Abstract
Since its “rebirth” in 1966, bipolar disorder (BPD) has rapidly come to occupy a central position in the research and treatment of mood disorders. Compared with major depressive disorder (MDD), BPD is a more serious condition, characterized by much more frequent recurrence, more complex comorbidity, and higher mortality. One major problem is the lack of valid definitions in adult and in child psychiatry; the current definitions are unsatisfactory, and heavily favor an overdiagnosis of MDD. Biological research is partially based on those definitions, which have a short half-life. An additional, dimensional, approach, quantifying hypomania, depression, and anxiety by self-assessment and symptom checklists is recommended, A further, related problem is the early recognition of the onset of BPD, especially in adolescence, and the identification of correlates in childhood. Early and timely diagnosis of BPD is necessary to enable prompt intervention and secondary prevention of the disorder. The paper describes the current status and future directions of developing clinical concepts of bipolarity
Keywords: bipolar spectrum, hypomania, diagnosis, comorbidity, dementia
Abstract
Desde que el trastorno bipolar (TB) fue rebautizado en 1966, éste ha llegado rápidamente a ocupar una posicíón central en la investigación y el tratamiento de los trastornos del ánimo. En comparación con el trastorno depresivo mayor (TDM) el TB es una condición más grave, caracterizada por recurrencias mucho más frecuentes, comorbilidad más compleja y mayor mortalidad. Un problema importante es la falta de definiciones validadas tanto en psiquiatría del adulto como de niños; las definiciones actuales son insatisfactorias y tienden fuertemente al sobre diagnóstico del TDM, La investigación biológica está basada parcialmente en estas definiciones, las cuales tienen una corta vida media. Se recomienda una aproximación dimensional adicional que cuantifique la hipomanía, la depresión y la ansiedad mediante autoevaluaciones y listas de chequeo de síntomas, Otro problema relacionado es el reconocimiento precoz de la aparición del TB, especialmente en el adolescente y la identificación de correlatos en la niñez. Se requiere de un diagnóstico precoz y oportuno del TB que permita una rápida intervención y una prevención secundaria del trastorno, El artículo describe el estado actual y las direcciones futuras sobre el desarrollo de conceptos clínicos de la bipolaridad.
Abstract
Depuis sa « renaissance » en 1966, la place du trouble bipolaire (TBP) est rapidement devenue centrale dans la recherche et le traitement des troubles de l'humeur. Le TBP est plus sévère que la dépression majeure (EDM), car caractérisé par de plus forts taux de récidive, une comorbidité plus complexe et des taux de mortalité plus élevés. L'absence de définition validée du trouble en psychiatrie de l'adulte et de l'enfant est un problème important ; les définitions actuelles ne sont pas satisfaisantes et orientent lourdement vers un excès de diagnostic d'EDM, La recherche biologique repose partiellement sur ces définitions dont la durée de vie est courte. Une autre approche, dimensionnelle, permettant de quantifier par I' auto-évaluation et la vérification des symptômes l'hypomanie, la dépression et l'anxiété est recommandée. Un autre problème est la reconnaissance précoce du début du TBP, surtout dans l'adolescence, et l'identification de ses corrélats dans l'enfance. Un diagnostic précoce et fait à temps est nécessaire pour permettre de traiter rapidement et de mettre en place la prévention secondaire du trouble. Cet article décrit l'état actuel et les orientations futures du développement des concepts cliniques de bipolarité.
Scale and source of the diagnostic problem
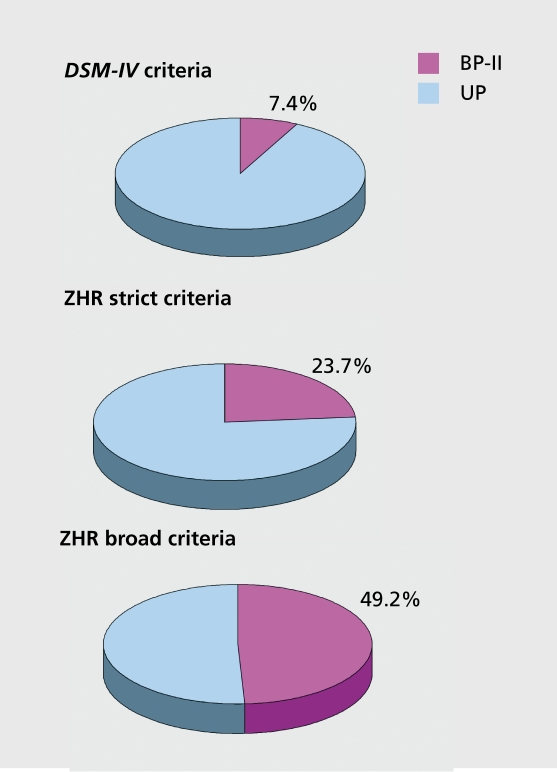
The basis for any discussion of bipolar disorder (BPD) is the diagnosis. The current definitions of bipolarity in DSM-IV1 and ICD-102 are valid, but. they are not. sensitive, with the result, that many cases are misdiagnosed as major depressive disorder (MDD). In the largest epidemiological studies, only about 10% to 20% of all subjects with major depressive episodes (MDE) were identified as having BPD using current, diagnostic criteria (Table I) 3-6 whereas the use of broader criteria has identified much higher proportions. Benazzi reports about 60% of treated ambulatory major dépressives as bipolar II (BP-II) patients,7 and in a nationwide French investigation in 994 GP patients with MDE and 772 psychiatric outpatients, 62% in each sample were identified by the Hypomania Checklist. 20 (HCL-20) as having BPII.8 In the Zurich Study of a. community cohort investigated prospectively from the ages of 20 to 40, that, proportion was about 50% (Figure 1).
Figure 1. Bipolar II disorder as a percentage of major depressive episodes. Age: 40/41 years; Zurich Cohort Study. BP-II, bipolar II; UP, unipolar .
Table I. Mood disorders: MDD and BPD lifetime prevalence. 3-6 MDD, manic-depressive disorder; BPD, bipolar disorder .
In community studies, the extent of the diagnostic problem is still underestimated, because there are no lifelong prospective studies on mood disorders. The most recent data from large epidemiological studies report, substantially higher prevalence rates for both major depressive and bipolar disorders compared with 10 to 15 years ago. One source of undcr-recognition in such studies is their cross-sectional design, which relies on subjects' lifetime memory of hypomania/mania. Epidemiological studies comprising more than one wave report, higher proportions of BPD compared with MDD. We have, then, to assume that, the latest figures still underestimate the problem due to nonreporting.
By the age of 20, subjects' recall of their previous history is already poor: about, 25% of a random sample of 1.05 normal subjects could no longer remember documented consultations with MDs, psychiatrists, and psychologists during their school years; there was no difference between externalizing and internalizing problems.9,10 It can be assumed that cross-sectional community studies underestimate lifetime prevalence rates by 25% to 50%; the dating of the age of onset, must, be equally problematic. However, the main impediment, to accurate measurement of the rates of bipolarity probably remains the overstrict concept, which fails to pick up BP-II and minor bipolar disorders in adults, adolescents, and children.
Current diagnostic criteria for bipolarity
DSM-IV-TR11 gives diagnostic criteria for manic, mixed, and hypomanic episodes, and for Bipolar I Disorder (B.PI), Bipolar II Disorder (BP-II), Cyclothymic Disorder, and Bipolar Disorder Not Otherwise Specified (BPNOS). In addition, there are important specifiers for the course, rapid cycling, seasonal patterns, and type of intcrcpisode recovery.
