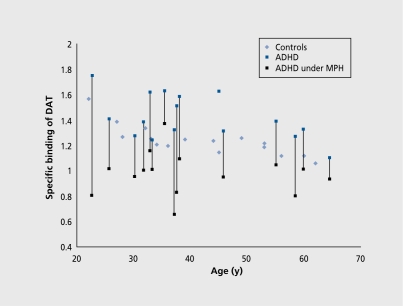
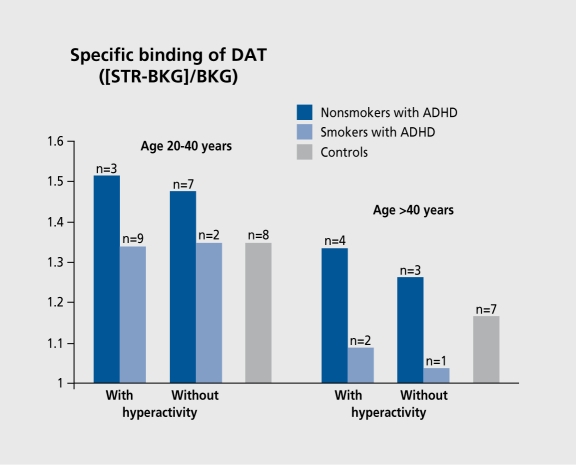
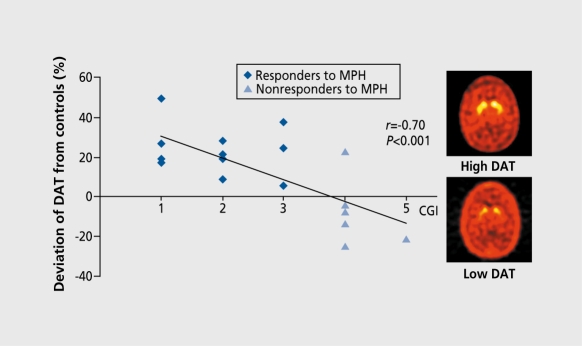
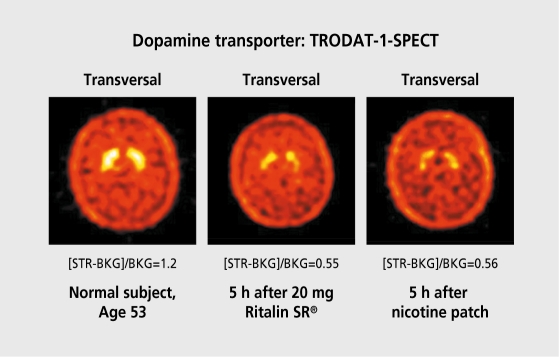
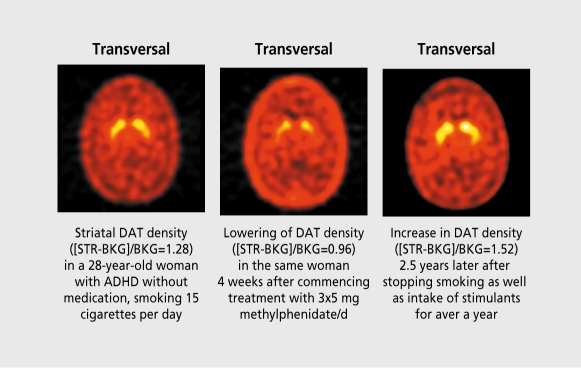
With regard to the suspected striatal impairment in ADHD and the known effect of methylphenidate on the DAT mainly localized in this section of the brain, since the end of the 1990s DAT has been investigated in patients with ADHD. This is carried out by using radioactive marked ligands which are known to bind effectively with the DAT system. A group of investigators from Boston used altropane marked with iodine-12320; our group from Munich and Philadelphia used the cocaine derivative TRODAT-1 marked with technetium 99m.21 Both studies showed a clearly higher availability of DAT in the striatum of adult patients with ADHD compared with the normal healthy controls.20-23 While DAT availability was found to be raised to 17% in the investigations using TRODAT-1 compared with the control collective (Figure 2), the group using altropane demonstrated a rise of 70% in 6 patients; this percentage was reduced to around 30% in a larger group of 19 patients on continuation of the altropane study (Spencer T, personal communication). Meanwhile, a rise in DAT availability was also detected in the basal ganglia of children with ADHD by means of an [123I] N-(3-iodopropen-2-yl)-2-carbo-methoxy-3β-(4-chlorphenyl) tropane (IPT)-SPECT investigation,24 following initial results with N-δ-fluoropropyl-2 β-carboxymethoxy-3 β-{4-iodophenyl} tropane (FP-CIT).25 Interestingly, a rise in the DAT could not, be detected in a SPECT investigation with β-CIT26; this could be due to the extremely slow kinetics of β-CIT (measurement 1 day after application) or another specificity of this radiotracer, which also binds with serotonin transporters and possibly holds other substructures of DAT compared with altropane, FP-CIT, IPT, or TRODAT-1. Our own initial results revealed that the DAT was raised not. only in the hyperactive-impulsive and combined type, but also in the inattentive type of ADHD (Figure 3). It, may be deduced from a neurochemical view that with an increase in DAT, which transports dopamine back from the synaptic cleft, less dopamine is available in the synaptic cleft of dopamine-dependent neurons. The results obtained by our group showed not, only the impairment of DAT but also reported for the first, time in vivo and intraindividually in patients with ADHD, that impaired metabolism can be improved with methylphenidate: on administration of 