Abstract
INTRODUCTION
Extra-anatomical bypass grafting is a recognised method of lower limb re-vascularisation in high-risk patients who cannot tolerate aortic cross clamping, or in those with a hostile abdomen. We present a single surgeon series of such procedures and determine relevant outcomes.
PATIENTS AND METHODS
A retrospective review was performed on a prospectively maintained database of patients undergoing femoro-femoral or axillo-femoral bypass surgery between 1986 and 2004.
RESULTS
Patency rates for femoral (n = 28; 32%) versus axillary (n = 59; 68%) bypass procedures at 1 month, 1, 3 and 5 years were (92% vs 93%), (69% vs 85%), (60% vs 72%) and (55% vs 67%), respectively. Patient survival rates for the corresponding procedures and time intervals were (96% vs 90%), (96% vs 67%), (85% vs 45%) and (73% vs 38%) and revealed a significantly lower survival rate in those undergoing axillary procedures (P = 0.002). Limb salvage rates were calculated at (100% vs 91%), (96% vs 84%), (96% vs 81%) and (92% vs 81%) with no statistically significant difference found between the two groups (P = 0.124). Two-thirds of the patients who required major amputation died within 12 months of surgery.
CONCLUSIONS
Acceptable 30-day morbidity, long-term primary patency and survival rates are obtainable in patients suitable for extra-anatomical bypass surgery despite having significant co-morbidities. We have shown 5-year patency rates in those that survive axillary procedures to be as good as those undergoing femoral procedures. Furthermore, surviving patients who evade amputation within a year have an excellent chance of long-term limb salvage.
Keywords: Extra-anatomical bypass grafting, Femoro-femoral, Axillo-femoral, Limb salvage
Since Freeman and Leeds1 first described the femoro-femoral crossover graft in 1952 and later, Blaisdell and Hall2 along with Louw3 proposed the now well-established axillo-femoral bypass in 1963, extra-anatomical bypass procedures have been a recognised method of lower limb revascularisation in patients with aorto-iliac disease.
At present, patients are increasingly being offered percutaneous angioplasty and stenting for lower limb ischaemia due to stenotic arterial disease. However, surgical approaches are still appropriate and have a major role to play in patients with severe symptoms due to long occlusions of the aorto-iliac segments or where angioplasty has failed. Furthermore, Whatling et al.4 have recently shown better long-term patency following femoro-femoral grafting when compared to angioplasty with stenting for aorto-iliac disease.
Although the surgical gold standard for aorto-iliac disease is a direct aorto-iliac/femoral replacement, extra-anatomical grafts have a place where patients have poor cardiac or respiratory reserve, who cannot tolerate a trans-abdominal approach or in those with a hostile abdomen where a direct approach would be contra-indicated due to the extent of abdominal pathology.
We present a review of a single surgeon's experience with extra-anatomical bypass procedures over an 18-year period in terms of 30-day morbidity and mortality and 1 month, 1, 3 and 5 year primary patency rates, patient survival and limb salvage rates.
Patients and Methods
A retrospective review was performed on a single surgeon's prospectively maintained database of consecutive patients undergoing femoro-femoral or axillo-femoral grafting procedures over an 18-year period.
Data collected included patient demographics, presenting symptoms, co-morbidities, the surgical procedure performed and postoperative complications. All patients were followed-up and graft patency determined by clinical assessment, duplex and ultrasonography. Follow-up at 5 years for all surviving patients was complete.
Patients were categorised as having ‘femoral procedures’ (femoro-femoral bypass surgery) or ‘axillary procedures’ (axillo-unifemoral bypass or axillo-bifemoral bypass surgery). All operations were performed under general anaesthetic. For both procedures, longitudinal incisions were made in the groin and 2000 units of unfractionated heparin given intravenously immediately before arterial clamping was undertaken. For femoral procedures, an 8-mm graft was tunnelled subcutaneously, all grafts were Dacron and all anastomotic sutures were polypropylene. In those patients undergoing axillary procedures, electively the right (rather than left) axilliary artery was mobilised and an 8-mm Dacron graft tunnelled subcutaneously in the mid-axilliary line. Again, polypropylene sutures were used for the graft anastomoses.
Statistical analyses were performed using the SPSS for Windows v.14.0 (SPSS Inc., Chicago, IL, USA), with survival rates calculated by the Kaplan–Meier method and differences assessed with the Mantel–Cox log rank test. Other data were analysed using Fisher's Exact test, with P < 0.05 considered significant.