Bipolar I and IT disorders are defined by the presence of depressive disorders associated with manic or hypomanic episodes respectively, which makes the definition of a hypomanic episode crucial.
DSM-IV hypomanic episodes
The definition of a hypomanic episode in DSM-IV comprises: (i) experience of a distinct period of expansive, elevated or irritable mood; (ii) a minimum episode duration of 4 days; (iii) the presence of three or more (in the case of irritable mood four or more) of 7 criterial symptoms of mania; (iv) the episode has to be associated with a change in functioning, which is observable by others; and (v) should not. be severe enough to cause marked impairment, hospitalization, or psychotic symptoms. All three criteria (i) to (iii) are to my mind problematic and in need of revision; criterion (iv) may also to be overrestrictive, but, this question needs further investigation. In the prospective Zurich Study we found a. cumulative incidence of 3% of DSM-IV hypomanic episodes from age 26/27 to 40/41. DSM-IV hypomania was rarely an independent disorder: only 2 of 19 subjects were pure cases; all others suffered also from major (12) or minor depressive disorders (7). Their family history showed an elevated rate of depression and anxiety among firstdegree relatives; in addition there were temperamental features of both depression and bipolarity (ups and downs of mood and energy, depression, hypomania and bipolarity in the General Behavior Inventory).12
The bind of structured interviews
All the most, frequently-used structured interviews: the Structured Clinical Interview for DSM-IV: Axis I, Disorders-Clinician Version, (SC.I.D-CV),13 Composite International Diagnostic Interview (CIDI),14 and Munich-Composite International Diagnostic Interview (M-CIDI),15 are based on the DSM-IV stem question for mania/hypomania (occurrence of “periods of expansive, elevated or irritable mood”) and restrict, further assessment, of the diagnostic symptoms to subjects who answer “yes” to it. A “no” answer eliminates the subject as bipolar.
From a clinical point of view, there is considerable skepticism about the sensitivity of this stem question, because it. presumes - wrongly - that the subject is always aware of a mood change; there is a serious problem of false negatives, which cannot, be solved easily.
Recent developments beyond the DSM-IV diagnosis of hypomanic episodes
To address these recognized difficulties, an international expert committee16 recommended adding the symptom “increased activity” to the stem question for hypomanic episodes. Moreover, two important psychiatric outpatient, studies assessed the criteria! symptoms for hypomania without the stem question, modifying the SCID-CV13 for this purpose.17,18 This resulted in the identification of 66% and 60% of major dépressives as having BP-II. These rates far exceed the ratio of unipolar to bipolar disorders reported by the best, epidemiological studies using DSMIV criteria for hypomanic episodes, which consistently found substantially fewer bipolar (10% to 20%) than unipolars (80% to 90%) among those with MDE. Where does the truth lie?
Departing from the usual procedure, since 1981 the Zurich Study has applied a more complex stem question, asking interviewees about, “periods of increased enterprise, increased activity, lower fatigability, less need for sleep than usual, talking more, traveling more and doing more other things.” Mood changes were only assessed as symptoms. The stem questions and a list, of 20 hypomanic symptoms, including an open question, were first published in 1991 .19 This procedure allows many more subjects to enter into the interview on hypomanic symptoms, and it. excludes the hierarchical precedence given to euphoria and irritability in the diagnostic manuals. It takes account, of the fact that, while subjects may very often not, register their hypomanic mood symptoms, they are aware of behavioral changes and their consequences. In addition, it, avoids the inclusion of irritability as a mandatory symptom. Irritability is diagnostically unspecific; it. occurs in 80% of cases of depression, in anxiety states, and in other syndromes.
In the same paper we demonstrated that the modal duration of hypomanic episodes was 1 to 3 days, clearly calling into question the DSM-IV 4-day temporal criterion. About. 40% of hypomanic episodes in adults last only 1 to 3 days.
The 4-day duration criterion for hypomania. is also often not met. by bipolar children. New definitions for B.P-NOS have therefore recently been developed. Leibenluft et al20 suggested a minimum duration of 1 to 3 days for hypomania in children. Another recent proposal went even further, with a minimum duration of 4 hours within 24 hours, present, during at least 4 cumulative lifetime days.21 These are certainly important, steps towards more specific and valid criteria for children, and in agreement with general observations in children and adolescents, who frequently manifest, manic symptoms persisting for only hours or days.22-24
Subdiagnostic hypomania as a relatively strict concept for bipolarity
For research purposes, the main question is whether bipolarity has to be defined by the presence of a clinically significant and relevant hypomanic episode. Collecting data on the continuum from mania to normal hypomanic symptoms, we identified many subjects with subdiagnostic hypomania, which can be distinguished from DSM-IV hypomanic episodes and from normal controls by a. number of validators.
Our strict. Zurich definition of subdiagnostic hypomania. requires a minimum duration of 1 or more days, the presence of 2 or more of 7 diagnostic symptoms, and the presence of a. change induced by the episode(s), which was reported by other persons or which created problems for the subject him- or herself. Our concept of subthreshold hypomania identifies about, one quarter of all dépressives as bipolar patients, with a prevalence rate around 5%.25 Eighty percent of subjects meeting the strict Zurich criteria for subthreshold hypomania had three or more manic symptoms; a. defining threshold of three instead of two symptoms as suggested by Benazzi,26 could therefore be considered. In sum, we found hypomanic periods to be present, cumulatively on about, 30 days per year. In the Zurich Study, 54of 74 subjects (73%) with subdiagnostic hypomania suffered from major or minor depressive disorders and therefore received diagnoses of BP-II or minor bipolar disorder (cumulative incidence rates of 11 .0% and 9.4% respectively). The remaining 23 subjects (27%) were considered to be pure hypomanics without depression (cumulative incidence of 3.3%). The DSM-IV hypomanics (N=3) were a minority, whereas subdiagnostic pure hypomania (N=20) predominated.27
Bipolar specifier for depression
In epidemiological studies, unlike patient studies, it. is not. usually possible to question family and friends about changes in the interviewee's mood/behavior - changes which will rarely be noticed by hypomanic subjects themselves, who tend only to complain about depressive symptoms; for this reason the impact, criterion for hypomania may be too restrictive. In the Zurich Study we tentatively introduced a yet broader definition of hypomania as a diagnostic specifier for bipolarity in subjects with a. diagnosis of depression, omitting the impact, criterion.27
We found that, this definition of hypomania. (brief spells, with a minimum of two symptoms), helped to identify a large group of hidden bipolar patients among dépressives (Figure 1); the validity of this concept was shown by Angst, ct al.28
The introduction of a broader specifier for bipolarity is compatible with child psychiatric data (reviewed by Evans24); it induces a. significant, diagnostic shift, from MDD to BP-II disorder, and from minor depressive disorders to minor bipolar disorders. This diagnostic specifier has been shown to classify about, half of all subjects' depressive disorders as BP-II.27-28 It does not, of course, change the prevalence rates of mood disorders, it, merely reclassifies many subjects as bipolar patients.
