Abstract
Overwhelming evidence suggests that compromised neuropsychological function is frequently observed in schizophrenia. The neuropsychological profile is typically characterized by prominent specific deficits in memory and learning, working memory, executive functions, attention, and processing speed, which are evident on a background of a generalized cognitive deficit This paper provides a review of studies of neuropsychological functioning in schizophrenia. The main cognitive ability areas affected in schizophrenia are described, and the degree of impairment in each ability area as found in studies of schizophrenia patients is summarized, based on meta-analytic findings. Recent studies that have compared neuropsychological functioning across psychotic disorders are presented, and finally, neuropsychological assessment batteries specifically developed for schizophrenia are introduced.
Keywords: schizophrenia, neuropsychology, assessment, meta-analysis, impairment
Abstract
Existe abundante evidencia que sugiere que en la esquizofrenia es frecuente observar alteraciones de la función neuropsicológica. El perfil neuropsicológico se caracteriza típicamente por marcados déficit específicos en la memoria y el aprendizaje, la memoria de trabajo, las funciones ejecutivas, la atención y la velocidad de procesamiento, los que son evidentes en el contexto de un déficit cognitivo generalizado. Este artículo proporciona una revisión de estudios acerca del funcionamiento neuropsicológico en la esquizofrenia. Se describen las principales áreas de capacidades cognitivas que están afectadas en la esquizofrenia y se resume el grado de deterioro de cada área de capacidad como se ha establecido en estudios de pacientes con esquizofrenia de acuerdo con los hallazgos de estudios de meta -análisis. Se presentan estudios recientes que han comparado el funcionamiento neuropsicológico en diversos trastornos psicóticos y finalmente se incorporan baterías de evaluación neuropsicológica específicamente desarrolladas para la esquizofrenia.
Abstract
Les preuves d'un dysfonctionnement neuropsychologique fréquent dans la schizophrénie ne se comptent plus. Le profil neuropsychologique se caractérise généralement par des déficits spécifiques importants de la mémoire et de l'apprentissage, de la mémoire de travail, des fonctions exécutives, de l'attention et de la vitesse de traitement de l'information, qui s'inscrivent dans un contexte de déficit cognitif généralisé. Cet article passe en revue des études sur le fonctionnement neuropsychologique dans la schizophrénie. Il décrit les principales aires de compétence cognitive touchées dans la shizophrénie et résume le degré d'atteinte de chaque aire de compétence à partir d'études sur les schizophrènes, basées sur des données métaanalytiques. Il rapporte enfin des études récentes qui ont comparé le fonctionnement neuropsychologique au cours des troubles psychotiques et finalement, présente des batteries de tests d'évaluation neuropsychologique développés spécifiquement pour la schizophrénie.
Patients with schizophrenia manifest a wide range of symptoms, including delusions, hallucinations, and impairments in communication, as well as motor, volitional, and emotional disorders. Through careful and comprehensive research it has become increasingly apparent that, in addition to the diverse symptoms that form the clinical definition of the illness, the disorder is, to a variable degree, accompanied by a cognitive impairment.1,2
Various observations (for review see ref 2) have led to the hypothesis that compromised cognitive functioning is a core feature of schizophrenia and not an artifact of other symptoms, treatment for the illness, or aspects of the course of the illness.3,4 It has further been proposed that the well-known diversity of schizophrenia in terms of functional outcome and recovery from the illness is best characterized by cognitive deficits, not by the classical symptoms.5 DSM-5, acknowledging the importance of cognition in schizophrenia, is likely to recommend obtaining a formal neuropsychological assessment in individuals with psychosis.6
This paper will provide an overview of findings from studies of cognitive functioning in schizophrenia. It will highlight cognitive functions which are severely impaired, as well as functions that are relatively spared; compare cognitive functioning across psychotic disorders; discuss the classification of cognitive impairment at the individual level, and present common cognitive assessment batteries.
Cognitive impairment in schizophrenia
Most neuropsychological assessment batteries used in schizophrenia studies have been adapted from clinical neuropsychology, which assesses the profile of neuropsychological strengths and weaknesses of an individual.7 In the first section of this paper we will review the study of cognitive functioning in schizophrenia. We will define the main cognitive ability areas, and describe the degree of impairment in each ability area as found in studies of schizophrenia patients. For descriptive purposes we have adopted the convention proposed by Cohen,8 and applied in meta-analytic studies that cognitive functioning is within normal limits if performance scores are within one fifth of a standard deviation of the normative standards, is mildly impaired if scores fall between 0.2 and 0.5 SDs below the normative standards, is moderately impaired between 0.5 and 0.8 SDs below the normative standards, and is severely impaired at 0.8 or more SD below the normative standards.