Results
A total of 87 patients underwent extra-anatomical bypass procedures (EABP) which included 28 (32%) femoral procedures and 59 (68%) axillary procedures.
The median patient age at surgery was 67 years (range, 36–94 years) and the gender distribution revealed a predominance of males (67%) to females (33%). Twenty patients (23%) underwent urgent surgery (following morning operating list) and the remaining 66 (77%) were elective procedures.
The indications for surgery were critical ischaemia in 44 (51%) and severe incapacitating claudication in 43 (49%). Of all patients, 68% were categorised by a consultant anaesthetist as having an American Society of Anesthesiologists (ASA) grade of 3 or above. Patient co-morbidities (Appendix 1 online) were found at similar frequencies in the two groups. However, there were significantly more patients with an ASA > 3 in those having an axillary procedure (46 of 59, compared with 13 of 28; P = 0.006).
Pre-operative angioplasty was performed on seven patients having femoral procedures and three patients having axillary procedures.
Thirty-day morbidity and mortality
Postoperative complications included a total of 19 (21%) infections (17 axillary, 2 femoral) of which 12 (14%) were local skin infections (11 axillary, 1 femoral) and seven (8%) were of the graft (6 axillary, 1 femoral). In six of these, the grafts had to be removed (5 axillary, 1 femoral). Early graft occlusion occurred in nine (10%) patients (7 axillary, 2 femoral). Of these, thrombectomy was performed in all nine, and was successful in four (3 axillary, 1 femoral). Revision surgery was undertaken in five (4 axillary, 1 femoral; Table 1]. Further surgery (excluding amputations) was performed in eight (7 axillary, 1 femoral).
Table 1.
Postoperative complications and further interventions
| Femoro-femoral (n = 28) | Axillo-femoral (n = 59) | Total (n = 87) | P-value | |
|---|---|---|---|---|
| Skin infection | 1 (3.6%) | 11 (18.6%) | 12 (13.7%) | 0.093 |
| Graft infection | 1 (3.6%) | 6 (10.2%) | 7 (8.0%) | 0.421 |
| Seroma | 0 | 4 (6.8%) | 4 (4.6%) | 0.301 |
| Early graft occlusion | 2 (7.1%) | 7 (11.9%) | 9 (10.3%) | 0.712 |
| Embolectomy | 0 | 1 (1.7%) | 1 (1.1%) | 1.00 |
| Thrombectomy | 2 (7.1%) | 7 (11.9%) | 9 (10.3%) | 0.712 |
| Patency successfully restored | 1 (3.6%) | 4 (6.8%) | 5 (5.7%) | 1.00 |
| Revision surgery | 1 (3.6%) | 4 (6.8%) | 5 (5.7%) | 1.00 |
| Further surgery | 1 (3.6%) | 7 (11.9%) | 8 (9.2%) | 0.428 |
| Removal of graft | 1 (3.6%) | 5 (8.5%) | 6 (6.9%) | 0.659 |
| Major amputation | 2 (7.1%) | 9 (15.3%) | 11 (12.6%) | 0.496 |
Eight (9%) patients died within 30 days of their operation (7 axillary, 1 femoral). Causes of death were cardiac (n = 4), septicaemia (n = 2), pneumonia (n = 1), and one cause was not recorded.
Primary patency and survival
The primary patency rates for femoral versus axillary procedures at 1 month, 1, 3 and 5 year were 92% vs 93%, 69% vs 85%, 60% vs 72% and 55% vs 67%, respectively. The survival curves of those undergoing each procedure are illustrated in Figure 1. The survival rates were found to be significantly less in those undergoing axillary procedures (P = 0.002). The causes of death at 5 years are shown in Table 2.
Figure 1.
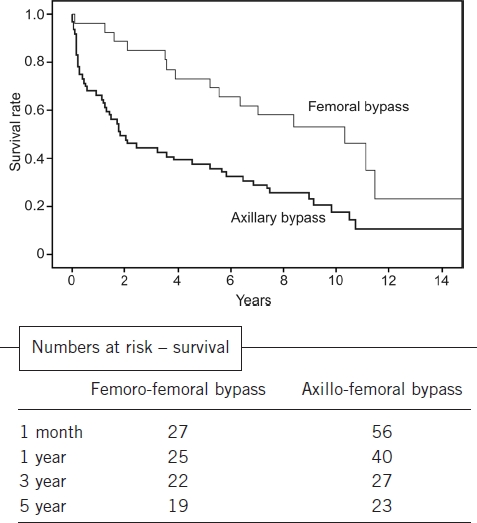
Kaplan-Meier estimates of survival for 15 years for femoral and axillary procedures.
