Abstract
Objective: To investigate patient's visual experience during vitreous surgery under local anesthesia. Methods: A prospective and randomized study of 76 patients that underwent vitreous surgeries in our hospital between July 2010 and December 2010 was designed. All patients were interviewed half an hour before and within 1 hour after the surgery using a standardized questionnaire. Basic characteristics of patients and their intraoperative visual experiences like light, color, moving object, pain, fear, and the desire for general anesthesia before and after the surgery were recorded. Results: Sixty patients (78.9%) perceived at least light perception, and 16 patients (21.1%) got no light perception throughout the entire duration of the operation. Forty one patients (53.9%) perceived only light, while 19 patients (25%) experienced moving objects. Thirty nine patients (51.3%) were frightened during their intraoperative visual experiences. Patients with better preoperative best-corrected visual acuity (BCVA) were more likely to be frightened (p=0.002). The frightened experience was affected notably by the different perceptions during operation, moving object (p=0.024), light (p=0.071), and color (p=0.071). Patients below 50 years old, especially from 20 to 30, were more likely to choose general anesthesia after the vitreous surgery. Conclusions: Most patients (78.9%) experienced at least light perception during the vitreous surgery under local anesthesia. There were no significant differences between the various visual experiences and their basic characteristics. Patients with better preoperative BCVA, perceived moving objects in their visual sensations seemed more likely to be frightened.
Keywords: Visual experience, regional anesthesia, vitreous surgery
Introduction
With the development of modern intraocular surgery, the number of patients undergoing a general anesthetic for vitreous surgery is declining. The safe and reliable orbital blocks made it an increasing percentage for local anesthesia surgeries. Therefore, it is of much importance to know what the patients had experienced during the entire duration of the surgery under local anesthesia. However, the visual experience under local anesthesia was not well recognized or understood until a few years ago. Most patients underwent vitreous surgery under local anesthesia experience a variety of intraoperative visual sensations [1, 2]. In a multicentre prospective study of 65 patients, 61.5% saw colors, 55.4% movements, and 50.8% instruments [3]. The cross-sectional study of Sugisaka et al showed that 73 patients (72.3%) saw colors, and 57 (56.4%) movements or moving objects [4].
Comprehension of the visual perceptions during the vitreous surgery under regional anesthesia is very important for the ophthalmologists. In a questionnaire survey of UK ophthalmologists, 58% thought that patients might be frightened by their intraoperative visual perceptions and 77% thought that preoperative counseling could help reduce this fear [5]. The well understanding of the intraoperative visual experiences could help ophthalmologists in the preoperative counseling to prevent fright and nervous associated syndrome in patients.
Our study compared the characteristics of patients who can see moving objects, light perception only and no light perception during the vitreous surgery under local anesthesia. We also analyzed the feature of patients who intended the surgery being done under general anesthesia after the surgery. We aimed to study the reason why patients were frightened during the surgery. To determine if the patients were frightened by the visual experiences or the fear was related to the basic characteristics of their own.
Methods
This prospective, randomized study was conducted in the Chinese People's Liberation Army (PLA) General Hospital. A total of 76 patients who underwent vitreous surgeries between July 2010 and December 2010 were studied. All patients were undergoing vitreous surgeries for the first time. Patients had preoperative visual acuity of no light perception in the operated eye, previous vitreous surgery, or lacked insight was excluded from the study. Medication or sedation was not used before the surgery. All patients were interviewed by trained interviewers half an hour before and within 1 hour after the surgery. A standardized questionnaire was used in all patients. All the questions related to visual experiences in the operated eyes were clearly explained. No patients approached refused to participate in our study.
The patients were asked to fulfill their personal data like age, gender, education background, preoperative sensation (frighten or not), and if they had aspiration for general anesthesia before surgery. Within 1 hour after the surgery, the patients were asked whether they had experienced light perception with the operated eye during the surgery. They were also asked if they had various visual experiences in the operation. These subjective perceptions included moving objects (instruments, surgeon's finger or hands, and surgeon or medical staff), and the color of light (yellow, white, red, green, blue, and uncertain light). Meanwhile, each patient was asked if they feel pain, and was frightened or not during the surgery. Whether regretted for not choose general anesthesia before surgery was the last question in the questionnaire.
Each patient provided written, informed consented to participate. The study protocol conformed to the tenets of the Declaration of Helsinki and it received ethical approval from the China Eye Research Institute Review Board.