5 mg 3 times daily it was seen that there was a clear reduction in DAT availability in all patients after a period of 4 weeks (Figure 2).22,23 With this very low dose, most of these patients demonstrated a lower concentration of DAT than did the control group. In a study involving six children with ADHD, an IPT-SPECT investigation confirmed a marked reduction in DAT density under administration of methylphenidate.27 Regarding normal healthy individuals, other authors were able to show evidence of a similar reduction in DAT under methylphenidate in a PET investigation with [C-ll] cocaine.28 In conclusion, the SPECT investigations on DAT confirmed the supposition that with ADHD an impairment is present mainly in the dopaminergic system. This can be improved with the introduction of stimulants. Our initial results show that, nonresponders to methylphenidate do not reveal raised DAT in striatum prior to therapy, whereas the responders seem to have a high DAT availability (Figure 4).29
Figure 2. DAT availability in striatum, measured with TRODAT-1 SPECT, in 17 adults with ADHD before and after (in 16 patients) 4 weeks of intake of 5 mg methylphenidate 3 times daily, compared with 16 controls, and in relation to age. DAT, dopamine transporter; SPECT, single photon emission computed tomography; ADHD, attention deficit hyperactivity disorder.
Figure 3. DAT availability in the striatum of smoking and nonsmoking adults with ADHD with only inattentive symptoms since childhood and with hyperactivity/impulsivity in the childhood, mostly in combination with attention deficit and in nonsmoking controls, shown by specific accumulation of [Tc-99m]TRODAT-1 in SPECT scans, in the age groups of 20 to 40 years and over 40 years. DAT, dopamine transporter; ADHD, attention deficit hyperactivity disorder; SPECT, single photon emission computed tomography; STR, specific binding in striatum; BKG, specific binding in the cerebellum as background. Reproduced from reference 12: Krause KH, Dresel SH, Krause J, la Fougère C, Ackenheil M. The dopamine transporter and neuroimaging in attention deficit hyperactivity disorder. Neurosci Biobehav Rev. 2003;27:605-613. Copyright © Elsevier 2003.
Figure 4. Specific binding of striatal DAT, measured with [99mTc]TRODAT-1 SPECT in 1 8 adults with ADHD (percentage of deviation from values of controls of the same age) in relation to CGI values after 10 weeks of intake of methylphenidate. DAT, dopamine transporter; SPECT, single photon emission computed tomography; ADHD, attention deficit hyperactivity disorder.