Table 2.
Causes of death at 5-year follow-up
| Cause of death | Femoro-femoral | Axillo-femoral | Total |
|---|---|---|---|
| MI/cardiac arrest/other cardiac | 3 | 15 | 18 |
| Pneumonia/COPD | 0 | 6 | 6 |
| Benign bowel pathology | 0 | 4 | 4 |
| Cardiac failure | 1 | 3 | 4 |
| Postoperative vascular complication | 0 | 3 | 3 |
| Cancer | 1 | 2 | 3 |
| Stroke | 0 | 1 | 1 |
| Sepsis | 3 | 1 | 4 |
| Abdominal aortic aneurysm | 0 | 1 | 1 |
| Not recorded | 1 | 3 | 4 |
MI, myocardial infarct; COPD, chronic obstructive airways disease.
Limb salvage rates
Limb salvage rates for those undergoing femoral versus axillary procedures in this series were calculated as 100% vs 91%, 96% vs 84%, 96% vs 81% and 92% vs 81% at 1 month, 1, 3 and 5 years, respectively. There was no statistically significant difference in limb salvage rates for the two procedures (P = 0.124).
Overall, six patients required an above-knee, and five had below-knee amputations totalling 12.6% of the 87 patients included in this study. Of these 11 amputations (9 axillary, 2 femoral), three followed removal of an infected graft. The mortality rates within this subgroup for patients requiring an amputation were 8%, 67%, 83% and 83% at 1 month, 1, 3, and 5 years, respectively.
Discussion
With the current wide-spread use of angioplasty for the treatment of iliac disease, extra-anatomical bypass procedures (EABP) are now less commonly performed. Upchurch et al.5 showed, during the late 1990s, that as angioplasty rates increased substantially, EABP rates fell, and it was recently suggested by Hertzer et al.6 that EABP rates have been falling since the mid-1980s. At our centre, all patients presenting with aorto-iliac disease are initially discussed in conjunction with consultant interventional radiologists regarding their suitability for angioplasty. Between January 1999 and December 2004, a total of 471 angioplasty procedures (excluding stents) were performed on 385 patients. Of these, 127 were of the common iliac artery and 81 were of the external iliac artery.
The TransAtlantic Inter-Society Consensus (TASC) Working Group7 concluded in 2000 that open surgery should be considered for long segment (> 10 cm) stenoses or ‘type D’ iliac occlusions. Furthermore, EABPs still have a role in high-risk patients, where angioplasty has previously failed and/or on those patients with an already hostile abdomen.
Our review has highlighted interesting findings which challenge current thinking surrounding EABP, particularly axillary procedures. It appears that, although there was a trend towards infection and early graft occlusion in patients undergoing axillary procedures, this was not found to be significant (P = 0.093). Moreover, we found better than expected primary patency rates but poorer survival rates in those having axillary procedures. In this series, 5-year primary patency rates following femoral and axillary procedures were 55% and 65%, respectively. Previous studies (Appendix 2 online) have shown comparable results following femoral procedures (52% to 83%) but poorer long-term patency following axillary procedures (27% to 62%).6,8–14
Five-year survival, in the present series, was found to be significantly higher after femoral procedures at 73% compared to 38% following axillary procedures. These figures compare favourably to other studies showing 5-year survival to be 42–80% for femoral procedures and 27–34% following axillary procedures.6,8–14 Poor survival following EABP has been related to the adverse affect of advancing age, diabetes, hypertension, critical limb ischaemia and ischaemic heart disease.15–17 The median age of all patients included in this series was greater than 65 years and the majority of patients had an ASA score of 3 or greater; therefore, the patients in this study were a high-risk population.
Regarding limb salvage rates, major amputation was required in 11% of patients in this series which is in line with previous studies which reported figures of 7.4–27%.6,13 Interestingly, further analysis of this subgroup revealed 67% of patients who required an amputation died within one year of their EABG.
Conclusions
Acceptable 30-day morbidity, long-term primary patency and survival rates are still obtainable in patients suitable for extra-anatomical bypass surgery despite having significant co-morbidities. We have shown 5-year patency rates, in those that survive axillary procedures, to be as good as those undergoing femoral procedures. It should be noted, however, that early mortality rates were higher overall in the axillary group. Furthermore, surviving patients who evade amputation within a year have an excellent chance at long-term limb salvage. With this in mind, it appears, despite the increasing popularity and use of angioplasty, EABG still has its place in selected patients with occlusive aorto-iliac disease.