All statistical analyses were carried out using SPSS 13.0 (SPSS, Inc., Chicago, IL) to calculate results. Chi-square tests and K independent samples were used to compare the results of various groups, and One-Way ANOVA used to compare means, with P values <0.05 considered statistically significant.
Results
Of the 76 patients (76 eyes) who participated in this study, 50 (65.79%) were men and 26 (34.21%) were women. The mean age of the patients was 41.5 years (range, 15 to 83 years, standard deviation SD±17.70). The demographic characteristics of the study population are detailed in Table 1.
Table 1.
Characteristics of patients undergoing vitreous surgery under regional anesthesia (n=76)
| Characteristics | Number of Patients | Percentage of Patients |
|---|---|---|
| Gender | ||
| Male | 50 | 65.79% |
| Female | 26 | 34.21% |
| Mean age (±SD) | ||
| All patients | 41.47±17.70 (range, 15-83) | |
| Male | 36.29±17.24 (range, 15-83) | |
| Female | 52.04±13.65 (range, 26-76) | |
| Eye operated | ||
| Right | 35 | 46.05% |
| Left | 41 | 53.95% |
| Education background (university or not) | ||
| Yes | 24 | 31.58% |
| Not | 52 | 68.42% |
| Preoperative best-corrected visual acuity (BCVA) | ||
| 20/20-20/40 | 14 | 18.42% |
| 20/50-20/150 | 17 | 22.37% |
| 20/200 & worse | 45 | 59.21% |
| Reason for surgery | ||
| Vitreous hemorrhage | 22 | 28.95% |
| Retinal detachment | 45 | 59.21% |
| Macular epiretinal membrane or macular hole | 9 | 11.84% |
| Preoperative sensation (nervous or not) | ||
| Yes | 57 | 75% |
| Not | 19 | 25% |
| Desire for general anesthesia before surgery | ||
| Yes | 20 | 26.32% |
| Not | 56 | 73.68% |
BCVA= best-corrected visual acuity; SD= standard deviation
Sixty patients (78.9%) perceived at least light perception throughout the entire surgery, 16 patients (21.1%) got no light perception throughout the entire duration of the operation. Forty one patients (53.9%) perceived only light during the surgery. The patients also described experiences of a variety of other visual sensations like moving objects (19 patients, 25%), which including instruments (8 patients, 10.5%), the surgeon's fingers or hands (9 patients, 11.8%), and the surgeon or medical staff (2 patients, 2.6%).
All the sixty patients (78.9%) experienced more than light sensations reported that they had the perception of colors. Some patients could even see different colors during the surgery. The various colors reported were yellow (24 patients, 31.6%), white (32 patients, 42.1%), red (5 patients, 6.6%), green (5 patients, 6.6%), blue (5 patients, 6.6%), and nonspecific, uncertain colors (2 patient, 2.6%).
Fifty seven patients (75%) felt nervous or afraid before the vitreous surgery. The number declined into 39 (51.3%) after the process of the operation. Twenty patients (26.32%) had a desire for general anesthesia when the questionnaire was filled before the operation, wherever this became 8 (10.5%) after the surgery.
We found that the characteristics of patients had no significant association between the different visual sensations (moving object, light perception only, and no light perception) during the vitreous surgery under regional anesthesia. There were no conspicuous differences between various perception and the age, gender, eye operated on, education background, etiological factor (vitreous hemorrhage, retinal detachment, or macular disease), or preoperative felling (nervous or afraid). The relationship between preoperative best corrected visual acuity (BCVA) (20/200 and better or with finger counting and worse) and the proportion of patients who experienced the different visual sensations among patients also of no statistically difference (p=0.570) (Table 2).
Table 2.