It should be noted, for possible diagnostic applications of SPECT, that the DAT concentration decreases with increase of age30 and that nicotine may influence DAT availability.12 The lowering of DAT with increasing age may be an explanation for our observation, that most, adults need lower doses of methylphenidate compared with children and adolescents. Nicotine seems to have a similar effect on the DAT as do stimulants (Figure 3). Investigating potential reasons for the lower elevation in the TRODAT-1 study compared with the altropane study, we found a subgroup of patients with relatively little increase in DAT despite severe clinical impairments; further questioning of these patients revealed that all of them were cigarette smokers. Comparison of 11 smoking nonmedicated patients with ADHD with sex- and agematched nonsmoking drug-naive adults with ADHD showed significantly higher DAT density in the nonsmoking patients, despite higher ADHD scores for the smokers.31 This finding suggests that nicotine may act, directly on DAT in the same manner as stimulants. In a self-trial, DAT availability was reduced by over 50% 5 hours after intake of 20 mg methylphenidate in a slow-release formulation; wearing a nicotine skin patch, equaling 10 to 20 cigarettes daily, for 5 hours. In the same subject 3 months later, an effect similar to that of methylphenidate was seen (Figure 5), confirming the view that the lowering of DAT after use of nicotine is not a sign of a neurochemical adaptation associated with chronic exposure to nicotine.12 Further evidence comes from the reevaluation of a woman with ADHD, who was smoking 15 cigarettes per day at, the time of first investigation with TRODAT-1, showing no remarkable elevation of DAT; 4 weeks of intake of 3x5 mg methylphenidate led to a marked reduction similar to the other patients in this group. One year later, the patient stopped the nicotine and methylphenidate intake; 2 years after the first investigation she returned with increased complaints of ADHD. At this time she underwent another TRODAT-1 SPECT scan, presenting with a 19% elevation compared with the first scan with nicotine and a 61 % elevation compared with the second scan with nicotine and methylphenidate (Figure 6). This finding is in accordance with the opinion that, the effect, of nicotine on DAT does not result, in a persistent, loss of DAT.32 In this context, it is of interest that an investigation with [123I]β-CIT SPECT showed no altered striatal uptake in smokers versus controls,33 a potential parallel to the above mentioned findings of no DAT elevation in ADHD with this method.
Figure 5. DAT availability in the striatum of a 53-year-old nonsmoker before (A), after 5 hours of intake of 20 mg methylphenidate (Ritalin SR®) (B), and 3 months later after 5 hours of wearing a 17.5 mg/24 h nicotine skin patch (C), shown by specific accumulation of [Tc-99m]TRODAT-1 in SPECT scans. DAT, dopamine transporter; SPECT, single photon emission computed tomography; STR, specific binding in striatum; BKG, specific binding in the cerebellum as background. Reproduced from reference 12: Krause KH, Dresel SH, Krause J, la Fougère C, Ackenheil M. The dopamine transporter and neuroimaging in attention deficit hyperactivity disorder. Neurosci Biobehav Rev. 2003;27:605-613. Copyright © Elsevier 2003.
Figure 6. DAT availability in the striatum of a 29-year-old female smoker with ADHD before (A), after 4 weeks of intake of 3x5 mg methylphenidate (Ritalin®) per day (B), and 2 years later after 1 year of cessation of nicotine abuse and intake of methylphenidate, shown by specific accumulation of [Tc99m]TRODAT-1 in SPECT scans. DAT, dopamine transporter; ADHD, attention deficit hyperactivity disorder; SPECT, single photon emission computed tomography; STR, specific binding in striatum; BKG, specific binding in the cerebellum as background. Reproduced from reference 12: Krause KH, Dresel SH, Krause J, la Fougère C, Ackenheil M. The dopamine transporter and neuroimaging in attention deficit hyperactivity disorder. Neurosci Biobehav Rev. 2003;27:605-613. Copyright © Elsevier 2003.
Treatment of adults
Most patients need multimodal therapy: psychoeducation concerning the special aspects of ADHD is essential. Many patients have problems with their self-esteem due to a misunderstanding of the symptoms and a childhood with parents suffering from ADHD-especially impulsivity-and they need additional psychotherapy.
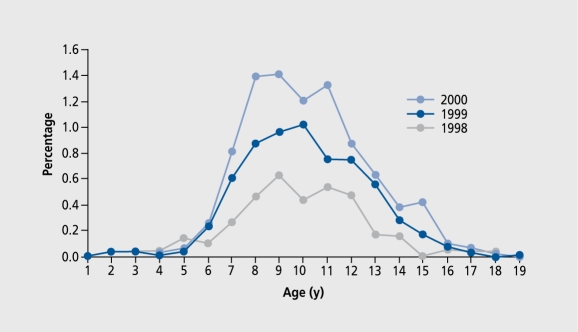
Treatment with stimulants is the drug therapy of first choice34 and is approved in the USA for adults (dmethylphenidate and amphetamines); stimulants for adult ADHD are as effective as in children. An investigation performed in the year 2000 in Germany showed that only 0.024‰ of the adults registered in the public health system - that is 90% of the adult, population - was treated with methylphenidate in Germany at, this time (Figure 7).35 That is about one out of 40 000 and includes all kinds of treatments, including for narcolepsy and other psychiatric diseases.