Minor bipolar disorders (MinBPD)
Our diagnostic specifier for bipolar depression reclassified about half of subjects with dysthymia and many with recurrent, brief depression (RBD) and minor depression (MinD) as having minor bipolar disorders, including cyclothymic disorders; the cumulative incidence rate was 9.4% . These minor bipolar subjects were found to be clinically more severely ill than their unipolar counterparts with dysthymia, RBD, or MinD in terms of treatment rates and comorbidity with alcohol use disorders.27
Pure subthreshold hypomania (ie, without depression)
Pure subdiagnostic hypomanic subjects should not be considered as patients, but, rather as characterized by a mix of hypomania's favorable and unfavorable consequences, as shown recently by Gamma et al (unpublished data). In the Zurich Study we found that such subjects rarely sought treatment. Compared with controls, they were successful in terms of higher incomes and higher marriage rates, and they were more interested in sex. The reverse side of the coin, however, was that they had more substance -use disorders (SUDs) and were more often in trouble with the law (fines, custodial and noncustodial sentences). They were also more affected by sleep problems, substance abuse, and binge eating than controls.
Unlike subjects with DSM-IV hypomania, pure subthreshold hypomanics did not report, a positive family history for depression among first-degree relatives, nor did they manifest traits of depression/dysthymia on the subscalcs of the General Behavior Inventory (GBI).
Normal subjects with hypomanic symptoms
Hypomanic symptoms arc elements of normal mood swings. We could not. find any relevant, differences between subjects experiencing some hypomanic symptoms and those with no symptoms at all. We all manifest depressive symptoms after experiencing disappointment, or loss (for example, bereavement) and likewise hypomanic symptoms when feeling euphoric. A striking example is falling in love: in a. study of young adults who had recently fallen in love, subjects scored as high as BP-II subjects on a hypomania self- assessment scale.28
Normal subjects with an anxious, hypomanic/hyperthymic, or cyclothymic temperament
Temperament is by definition a. persistent behavioral trait of normal persons, for instance behavioral inhibition (describing anxious temperament).30,31 In Three Seductive Ideas32 Kagan states that the modern assumption that anxiety is abnormal and maladaptive (p 19) is wrongheaded, arguing that ”The belief that humans can and should be free of anxiety is one of the distinguishing illusions in Western thought in this century“ (p 18). Of course, exactly the same may be said about, depressive and hypomanic phenomena. The author also stresses that psychological traits are not stable structures hidden deep in the person's core; they can change. This, too, is true for affective temperaments.
From a historical perspective, Kraepelin's basic states (Grundzustânde) correspond to temperamental and personality traits.33 Falrct34 and Kretschmer35 (on the basis of family studies) created a continuum from cyclothymic temperament via. cycloid personality to manic-depressive disorder. Kretschmer maintained that all transitions and variations could be observed in families and in an individual's development over lifetime. Kretschmer's cycloid personalities are very close to, and indeed overlap with, the cyclothymic disorder of DSM-IV. Akiskal's well-known concepts of temperament and of a bipolar spectrum develop Kretschmer's work; an interesting history of the notions of temperament is provided in Akiskal et al.36
The modern development, of quantitative temperamental measures is very promising for clinical and epidemiological research into the continuum from normal to pathological mood changes. The GBI37,38 and the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire (TEMPS- A) of Akiskal et al39 are instruments for self-assessment, and the GBI can be used for the diagnosis of normal temperament and of hypomanic or bipolar conditions.
In Brazil, the TEMPS-A was shown to differentiate remitted bipolar patients from the healthy relatives of bipolar patients and normal controls from the community.”40 The bipolar group scored highest on the depressive, cyclothymic, irritable, and anxious temperament scales, whereas the healthy relatives took an intermediate position between the bipolar patients and the controls. The hyperthymic scale did not clearly differentiate between the groups. The factor structure seems to be transculturally stable.41 TEMPS-A cyclothymia and dysthymia were also found to correlate positively with creativity as assessed by the Baron-Welsh Art Scale.42,43
Temperament characterizes a normal state, and cannot, serve as a diagnostic criterion for a pathological state. It would, for instance, be misleading and conceptually mistaken to diagnose a depressive patient with a cyclothymic temperament as being bipolar, although such a patient, may be at greater risk than others of developing bipolar disorder over lifetime. A diagnostic application could be found in validated cutoffs on temperamental scales.
Future research will need to use continuous measures for assessing temperament in population samples of different, ages. Mood lability is normal in children, but. can be pathological in adolescents. Expressions of temperament certainly change markedly over the lifespan. Age- and sex-specific norms are required.
Stigma
Stigmatization focuses on defined minorities; the best. weapon against it. is the demonstration that we are “all in the same boat.” Research with quantitative measures on the continuum from normal mood variations and temperament to minor and major bipolar disorders can provide that demonstration.44 We all score on instruments measuring anxiety, depression, and hypomania. The distribution is not. bimodal but. log-normal, with no clear cutoff between normal and pathological mood variations. Stigmatizing attitudes are fuelled by ignorance regarding what it. is to be a human being.
Further research in this context should not only focus on psych opathology, but, should also look at. the distinct. advantages of being hypomanic or cyclothymic, about, which there is very little representative data, although the association of creativity with hypomania and bipolarity is well-established on biographical grounds.45 Whybrow46 and Gartner47 have also described how American society has always been marked by the insatiable demands, high energy, and drive associated with hypomania.
The onset of bipolar disorder
We know regrettably little about the onset of bipolar disorder, which in one third of adult cases is retrospectively dated before the age 20. In childhood, bipolar disorder is veiy difficult to diagnose because the full hypomanic syndrome is usually lacking. It. is certainly not possible to apply DSM-IV hypomania criteria for the early recognition of BPD. As Duffy states, most, bipolar disorders begin as depression, activated episodes are rare before 12 years of age, and the validity of the diagnosis of BPD in impulsive, irritable, labile, or behaviorally dysregulated children remains to be proven.48
According to a meta-analysis of the literature, the offspring of bipolar parents have a fourfold risk of developing affective disorders.49 Prospective studies of high-risk children and adolescents are therefore methodologically a. very promising approach. However, the reported early symptoms of BPD vary widely, and are subject, to very diverse interpretation.
The 10-year prospective Amish study, for example, reports that compared with controls (the offspring of well parents), the children of BPD parents episodically manifested potentially prodromal signs and symptoms, namely: anxious/worried, attention poor/distractible in school, easily excited, hyperalert, mood changes/labile, role impairment, in school, somatic complaints, and stubborn-determined.50 Similarly Radke-Yarrow51 found the children of bipolar parents to be more often depressed and disruptive, and to have many behavioral problems compared with controls. In early adolescence there was lack of impulse control (71%), pressured speech (86%), and racing thoughts (43 %).52 Another high-risk study identified vegetative lability/somatization (which are also components of ncuroticism) and perception of stress as vuln erability factors.53,54
A prospective Dutch study in bipolar offspring found that later-onset bipolar subjects performed well socially until the disorder manifested clearly.55 In a 5-ycar prospective study, Duffy et al56 found more anxiety and sleep disorders as well as bipolar and depressive disorders among the offspring of bipolar parents than among control offspring. SUDs were found to be secondary to mood disorders. Attention deficit-hyperactivity disorder (ADHD) was in some cases an antecedent of mood disorders. A potentially bipolar prodromal syndrome of BPD was described by Corrcll et al,57 consisting of decreased school work or functioning, mood lability, outbursts of anger, social isolation and anxiety, specific depressive symptoms (depressed mood, anhedonia, insomnia, feeling worthless) or hypomanic symptoms (irritability, increased energy/activity, psychomotor agitation). The role of premorbid cognitive problems is also currently a subject, of investigation.58-60
There is agreement that the phenomenology of BPD differs between children and adolescents.61 In early-onset-cases there appears to be a. global delay or arrest, in the development, of appropriate affect, regulation (as a developmental disorder), whereas in adolescent-onset BPD the emotional dysregulation presents as an intermittent, phenomenon. In addition, in terms of comorbidity and course, early-onset cases are often highly comorbid with internalizing and externalizing symptomatology (anxiety, disruptive behavior, neuropsychiatrie, cognitive, and developmental symptoms).62,63
The main conclusion regarding the onset, of BPD is that the disorder seems most typically to start, between 11/12 and 20 years of age as depression or, in some cases, as behavioral problems or SUDs.64 In a. study of psychotic manic patients, 60.9% of those under 21 years of age had a pre-existing externalizing disorder and 26.1% a preexisting adjustment or anxiety disorder.65
BPD and externalizing problems
There is a confusingly high overlap between ADHD and
BPD, with estimates of between 59% and 90% ,66-68 which can only be clarified by conducting more large prospective studies following the high-risk children of bipolar parents and children with ADHD from childhood through to adulthood.