Comparison of possible factors of patients who can see moving object, light perception only or no light perception during vitreous surgery under regional anesthesia
| Characteristics | Moving Object(%) (n=19) | Light Perception Only(%)(n=41) | No light Perception (%)(n=16) | P value |
|---|---|---|---|---|
| Gender | 0.896 | |||
| Male | 13(68.4%) | 26(63.4%) | 11(68.8%) | |
| Female | 6(31.6%) | 15(36.6%) | 5(31.2%) | |
| Mean age (±SD) | ||||
| All patients | 45.21±16.23 | 40.78±17.29 | 38.81±20.63 | 0.536 |
| Male | 43.15±16.48 | 35.22±17.49 | 30.82±16.36 | 0.197 |
| Female | 49.67±16.19 | 51.5±10.97 | 56.4±19.11 | 0.717 |
| Eye operated | 0.873 | |||
| Right | 8(42.1%) | 20(48.8%) | 7(43.8%) | |
| Left | 11(57.9%) | 21(51.2%) | 9(56.3%) | |
| Education background (university or not) | 0.335 | |||
| Yes | 8(42.1%) | 10(24.4%) | 6(37.5%) | |
| Not | 11(57.9%) | 31(75.6%) | 10(62.5%) | |
| Preoperative best-corrected visual acuity (BCVA) | 0.570 | |||
| 20/20-20/40 | 4(21.1%) | 7(17.1%) | 3(18.8%) | |
| 20/50-20/150 | 6(31.6%) | 8(19.5%) | 3(18.8%) | |
| 20/200 & worse | 9(47.4%) | 26(63.4%) | 10(62.5%) | |
| Reason for surgery | 0.538 | |||
| Vitreous hemorrhage | 6(31.6%) | 10(24.4%) | 6(37.5%) | |
| Retinal detachment | 12(63.2%) | 25(61.0%) | 8(50.0%) | |
| Macular hole or macular epiretinal membrane | 1(5.3%) | 6(14.6%) | 2(12.5%) | |
| Preoperative sensation (nervous or not) | 0.782 | |||
| Yes | 15(78.9%) | 31(75.6%) | 11(68.8%) | |
| Not | 4(21.1%) | 10(24.4%) | 5(31.2%) | |
| Desire for general anesthesia before surgery | 0.476 | |||
| Yes | 7(36.8%) | 9(22.0%) | 4(25.0%) | |
| Not | 12(63.2%) | 32(78.0%) | 12(75.0%) |
BCVA= best-corrected visual acuity; SD= standard deviation
There were no significant statistical differences between a pain experience and the patients who only perceived light and no light perception. The fear experience and the desire for general anesthesia after vitreous operation were also of no obvious relationship in the two groups (Table 3).
Table 3.
Comparison of intraoperative visual experiences of patients who had light perception only and no light perception during vitreous surgery under regional anesthesia
| Characteristics | Light Perception Only (%)(n=41) | No Light Perception(%) (n=16) | P value |
|---|---|---|---|
| Pain | 0.269 | ||
| Yes | 27 (65.9%) | 8 (50%) | |
| Not | 14 (34.1%) | 8 (50%) | |
| Fear | 0.231 | ||
| Yes | 20 (48.8%) | 5 (31.3%) | |
| Not | 21 (51.2%) | 11 (68.7%) | |
| Desire for general anesthesia after surgery | 0.534 | ||
| Yes | 3 (7.3%) | 2 (12.5%) | |
| Not | 38(92.7%) | 14(87.5%) |
The patients who perceived moving objects or light perception only had experienced different colors during the whole operation. Yellow (24/76, 31.6%) and white (32/76, 42.1%) were the most two colors perceived in both of the two groups. There was no significant relationship between pain and fear in the two groups. A higher proportion of patients who perceived moving objects (12 patients, 63.2%) were frightened compared with those who could only experienced light sensation (20 patients, 48.8%) although this difference was not statistically significant (P=0.073) (Table 4).
Table 4.
Comparison of intraoperative visual experiences of patients who perceived moving object and light perception only during vitreous surgery under regional anesthesia
| Characteristics | Moving object (%) (n=19) | Light Perception (%)Only(n=41) | P value |
|---|---|---|---|
| Color of Light* | 0.393 | ||
| Yellow | 10(52.6%) | 14(34.1%) | |
| White | 9(47.4%) | 23(56.1%) | |
| Red | 3(15.8%) | 2(4.9%) | |
| Green | 1(5.3%) | 4(9.8%) | |
| Blue | 1(5.3%) | 2(4.9%) | |
| Uncertain | 0 | 2(4.9%) | |
| Pain | 0.839 | ||
| Yes | 12(63.2%) | 27(65.9%) | |
| Not | 7(36.8%) | 14(34.1%) | |
| Fear | 0.070 | ||
| Yes | 14 (63.2%) | 20(48.8%) | |
| Not | 5 (36.8%) | 21(51.2%) | |
| Desire for general anesthesia after surgery | 0.309 | ||
| Yes | 3(15.8%) | 3(7.3%) | |
| Not | 16(84.2%) | 38(92.7%) |
Some patients perceived more than 1 kind of colors.