General intellectual ability
Dating back to the work of Spearman,9 a distinction has been made between general and specific cognitive abilities. Two widely used indices of generalized cognitive performance have been applied in schizophrenia research: general measures of intelligence quotient, or IQ, and composite scores or profiles derived from test batteries comprising multiple neuropsychological tests. While both provide a measure of an individual's overall cognitive functioning, the results of these assessments often do not overlap to a substantial degree. Neuropsychological test batteries typically focus on assessment of multiple cognitive abilities, such as memory, executive functions, and attention, and these include a strong component of novelty of testing requirements. IQ tests, on the other hand, have a lesser emphasis on specific abilities and novelty and greater emphasis on the assessment of crystallized abilities.10
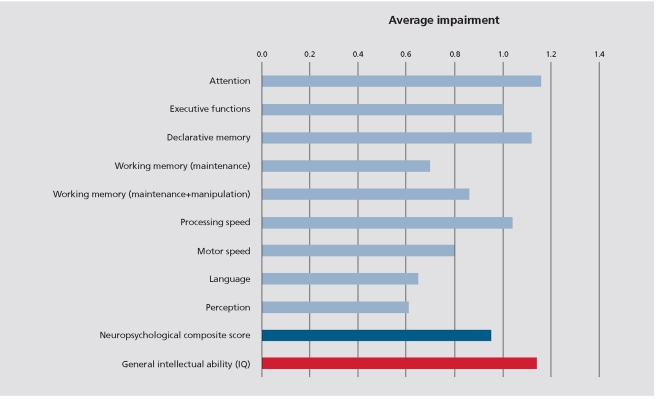
Schizophrenia patients show a substantial and very severe generalized impairment (Figure 1). As demonstrated by meta-analytic studies,11-16 the generalized impairment as indexed by IQ seems to be consistently greater than the one indexed by neuropsychological composite scores (Figure 1). The impairment in performance IQ is almost 50% larger than that observed for verbal IQ.2 The impairment in general ability seems to be almost as severe as those observed for more specific neuropsychological functions, suggesting that any specific neuropsychological deficit in schizophrenia occurs in the context of a background of a very severe general intellectual impairment.2
Figure 1. Neuropsychological performance profile of schizophrenia. Summary of results from meta-analytic studies presented in effect-size units (median effect size was calculated from available meta-analyses).
Specific cognitive abilities
Attention
Early descriptions of schizophrenia recognized attentional impairments as fundamental aspects of schizophrenia long before the advent of formal neuropsychological testing or modern experimental psychology.17,18 It is clear that attention is not a unitary construct. Posner and Petersen19 proposed that attention should be broken down into three main functions: alerting, orienting, and executive control. Alerting is defined as achieving and maintaining an alert state; orienting is the selection of information from sensory input; and executive control is defined as resolving conflict among responses.20
Alerting has received considerable research attention in schizophrenia, and simple reaction time studies using different versions of Continuous Performance Tests have been conducted. Meta-analytic studies suggest moderate to severe impairments in this attentional domain (Figure 1).11,12,14 Orienting has not been studied as much. It is important to remember that attentional impairments may disrupt many other cognitive functions. One could assume that poor attention would prevent many types of information from being processed appropriately. However, correlational studies have generally demonstrated that attentional dysfunction explains only a small proportion of the variance in other cognitive functions in schizophrenia.21,22
Executive functions
The term “executive functions” has its historical roots in attempts to delineate higher cognitive functions of the prefrontal cortex, and has been used synonymously with the term “frontal-lobe functions.” More recent conceptualizations of executive functions include fractionation into subprocesses,23 and the view that not all executive processes are uniquely sustained by the frontal cortex. Specifically, some executive processes may be sustained by a distributed cortical network, rather than by a unique frontal region which may or may not be associated with the frontal lobes.24,30
Executive functions are involved in the maintenance and shifting of cognitive and behavioral responses to environmental demands permitting the control of action and longterm goal-directed behavior.31,32 Such control requires consideration of current and future circumstances, generation and evaluation of response alternatives, choice and implementation of a specific course of action and monitoring/reevaluation in response to environmental feedback. Abilities underlying such activities are thought to include: searching long-term knowledge stores, abstraction and planning, reasoning and problem-solving skills, initiation, self-monitoring, mental flexibility, and inhibition of immediate responses in pursuit of longer-term goals.32
A great deal of research has focused on executive dysfunction in schizophrenia. First, many of the clinical features of schizophrenia are phenomenologically similar to those associated with frontal lesions, such as reduced spontaneity, avolition, mental rigidity, and lack of social judgment.33,34 A second reason has to do with the dominant view about the etiology of schizophrenia. The socalled “neurodevelopmental hypothesis” postulates that schizophrenia arises from early, possibly fetal brain abnormalities of genetic and/or environmental origin which remains largely “static” or “silent” until it interacts with normal brain maturation processes, namely, those of the frontal lobes.35,36
The most commonly employed tests in studies of executive functions in schizophrenia include the Wisconsin Card Sorting Test (WCST), the Stroop test, the Controlled Oral Word Association test (COWAT), and the Trail Making Test - Part B (TMT-B) (For a detailed description of the tests see ref 37). These tasks have been traditionally regarded as executive tests, since successful performance requires engagement of some form of executive control in addition to any of the more basic cognitive processes.32 As indicated by meta-analytic studies impairments in all of the above tests performance are severe (Figure 1).11,16,38,39
Memory
Kraepelin17 wrote that among individuals with schizophrenia memory “is comparatively little disordered.”
Bleuler18 was even more unequivocal when he wrote that “memory as such does not suffer in this disease.” Their perspective regarding memory in schizophrenia was based on day-to-day clinical observations and on informal testing, indicating that patients were reasonably adept at remembering details of their lives and the lives of their caregivers, and could recall information learned in school.40 Modern views of memory disorder in schizophrenia are based on more precise, standardized neuropsychological measurement techniques, and contrast with the early clinical observations of memory functioning.