Figure 7. Percentage of patients treated with methylphenidate in relation to age in the years 1998 (N=65 412), 1999 (N=64 701) and 2000 (N=63 115) in a German district. Reproduced from reference 35: Ferber L v, Lehmkuhl G, Köster I, et al. Methylphenidatgebrauch in Deutschland: Versichertenbezogene epidemiologische Studie uber die Entwicklung von 1998 bis 2000. Dtsch Ärztebl. 2003;100:A41-46. Copyright © Deutsches Arzeblatt 2003.
In the treatment, of adults with ADHD we start with a daily dose of 5 mg, reaching 15 mg methylphenidate after 14 days of treatment. Titration up to 40 mg follows, if the patient needs more than the initial end point of the 15mg dose. But more than 70% of our patients did not tolerate doses above 30 mg without having marked side effects. Frequently, they felt an increased inner tension. With higher doses, they also described a state resembling the impairments they experienced before the treatment. Most, of them had a good stabilization with a combination of methylphenidate in a dose up to 20 mg and additional antidepressants.
With all patients we try to start monotherapy with stimulants. When methylphenidate has no positive effect on depressive or other comorbid symptoms, we start an additional medication after 4 weeks of treatment. Some patients do not tolerate methylphenidate well; they feel more depressed after starting the methylphenidate medication, but they are not as inattentive as before the beginning of therapy; in this situation we change from methylphenidate to amphetamines; some patients have more benefits from this kind of stimulants acting in dual ways. When selecting the additional medication it, is important to regard the comorbid disorder. We experienced good clinical response with the following medication:
Depression: venlafaxine 18.75-150 mg/d
Depression combined with severe distraction: amisulpride 25 - 100 mg/d
OCD: sertraline 50-100 mg/d
Borderline syndrome: venlafaxine 37.5 mg -150 mg/d
Slight autistic symptoms: fluoxetine 10-20 mg/d
The use of tricyclic antidepressants is problematic, as the long-term effect is not as good as that of treatment with new antidepressants. The change seems to take place after 3 months. The side effects often lead to treatment dropouts. In recent years the norepinephrine reuptake inhibitor atomoxetine was introduced as an additional possibility to treat ADHD.36 This substance does not influence the dopamine in the striatum, but in the prefrontal cortex, where dopamine transport is mediated by norepinephrine transporter.37
Selected abbreviations and acronyms
- ADHD
attention deficit hyperactivity disorder
- DAT
dopamine transporter
- MRI
magnetic resonance imaging
- PET
photon-emission tomography
- SPECT
single photon-emission computed tomography
Contributor Information
Johanna Krause, Outpatient Clinic for Psychiatry and Psychotherapy, Ottobrunn, Germany; Ludwig-Maximilians-University, D-80336 Munich, Germany.
Klaus-Henning Krause, Friedrich-Baur-lnstitute, Ludwig-Maximilians-University, Munich, Germany.
Stefan H. Dresel, Department of Nuclear Medicine; Ludwig-Maximilians-University, D-80336 Munich, Germany.
Christian la Fougère, Department of Nuclear Medicine; Ludwig-Maximilians-University, D-80336 Munich, Germany.
Manfred Ackenheil, Department of Neurochemistry; Ludwig-Maximilians-University, D-80336 Munich, Germany.
