Abstract
INTRODUCTION
We observed that a number of patients presenting to our clinic with diverticular fistulation were taking nicorandil for angna. Recognised side effects of nicorandil include gastrointestinal and genital ulceration. The aim of our study was to determine whether nicorandil is an aetiological agent in diverticular fistulation.
PATIENTS AND METHODS
We conducted a case-control study of patients with diverticular disease related enteric fistulae. Two patient groups were identified: a study group of patients with diverticular fistulae, and a control group with uncomplicated diverticular disease. The proportion of patients who had ever used nicorandil was compared between the two groups.
RESULTS
A total of 153 case notes were analysed, 69 patients with fistulae and 84 control patients with uncomplicated diverticular disease. Female to male ratio in both groups was 2:1. The mean age was 71 years in the fistula group and 69 years in the control diverticular disease group (P = ns). Of those with colonic fistulae, 16% were taking nicorandil compared with 2% of the control group (odds ratio 7.8; 95% confidence interval 1.5–39.1; P = 0.008). There was no significant difference in rates of ischaemic heart disease between fistula and control groups.
CONCLUSIONS
Nicorandil is associated with fistula formation in diverticular disease.
Keywords: Diverticular disease, Fistulation, Nicorandil, Colovaginal, Colovesical
Nicorandil (Ikorel, Sanofi Aventis) is used as a second-line treatment for angina. It is the only licensed drug in its class of nicotinamide esters and was launched in the UK in 1994. It has a novel dual action as both potassium channel activator and vasodilator via nitric oxide (NO) donation.1 It acts as both an arteriolar vasodilator and venodilator, thereby reducing both afterload and preload.
Over the last 10 years, there have been several reports of an association between nicorandil and ulceration of the gastrointestinal tract.2–4 Oral and anal ulceration have been most frequently reported, though colorectal,2 ileal, peristomal5 and genital ulceration6,7 have also been described. Ulceration has been reported at various times following starting treatment with the drug ranging from weeks to years. The ulcers generally heal rapidly following cessation of nicorandil.
After noticing that a high proportion of patients in our clinic with diverticular fistulation were taking nicorandil, we decided to investigate further. We designed a case control study to establish whether a link exists between nicorandil and diverticular fistulation. Given the reported link between the drug and colonic ulceration,2 we hypothesised that the inflammation and epithelial destruction associated with colonic ulceration might be enough to cause a fistula in pre-existing diverticular disease. If nicorandil-associated ulceration were to affect a portion of the sigmoid colon already diseased with diverticulosis, it might induce fistulation into adjacent bladder or other organs.
Patients and Methods
Patient notes were reviewed in a case-control study of patients with diverticular enteric fistulation. Two patient groups were identified – a study group of patients with diverticular colonic fistulae and a control group with uncomplicated diverticular disease. The time frame used for patient selection was January 2000 to July 2009, beginning 6 years after the UK launch of nicorandil in 1994 to allow time for usage levels to stabilise and possible complications to appear. The ICD-10 codes N32.1 – vesico-intestinal Fistula, N82.3 – fistula of vagina to large intestine, and N82.4 – other female intestinal-genital tract fistulae were used to identify patients with fistulation. Notes were reviewed, selecting only those cases where fistulation was due to diverticular disease. Cases of fistulation due to other pathology (e.g. Crohn's disease or cancer) were excluded. The diagnosis was based on histopathology whenever possible, and on radiological and endoscopic appearances when disease was managed non-surgically.
The control group consisted of patients with a clinical coding of diverticular disease from the same time period. These were patients with endoscopically confirmed diverticulosis who had presented with various gastrointestinal symptoms, principally abdominal pain, per rectal bleeding and diarrhoea. Although all control patients had uncomplicated diverticular disease at baseline enrolment, some went on to develop complications of diverticulosis over the 9-year duration of the study.
Case notes were studied to establish whether the patients in both groups had ever taken nicorandil by examination of all medical notes, discharge summaries, clinic letters and drug administration charts. We also recorded co-morbidities, demographics, aetiology, anatomy of fistula and operative management. Power calculations based on an assumption that 15% of fistula patients might be taking nicorandil and 5% of controls, showed a minimum of 49 patients were needed per group to demonstrate a significant effect. Differences between case and control groups were assessed by odds ratios and two tailed Fisher's exact test using the Statview statistical package (Abacus Concepts, Berkley, CA, USA).