Patients with better preoperative BCVA were more likely to be frightened (p=0.002). Besides, patients who were frightened by their visual experiences were more likely to see moving objects (14 patients, 35.9%) than those who were not frightened (5 patients, 13.5%). There was no significant association between a frightening visual experience and the patient's gender, eye operated on, education background, light and color perception, or the pain perceived during the surgery (Table 5).
Table 5.
Comparison of intraoperative visual experiences of patients who felt frightened against those who were not frightened
| Characteristics | Patients who felt frightened (%) (n=39) | Patients who were not frightened (%) (n=37) | P value |
|---|---|---|---|
| Gender | 0.750 | ||
| Male | 25(64.1%) | 25(67.6%) | |
| Female | 14(35.9%) | 12(32.4%) | |
| Age | 0.253 | ||
| Below 50 years | 29(74.4%) | 23(62.2%) | |
| Above 50 years | 10(25.6%) | 14(37.8%) | |
| Eye operated | 0.985 | ||
| Right | 18(46.2%) | 17(45.9%) | |
| Left | 21(53.8%) | 20(54.1%) | |
| Education background (university or not) | 0.876 | ||
| Yes | 12(30.8%) | 12(32.4%) | |
| Not | 27(69.2%) | 25(67.6%) | |
| Preoperative best-corrected visual acuity (BCVA) | 0.002* | ||
| 20/20-20/40 | 13(33.3%) | 1(2.7%) | |
| 20/50-20/150 | 6(15.4%) | 11(29.7%) | |
| 20/200 & worse | 20(51.3%) | 25(67.6) | |
| Moving object | 0.024* | ||
| Present | 14(35.9%) | 5(13.5%) | |
| Absent | 25(64.1%) | 32(86.5%) | |
| Light perception | 0.071 | ||
| Present | 34(87.2%) | 26(70.3%) | |
| Absent | 5(12.8%) | 11(29.7%) | |
| Colors | 0.071 | ||
| Present | 34(87.2%) | 26(70.3%) | |
| Absent | 5(12.8%) | 11(29.7%) | |
| Pain | 0.955 | ||
| Present | 24(61.5%) | 23(62.2%) | |
| Absent | 15(38.5%) | 14(37.8%) |
BCVA= best-corrected visual acuity
P<0.05
Twenty patients (26.3%) had a desire for general anesthesia before the operation to avoid experiencing the intraoperative visual experiences, even after they were informed the complications might associate with general anesthesia. Eight patients (10.5%) indicated that they would have preferred general anesthesia after the surgery. Seven of 8 (87.5%) were men and 1 (12.5%) was women. The mean age of them was 34.13 (range, 19 to 73 years, standard deviation SD±18.60). Seven patients (87.5%) felt pain during the operation. Three patients (37.5%) chose regional anesthesia before operation (Table 6).
Table 6.
Characteristics of patients who want general anesthesia after vitreous surgery under regional anesthesia (n=7)
| Characteristics | Number of Patients | Percentage of Patients |
|---|---|---|
| Gender | ||
| Male | 7 | 87.5% |
| Female | 1 | 12.5% |
| Eye operated | ||
| Right | 4 | 50% |
| Left | 4 | 50% |
| Education background (university or not) | ||
| Yes | 5 | 62.5% |
| Not | 3 | 37.5% |
| Preoperative best-corrected visual acuity (BCVA) | ||
| 20/20-20/40 | 3 | 37.5% |
| 20/50-20/150 | 1 | 12.5% |
| 20/200 & worse | 4 | 50% |
| Reason for surgery | ||
| Vitreous hemorrhage | 3 | 37.5% |
| Retinal detachment | 1 | 12.5% |
| Macular epiretinal membrane or macular hole | 4 | 50% |
| Preoperative sensation (nervous or not) | ||
| Yes | 6 | 75% |
| Not | 2 | 25% |
| Intraoperative visual experience | ||
| Moving object | 1 | 12.5% |
| Light perception only | 5 | 62.5% |
| No light perception | 2 | 25% |
| Color of Light | ||
| Yes | 6 | 75% |
| Not | 2 | 25% |
| Pain | ||
| Yes | 7 | 87.5% |
| Not | 1 | 12.5% |
| Fear | ||
| Yes | 3 | 37.5% |
| Not | 5 | 62.5% |
Discussion
Since more and more ophthalmic surgery is undergoing local anaesthesia, it has brought about an increasing awareness of the patient's subjective visual experiences during the operation. As cataract surgery is the most common and routine type of the intraocular surgery performed under local anesthesia, it has been widely reported previously [6-10]. In addition to seeing bright light, patients have reported seeing various other visual perceptions. Although the surgical procedures differ considerably between cataract surgery and vitreous operation, our study demonstrates that most patients (60, 78.9%) retain at least light perception during the entire surgery. Sixteen (21.1%) of the patients reported a total loss of light perception, indicating that neural conduction along the optic nerve was completely blocked. This compared favorably with previous reports [3, 4, 9, 11, 12]. However, the proportion is higher than cataract surgery which ranged from 0% to 20% [13, 14]. The possible reason might be summarized as the volume of anesthetic agent, preexisting ocular pathology, the surgical procedure, the duration of the surgery, the mental status before operation, and so on.