Influential and well-researched classification schemes have distinguished two types of long-term memory, declarative memory and nondeclarative memory, characterized by several key differences. Declarative memory encompasses both episodic memory (memory for events) and semantic memory (memory for facts), whereas nondeclarative memory encompasses simple classical conditioning, nonassociative learning, priming, and procedural memory. Unlike declarative memory, nondeclarative memory can take place without conscious awareness that anything has been learned.41
Deficits in declarative memory are consistently reported in schizophrenia. Of 110 studies reviewed by Cirello and Seidman,40 101 found evidence of impairment among schizophrenia patients on measures of declarative memory. Meta-analyses consistently report severe impairments in immediate and delayed verbal and nonverbal memory in schizophrenia, commonly assessed using verbal or nonverbal list-learning tests (Figure 1).11,12,14,16,42
Nondeclarative memory has been considerably less studied in schizophrenia, and has not been the focus of metaanalytic investigations. Nevertheless, research suggests that this aspect of memory is relatively preserved in schizophrenia patients. For example, procedural learning (“learning by doing”) may be defined as the development of skills in which the strategy of execution cannot be explicitly described. Schizophrenia patients show near perfect performance43,44 or only mild impairment45 on tasks of procedural learning.
Working memory
Working memory, a term first introduced by Miller, Galanter, and Pribram46 has been often defined as a “system for temporarily storing and manipulating information in the execution of complex cognitive tasks such as
learning, reasoning and comprehension.” 47 The criterion of transience distinguishes working memory from other forms of memory where the information of interest is maintained over longer periods of time.48
In accordance with the Baddeley and Hitch (1974) model of working memory, in the schizophrenia literature there is a tendency to use a process-oriented definition of working memory with tasks requiring storage and maintenance compared with tasks requiring both maintenance and manipulation of task-relevant information.49 A distinction is also made between two modalities of working memory: verbal and visuospatial, again in line with the Baddeley and Hitch (1974) model.
The most commonly employed tests in studies of working memory are the Digit Span and Spatial Span.50 These tests include two conditions: forward and backward; the former is a task of maintenance only, while the latter requires both maintenance and manipulation. Meta-analytic studies (Figure 1) suggest that impairments in tasks requiring both maintenance and manipulation of information are noticeably larger in schizophrenia than tasks requiring maintenance only12,16,42,51,52
Processing speed
“Processing speed” refers to the speed with which different cognitive operations can be executed. Psychometrically, processing speed is typically indexed by the number of trials of a simple task that a subject can complete during a brief interval. The importance of processing speed lies in the fact that many higher cognitive operations - including perceptual processes, encoding and retrieval operations, transformation of information held in active memory, and decision processes - involve internal dynamics that are speed-dependent to some extent. Coding tasks, such as the Wechsler Digit Symbol Coding, are sensitive to a wide array of neuropsychiatric conditions50 including schizophrenia, and are particularly impaired in schizophrenia.12 According to meta-analyses,11,12,16,39,52 both simple and more complex tasks of processing speed show a severe and substantial impairment in schizophrenia.
Language, perception, visuospatial ability, and motor speed
Language is often assessed using reading and spelling of single words, or vocabulary tests, skills acquired quite early in life. As indicated by the meta-analytic studies, these functions are relatively preserved in schizophrenia, with only mild impairments (Figure 1).11,12,16,52 Metaanalyses suggest moderate to severe deficits in tasks of simple motor speed.11,12,16 The magnitude of these deficits is smaller than the one evident for memory or executive functions (Figure 1). Moderate to severe impairments have also been observed in pure perceptual problems (Figure 1).11,12,16
Possible moderating factors
A possible explanation for the presence of cognitive deficits in schizophrenia is that the neurocognitive deficit is secondary, peripheral, rather than central to the illness. Thus, symptom severity should be associated with severity of cognitive impairments. Other demographic characteristics such as age, education, or duration of illness may also account for some of the neuropsychological deficits. Overall studies indicate that the effect of moderator variables is quite limited: medication status, duration of illness, severity of psychopathology, and positive symptoms were not significantly associated with severity of neuropsychological impairment.11,12,38,42 There is some consistency in documenting an association between negative symptoms and severity of cognitive deficits, in particular deficits in executive functions,5,13,38 and considerable inconsistency with regard to the association of positive symptoms to neuropsychological functioning (see for example, refs 38,42). However, even when strong associations between symptom severity and cognitive function are evident, even schizophrenia patients with low severity of such symptoms exhibit profound cognitive impairments.42 The inconsistency regarding the association of positive symptoms and cognitive function strongly suggests that neuropsychological test results should be interpreted in great caution if carried out when patients are actively psychotic. In research settings, cognitive assessments are almost always done when the patient is improved or in remission.
Cognitive deficits in other psychotic disorders
The evidence presented in the previous sections indicates that individuals with schizophrenia present severe impairments in attention, executive functions, episodic memory, certain aspects of working memory performance, and processing speed. Cognitive functions that are relatively spared in schizophrenia include language functions, perceptual processes and nondeclarative memory. Studies have suggested that patients with other psychotic disorders could also demonstrate a disruption of normal cognitive performance, but results have not always been consistent.