No data have yet identified ADHD as a significant antecedent of bipolar disorder in high-risk children: two follow-up studies of ADHD in children found no BPD in adulthood,69,70 and a more recent, and relatively small follow-up study conducted over 6 years failed to establish a close relationship between ADHD and BPD.71,72 Some authors have suggested that there is an especially severe subgroup of BPD characterized by comorbidity with ADHD.73,74 At the same time, an Australian followup study75 raises doubts as to whether any link whatsoever exists between the manic symptoms associated with ADHD in childhood and BPD in late adolescence/early adulthood. The results are contradictory: a European group found that, the children of bipolar parents had no elevated risk for ADHD or conduct disorder; in almost, all cases BPD started as a. major or minor form of depression76; whereas Chang et al77 found high rates of ADHD among the offspring of bipolar parents.
Another area of ongoing debate is whether a specific subtype of conduct, disorder can be linked with BPD, as suggested by several studies.67,78-83 Juvenile antisocial behavior was present in 55% of 80 adolescents newly diagnosed and hospitalized for BPD.84 On the basis of retrospective data, in the Zurich Study of young adults we found a. significant association of BPD with certain conduct problems.85
BPD and DUDs
An important field of investigation is the early manifestation of SUDs in subjects who simultaneously or subsequently develop bipolar disorders.64,65,86 A birth cohort, study conducted in New Zealand, which demonstrated the existence of a common vulnerability factor for tobacco, cannabis, and alcohol abuse in adolescents,87 unfortunately did not assess bipolarity.
There is ample research on the association of BP-I with SUDs,88 especially in women, as summarized recently by Lavander et al,89 but little investigation of its association with the bipolar spectrum. There is evidence from the Zurich Study that, the traditional association between major depression and SLID may be misleading and based on an underdiagnosis of bipolarity, because a widening of the definition shifted the comorbidity to BP-II, and the association with MDD dwindled to insignificance. This finding is in sharp contrast, with the extensive literature reporting the association of MDD with alcohol use disorder (AUD) on the basis of conventional DSM diagnoses.90 SUD is correlated with violent behavior87; BPD subjects may therefore be more prone to offending; this has been shown for bipolar women.91
BPD and anxiety disorders
Symptoms of anxiety are elements of the depressive syndrome and integrated into depression rating scales. Intuitively, one would therefore expect, generalized anxiety disorders (GAD) and repeated panic attacks to be more strongly associated with major depression than with BPD. However, the opposite would appear to be true. In the Zurich Study community sample, applying broad criteria for bipolarity, we found significant, associations between BP-II and GAD (OR=5.6), panic attacks (OR=4.0) and obsessive-compulsive syndromes (OR=3.9), whereas no such significant association was found with MDD. This new, unpublished finding is a consequence of the broadened definition of bipolarity; as in the case of comorbidity with alcohol use disorders mentioned above, a. major part of comorbidity is shifted from MDD to BP-II.
Studies of comorbidity can be a fruitful method of checking the consequences of changing diagnostic criteria.
Suicidal thoughts, suicide attempts, and completed suicides
The relationship between suicidal ideation, suicide attempts, and suicides is not. simple. Suicide attempts occur most, frequently among adolescents and young adults, whereas suicide rates rise sharply with age. In addition, in most cultures women make more suicide attempts than men, but. more men than women commit, suicide. Suicide attempts appear to be weak predictors of suicide. In our lifelong prospective study in 220 hospitalized bipolar patients92 only 3 of the 57 patients who had attempted suicide committed suicide later; overall, only 3 of 17 patients who committed suicide had previously made a suicide attempt.
Suicide is not, just a result, of depression (although 80% to 90% of suicides are associated with major or minor depressive disorders) but. is also closely associated with aggression/impulsivity.
Prospective treatment research in this field is sparse, although suicide prevention by long-term medication is effective. As demonstrated by a lifelong follow-up study of 406 patients with major mood disorders,92 it, would appear that drugs which have antiaggressive effects, such as lithium and clozapine, could be especially promising for suicide prevention in bipolar subjects. The hypothesis of a long-term antisuicidal effect, of modern atypical neuroleptics - about which there is so far no data - should therefore be carefully studied.
BPD and dementia
The association of BPD with dementia has been little investigated. A large Danish study found a correlation between dementia and the number of hospitalizations in bipolar patients,93 whereas we found no comparable relationship in a. long-term follow-up of hospitalized patients.94 Recently we published preliminary evidence that longterm medication with lithium or with clozapine may attenuate the severity of dementia.95 In addition, Nunes et al96 found evidence that, compared with a sample treated with other mood stabilizers, Alzheimer's disease is reduced in elderly bipolar patients treated with lithium. These findings are compatible with research on the neurotrophic and neuroprotective properties of some drugs, and will hopefully stimulate research into the long-term effects of atypical neuroleptics prescribed in large amounts today. The negative findings of the general practice study by Dunn et al,97 who even found a correlation between numbers of prescriptions of lithium and dementia, may be explained by the severity of the disorders and a lack of an adequate untreated group of bipolar patients; comparisons using the general population as controls are not. conclusive, because BPD per se is correlated with all kinds of somatic disorders, including dementia, cerebrovascular disorders, diabetes, hypertension, etc.98
Early recognition of bipolarity
The early recognition and treatment of bipolarity is
essential for preventing the serious social consequences, rapid cycling, chronicity, and suicidally associated with it, as well as for reducing the economic costs, as shown by McCombs et al.99 It has already been stressed that there is a. serious gap in our knowledge about, the onset, of BPD in child psychiatry; the timely diagnosis of BPD raises unsolved problems in adult psychiatry, as well.
Hauser et al100 recently summarized the present, difficulties in recognizing bipolarity. The authors concluded that we need validated thresholds for true caseness on temperamental measures such as the TEMPS-A scale, we require more data on frequent “ups and downs” as a strong correlate of bipolar disorder, and we need intensive research on hypomanic symptoms without restrictions as to the minimal duration or the consequences of the symptoms. We should not, however, mix trait measures (TEMPS-A) with state measures.
Screening tools for hypomania
The well-recognized difficulties of identifying bipolarity have led to the development, of modern screening tools for the self-assessment of hypomanic/manic symptoms, a development, which is still in its early stages. The bestknown instrument, is the mood disorder questionnaire (MDQ) of Hirschfeld et al,101 fitting DSM-IV criteria for mania and hypomania.