Results
We retrieved a total of 153 case notes, 69 patients with fistulae, and 84 patients with uncomplicated diverticular disease. In the fistula group, 25 were excluded because of non-diverticular disease aetiology, including 14 with colorectal cancer and three with Crohn's disease as the primary cause of fistulation. This left a study group of 44 with diverticular fistulae. In the fistula group, there were 28 females and 16 males, compared with 54 females and 30 males in the control group (P = ns). The mean age was 71 years in the fistula group (range, 34–92 years) and 69 years in the control diverticular disease group (range, 44–89 years; P = ns).
Of the control group (84 patients), seven had Hartmann's procedure for perforation and two had resection with anastomosis for diverticular stricture (1 sigmoid colectomy, 1 anterior resection). One patient had successful radiological drainage of a diverticular abscess without surgical intervention.
In the fistula group, 31 patients had fistulae between the sigmoid colon and bladder, nine between sigmoid and vagina, and four involved upper rectum and vagina (Fig. 1). Management of the fistula group comprised 21 patients having sigmoid colectomy, nine having anterior resections, six having Hartmann's resections, six being managed conservatively, one had a defunctioning colostomy and one a defunctioning ileostomy (Fig. 2).
Figure 1.
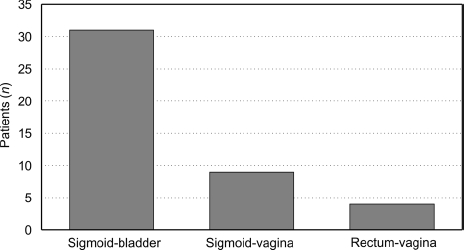
Anatomy of diverticular fistulas – site of communication.
Figure 2.

Management of diverticular fistulas – operative or conservative.
Of those with diverticular fistulas, 16% (7 of 44) were taking nicorandil compared with only 2% (2 of 84) of the control diverticular disease group (Fig. 3; odds ratio 7.8; 95% confidence interval 1.5–39.1; P = 0.008). It was not always possible to establish duration of nicorandil therapy prior to fistulation, but where this was stated in the notes it ranged from 17–108 months.
Figure 3.
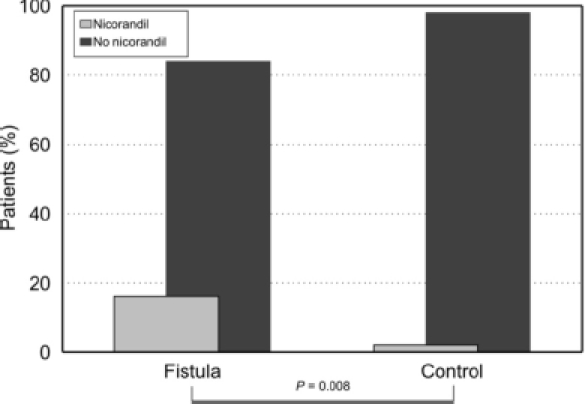
Frequency of nicorandil usage amongst fistula and control patients.
Rates of ischaemic heart disease (IHD) were compared between the two groups. Mentions of the terms IHD, myocardial infarction, angina and atrial fibrillation were recorded for the case notes in both groups. There was no significant difference in IHD rates between the two groups. In the fistula group, 18 of 44 patients had a record of IHD, compared with 21 of 85 in the diverticular disease group (P = ns).
Discussion
An association between colorectal ulceration and nicorandil use has already been described in the literature.2 We speculated that nicorandil-induced ulceration on the background of diverticulosis might cause fistulation between the colon and adjacent viscera. To test this hypothesis, we conducted a case-control study to establish whether such an association may exist.
On comparing case notes of patients with fistulating diverticular disease and patients with uncomplicated diverticular disease, we observed an association between nicorandil and fistulation. A significantly higher proportion of patients with fistulas were taking nicorandil than control patients with diverticulosis alone.
It is possible that higher rates of nicorandil use in the fistula group were simply a surrogate marker for higher rates of underlying IHD. It might be that more IHD in the fistula group means more ischaemic colitis which could predispose to fistulation, instead of a direct effect of nicorandil. There was, in fact, no significant difference in rates of IHD between the two groups. This reinforces the case for a causal relationship between nicorandil and fistulation rather than a link via another underlying cause such as bowel ischaemia.