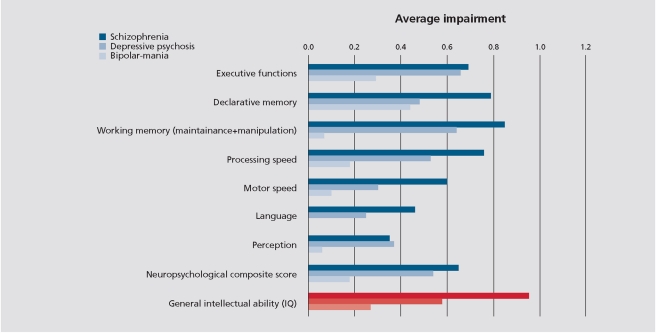
The question of specificity of cognitive impairment has been recently investigated in two large epidemiological samples.53,54 These studies compared neuropsychological functioning between psychotic patients with a diagnosis of schizophrenia, bipolar mania, and depressive psychosis, and have shown that differences in neuropsychological performance between schizophrenia and other psychotic disorders are quantitative and not qualitative. Cognitive deficits are present in all psychotic disorders following the first psychotic episode, but are most severe and pervasive in schizophrenia and least so in bipolar manic disorder (Figure 2).
Figure 2. Neuropsychological performance profile of schizophrenia, psychotic major depressive disorder, and psychotic bipolar disorder. Performance was compared with healthy controls and is presented in standard deviation units (effect sizes). Data are from the AESOP first-episode study53 .
The results of meta-analyses clearly demonstrate that the cognitive deficit also persists throughout euthymic states in bipolar mania,55,58 although it is slightly less pronounced.57 These results suggest that, as in schizophrenia, cognitive deficit is not simply a by-product of other symptoms.59 However, some of the cognitive deficits observed in euthymic patients could be related to the effects of illness-related factors. Similarly to schizophrenia,39 medication effects on the magnitude of processing speed impairment have been reported.60 Significant moderator effects on cognition in bipolar mania have also been reported for age of onset,60 number of manic episodes,61,62 and duration of illness.63 Unlike bipolar mania, however, there is less evidence for cognitive impairments in remitted patients with a history of depression,64 but further studies are needed to examine cognitive deficits in remitted patients with major depression, especially psychotic depression.59
Epidemiological studies of premorbid cognitive functioning (eg, in childhood or adolescence) may point to a possible qualitative difference between different psychotic disorders. There is a well documented premorbid cognitive deficit in schizophrenia. A recent meta-analysis estimated that, on average, future schizophrenia cases exhibit an 8-point deficit (.5 standard deviations) in their childhood IQ. 65 Recent studies suggest that abnormal premorbid IQ is also a characteristic of depression.66,67 In contrast, epidemiological research suggests that future bipolar disorder patients may have superior intellectual ability. This has been reported in some,66,68,69 although not all studies,70,71 and requires further investigation. If supported, the differences in premorbid functioning may point to potential developmental discrimination between schizophrenia, depression, and bipolar disorder.
“Cognitive impairment” in schizophrenia: who is impaired and who is not?
From the previous sections it is well accepted that schizophrenia patients, as a group, have cognitive deficits. Several previous studies, however, demonstrate that in some persons with schizophrenia, cognitive abilities are unimpaired or normal.3,72,74 The central issue is which patients can be identified as having a cognitive deficit.75 Some conceptualizations of this issue have relied on approaches from clinical neuropsychology to define cognitive impairment. These definitions are based on a performance deficit compared with a healthy control population (or normative data), such as one standard deviation below the mean on one or more areas of cognitive function. Using such definitions the estimated percentage of schizophrenia patients who have a cognitive impairment has varied from between 70% to 80%54,73 to no more than 55 %.74
A recent study54 compared various classification methods of cognitive impairment using neuropsychological assessment data from the Suffolk County Mental Health Project cohort.76,77 Of the 94 persons with schizophrenia in the study, 82% to 84% were classified as neuropsychologically impaired (Figure 3) . The rate of impairment was lower for other psychotic disorders.54
Figure 3. Rates and severity of cognitive impairment in schizophrenia patients. Data came from the Suffolk County Mental Health Project cohort54,76,77 (N=94 cases). Definition of impairment Mild: Performance between 1 and 2 standard deviations below norms on at least 2 cognitive ability areas. Moderate Performance between 2 and 3 standard deviations below norms on at least 2 cognitive ability areas. Severe: Performance 3 or more standard deviations below norms on at least 2 cognitive ability areas.
Schizophrenia-specific and abbreviated neuropsychological assessment batteries
Traditionally, many of the neuropsychological assessment batteries used are long and complex and may require several hours to administer.7 The adaptation of assessment batteries for schizophrenia research has kept some of the length that was originally necessary for individual assessment but may no longer be necessary for clinically oriented research.7 Until recently there was no standard, easily administered test battery that specifically and efficiently assesses the important cognitive deficits in patients with schizophrenia.
Short assessment of general intellectual ability (IQ)
As described above schizophrenia patients show a substantial and very severe generalized impairment. Therefore, IQ total score can be a useful single descriptive measure of overall intellectual ability and also provide an interpretive context for other test results. Blyler et al78 developed a short form of the Wechsler Adult Intelligence Scales (WAIS)-III50 that was highly predictive of full-scale IQ in individuals with schizophrenia (R2=0.90; using the Information, Block design, Arithmetic, and Digit symbol coding subtests). We recently demonstrated that a two-subtest combination (Similarities and Arithmetic) could also provide accurate full-scale IQ estimates in schizophrenia patients (R2 = 0.91, Sela et al, unpublished data).