References
- 1.Freeman NE, Leeds FH. Operations on large arteries; application of recent advances. Calif Med. 1952;77:229–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Blaisdell FW, Hall AD. Axillary-femoral artery bypass in lower extremity ischaemia. Surgery. 1963;54:563–8. [PubMed] [Google Scholar]
- 3.Louw JH. Splenic to femoral and axillary to femoral bypass grafts in diffuse artherosclerotic occlusive disease. Lancet. 1963;1:1401–2. [Google Scholar]
- 4.Whatling PJ, Gibson M, Torrie EP, Magee TR, Galland RB. Iliac occlusions: stenting or crossover grafting? An examination of patency and cost. Eur J Vasc Endovasc Surg. 2000;20:36–40. doi: 10.1053/ejvs.2000.1113. [DOI] [PubMed] [Google Scholar]
- 5.Upchurch GR, Jr, Dimmick JB, Wainess RM, Eliason JL, Henke PK, et al. Diffusion of new technology in health care: the case of aorto-iliac occlusive disease. Surgery. 2004;136:812–8. doi: 10.1016/j.surg.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 6.Hertzer NR, Bena JF, Karafa MT. A personal experience with direct reconstruction and extra-anatomic bypass for aortoiliofemoral occlusive disease. J Vasc Surg. 2007;45:527–35. doi: 10.1016/j.jvs.2006.09.065. [DOI] [PubMed] [Google Scholar]
- 7.TransAtlantic Inter-Society Consensus (TASC) Working Group. Management of peripheral arterial disease. J Vasc Surg. 2000;31(Suppl):1–296. [PubMed] [Google Scholar]
- 8.Harris KA, Niesobska V, Carroll SE, De Rose G, Jamieson WG, et al. Extra-anatomic bypass grafting: a rational approach. Can J Surg. 1989;32:113–8. [PubMed] [Google Scholar]
- 9.Cuschieri RJ, Gilmour DG, Leiberman DP. Extra-anatomic bypass grafts for severe lower limb ischaemia. J R Coll Edinb. 1988;33:84–7. [PubMed] [Google Scholar]
- 10.Rutherford RB, Patt A, Pearce WH. Extra-anatomic bypass: a closer view. J Vasc Surg. 1987;6:437–46. [PubMed] [Google Scholar]
- 11.Kalman P, Hosang M, Johnston KW, Walker PM. The current role for femoro-femoral bypass. J Vasc Surg. 1987;6:71–6. doi: 10.1067/mva.1987.avs0060071. [DOI] [PubMed] [Google Scholar]
- 12.Kalman P, Hosang M, Johnston KW, Walker PM. Unilateral iliac disease: the role of iliofemoral bypass. J Vasc Surg. 1987;6:139–43. doi: 10.1067/mva.1987.avs0060139. [DOI] [PubMed] [Google Scholar]
- 13.Foster MC, Mikulin T, Hopkinson BR, Makin GS. A review of 155 extra-anatomic bypass grafts. Ann R Coll Surg Engl. 1986;68:216–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Aamold J, Baardsen A, Bjørnland G, Capoferro R, Folleras G, et al. Extra-anatomic axillo-femoral and femoro-femoral bypass grafting. VASA. 1980;9:293–5. [PubMed] [Google Scholar]
- 15.Crawford ES, Bomberger RA, Glaeser DH, Saleh SA, Russell WL. Aortoiliac occlusive disease: factors influencing survival and function following reconstructive operation over a twenty-five-year period. Surgery. 1981;90:1055–67. [PubMed] [Google Scholar]
- 16.Reed AB, Conte MS, Donaldson MC, Mannick JA, Whittemore AD, Belkin M. The impact of patient age and aortic size on the results of aortobifemoral bypass grafting. J Vasc Surg. 2003;37:1219–25. doi: 10.1016/s0741-5214(02)75179-3. [DOI] [PubMed] [Google Scholar]
- 17.Faries PL, LoGerfo FW, Hook SC, Pulling MC, Akbari CM, et al. The impact of diabetes on arterial reconstructions for multi-level arterial occlusive disease. Am J Surg. 2001;181:251–5. doi: 10.1016/s0002-9610(01)00551-7. [DOI] [PubMed] [Google Scholar]


