Abstract
Spectral domain optical coherence tomography (SD-OCT) images from an infant victim of shaken baby syndrome who presented with vitreous hemorrhage in the left eye and bilateral, large hemorrhages over both maculae. Both RetCam and SD-OCT images were obtained, demonstrating the position of the blood beneath the internal limiting membrane of the right macula. Image registration software was used to register the photographic images with the surface projection images obtained by the SD-OCT. In the left eye, the vitreous hemorrhage was removed with vitrectomy, and the retinoschisis cavity incised to allow drainage.
INTRODUCTION
Reported by Caffey in 1972,1 retinal hemorrhages have been well described in the shaken baby syndrome (SBS). Hemorrhages have been reported in all retinal layers as well as in the pre-retinal and vitreous spaces.2–6 Prior reports have also described macular retinoschisis, with blood collecting between the separated retinal layers.3 In particular, dome shaped collections of blood, overlying the macula and lying under the internal limiting membrane (ILM) have been described in clinical reports and histopathology.3,7
Optical coherence tomography (OCT) enables non-invasive, cross-sectional imaging of the living retina. The use of a handheld scanner permits imaging of the anesthetized infant retina,8 and has recently been used to image infants with SBS.9,10 We present OCT images and fundus photographs depicting one of the first in-vivo demonstrations of a hemorrhagic retinoschisis cavity in a victim of SBS.
CASE DESCRIPTION
The patient was a 3½-month-old male infant who became apneic and unresponsive at home. On transport to the hospital, she developed seizures, was found to have intracranial hemorrhage, and was admitted to the ICU. Fundus examination demonstrated extensive, bilateral retinal hemorrhages in multiple layers, including large dome-shaped hemorrhages overlying both maculae. Subsequently, the left eye developed break-through vitreous hemorrhage. Two months later, once she was sufficiently stable, she underwent examination under anesthesia (EUA) and vitrectomy in the left eye.
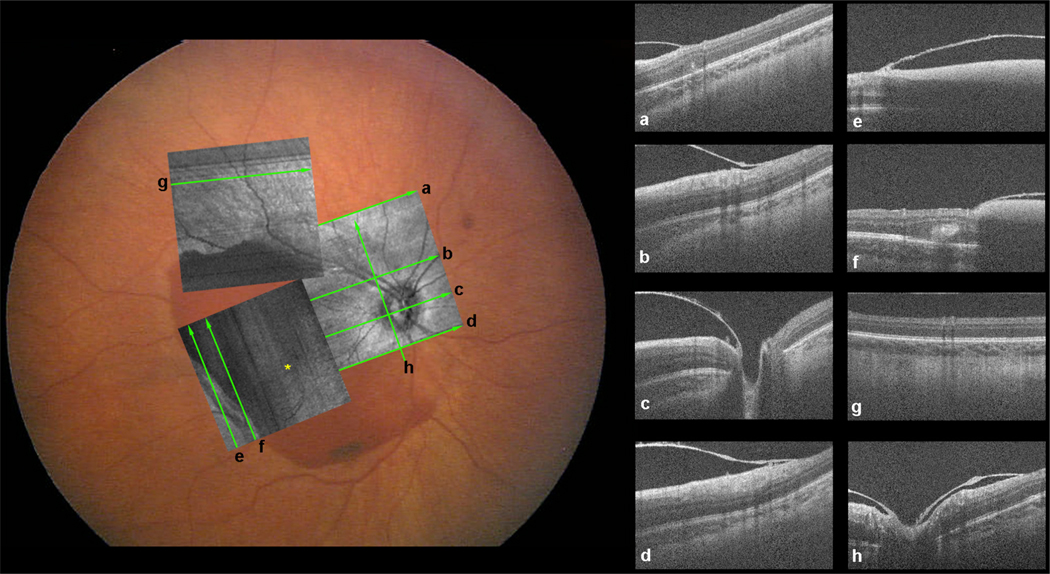
During the EUA, RetCam (Clarity Medical Systems, Inc., Pleasanton, CA) photographs were taken of the right eye. A handheld SD-OCT probe (Bioptigen Inc., Research Triangle Park, NC) was used to acquire images of the right eye as well. The handheld SD-OCT probe does not afford acquisition of a simultaneous fundus image, as is possible with a standard SD-OCT interface. However the “summed volume intensity projection,” which is a surface image created from the OCT volumetric data, can be used to precisely localize the retinal location of the OCT scans. This is done by registering the “summed volume intensity projection” to the fundus image obtained with the RetCam using the vasculature visible in both images. The results are in Figures 1 and 2. The SD-OCT images show the retinoschisis cavity overlying the macula with sub-ILM hemorrhage extending to the optic nerve. Features that were not visible in the RetCam image were seen in the corresponding OCT image, illustrating the complementary relationship between these imaging modalities.