Short assessment of specific cognitive functions
The MATRICS Consensus Cognitive Battery (MCCB)79,80 is a neuropsychological assessment battery developed through an expert consensus process initially designed to establish an accepted way to evaluate cognition-enhancing agents in schizophrenia. Nevertheless, it also aids in providing a standardized evaluation of the core cognitive deficits of schizophrenia. Following a review and integration of results from factor-analytic studies of cognitive performance in schizophrenia, seven separable cognitive domains were determined, including speed of processing, attention/vigilance, working memory, verbal learning, visual learning, and reasoning and problem-solving (executive functions). The seventh domain, social cognition, was included because it was viewed as an ecologically important domain of cognitive deficit in schizophrenia that shows promise as a mediator of neurocognitive effects on functional outcome, although studies of this domain in schizophrenia are too new for such measures to have been included in the various factor-analytic studies.79 The MCCB takes approximately 60 minutes to complete, has alternate forms, its reliability, validity, and comparability of original forms have been established empirically, and normative data has been collected.79,80 Another abbreviated assessment battery (Brief Assessment of Cognition in Schizophrenia - BACS)7 evaluates four of the seven cognitive domains included in the MCCB: executive functions (reasoning and problem solving), processing speed, verbal memory, and working memory. The battery takes approximately 30 minutes to administer, has alternate forms, established reliability and validity, and available normative data.81 Other abbreviated test batteries are also available with normative data (eg, Repeatable Battery for the Assessment of Neuropsychological Status8283; CogState,84 a computerized battery) but often do not assess all seven cognitive domains identified by the MATRICS as important for schizophrenia.
Summary and conclusions
Assessment of neuropsychological functions greatly broadens the understanding of schizophrenia. In this paper, we have summarized the evidence for cognitive impairments in schizophrenia, and for methods of assessment. One of the main incentives for understanding the signature of cognitive impairment in schizophrenia is the strong relationship between cognitive performance and functional skills and functional outcome.85 For this, cognitive impairment may be the most relevant aspect of the illness. We are only beginning to understand the role of specific cognitive functions in different aspects of outcome,86 and better characterization of fundamental impaired cognitive processes is critical. Additionally, cognitive functioning may be used as a vulnerability marker.87,88 Cognitive impairments are proving to be one of the symptoms within a cluster that may eventually enhance the ability to determine who is at risk of devel oping a psychotic disorder, and, in those already ill, may provide a prognostic marker for future functional outcome.2 Hence the importance of assessing and understanding the cognitive impairment in schizophrenia.
REFERENCES
- 1.Seidman LJ. Schizophrenia and brain dysfunction: an integration of recent neurodiagnostic findings. Psychol Bull. 1983;94:195–238. [PubMed] [Google Scholar]
- 2.Reichenberg A, Harvey PD. Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychol Bull. 2007;133:833–858. doi: 10.1037/0033-2909.133.5.833. [DOI] [PubMed] [Google Scholar]
- 3.Kremen WS, Seidman LJ, Faraone SV, Toomey R, Tsuang MT. The paradox of normal neuropsychological function in schizophrenia. J Abnorm Psychol. 2000;109:743–752. doi: 10.1037//0021-843x.109.4.743. [DOI] [PubMed] [Google Scholar]
- 4.Elvevag B, Goldberg TE. Cognitive impairment in schizophrenia is the core of the disorder. Crit Rev Neurobiol. 2000;14:1–21. [PubMed] [Google Scholar]
- 5.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association DSM-5 Available at: http://www.dsm5org/Pages/ RecentUpdatesaspx. Accessed April 6 2010 [Google Scholar]
- 7.Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68:283–297. doi: 10.1016/j.schres.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1988 2nd ed. Hillsdale, NJ: L. Erlbaum Associates. [Google Scholar]
- 9.Spearman C. The Abilities of Men, their Nature and Measurement. 1927 New York, NY: MacMillan Company. [Google Scholar]
- 10.Bratti IM, Blder, R.M. . Neurocognitive deficits and first-episode schizophrenia: characterization and course. In: Sharma T, Harvey, PD, eds. The Early Course of Schizophrenia. Oxford, UK: Oxford University Press 2006:87–110. [Google Scholar]
- 11.Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–445. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- 12.Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: a metaanalytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry. 2007;64:532–542. doi: 10.1001/archpsyc.64.5.532. [DOI] [PubMed] [Google Scholar]