We previously thought that the basic characteristics such as gender, age, the eye being operated on, education background, preoperative BCVA, or etiological factor might play a role in the visual experiences during the vitreous operation. However, our study showed no statistically difference when we compared the characteristics of the 3 groups of patients who had perceived moving objects, light sensation only, and no light perception (Table 2). Comparison of intraoperative visual experience of the 3 groups of patients is also of no significant difference (Table 3, 4). That might means whatever patients perceived during the operation, moving objects, light only, or no light perception, the visual experience is identical in statistic. Gender, age, the eye being operated on, education background, preoperative BCVA, and etiological factor are not the primary key open the journey of their visual experience during vitreous surgery under local anesthesia.
Perception of fear is of the most interest during the entire surgery in majority previous reports. A frightening visual experience is clinically significant because it may lead to a sympathetic surge resulting in unwanted systemic side effects like tachycardia, hypertension, hyperventilation, and acute panic attacks [15]. The satisfaction of the operation could also be declined because of the frightened visual experience. It could make more patients choose general anesthesia next time if possible, and recommend to their friends. Thirty nine patients (51.3%) were frightened during their intraoperative visual experiences in our study. This proportion is much higher than patients undergoing cataract surgery and other vitreous operation [1, 3, 8, 10, 11, 12, 16, 17]. The possible reason might be the difference of education background. Fifty two patients (68.42%) in our study had never gone to college, and almost half of them came from rural area in China mainland. The use of preoperative counseling is of much importance to prevent fright associated with visual experiences. Less understanding of preoperative counseling could significantly increase the fear sensation during the surgery after controlling for age, gender, and whether it was first or second eye operation [18].
Our study showed preoperative BCVA play an important role in patients who were frightened during their visual experience. Patients with better preoperative BCVA were more likely to be frightened (p=0.002). Meanwhile, the frightened experience was affected notably by the different perceptions during operation, moving object (p=0.024), light (p=0.071), and color (p=0.071) (Table 5). It is possibly because that the more and clear patients perceived the more inconceivability would happen. That might make them frightened. However, the data seemed conversely with the frighten experience in Table 3 and Table 4. Although there was no statistical significance when we compared the 3 groups of visual experiences, more patients frightened in moving objects group (63.2%) and light perception only group (48.8%) than no light perception group (31.3%).
The multicenter study of Tan and associates showed that younger patients were statistically more likely to be frightened [3]. Some studies on patients undergoing cataract surgery also have reported similar findings in spite of the differences were not statistically significant [1, 8, 16, 17]. In spite of no statistical difference in age in our study (p=0.253), we found patients below 50 years (29 patients, 38.2%) seemed more likely to be frightened compared with those aged 50 or older.
Fifty seven patients (75%) felt nervous or afraid, and 20 (26.32%) had a desire for general anesthesia when the questionnaire was filled before the operation. Eight patients (10.5%) insisted on general anesthesia after the surgery, even after being counseled on the higher risks associated with this form of anesthesia. This proportion is similar to the 7.7% in the multicenter study and a research about the cataract surgery [1, 3, 8]. Furthermore, we found patients below 50 years old, especially from 20 to 30, were more likely to choose general anesthesia after the vitreous surgery (Figure 1). Male patients (87.5%) and intraoperative pain perception (87.5%) might likewise contribute to the decision of general anesthesia (Table 6).