Another was derived from a symptom checklist, of 20 hypomanic symptoms, used since 1986 in the interviews of the Zurich Study, and applied successfully by Hantouche as the self-assessment hypomania checklist HCL-20 in several large French studies.8,102,103 In the EPIDEP study,98 the rate of BP-II among patients originally diagnosed with MDE almost doubled when they were screened with the H.CL-201 month later. The Hypomania Checklist-32104 is
an extended version of the instrument; it. has been translated into more than 20 languages (available on request) and underwent recently a first, revision (HCL-32 R-1). It is currently being validated in different, cultures, in order to ascertain whether there are universal core symptoms. A recent Taiwanese study105 identified the same two-factor structure of hypomania as found in earlier studies carried out, in Italy and Sweden104 and Spain.106 A future task will be to identify a. factor solution which is cross-culturally stable. A cutoff of 10 on the H.CL-20 and of 14 on the HCL-32 seems to identify a. large proportion of MDE, cases as bipolar patients.
Conclusions
This article illustrates that conclusive clinical research into bipolar disorder still has a. long way to go. We need more and longer representative prospective studies in children, adolescents, and adults. Major depressive disorder is still heavily overdiagnosed; it. is usually the initial diagnosis, at the expense of bipolar disorder. We will have to revise and broaden the definition of bipolar disorder; this will have a great impact on rates of prevalence and comorbidity and on treatment. Estimates of the burden and costs of the disorder will have to be corrected upwards. This process could take at least, another 10 years. The forthcoming DSM-V and ICD-11 may not, yet, be in a position to solve the serious diagnostic problem, because the data for the necessary revision are sparse. The second, eternal, problem remains, “what is a case?”107-109 on the continuum on hypomania scales/checklists from healthy to ill. No definitive answer to this question has yet. been found. However, this is nothing to be ashamed of: in medicine the norms for pathological blood pressure have changed repeatedly. A clear cutoff is probably always to a certain extent, questionable, neglecting the normal interindividual variation of the population.
It is conceptually important, to add dimensional measures for depression, hypomania, and anxiety to the categorical approach in classifying mood disorders110 and not, base expensive biological and clinical research exclusively on diagnostic categories whose definitions have a short, halflife.
Finally, we need long-term treatment studies focusing on the potential effects of mood stabilizers and atypical neuroleptics against dementia, suicide, and vascular mortality.
Selected abbreviations and acronyms
- ADHD
attention deficit-hyperactivity disorder
- BPD
bipolar disorder
- MDD
major depressive disorder
- MDE
major depressive episode
- SUD
substance-use disorder
REFERENCES
- 1.American Psychiatrie Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- 2.World Health Organization. The ICD-W Classification of Mental and Behavioral Disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: World Health Organization; 1992 [Google Scholar]
- 3.Weissman MM., Bruce LM., Leaf PJ., Florio L., Holzer C. Affective disorders. In: Robins LN, Regier DA, eds. Psychiatric disorders in America. The Epidemiologic Catchment Area Study. New York, NY: The Free Press; 1991:53–80. [Google Scholar]
- 4.Kessler RC. The National Comorbidity Survey of the United States. Int Rev Psychiatry. 1994;6:365–376. [Google Scholar]
- 5.Kessler RC., Berglund P., Dernier O., et al. The epidemiology of major depressive disorder. Results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 6.Bijl RV., Ravelli A., van Zerssen G. Prevalence of psychiatric disorder in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 7.Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in private practice. J Affect Disord. 1997;43:163–166. doi: 10.1016/s0165-0327(96)01421-8. [DOI] [PubMed] [Google Scholar]
- 8.Hantouche EG., Angst J. Enquête nationales bipolact. À la recherche de l'hypomanie dans les dépressions difficiles. Bipolact. 2007;1:4–12. [Google Scholar]
- 9.Kaeser D. Psychiatrische Katamnese von ehemaligen schulpsychiatrischen Fallen [Medical Thesis] Zurich: University of Zurich; 1979 [Google Scholar]
- 10.Weber M. Zuverlâssigkeit der Beantwortung eines anamnetischen Fragebogens bei zwanzigjàhrigen Zùrchern. [Medical Thesis]. Zurich: University of Zurich; 1979 [Google Scholar]
- 11.American Psychiatrie Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Revision. Washington, DC: American Psychiatric Association. 2000 [Google Scholar]
- 12.Gamma A., Angst J., Ajdacic-Gross V., Rôssler W. Are hypomanics the happier normals? J Affect Disord. 2008. In press doi: 10.1016/j.jad.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 13.First MB., Spitzer RL., Gibbon M., Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - clinician version (SCID-CV). Washington DC American Psychiatric Press; 1997 [Google Scholar]
- 14.Kessler RC., Ustiin TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lachner G., Wittchen H-U., Perkonigg A., et al. Structure, content and reliability of the Munich-Composite International Diagnostic Interview (MCIDI) substance use sections. Eur Addict Res. 1998;4:28–41. doi: 10.1159/000018922. [DOI] [PubMed] [Google Scholar]
- 16.Akiskal HS., Hantouche EG., Bourgeois ML., et al. Toward a refined phenomenology of mania: combining clinican-assessment and self-report in the French EPIMAN study. J Affect Disord. 2001;67:89–96. doi: 10.1016/s0165-0327(01)00441-4. [DOI] [PubMed] [Google Scholar]
- 17.Benazzi F., Âkiskal H. Refining the evaluation of bipolar II: beyond the strict SCID-CV guidelines for hypomania. J Affect Disord. 2003;73:33–38. doi: 10.1016/s0165-0327(02)00327-0. [DOI] [PubMed] [Google Scholar]
- 18.Akiskal HS., Benazzi F. Optimizing the detection of bipolar II disorder in outpatient private practice: toward a systematization of clinical diagnostic wisdom. J Clin Psychiatry. 2005;66:914–921 . doi: 10.4088/jcp.v66n0715. [DOI] [PubMed] [Google Scholar]
- 19.Wicki W., Angst J. The Zurich Study. X. Hypomania in a 28- to 30-year-old cohort. Eur Arch Psychiatry Clin Neurosci. 1991;240:339–348. doi: 10.1007/BF02279764. [DOI] [PubMed] [Google Scholar]
- 20.Leibenluft E., Charney DS., Towbin KE., Bhangoo RK., Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160:430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 21.Birmaher B., Axelson D. Course and outcome of bipolar spectrum disorder in children and adolescents: a review of the existing literature. Dev Psychopathol. 2006;18:1023–1035. doi: 10.1017/S0954579406060500. [DOI] [PubMed] [Google Scholar]