- 13.Henry JD, Crawford JR. A meta-analytic review of verbal fluency deficits in schizophrenia relative to other neurocognitive deficits. Cogn Neuropsychiatry. 2005;10:1–33. doi: 10.1080/13546800344000309. [DOI] [PubMed] [Google Scholar]
- 14.Fioravanti M, Carlone O, Vitale B, Cinti ME, Clare L. A meta-analysis of cognitive deficits in adults with a diagnosis of schizophrenia. Neuropsycholol Rev. 2005;15:73–95. doi: 10.1007/s11065-005-6254-9. [DOI] [PubMed] [Google Scholar]
- 15.Laws KR. A meta-analytic review of Wisconsin Card Sort studies in schizophrenia: general intellectual deficit in disguise? Cogn Neuropsychiatry. 1999;4:1–30. doi: 10.1080/135468099396025. [DOI] [PubMed] [Google Scholar]
- 16.Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23:315–336. doi: 10.1037/a0014708. [DOI] [PubMed] [Google Scholar]
- 17.Kraepelin E. Dementia Praecox. Melbourne, FL: Robert E. Krieger 1913 [Google Scholar]
- 18.Bleuler E. Dementia Praecox; or, the Group of Schizophrenias. Madison, CT: International Universities Press 1952 [Google Scholar]
- 19.Posner MI, Petersen SE. The attention system of the human brain. Ann Rev Neurosci. 1990;13:25–42. doi: 10.1146/annurev.ne.13.030190.000325. [DOI] [PubMed] [Google Scholar]
- 20.Fan J, McCandliss BD, Sommer T, Raz A, Posner MI. Testing the efficiency and independence of attentional networks. J Cogn Neurosci. 2002;14:340–347. doi: 10.1162/089892902317361886. [DOI] [PubMed] [Google Scholar]
- 21.Keefe RS, Bilder RM, Harvey PD, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology. 2006;31:2033–2046. doi: 10.1038/sj.npp.1301072. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg TE, David A. Gold JM. Neurocognitive deficits in schizophrenia. In: Hirsch SR, Weinberger DR, eds. Schizophrenia. 2nd ed. Oxford, UK: Blackwell Publishing 2003:168–186. [Google Scholar]
- 23.Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- 24.Baddeley AD, Della Sala S, Papagno C, Spinnler H. Dual-task performance in Dysexecutive and Nondysexecutive patients with frontal lesion. Neuropsychology. 1997;11:187–194. doi: 10.1037//0894-4105.11.2.187. [DOI] [PubMed] [Google Scholar]
- 25.Allain P, Etcharry-Bouyx F, Le Gall D. A case study of selective impairment of the central executive component of working memory after a focal frontal lobe damage. Brain Cogn. 2001;45:21–43. doi: 10.1006/brcg.2000.1249. [DOI] [PubMed] [Google Scholar]
- 26.Van der Linden M, Coyette F, Seron X. Selective impairment of the “central executive” component of working memory: a single case study. Cogn Neuropsychology. 1992;9:301–336. [Google Scholar]
- 27.Carpenter PA, Just MA, Reichle ED. Working memory and executive function: evidence from neuroimaging. Curr Opin Neurobiol. 2000;10:195–199. doi: 10.1016/s0959-4388(00)00074-x. [DOI] [PubMed] [Google Scholar]
- 28.Garavan H, Ross TJ, Li SJ, Stein EA. A parametric manipulation of central executive functioning. Cereb Cortex. 2000;10:585–592. doi: 10.1093/cercor/10.6.585. [DOI] [PubMed] [Google Scholar]
- 29.Andres P. Frontal cortex as the central executive of working memory: time to revise our view. Cortex. 2003;39:871–895. doi: 10.1016/s0010-9452(08)70868-2. [DOI] [PubMed] [Google Scholar]
- 30.Andres P, Van der Linden M. Supervisory attentional system in patients with focal frontal lesions. J Clin Exp Neuropsychol. 2001;23:225–239. doi: 10.1076/jcen.23.2.225.1212. [DOI] [PubMed] [Google Scholar]
- 31.Shallice T, Burgess P. The domain of supervisory processes and temporal organization of behaviour. In: Roberts AC, Robbins TW, Weiskrantz L, eds. The Prefrontal Cortex Executive and Cognitive Functions. New York, NY: Oxford University Press 1998:2–35. [Google Scholar]
- 32.Palmer BW, Heaton RK. Executive dysfunction in schizophrenia. In: Sharma T, Harvey PD, eds. Cognition in Schizophrenia: Impairments, Importance and Treatment Strategies. Oxford, UK: Oxford University Press 2000:51–72. [Google Scholar]
- 33.David AS. Frontal lobology--psychiatry's new pseudoscience. Br J Psychiatry. 1992;161:244–248. doi: 10.1192/bjp.161.2.244. [DOI] [PubMed] [Google Scholar]
- 34.Benson DF, Miller, B.L. . Frontal lobes: clinical and anatomic aspects. In: Feinberg TE, Farah MJ, eds. Behavioral Neurology and Neuropsychology. New York, NY: McGraw-Hill 1997:401–408. [Google Scholar]
- 35.Murray RM, Lewis SW. Is schizophrenia a neurodevelopmental disorder? BMJ (Clin Res Ed) 1987;295:681–682. doi: 10.1136/bmj.295.6600.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 37.Spreen O, Strauss E. A Compendium of Neuropsychological Tests. 2nd ed. New York, NY: Oxford University Press 1998 [Google Scholar]
- 38.Johnson-Selfridge M, Zalewski C. Moderator variables of executive functioning in schizophrenia: meta-analytic findings. Schizophr Bull. 2001;27:305–316. doi: 10.1093/oxfordjournals.schbul.a006876. [DOI] [PubMed] [Google Scholar]
- 39.Knowles EE, David AS, Reichenberg A. Processing-speed deficits in schizophrenia: re-examining the evidence. Am J Psychiatry. 2010;167:828–835. doi: 10.1176/appi.ajp.2010.09070937. [DOI] [PubMed] [Google Scholar]