Figure 1.
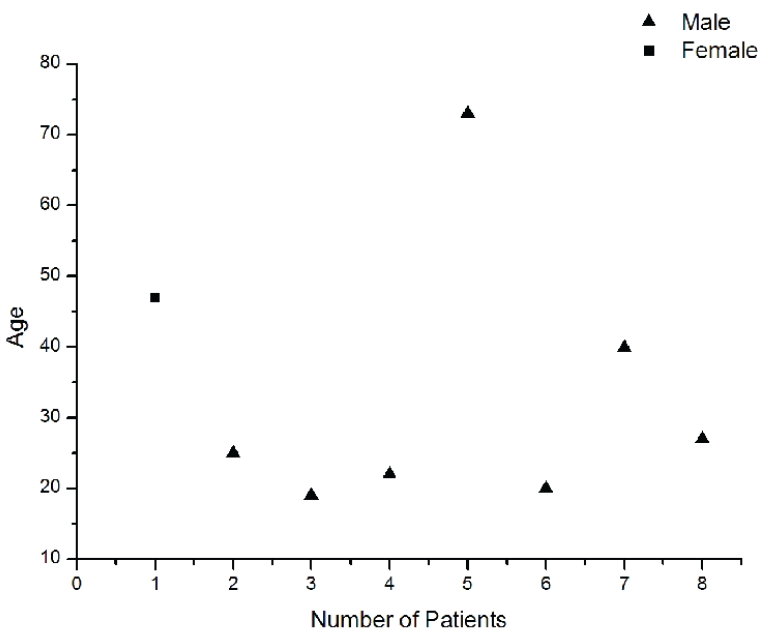
Characteristics of age distribution of patients who would like to choose general anesthesia after the vitreous surgery. Patients below 50 years old, especially from 20 to 30, were more likely to choose general anesthesia after the vitreous surgery.
Subjective visual experiences during intraocular ophthalmic surgery like cataract, glaucoma, or vitreous surgery under regional anesthesia are now been well recognized. However, mechanisms of these visual perceptions are less understood. It might be a combination of images of objects close to but outside the eye, such as fingers and instruments, and entoptic phenomena produced by objects and structures on the corneal surface and in the eye [19]. The most likely explanation for visual perception is a combination of optical and entoptic phenomena [20]. Further researches need to focus on the genesis of visual experience and the different stage of visual sensation during the vitreous operation.
Our study demonstrated that most patients (78.9%) experienced at least light perception during the vitreous surgery under local anesthesia. There were no significant differences between the various visual experiences (moving object, light perception only, and no light perception) and their basic characteristics. About half of the patients perceived intraoperative frightened experience, which was much higher than previous reports. Patients with better pre-operative BCVA, perceived moving objects in their visual sensations seemed more likely to be frightened. Additionally, we found patients below 50 years old, especially from 20 to 30 were more willing to choose general anesthesia after the vitreous surgery.
Acknowledgments
None. No authors have any financial/conflicting interests to disclose.
References
- 1.Au Eong KG, Low CH, Heng WJ, et al. Subjective visual experience during phacoemulsification and intraocular lens implantation under topical anesthesia. Ophthalmology. 2000;107:248–50. doi: 10.1016/s0161-6420(99)00080-9. [DOI] [PubMed] [Google Scholar]
- 2.Prasad N, Kumar CM, Patil BB, Dowd TC. Subjective visual experience during phacoemulsification cataract surgery under sub-Tenon's block. Eye (Lond) 2003;17:407–9. doi: 10.1038/sj.eye.6700370. [DOI] [PubMed] [Google Scholar]
- 3.Tan CS, Mahmood U, O'Brien PD, et al. Visual experiences during vitreous surgery under regional anesthesia: a multicenter study. Am J Ophthalmol. 2005;140:971–5. doi: 10.1016/j.ajo.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 4.Sugisaka E, Shinoda K, Ishida S, et al. Patients' descriptions of visual sensations during pars plana vitrectomy under retrobulbar anesthesia. Am J Ophthalmol. 2007;144:245–51. doi: 10.1016/j.ajo.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Laude A, Eong Au, Mills KB. Knowledge of visual experience during cataract surgery under local anaesthesia: a nationwide survey of UK ophthalmologists. Br J Ophthalmol. 2009;93:510–2. doi: 10.1136/bjo.2006.097030. [DOI] [PubMed] [Google Scholar]
- 6.Murdoch IE, Sze P. Visual experience during cataract surgery. Eye (Lond) 1994;8:666–7. doi: 10.1038/eye.1994.164. [DOI] [PubMed] [Google Scholar]