- 22.Carlson GA., Kelly KL. Manic symptoms in psychiatrically hospitalized children -what do they mean? J Affect Disord. 1998;51:123–125. doi: 10.1016/s0165-0327(98)00211-0. [DOI] [PubMed] [Google Scholar]
- 23.Geller B., Sun K., Zimerman B., Luby J., Frazier J., Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995;34:259–268. doi: 10.1016/0165-0327(95)00023-g. [DOI] [PubMed] [Google Scholar]
- 24.Evans DL., Foa EB., Gur RE., et al. eds Treating and Preventing Adolescent Mental Health Disorders. What We Know and What We Don 't Know a Research Agenda for improving the Mental Health of Our Youth. Oxford, UK: Oxford University Press; 2005 [Google Scholar]
- 25.Angst J., Gamma A., Benazzi F., Ajdacic V., Eich D., Rôssler W. Toward a redefinition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-ll, minor bipolar disorders and hypomania. J Affect Disord. 2003;73:133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 26.Benazzi F. Testing new diagnostic criteria for hypomania. Ann Clin Psychiatry. 2007;19:1–6. doi: 10.1080/10401230701338219. [DOI] [PubMed] [Google Scholar]
- 27.Angst J., Marneras A., Gamma A., Ajdacic-Gross V., Rôssler W. The affective spectrum and its neglected sub-diagnostic groups. In: Marneros A, Rôttig D, eds. Biogenese und Psychogenese. Regensburg, Germany: S. Roderer Verlag. In press [Google Scholar]
- 28.Angst J., Gamma A., Benazzi F., Ajdacic V., Eich D., Rôssler HW. Diagnostic issues in bipolar disorder. Eur Neuropsychopharmacol. 2003;13:S43–S50. doi: 10.1016/s0924-977x(03)00077-4. [DOI] [PubMed] [Google Scholar]
- 29.Brand S., Luethi M., von Planta A., Hatzinger M., Holsboer-Trachsler E. Romantic love, hypomania, and sleep pattern in adolescents. JAdolesc Health. In press. doi: 10.1016/j.jadohealth.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 30.Kagan J., Reznik JS., Clarke C., Snidman N. Behavioral inhibition to the unfamiliar. Child Dev. 1984;55:2212–2225. [Google Scholar]
- 31.Kagan J., Snidman N., Arcus D., Reznick JS. Galen's prophecy. In: Galen's Prophecy Temperament in Human Nature. New York, NY: Basic Books; 1994;55:232–236. [Google Scholar]
- 32.Kagan J. Three Seductive Ideas. Cambridge London: Harvard University Press. 1998 [Google Scholar]
- 33.Kraepelin E. Psychiatrie. Ein Lehrbuch fur Studierende und Aerzte. 6. voilständig umgearbeitete Ausgabe ed. Leipzig, Germany: Verlag Johann Ambrosius Barth. 1899 [Google Scholar]
- 34.Falret JP. Leçons à l'Hospice de la Sâlpetrière. Gazette Hôpitaux. 1851;258:23–24. [Google Scholar]
- 35.Kretschmer E. Kôrperbau und Charakter. Untersuchungen zum Konstitutionsproblem und zur Lehre von den Temperamenten. Berlin, Germany: Springer; 1921 [Google Scholar]
- 36.Akiskal HS., Brieger P., Mundt C., Angst J., Marneros A. Temperament und affektive Stôrungen. Die TEMPS-A-Skala als Konvergenz europàischer und US-amerikanischer Konzepte. Nervenarzt. 2002;73:262–271. doi: 10.1007/s00115-001-1230-y. [DOI] [PubMed] [Google Scholar]
- 37.Depue RA., Monroe SM. Learned helpnessness in the perspective of the depressive disorders: conceptual and definitional issues. J Abnorm Psychol. 1978;87:3–20. doi: 10.1037//0021-843x.87.1.3. [DOI] [PubMed] [Google Scholar]
- 38.Depue RA., Monroe SM. The unipolar-bipolar distinction in the depressive disorders. Psychol Bull. 1978;85:1001–1029. [PubMed] [Google Scholar]
- 39.Akiskal HS., Akiskal KK., Haykal RF., Manning JS., Connor PD. TEMPS-A: progress towards validation of a self-rated clinical version ot the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord. 2005;85:3–16. doi: 10.1016/j.jad.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 40.Mendlowicz MV., Girardin J-L., Kelsoe JR., Akiskal HS. A comparison of recovered bipolar patients, healthy relatives of bipolar probands, and normal controls using the short TEMPS-A. J Affect Disord. 2005;85:147–151. doi: 10.1016/j.jad.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 41.Karam EG., Mneimneh ZN., Salamoun MM., Akiskal HS., Akiskal KK. Suitability of the TEMPS-A for population-based studies: ease of administration and stability of affective temperaments in its Lebanese version. J Affect Disord. 2007;98:45–53. doi: 10.1016/j.jad.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 42.Strong CM., Nowakowska C., Santosa CM., Wang JL., Kraemer HC., Ketter TA. Temperament-creativity relationships in mood disorder patients, healthy contraband highly creative individuals. J Affect Disord. 2007;100:41–48. doi: 10.1016/j.jad.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 43.Santosa CM., Strong CM., Nowakowska C., Wang PW., Rennicke CM., Ketter TA. Enhanced creativity in bipolar disorder patients: a controlled study. J Affect Disord. 2007;100:31–39. doi: 10.1016/j.jad.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 44.Cassano GB., Rucci P., Frank E., Fagiolini A., Dell'Osso L., Shear MK., et al. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 2004;161:1264–1269. doi: 10.1176/appi.ajp.161.7.1264. [DOI] [PubMed] [Google Scholar]
- 45.Jamison KK. Touched With Fire. New York, NY: Free Press; 1993 [Google Scholar]
- 46.Whybrow PC. Wenn MEHR nicht genug ist Analyse einer gierigen Gesellschaft. Munich, Germany: Vedra Verlag; 2007 [Google Scholar]
- 47.Gartner JD. The Hypomanic Edge: the Link Between (a Little) Craziness and (a Lot Ofj Success in America. New York, NY: Simon & Schuster; 2005 [Google Scholar]
- 48.Duffy A. Does bipolar disorder exist in children? A selected review. Can J Psychiatry. 2007;52:409–417. doi: 10.1177/070674370705200702. [DOI] [PubMed] [Google Scholar]
- 49.Lapalme M., Hodgins S., LaRoche C. Children of parents with bipolar disorders: a metaanalysis of risk for mental disorders. Can J Psychiatry. 1997;42:623–631 . doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- 50.Shaw JA., Egeland JA., Endicott J., Allen CR., Hostetter AM. A 10-year prospective study of prodromal patterns for bipolar disorder among Amish youth. J Am Acad Child Adolesc Psychiatry. 2005;44:1104–1117. doi: 10.1097/01.chi.0000177052.26476.e5. [DOI] [PubMed] [Google Scholar]
- 51.Radke-Yarrow M., Nottelmann ED., Martinez P., Fox MB., Belmont B. Young children of affectively ill parents: a longitudinal study of psychosocial development. J Am. Acad Child Adolesc Psychiatry. 1992;31:68–77. doi: 10.1097/00004583-199201000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Radke-Yarrow M. Common and diverse pathways, mechanisms, and outcomes. In: Children of Depressed Mothers. Cambridge, UK; New York, NY: Melbourne, Australia: Cambridge University Press; 1998:166–184. [Google Scholar]
- 53.Modell S., Huber J., Holsboer F., Lauer CJ. The Munich vulnerability study on affective disorders: risk factors for unipolarity versus bipolarity. J Affect Disord. 2003;74:173–184. doi: 10.1016/s0165-0327(02)00010-1. [DOI] [PubMed] [Google Scholar]
- 54.Ising M., Lauer CJ., Holsboer F., Modell S. The Munich vulnerability study on affective disorders: premorbid psychometric profile of affected individuals. Acta Psychiatr Scand. 2004;109:332–338. doi: 10.1111/j.1600-0447.2004.00309.x. [DOI] [PubMed] [Google Scholar]