Figure 1.
RetCam photo with spectral domain optical coherence tomography (SD OCT) fundus image overlaid on top after image registration. The lines show the locations of the SD OCT scans in the boxes to the right; each line and SD OCT image has a corresponding label. The OCT images show the retinoschisis cavity with sub-internal limiting membrance (ILM) hemorrhage extending to the optic nerve.
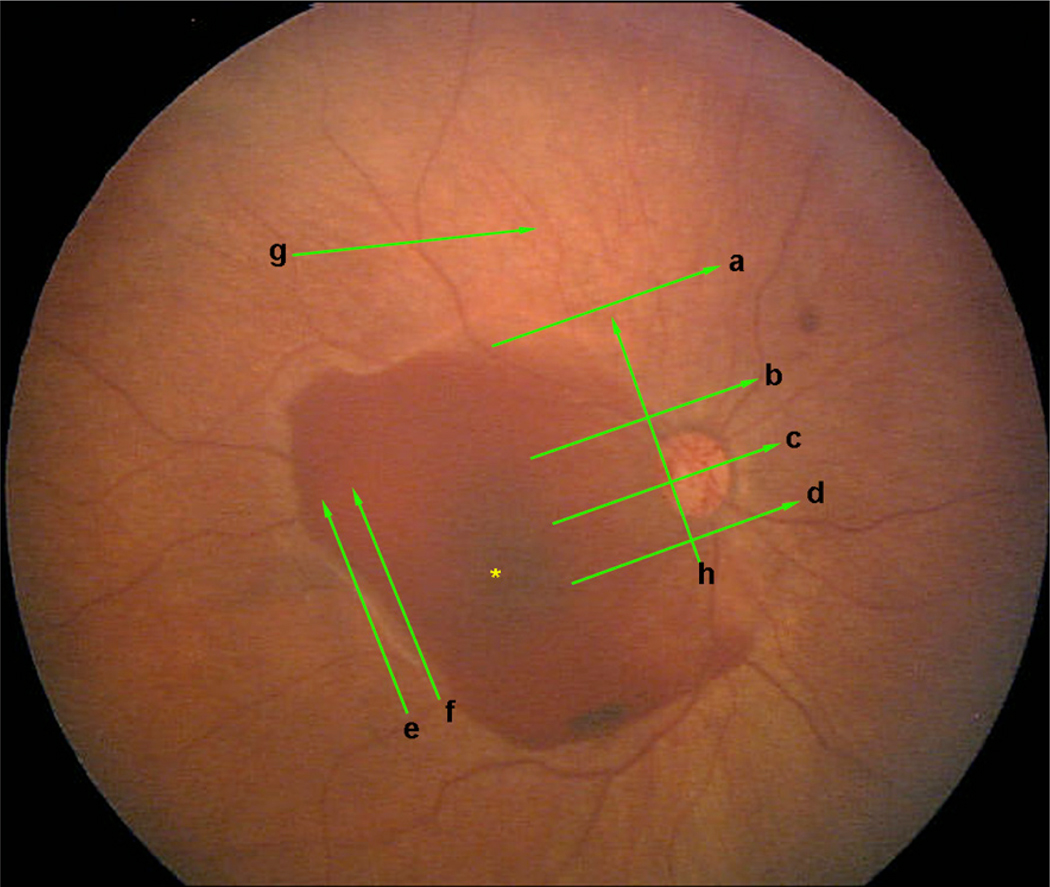
Figure 2.
RetCam photo without spectral domain optical coherence tomography (SD-OCT) fundus image overlay but with scan positions depicted.
Vitrectomy was performed on the left eye using a lens sparing technique and an irrigating light pipe. Once the vitreous hemorrhage was cleared, a large, dome shaped, sub-ILM hemorrhage was seen to overlie the macula, just as in the right eye. A small incision was made in the inferior aspect of the ILM, with the goal of allowing the hemorrhage to disperse and become absorbed. At the most recent follow-up, 3 weeks post-surgery, both eyes were seen to have improved substantially. The hemorrhages overlying both maculae had largely resorbed, and the remainder had layered inferior to the central macula.
DISCUSSION
In this paper, we have shown SD-OCT images of a large retinoschisis cavity with a sub-ILM hemorrhage resulting from SBS. These images were obtained using a handheld probe during an EUA. Previously, these large hemorrhagic cavities had only been reported with fundus photos and pathology slides. Bullous, sub-ILM hemorrhages resemble preretinal, sub-hyaloid hemorrhages on examination. The OCT scan in this case demonstrates the ILM overlying the hemorrhage. The sharp insertion into the optic nerve of the boundary overlying the hemorrhage is probably more consistent with ILM than with the posterior vitreous face. Conservative management in this case, with simple incision of the ILM during vitrectomy, allowed the blood to clear.