This study is the first to show a link between nicorandil and colorectal fistulation. Others have shown an association between nicorandil and gastrointestinal ulceration, as well as fistula-in-ano. As this is a retrospective case-control study, it is limited in being unable to ascribe a direct aetiology. Although we can conclude there is a link between nicorandil and fistulation, we cannot say that nicorandil directly causes fistulation.
The pathophysiology of diverticular fistulation versus free perforation is poorly understood. Whether the two represent completely distinct entities or overlapping manifestations of the same underlying process is unknown. We feel that free perforation may relate to a more rapid and pneumatic pressure dependent process; whereas fistulation may relate to a more chronic inflammatory and ulcerative dependent process hence the association with nicorandil. We accept, however, that the distinction may be purely one of ‘geography’, relating to the anatomic relations of the sigmoid colon. There is no strong evidence to support either hypothesis. Nevertheless, if allowance is made for this possibility, and the data are re-analysed with the cases which later perforated added to the fistula group, the comparison remains statistically significant, albeit with a smaller P-value (0.028 versus 0.008).
We can propose a mechanism by which nicorandil may cause fistulation. The drug owes part of its effect to its property as a nitrate and NO donor.8 Endothelial derived relaxation factor, or NO, is produced in the body by endothelial derived nitric oxide synthase (eNOS) to induce vasodilation. It is also produced by inducible nitric oxide synthase (iNOS), as a pro-inflammatory mediator in macrophages. It may be that nicorandil releases pro-inflammatory NO in the sigmoid mucosa to promote fistulation in areas of diverticulosis.
More work is necessary before strong conclusions may be made regarding whether nicorandil actually causes fistulation. Larger scale studies and longitudinal cohort studies following patients on nicorandil are necessary to ascribe causation confidently. However, it may be prudent to avoid the use of nicorandil in patients with clinical, radiological or endoscopic evidence of diverticular disease.
Acknowledgments
The authors are grateful to the Audit Department of Russell's Hall Hospital for assistance in retrieving case notes.
References
- 1.Nakae I, Quan L, Hashimoto K, Sugimoto Y, Tsutamoto T, Kinoshita M. Mechanism of the vasodilatory action of nicorandil on coronary circulation in dogs. Cardiovasc Drugs Ther. 1994;8:137–45. doi: 10.1007/BF00877102. [DOI] [PubMed] [Google Scholar]
- 2.Brown R, Lee A, Welfare M. Nicorandil-induced colonic ulceration. Heart. 2008;94:678. doi: 10.1136/hrt.2007.134379. [DOI] [PubMed] [Google Scholar]
- 3.Egred M, Andron M, Morrison WL. Nicorandil may be associated with gastrointestinal ulceration. BMJ. 2006;332:889. doi: 10.1136/bmj.332.7546.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Healy CM, Smyth Y, Flint SR. Persistent nicorandil induced oral ulceration. Heart. 2004;90:e38. doi: 10.1136/hrt.2003.031831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdelrazeq AS, Owen C, Smith L, McAdam JG, Pearson HJ, Leveson SH. Nicorandil-associated para-stomal ulceration: case series. Eur J Gastroenterol Hepatol. 2006;18:1293–5. doi: 10.1097/01.meg.0000243880.02197.8b. [DOI] [PubMed] [Google Scholar]
- 6.Birnie A, Dearing N, Littlewood S, Carlin E. Nicorandil-induced ulceration of the penis. Clin Exp Dermatol. 2008;33:215–6. doi: 10.1111/j.1365-2230.2007.02650.x. [DOI] [PubMed] [Google Scholar]
- 7.Chan SK, Harris MD, Baldwin PJ, Sterling JC. Vulvovaginal ulceration during prolonged treatment with nicorandil. Br J Obstet Gynaecol. 2009;116:1403–5. doi: 10.1111/j.1471-0528.2009.02259.x. [DOI] [PubMed] [Google Scholar]
- 8.Kukovetz WR, Holzmann S, Poch G. Molecular mechanism of action of nicorandil. J Cardiovasc Pharmacol. 1992;20(Suppl 3):S1–7. doi: 10.1097/00005344-199206203-00002. [DOI] [PubMed] [Google Scholar]