- 55.Reichart CG., van der Ende J., Wals M., Hillegers MHJ., Nolen WA., Ormel J., et al. Social functioning of bipolar offspring. J Affect Disord. 2007;98:207–213. doi: 10.1016/j.jad.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 56.Duffy A., Aida M., Crawford L., Milin R., Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disord. 2007;9:1–11. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 57.Correll CU., Penzner JB., Lencz T., Auther A., Smith CW., Malhotra AK., et al. Early identification and high-risk strategies for bipolar disorder. Bipolar Disord. 2007;9:324–338. doi: 10.1111/j.1399-5618.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 58.Meyer SE., Carlson GA., Wiggs EA., Martinez PE., Ronsaville DS., KlimesDougan B., et al. A prospective study of the association among impaired executive functioning, childhood attentional problems, and the development of bipolar disorder. Dev Psychopathol. 2004;16:461–467. doi: 10.1017/s095457940404461x. [DOI] [PubMed] [Google Scholar]
- 59.Meyer SE., Carlson GA., Wiggs EA., et al. A prospective high-risk study of the association among maternal negativity, apparent frontal lobe dysfunction, and the development of bipolar disorder. Dev Psychopathol. 2006;18:573–589. doi: 10.1017/S0954579406060299. [DOI] [PubMed] [Google Scholar]
- 60.Vinberg Christensen M. Family history of affective disorder, a cross-sectional high-risk study (abstract). In: The International Society for Affective Disorders (BAD). 3rd Biennial Conference, Lisbon, Portugal 3rd-6th March 2006. J Affect Disord. 2006 [PubMed] [Google Scholar]
- 61.Carlson GA., Meyer SE. Phenomenology and diagnosis of bipolar disorder in children, adolescents, and adults: complexities and developmental issues. Dev Psychopathol. 2006;18:939–969. doi: 10.1017/S0954579406060470. [DOI] [PubMed] [Google Scholar]
- 62.Carlson GA. Bipolar disorder in children and adolescents. A critical review. In: Shaffer D, Waslick BD, eds. The Many Faces of Depression in Children and Adolescents. Washington DC, London, UK: American Psychiatric Publishing Inc.; 2002:105–128. [Google Scholar]
- 63.Singh MK., DelBello MP., Stanford KE., Soutullo C., McDonough-Ryan P., McElroy SL., et al. Psychopathology in children of bipolar parents. J Affect Disord. 2007;102:131–136. doi: 10.1016/j.jad.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 64.Aichhorn W., Stuppâck C., Kralovec K., Yazdi K., Aichhorn M., Hausmann A. Bipolare Affektive Stôrungen im Kindes- und Jugendalter. Neuropsychiatrie. 2007;21:84–92. [PubMed] [Google Scholar]
- 65.Râsànen P., Tiihonen J., Hakko H. The incidence and onset-age of hospitalized bipolar affective disorder in Finland. J Affective Disord. 1998;48:63–68. doi: 10.1016/s0165-0327(97)00141-9. [DOI] [PubMed] [Google Scholar]
- 66.Yazgan MY., Fis NP., Scahill LL. Pediatric bipolar disorder: from the perspective of North America. In: Diler RS, ed. Pediatric Bipolar Disorder: a Global Perspective. New York, NY: Nova Biomedical Books; 2007:1–31. [Google Scholar]
- 67.Biederman J., Faraone SV., Wozniak J., Mick E., Kwon A., Aleardi M. Further evidence of unique developmental phenotypic correlates of pediatric bipolar disorder: findings from a large sample of clinically referred préadolescent children assessed over the last 7 years. J Affect Disord. 2004;82S:S45–S58. doi: 10.1016/j.jad.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 68.Kent L., Craddock N. Is there a relationship between attention deficit hyperactivity disorder and bipolar disorder? J Affect Disord. 2003;73:211–221. doi: 10.1016/s0165-0327(02)00092-7. [DOI] [PubMed] [Google Scholar]
- 69.Gittelman R., Mannuzza S., Shenker R., Bonagura N. Hyperactive boys almost grown up. I. Psychiatric status. Arch Gen Psychiatry. 1985;42:937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- 70.Weiss G., Hechtman L., Milroy T., Perlman T. Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Adolesc Psychiatry. 1985;24:211–220. doi: 10.1016/s0002-7138(09)60450-7. [DOI] [PubMed] [Google Scholar]
- 71.Hazell PL., Carr V., Lewin TJ., Sly K. Manic symptoms in young males with ADHD predict functioning but not diagnosis after 6 years. J Am Acad Child Adolesc Psychiatry. 2003;42:552–560. doi: 10.1097/01.CHI.0000046830.95464.33. [DOI] [PubMed] [Google Scholar]
- 72.Geller B. Attention-deficit hyperactivity disorder with bipolar disorder: a familial subtype? (Discussion). J Am Acad Child Adolesc Psychiatry. 1997;36:1387–1390. doi: 10.1097/00004583-199710000-00020. [DOI] [PubMed] [Google Scholar]
- 73.Faraone SV., Biederman J., Mennin D., Wozniak J., Spencer T. Attentiondeficit hyperactivity disorder with bipolar disorder: a familial subtype? J Am Acad Child Adolesc Psychiatry. 1997;36:1378–87. doi: 10.1097/00004583-199710000-00020. [DOI] [PubMed] [Google Scholar]
- 74.Henin A., Biederman J., Mick E., et al. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry. 2005;58:554–561. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 75.Hazell P. Pediatric bipolar disorder: from the perspective of Australia and New Zealand. In: Diler RS, ed. Pediatric Bipolar Disorder: a Global Perspective. New York, NY: Nova Biomedical Books; 2007:33–55. [Google Scholar]
- 76.Hillegers MHJ., Reichart CG., Wals M., Verhulst FC., Ormel J., Nolen WA. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disord. 2005;7:344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 77.Chang KD., Steiner H., Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. J Am Acad Child Adolesc Psychiatry. 2000;39:453–460. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 78.Kutscher SP., Marton P., Korenblum M. Relationship between psychiatric illness and conduct disorder in adolescents. Can J Psychiatry. 1989;34:526–529. doi: 10.1177/070674378903400608. [DOI] [PubMed] [Google Scholar]
- 79.Biederman J., Faraone SV., Chu MP., Wozniak J. Further evidence of a bidirectional overlap between juvenile mania and conduct disorder in children. J Am Acad Child Adolesc Psychiatry. 1999;38:468–476. doi: 10.1097/00004583-199904000-00021. [DOI] [PubMed] [Google Scholar]
- 80.Biederman J., Mick E., Wozniak J., Monuteaux MC., Galdo M., Faraone SV. Can a subtype of conduct disorder linked to bipolar disorder be identified? integration of findings from the Massachusetts General Hospital Pediatric Psychopharmacology Research Program. Biol Psychiatry. 2003;53:952–960. doi: 10.1016/s0006-3223(03)00009-x. [DOI] [PubMed] [Google Scholar]
- 81.Geller B., Fox LW., Clark KA. Rate and predictors of prepubertal bipolarity during follow-up of 6- to 12-year-old depressed children. J Am Acad Child Adolesc Psychiatry. 1994;33:461–468. doi: 10.1097/00004583-199405000-00003. [DOI] [PubMed] [Google Scholar]