Retinoschisis cavities have often been reported in conjunction with retinal folds.2–7,10 No such folds were seen in this case. Recently, OCT images have been reported in cases of SBS. Sturm et al.9 used time domain OCT to image vitreoretinal traction and small, residual retinoschisis after the resolution of a hemorrhage. This vitreoretinal traction was speculated to contribute to the pathogenesis of retinal folds. Scott et al.10 used SD-OCT, also with a handheld probe, to image traumatic macular holes and epiretinal membranes after SBS. In this case, the epiretinal membrane was dual layered. The outer layer was postulated to be detached ILM, presumably after a prior hemorrhage had resorbed. However, images depicting the insertion of the membrane into intact retina were not presented.
The handheld OCT probe used here and in10 further improves the information that may be obtained during surgery and EUAs. Though Sturm et al.9 were able to position a patient with the typical slit lamp OCT interface, a handheld probe allows imaging the patient in a supine position and is more practical in an OR environment.
Registering the OCT images with the wide-field, color fundus photos of the RetCam facilitated the precise localization of the OCT scans. Cross-modality image registration was particularly helpful because the Bioptigen SD-OCT probe does not provide a true fundus image. Rather, it shows a narrow-field, “summed volume intensity projection”, which recreates a retinal surface image from the OCT volume data. Co-registration of images from different modalities and devices, whether in the normal or pathologic retina, provides a richer perspective of the relationship between the various images and assists in the process of interpreting specific features within a given image.
Acknowledgments
Supported by NIH EY001931, NIH EY014537, and NIH EY017607; Career Development Award, Research to Prevent Blindess, Inc., New York, New York (J. Caroll, PhD); The Gene and Ruth Posner Foundation, Milwaukee, Wisconsin; The E. Matilda Ziegler Foundation for the Blind, Darien, Connecticut; R.D. & Linda Peters Foundation, Brillion, Wisconsin; The Estate of James S. Panos; The Estate of Eunice C. Caron; and an unrestricted grant from Research to Prevent Blindness, Inc., New York, New York.
Footnotes
The authors have no financial or proprietary interest in the materials presented herein.
REFERENCES
- 1.Caffey J. On the theory and practice of shaking infants. Its potential residual effects of permanent brain damage and mental retardation. Am J Dis Child. 1972;124:161–169. doi: 10.1001/archpedi.1972.02110140011001. [DOI] [PubMed] [Google Scholar]
- 2.Kivlin JD. Manifestations of the shaken baby syndrome. Curr Opin Ophthalmol. 2001;12:158–163. doi: 10.1097/00055735-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Emerson MV, Jakobs E, Green WR. Ocular autopsy and histopathologic features of child abuse. Ophthalmology. 2007;114:1384–1394. doi: 10.1016/j.ophtha.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Marshall DH, Brownstein S, Dorey MW, Addison DJ, Carpenter B. The spectrum of postmortem ocular findings in victims of shaken baby syndrome. Canadian Journal of Ophthalmology-Journal Canadien D. Ophtalmologie. 2001;36:377–383. doi: 10.1016/s0008-4182(01)80081-8. [DOI] [PubMed] [Google Scholar]
- 5.Levin AV. Ophthalmology of shaken baby syndrome. Neurosurgery Clinics of North America. 2002;13:201–211. doi: 10.1016/s1042-3680(02)00004-9. [DOI] [PubMed] [Google Scholar]
- 6.Watts P, Obi E. Retinal folds and retinoschisis in accidental and non-accidental head injury. Eye. 2008;22:1514–1516. doi: 10.1038/eye.2008.224. [DOI] [PubMed] [Google Scholar]
- 7.Greenwald MJ, Weiss A, Oesterle CS, Friendly DS. Traumatic retinoschisis in battered babies. Ophthalmology. 1986;93:618–625. doi: 10.1016/s0161-6420(86)33688-1. [DOI] [PubMed] [Google Scholar]
- 8.Gerth C, Zawadzki RJ, Heon E, Werner JS. High-resolution retinal imaging in young children using a handheld scanner and Fourier-domain optical coherence tomography. J AAPOS. 2009;13:72–74. doi: 10.1016/j.jaapos.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sturm V, Landau K, Menke MN. Optical coherence tomography findings in Shaken Baby syndrome. Am J Ophthalmol. 2008;146:363–368. doi: 10.1016/j.ajo.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 10.Scott AW, Farsiu S, Enyedi LB, Wallace DK, Toth CA. Imaging the Infant Retina with a Hand-held Spectral-Domain Optical Coherence Tomography Device. Am J Ophthalmol. 2009;147:364–373. doi: 10.1016/j.ajo.2008.08.010. [DOI] [PubMed] [Google Scholar]