- 40.Cirillo MA, Seidman LJ. Verbal declarative memory dysfunction in schizophrenia: from clinical assessment to genetics and brain mechanisms. Neuropsychol Rev. 2003;13:43–77. doi: 10.1023/a:1023870821631. [DOI] [PubMed] [Google Scholar]
- 41.Otto T, Eichenbaum, H Toward a comprehensive account of hippocampal function: Studies of olfactory learning permit an integration of data across multiple levels of neurobiological analysis. In: Squire LR, Butters N, eds. Neuropsychology of Memory. New York, NY: Guilford Press 1992:415–428. [Google Scholar]
- 42.Aleman A, Hijman R, de Haan EH, Kahn RS. Memory impairment in schizophrenia: a meta-analysis. Am J Psychiatry. 1999;156:1358–1366. doi: 10.1176/ajp.156.9.1358. [DOI] [PubMed] [Google Scholar]
- 43.Goldberg TE, Saint-Cyr JA, Weinberger DR. Assessment of procedural learning and problem solving in schizophrenic patients by Tower of Hanoi type tasks. J Neuropsychiatry Clin Neurosci. 1990;2:165–173. doi: 10.1176/jnp.2.2.165. [DOI] [PubMed] [Google Scholar]
- 44.Scherer H, Stip E, Paquet F, Bedard MA. Mild procedural learning disturbances in neuroleptic-naive patients with schizophrenia. J Neuropsychiatry Clin Neurosci. 2003;15:58–63. doi: 10.1176/jnp.15.1.58. [DOI] [PubMed] [Google Scholar]
- 45.Altshuler LL, Ventura J, van Gorp WG, Green MF, Theberge DC, Mintz J. Neurocognitive function in clinically stable men with bipolar I disorder or schizophrenia and normal control subjects. Biol Psychiatry. 2004;56:560–569. doi: 10.1016/j.biopsych.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 46.Miller GA, Galanter E, Pribram KH. Plans and the Structure of Behavior. New York, NY: Holt, Rinehart &;Winston; 1960 [Google Scholar]
- 47.Baddeley AD, Hitch GJ. Working memory. In: Bower G, ed. Recent Advances in Learning and Motivation. New York, NY: Academic Press; 1974:47–90. [Google Scholar]
- 48.Goldman-Rakic PS. Working memory dysfunction in schizophrenia. J Neuropsychiatry Clin Neurosci. 1994;6:348–357. doi: 10.1176/jnp.6.4.348. [DOI] [PubMed] [Google Scholar]
- 49.Goldman-Rakic PS. Prefrontal cortical dysfunction in schizophrenia: The relevance of working memory. In: Carroll B, Barrett JE, eds. Psychopathology and the Brain. New York, NY: Raven Press 1991:1–23. [Google Scholar]
- 50.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York, NY: Oxford University Press 2004 [Google Scholar]
- 51.Lee J, Park S. Working memory impairments in schizophrenia: a metaanalysis. J Abnorm Psychol. 2005;114:599–611. doi: 10.1037/0021-843X.114.4.599. [DOI] [PubMed] [Google Scholar]
- 52.Zakzanis KK, Leach L, Kaplan E. Schizophrenia. In: Zakzanis KK, Leach L, Kaplan E, eds. Neuropsychological Differential Diagnosis. Amsterdam, the Netherlands: Swets and Zeitlinger 1999:139–152. [Google Scholar]
- 53.Zanelli J, Reichenberg A, Morgan K, et al. Specific and generalized neuropsychological deficits: a comparison of patients with various first-episode psychosis presentations. Am J Psychiatry. 2010;167:78–85. doi: 10.1176/appi.ajp.2009.09010118. [DOI] [PubMed] [Google Scholar]
- 54.Reichenberg A, Harvey PD, Bowie CR, et al. Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr Bull. 2009;35:1022–1029. doi: 10.1093/schbul/sbn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stefanopoulou E, Manoharan A, Landau S, Geddes JR, Goodwin G, Frangou S. Cognitive functioning in patients with affective disorders and schizophrenia: a meta-analysis. Int Rev Psychiatry. 2009;21:336–356. doi: 10.1080/09540260902962149. [DOI] [PubMed] [Google Scholar]
- 56.Bora E, Yucel M, Pantelis C. Neurocognitive markers of psychosis in bipolar disorder: a meta-analytic study. J Affect Disord. In press doi: 10.1016/j.jad.2010.02.117. [DOI] [PubMed] [Google Scholar]
- 57.Bora E, Yucel M, Pantelis C. Cognitive impairment in affective psychoses: a meta-analysis. Schizophr Bull. 2010;36:112–125. doi: 10.1093/schbul/sbp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl. 2007:17–26. doi: 10.1111/j.1600-0447.2007.01055.x. [DOI] [PubMed] [Google Scholar]
- 59.Bora E, Yucel M, Pantelis C. Cognitive impairment in schizophrenia and affective psychoses: implications for DSM-V criteria and beyond. Schizophr Bull. 2010;36:36–42. doi: 10.1093/schbul/sbp094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bora E, Yucel M, Pantelis C. Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord. 2009;113:1–20. doi: 10.1016/j.jad.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 61.Martinez-Aran A, Vieta E, Colom F, Torrent C, Sanchez-Moreno J, Reinares M, et al. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord. 2004;6:224–332. doi: 10.1111/j.1399-5618.2004.00111.x. [DOI] [PubMed] [Google Scholar]
- 62.Martinez-Aran A, Vieta E, Reinares M, Colom F, Torrent C, SanchezMoreno J, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 63.Robinson LJ, Ferrier IN. Evolution of cognitive impairment in bipolar disorder: a systematic review of cross-sectional evidence. Bipolar Disord. 2006;8:103–116. doi: 10.1111/j.1399-5618.2006.00277.x. [DOI] [PubMed] [Google Scholar]