- 82.Birmaher B., Kennah A., Brent D., Ehmann M., Bridge J., Axelson D. Is bipolar disorder specifically associated with panic disorder in youths? J Clin Psychiatry. 2002;63:414–419. doi: 10.4088/jcp.v63n0507. [DOI] [PubMed] [Google Scholar]
- 83.Masi G., Toni C., Perugi G., Travierso MC., Millepiedi S., Mucci M., et al. Externalizing disorders in consecutively referred children and adolescents with bipolar disorder. Compr Psychiatry. 2003;44:184–189. doi: 10.1016/S0010-440X(03)00002-6. [DOI] [PubMed] [Google Scholar]
- 84.Barzman DH., DelBello MP., Fleck DE., Lehmkuhl H., Strakowski SM. Rates, types, and psychosocial correlates of legal charges in adolescents with newly diagnosed bipolar disorder. Bipolar Disord. 2007;9:339–344. doi: 10.1111/j.1399-5618.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 85.Endrass J., Vetter S., Gamma A., et al. Are behavioral problems in childhood and adolescence associated with bipolar disorder in early adulthood? Eur Arch Psychiatry Clin Neurosci. 2007;257:217–221 . doi: 10.1007/s00406-006-0710-2. [DOI] [PubMed] [Google Scholar]
- 86.Vornik LA., Brown ES. Substance-abuse comorbidity in bipolar disorder: general considerations and treatment approaches. Clin Approaches Bipolar Disord. 2007;6:3–11 . [Google Scholar]
- 87.Lynskey MT., Fergusson DM., Horwood LJ. The origins of the correlations between tabacco, alcohol, and cannabis use during adolescence. J Child Psychol Psychiatry. 1998;39:995–1005. [PubMed] [Google Scholar]
- 88.Swanson JW., Holzer CE., Ganju VK., Tsumotu Jono R. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area Surveys. Hosp Community Psychiatry. 1990;41:761–770. doi: 10.1176/ps.41.7.761. [DOI] [PubMed] [Google Scholar]
- 89.Lavander E., Frye MA., McElroy SL., et al. Alcoholism and anxiety in bipolar illness: differential lifetime anxiety comorbidity in bipolar I women with and without alcoholism. J Affect Disord . 2007;101:211–217. doi: 10.1016/j.jad.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 90.Angst J., Gamma A., Endrass J., et al. Is the association of alcohol use disorders with major depressive disorder a consequence of undiagnosed bipolar-II disorder? Eur Arch Psychiatry Clin Neurosci. 2006;256:452–457. doi: 10.1007/s00406-006-0673-3. [DOI] [PubMed] [Google Scholar]
- 91.McDermont BE., Quanbeck CD., Frye MA. Comorbid substance use disorder in women with bipolar disorder associated with criminal arrest. Bipolar Disord. 2007;9:536–540. doi: 10.1111/j.1399-5618.2007.00346.x. [DOI] [PubMed] [Google Scholar]
- 92.Angst J., Angst F., Gerber-Werder R., Gamma A. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years' follow-up. Arch Suicide Res. 2005;9:279–300. doi: 10.1080/13811110590929488. [DOI] [PubMed] [Google Scholar]
- 93.Kessing LV., Andersen PK. Does the risk of developing dementia increase with the number of episodes in patients with depressive disorder and in patients with bipolar disorder? J Neurol Neurosurg Psychiatry. 2004;75:1662–1666. doi: 10.1136/jnnp.2003.031773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Angst J., Preisig M. Outcome of a clinical cohort of unipolar, bipolar and schizoaffective patients. Results of a prospective study from 1959 to 1985. SchweizArch Neurol Psychiatr. 1995;146:17–23. [PubMed] [Google Scholar]
- 95.Angst J., Gamma A., Gerber-Werder R., Zarate CA Jr., Manji HK. Does long-term medication with lithium, clozapine or antidepressants prevent or attenuate dementia in bipolar and depressed patients? int J Psychiatr Clin Pract. 2007;11:2–8. doi: 10.1080/13651500600810133. [DOI] [PubMed] [Google Scholar]
- 96.Nunes PV., Forlenza OV., Gattaz WF. Lithium and risk for Alzheimer's disease in elderly patients with bipolar disorder. Br J Psychiatry. 2007;190:359–360. doi: 10.1192/bjp.bp.106.029868. [DOI] [PubMed] [Google Scholar]
- 97.Dunn N., Holmes C., Mullee M. Does lithium therapy protect against the onset of dementia? Alzheimer Dis Assoc Disord. 2005;19:20–22. doi: 10.1097/01.wad.0000155068.23937.9b. [DOI] [PubMed] [Google Scholar]
- 98.Ôsby U., Brandt L., Correia N., Ekbom A., Sparén P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- 99.McCombs JS., Ahn J., Tencer T., Shi L. The impact of unrecognized bipolar disorders among patients treated for depression with antidepressants in the fee-for-services California Medicaid (Medi-Cal) program: a 6-year retrospective analysis. J Affect Disord. 2007;97:171–179. doi: 10.1016/j.jad.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 100.auser M., Pfennig A., Ôzgûrdal S., Heinz A., Bauer M., Juckel G. Early recognition of bipolar disorder. Eur Psychiatry. 2007;22:92–98. doi: 10.1016/j.eurpsy.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 101.irschfeld RMA., Calabrese JR., Weissman MM., et aI. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64:53–59. doi: 10.4088/jcp.v64n0111. [DOI] [PubMed] [Google Scholar]
- 102.Allilaire JF., Hantouche EG., Sechter D., et al. Fréquence et aspects cliniques du trouble bipolaire II dans une étude rnulticentrique française: EPIDEP. Encéphale. 2001;XXVII:149–158. [PubMed] [Google Scholar]
- 103.Hantouche E., Angst J., Lancrenon S., Gérard D., Allilaire J-F. Faisabilité de l'autoévaluation dans le dépistage de l'hypomanie. Feasibility of auto-evaluation in the detection of hypomania. Annales Médico Psychologiques. 2006;164:721–725. [Google Scholar]
- 104.Angst J., Adolfsson R., Benazzi F., et al. The HCL-32: Towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord. 2005;88:217–233. doi: 10.1016/j.jad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 105.Wu YS., Angst J., Ou CS., Chen HC., Lu RB. Validation of the Chinese version of the Hypomania Checklist (HCL-32) as an instrument for detecting hypomania in patients with mood disorders. J Affect Disord. 2008;106:133–143. doi: 10.1016/j.jad.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 106.Vieta E., Sanchez-Moreno J., Bulbena A., Chamorro K., Ramos JL., Artal J., et al. Cross validation with the mood disorder questionnaire (MDQ) of an instrument for the detection of hypomania in Spanish: the 32 item hypomania symptom check list (HCL-32). J Affect Disord. 2007;101:43–55. doi: 10.1016/j.jad.2006.09.040. [DOI] [PubMed] [Google Scholar]
- 107.Wing JK., Bebbington P., Robins LN., eds What is a Case? The Problem of Definition in Psychiatric Community Surveys. London, UK: Grant Mclntyre; 1981 [Google Scholar]
- 108.Eaton WW., Regier DA., Locke BZ., Taube CA. The NIMH Epidemiologic Catchment Area Program. In: Wing JK, Bebbington PE, Robins LN, eds. What is a Case? The Problem of Definition in Psychiatric Community Surveys. London, UK: Grant Mclntyre; 1981;223-236:99–106. [Google Scholar]
- 109.opeland JRM. What is a “case”? A case for what? In: Wing JK, Bebbington PE, Robins LN, eds. What is a Case? The Problem of Definition in Psychiatric Community Surveys. London, UK: Grant Mclntyre; 1981:9–11. [Google Scholar]
- 110.Angst J. The bipolar spectrum. Br J Psychiatry. 2007;190:189–191. doi: 10.1192/bjp.bp.106.030957. [DOI] [PubMed] [Google Scholar]