REFERENCES
- 1.Spencer T., Biederman J., Wilens T., et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry: 2005;57:456–463. doi: 10.1016/j.biopsych.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 2.Swanson JM., Sergeant JA., Taylor E., Sonuga-Barke EJ., Jensen PS., Cantwell DP. Attention-deficit hyperactivity disorder and hyperkinetic disorder. Lancet. 1998;351:429–433. [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- 4.Wolf LE., Wasserstein J. Adult ADHD. Concluding thoughts. Ann N Y Acad Sci. 2001;931:396–408. [PubMed] [Google Scholar]
- 5.Wender PH. Attention-Deficit Hyperactivity Disorder in Adults. New York, NY, Oxford, UK: Oxford University Press; 1995 [Google Scholar]
- 6.Faraone SV., Sergeant J., Gillberg C., Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2:104–113. [PMC free article] [PubMed] [Google Scholar]
- 7.Yan W. An investigation of adult outcome of hyperactive children in Shanghai. Chin MedJ. 1996;109:877–880. [PubMed] [Google Scholar]
- 8.Yan W. An investigation of adult outcome of hyperactive children in Shanghai. Psychiatry Clin Neurosci. 1998;52(suppl):S303–S305. doi: 10.1111/j.1440-1819.1998.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 9.Faraone SV. Genetics of childhood disorders: XX. ADHD, Part 4: is ADHD genetically heterogeneous? J Am Acad Child Adolesc Psychiatry. 2000;39:1455–1457. doi: 10.1097/00004583-200011000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Bush G., Valera EM., Seidman U. Functional neuroimaging of attention-deficit/hyperactivity disorder: a review and suggested future directions. Biol Psychiatry. 2005;57:1273–1284. doi: 10.1016/j.biopsych.2005.01.034. [DOI] [PubMed] [Google Scholar]
- 11.Castellanos FX., Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nature Rev Neurosci. 2002;3:617–628. doi: 10.1038/nrn896. [DOI] [PubMed] [Google Scholar]
- 12.Krause KH., Dresel SH., Krause J., la Fougère C., Ackenheil M. The dopamine transporter and neuroimaging in attention deficit hyperactivity disorder. Neurosci Biobehav Rev. 2003;27:605–613. doi: 10.1016/j.neubiorev.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 13.Spencer TJ., Biederman J., Madras BK., et al. In vivo neuroreceptor imaging in attention-deficit/hyperactivity disorder: a focus on the dopamine transporter. Biol Psychiatry. 2005;57:1293–1300. doi: 10.1016/j.biopsych.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 14.Chen CK., Chen SL., Mill J., et al. The dopamine transporter gene is associated with attention deficit hyperactivity disorder in a Taiwanese sample. Mol Psychiatry. 2003;8:393–396. doi: 10.1038/sj.mp.4001238. [DOI] [PubMed] [Google Scholar]
- 15.Cook EH Jr., Stein MA., Krasowski MD., et al. Association of attention-deficit disorder and the dopamine transporter gene. Aw J Hum Genet. 1995;56:993–998. [PMC free article] [PubMed] [Google Scholar]
- 16.Cornish KM., Manly T., Savage R., et al. Association of the dopamine transporter (DAT1) 10/10-repeat genotype with ADHD symptoms and response inhibition in a general population sample. Mol Psychiatry. 2005;10:686–698. doi: 10.1038/sj.mp.4001641. [DOI] [PubMed] [Google Scholar]
- 17.Faraone SV., Perlis RH., Doyle AE., et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57:1313–1323. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 18.Gill M., Daly G., Heron S., Hawi Z., Fitzgerald M. Confirmation of association between attention deficit hyperactivity disorder and a dopamine transporter polymorphism. Mol Psychiatry. 1997;2:311–313. doi: 10.1038/sj.mp.4000290. [DOI] [PubMed] [Google Scholar]
- 19.Waldman ID., Rowe DC., Abramowitz A., et al. Association and linkage of the dopamine transporter gene and attention-deficit hyperactivity disorder in children: Heterogeneity owing to diagnostic subtype and severity. Am J Hum Genet. 1998;63:1767–1776. doi: 10.1086/302132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dougherty DD., Bonab AA., Spencer TJ., Rauch SL., Madras BK., Fischman AJ. Dopamine transporter availability in patients with attention deficit hyperactivity disorder. Lancet. 1999;354:2132–2133. doi: 10.1016/S0140-6736(99)04030-1. [DOI] [PubMed] [Google Scholar]
- 21.Dresel SH., Kung MP., Plossl K., Meegalla SK., Kung HF. Pharmacological effects of dopaminergic drugs on in vivo binding of [99mTc]TRODAT-1 to the central dopamine transporters in rats. Eur J Nucl Med. 1998;25:31–39. doi: 10.1007/s002590050191. [DOI] [PubMed] [Google Scholar]