- 64.Paelecke-Habermann Y, Pohl J, Leplow B. Attention and executive functions in remitted major depression patients. J Affect Disord. 2005;89:125–135. doi: 10.1016/j.jad.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 65.Woodberry KA, Giuliano AJ, Seidman LJ. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165:579–587. doi: 10.1176/appi.ajp.2008.07081242. [DOI] [PubMed] [Google Scholar]
- 66.Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, et al. Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am J Psychiatry. 2009;166:50–57. doi: 10.1176/appi.ajp.2008.08030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reichenberg A, Caspi A, Harrington H, et al. Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. Am J Psychiatry. 2010;167:160–169. doi: 10.1176/appi.ajp.2009.09040574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.MacCabe JH, Lambe MP, Cnattingius S, et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br J Psychiatry. 2010;196:109–115. doi: 10.1192/bjp.bp.108.060368. [DOI] [PubMed] [Google Scholar]
- 69.Tiihonen J, Haukka J, Henriksson M, et al. Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts. Am J Psychiatry. 2005;162:1904–1910. doi: 10.1176/appi.ajp.162.10.1904. [DOI] [PubMed] [Google Scholar]
- 70.Reichenberg A, Weiser M, Rabinowitz J, et al. A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder. Am J Psychiatry. 2002;159:2027–2035. doi: 10.1176/appi.ajp.159.12.2027. [DOI] [PubMed] [Google Scholar]
- 71.Zammit S, Allebeck P, David AS, D, et al. A longitudinal study of premorbid IQ Score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004;61:354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- 72.Saykin AJ, Gur RC, Gur RE, Mozley PD, Mozley LH, Resnick SM, et al. Neuropsychological function in schizophrenia. Selective impairment in memory and learning. Arch Gen Psychiatry. 1991;48:618–624. doi: 10.1001/archpsyc.1991.01810310036007. [DOI] [PubMed] [Google Scholar]
- 73.Palmer BW, Heaton RK, Paulsen JS, et al. Is it possible to be schizophrenic yet neuropsychologically normal? Neuropsychology. 1997;11:437–446. doi: 10.1037//0894-4105.11.3.437. [DOI] [PubMed] [Google Scholar]
- 74.Bryson GJ, Silverstein ML, Nathan A, Stephen L. Differential rate of neuropsychological dysfunction in psychiatric disorders: comparison between the Halstead-Reitan and Luria-Nebraska batteries. Percept Mot Skills. 1993;76:305–306. [PubMed] [Google Scholar]
- 75.Keefe RS, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57:688–691. doi: 10.1016/j.biopsych.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 76.Bromet EJ, Schwartz JE, Fennig S, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18:243–255. doi: 10.1093/schbul/18.2.243. [DOI] [PubMed] [Google Scholar]
- 77.Bromet EJ, Jandorf L, Fennig S, et al. The Suffolk County Mental Health Project: demographic, pre-morbid and clinical correlates of 6-month outcome. Psychol Med. 1996;26:953–962. doi: 10.1017/s0033291700035285. [DOI] [PubMed] [Google Scholar]
- 78.Blyler CR, Gold JM, Iannone VN, Buchanan RW. Short form of the WAISIII for use with patients with schizophrenia. Schizophr Res. 2000;46:209–215. doi: 10.1016/s0920-9964(00)00017-7. [DOI] [PubMed] [Google Scholar]
- 79.Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- 80.Kern RS, Nuechterlein KH, Green MF, et al. The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am J Psychiatry. 2008;165:214–220. doi: 10.1176/appi.ajp.2007.07010043. [DOI] [PubMed] [Google Scholar]
- 81.Keefe RS, Harvey PD, Goldberg TE, et al. Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS) Schizophr Res. 2008;102:108–115. doi: 10.1016/j.schres.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 82.Hobart MP, Goldberg R, Bartko JJ, Gold JM. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia, II: convergent/discriminant validity and diagnostic group comparisons. Am J Psychiatry. 1999;156:1951–1957. doi: 10.1176/ajp.156.12.1951. [DOI] [PubMed] [Google Scholar]
- 83.Gold JM, Queern C, Iannone VN, Buchanan RW. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia I: sensitivity, reliability, and validity. Am J Psychiatry. 1999;156:1944–1950. doi: 10.1176/ajp.156.12.1944. [DOI] [PubMed] [Google Scholar]
- 84.Pietrzak RH, Olver J, Norman T, Piskulic D, Maruff P, Snyder PJ. A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol. 2009;31:848–859. doi: 10.1080/13803390802592458. [DOI] [PubMed] [Google Scholar]
- 85.Bowie CR, Harvey PD. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin N Am. 2005;28:613–33, 26. doi: 10.1016/j.psc.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 86.Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- 87.Davidson M, Reichenberg A, Rabinowitz J, Weiser M, Kaplan Z, Mark M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry. 1999;156:1328–1335. doi: 10.1176/ajp.156.9.1328. [DOI] [PubMed] [Google Scholar]
- 88.Cornblatt B, Lencz T, Obuchowski M. The schizophrenia prodrome: treatment and high-risk perspectives. Schizophr Res. 2002;54:177–186. doi: 10.1016/s0920-9964(01)00365-6. [DOI] [PubMed] [Google Scholar]