- 7.Newman DK. Visual experience during phacoemul-sification cataract surgery under topical anaesthesia. Br J Ophthalmol. 2000;84:13–5. doi: 10.1136/bjo.84.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaylali V, Yildirim C, Tatlipinar S, Demirlenk I, Arik S, Ozden S. Subjective visual experience and pain level during phacoemulsification and intraocular lens implantation under topical anesthesia. Ophthalmologica. 2003;217:413–6. doi: 10.1159/000073071. [DOI] [PubMed] [Google Scholar]
- 9.Chung CF, Lai JS, Lam DS. Visual sensation during phacoemulsification and intraocular lens implantation using topical and regional anesthesia. J Cataract Refract Surg. 2004;30:444–8. doi: 10.1016/S0886-3350(03)00612-6. [DOI] [PubMed] [Google Scholar]
- 10.Ang CL, Au Eong KG, Lee SS, Chan SP, Tan CS. Patients' expectation and experience of visual sensations during phacoemulsification under topical anaesthesia. Eye(Lond) 2007;21:1162–7. doi: 10.1038/sj.eye.6702427. [DOI] [PubMed] [Google Scholar]
- 11.Rengaraj V, Radhakrishnan M, Au Eong KG, et al. Visual experience during phacoemulsification under topical versus retrobulbar anesthesia: results of a prospective, randomized, controlled trial. Am J Ophthalmol. 2004;138:782–7. doi: 10.1016/j.ajo.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 12.Tan CS, Au Eong KG, Kumar CM. Visual experiences during cataract surgery: what anesthesia providers should know. Eur J Anaesthesiol. 2005;22:413–9. doi: 10.1017/s0265021505000700. [DOI] [PubMed] [Google Scholar]
- 13.Brent BD, Singh H. The effect of retrobulbar anesthesia on visual acuity in planned extra-capsular cataract extraction. Ophthalmic Surg. 1991;22:392–5. [PubMed] [Google Scholar]
- 14.Schimek F, Steuhl KP, Fahle M. Retrobulbar blockade of somatic, motor, and visual nerves by local anesthetics. Ophthalmic Surg. 1993;24:171–80. [PubMed] [Google Scholar]
- 15.Tan CS, Rengaraj V, Au Eong KG. Visual experiences of cataract surgery. J Cataract Refract Surg. 2003;29:1453–4. doi: 10.1016/s0886-3350(03)00480-2. [DOI] [PubMed] [Google Scholar]
- 16.Au Eong KG, Lim TH, Lee HM, Yong VS. Subjective visual experience during phacoemulsification and intraocular lens implantation using retrobulbar anesthesia. J Cataract Refract Surg. 2000;26:842–6. doi: 10.1016/s0886-3350(99)00452-6. [DOI] [PubMed] [Google Scholar]
- 17.Tranos PG, Wickremasinghe SS, Sinclair N, et al. Visual perception during phacoemulsification cataract surgery under topical and regional anaesthesia. Acta Ophthalmol Scand. 2003;81:118–22. doi: 10.1034/j.1600-0420.2003.00029.x. [DOI] [PubMed] [Google Scholar]
- 18.Voon LW, Au Eong KG, Saw S-M, Verma D, Laude A. Effect of preoperative counseling on patient fear from the visual experience during phacoemulsification under topical anesthesia: multicentre randomized clinical trial. J Cataract Refract Surg. 2005;31:1966–9. doi: 10.1016/j.jcrs.2005.03.059. [DOI] [PubMed] [Google Scholar]
- 19.Sumich PM, Francis IC, Kappagoda MB, Alexander SL. Retained visual sensation during cataract surgery. Ophthalmology. 2001;108:1003. doi: 10.1016/s0161-6420(00)00423-1. [DOI] [PubMed] [Google Scholar]
- 20.Yavuz GA, Unver YB, Sinclair SH. Entoptic phenomenon following pars plana vitrectomy caused by retained preretinal gel. Ophthalmic Surg Lasers Imaging. 2009;40:188–91. doi: 10.3928/15428877-20090301-01. [DOI] [PubMed] [Google Scholar]