- 22.Dresel S., Krause J., Krause KH., et al. Attention deficit hyperactivity disorder: binding of [99mTc]TRODAT-1 to the dopamine transporter before and after methylphenidate treatment. Eur J Nucl Med. 2000;27:1518–1524. doi: 10.1007/s002590000330. [DOI] [PubMed] [Google Scholar]
- 23.Krause KH., Dresel SH., Krause J., Kung HF., Tatsch K. Increased striatal dopamine transporter in adult patients with attention deficit hyperactivity disorder: effects of methylphenidate as measured by single photon emission computed tomography. Neurosci Lett. 2000;285:107–110. doi: 10.1016/s0304-3940(00)01040-5. [DOI] [PubMed] [Google Scholar]
- 24.Cheon KA., Ryu YH., Kim JW., Cho DY. The homozygosity for 10-repeat allele at dopamine transporter gene and dopamine transporter density in Korean children with attention deficit hyperactivity disorder: relating to treatment response to methylphenidate. Eur Neuropsychopharmacol. 2005;15:95–101. doi: 10.1016/j.euroneuro.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 25.AI Younis ICH. Attention deficit hyperactivity disorder: neuroimaging before and after treatment with methylphenidate in children. J Nucl Med. 2002;43(suppl 5):347P. [Google Scholar]
- 26.van Dyck CH., Quinlan DM., Cretella LM., et al. Unaltered dopamine transporter availability in adult attention deficit hyperactivity disorder. Am J Psychiatry. 2002;159:309–312. doi: 10.1176/appi.ajp.159.2.309. [DOI] [PubMed] [Google Scholar]
- 27.Vies JS., Feron FJ., Hendriksen JG., Jolies J., van Kroonenburgh MJ., Weber WE. Methylphenidate down-regulates the dopamine receptor and transporter system in children with attention deficit hyperkinetic disorder (ADHD). Neuropediatrics. 2003;34:77–80. doi: 10.1055/s-2003-39602. [DOI] [PubMed] [Google Scholar]
- 28.Volkow ND., Wang GJ., Fowler JS., et al. Dopamine transporter occupancies in the human brain induced by therapeutic doses of oral methylphenidate. Am J Psychiatry. 1998;155:1325–1331. doi: 10.1176/ajp.155.10.1325. [DOI] [PubMed] [Google Scholar]
- 29.Krause J., la Fougère C., Krause KH., Ackenheil M., Dresel SH. Influence of striatal dopamine transporter availability on the response to methylphenidate in adult patients with ADHD. Eur Arch Psychiatry Clin Neurosci. 2005;255:428–431. doi: 10.1007/s00406-005-0602-x. [DOI] [PubMed] [Google Scholar]
- 30.Volkow ND., Ding YS., Fowler JS., et al. Dopamine transporters decrease with age. J Nucl Med. 1996;37:554–559. [PubMed] [Google Scholar]
- 31.Krause KH., Dresel SH., Krause J., Kung HF., Tatsch K., Ackenheil M. Stimulant-like action of nicotine on striatal dopamine transporter in the brain of adults with attention deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2002;5:111–113. doi: 10.1017/S1461145702002821. [DOI] [PubMed] [Google Scholar]
- 32.Court JA., Lloyd S., Thomas N., et al. Dopamine and nicotinic receptor binding and the levels of dopamine and homovanillic acid in human brain related to tobacco use. Neuroscience. 1998;87:63–78. doi: 10.1016/s0306-4522(98)00088-8. [DOI] [PubMed] [Google Scholar]
- 33.Staley JK., Krishnan-Sarin S., Zoghbi S., et al. Sex differences in [123l]beta-CIT SPECT measures of dopamine and serotonin transporter availability in healthy smokers and nonsmokers. Synapse. 2001;41:275–284. doi: 10.1002/syn.1084. [DOI] [PubMed] [Google Scholar]
- 34.Faraone SV., Spencer T., Aleardi M., Pagano C., Biederman J. Meta-analysis of the efficacy of methylphenidate for treating adult attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 2004;24:24–29. doi: 10.1097/01.jcp.0000108984.11879.95. [DOI] [PubMed] [Google Scholar]
- 35.Ferber L v., Lehmkuhl G., Köster I., et al. Methylphenidatgebrauch in Deutschland: Versichertenbezogene epidemiologische Studie über die Entwicklung von 1998 bis 2000. Dtsch Arztebl. 2003;100:A41–46. [Google Scholar]
- 36.Michelson D., Adler L., Spencer T., et al. Atomoxetine in adults with ADHD: two randomized, placebo-controlled studies. Biol Psychiatry. 2003;53:112–120. doi: 10.1016/s0006-3223(02)01671-2. [DOI] [PubMed] [Google Scholar]
- 37.Stahl SM. Neurotransmission of cognition, part 1. Dopamine is a hitchhiker in frontal cortex: norepinephrine transporters regulate dopamine. J Clin Psychiatry. 2003;64:4–5. doi: 10.4088/jcp.v64n0101. [DOI] [PubMed] [Google Scholar]