Abstract
Background and Purpose
Prior studies of intracerebral hemorrhage (ICH) outcome prediction models have not systematically included adjustment for comorbid conditions. The purpose of this study was to assess whether the Charlson Comorbidity Index (CCI), was associated with early mortality and long-term functional outcome in patients with intracerebral hemorrhage.
Methods
We performed a retrospective analysis on a prospective observational cohort of patients with ICH admitted to two UCSF hospitals from 6/1/2001-5/31/2004. Components of the ICH Score and use of early care limitations were recorded. Outcome was assessed using the modified Rankin Scale (mRS) out to 12-months. The CCI was derived using hospital discharge ICD-9 CM codes and patient history obtained from standardized case report forms.
Results
In this cohort of 243 ICH patients comorbid conditions were common, with CCI scores ranging from 0 to 12. Only 29% of patients with high CCI scores (≥3) achieved a 12-month mRS score of 3 or better compared with 48% of patients with CCI scores of 0 (p=0.02). CCI score was independently predictive of 12-month functional outcome, with higher CCI having a greater impact (CCI=2, OR=2.3, p=0.06; CCI ≥3, OR=3.5, p=0.001).
Conclusion
Comorbid medical conditions as measured by the CCI independently influence outcome after ICH. Future ICH outcome studies should account for the impact of comorbidities on patient outcome.
Keywords: Intracerebral hemorrhage, Charlson Comorbidity Index, Stroke Outcome, Comorbidity
INTRODUCTION
Medical comorbidities are common in patients with intracerebral hemorrhage (ICH).1 While it seems intuitive that comorbid conditions influence outcome after ICH, studies assessing specific predictors of ICH outcome have generally not evaluated the independent impact of these comorbidities and none have used a systematic approach to comorbidity adjustment.2 The Charlson Comorbidity Index (CCI) accounts for multiple comorbidities by creating a sum score weighted according to the presence of various conditions. The CCI has been validated in various diseases in longitudinal studies including ischemic stroke.3. Although some studies have included patients with ICH,4 none have focused on the impact of the CCI on ICH outcome. The purpose of this study was to assess if the CCI is associated with long-term functional outcome and 30-day mortality independent of factors known to influence ICH outcome.
METHODS
Study Design and Subjects
We performed a retrospective analysis on a prospective observational cohort of patients with non-traumatic ICH who presented to two UCSF hospital emergency departments from June 1, 2001, through May 31, 2004. The details of the study design have been published previously.5
Measurements
The CCI was derived from discharge ICD-9-CM codes using a method adapted for this use.6 If patients were readmitted to the same hospital within the 12-month follow-up period after initial ICH, then discharge ICD-9-CM codes from these additional hospitalizations were also used in calculating the CCI. Additional information obtained from study case report forms was then used to supplement ICD-9-CM derived data.
Statistical Analysis
For the purposes of analysis, CCI scores were categorized as 0, 1, 2, and 3 or greater. Outcome on the modified Rankin Scale (mRS) was considered in two ways: as an ordinal variable using all mRS categories and dichotomized (favorable outcome mRS 0-3, unfavorable outcome mRS 4-6). Univariate analysis was performed using the Chi-square test for categorical variables. In order to assess whether the CCI independently influenced 12-month mRS, multivariable ordinal logistic regression was performed using the entire mRS and adjusting for components of the ICH Score. Because the use of DNR orders within the first day of hospital admission (early DNR orders) is known to influence ICH mortality, this was included in the multivariable model.7 Multivariable logistic regression was also preformed to assess the independent impact of the CCI on risk of 30-day mortality. Statistical analysis was performed using Stata (Version 11.1, College Station, TX), and significance was considered as p < 0.05.
RESULTS
The demographics of this cohort have been previously described.5 Table 1 shows the frequency of comorbidities represented in the CCI throughout the ICH cohort. The CCI score was significantly associated with an unfavorable 12-month outcome (p=0.02). Overall, 29% of patients with high CCI scores (≥3) had a favorable 12-month functional outcome compared with 48% of patients with a CCI score of 0. CCI scores were not associated with the use of early DNR orders (p=0.66) or withdrawal of medical support (p=0.08) suggesting that these care limitations were likely not instituted principally because of the presence of comorbid medical conditions.
Table 1.
Frequency of Charlson Comorbidity Index (CCI) Categories in ICH Cohort (n=243)
| Condition | CCI Weight | Frequency, % (n) |
|---|---|---|
| Myocardial Infarct | 1 | 9.1 (22) |
| Congestive Heart Failure | 1 | 9.5 (23) |
| Peripheral Vascular Disease | 1 | 2.9 (7) |
| Cerebrovascular Disease | 1 | 23.5 (57) |
| Dementia | 1 | 10.3 (25) |
| Chronic Pulmonary Disease | 1 | 11.1 (27) |
| Connective Tissue Disease | 1 | 3.3 (8) |
| Ulcer Disease | 1 | 2.5 (6) |
| Mild Liver Disease | 1 | 5.8 (14) |
| Diabetes | 1 | 19.8 (48) |
| Hemiplegia | 2 | 5.3 (13) |
| Moderate or Severe Renal Disease | 2 | 10.7 (26) |
| Diabetes with End Organ Damage | 2 | 2.9 (7) |
| Any Tumor | 2 | 6.6 (16) |
| Leukemia | 2 | 0.8 (2) |
| Lymphoma | 2 | 0.4 (1) |
| Moderate or Severe Liver Disease | 3 | 0 (0) |
| Metastatic Solid Tumor | 6 | 0.8 (2) |
| AIDS | 6 | 2.9 (7) |
In multivariate analysis, higher CCI was independently associated with worsened 12-month functional outcome independent of the components of the ICH Score, and use of early DNR orders (Table 2). Patients with a high CCI score (≥3) had 3.5 times greater odds of having a one point increase in the mRS at 12-months compared with those patients without CCI comorbidities (p=0.001). Per Table 2, there is a trend towards a dose-response relationship between increasing CCI score and increasing odds of worsened 12-month functional outcome. CCI score was also independently predictive of 30 day mortality. In multivariate analysis adjusting for the components of the ICH score, early DNR, and withdrawal of support, high CCI score (≥3) was associated with an 8.8 times increased odds of death at 30 days (95% CI 1.3-60.1, p=0.03). Sensitivity analyses including 3 patients with recurrent ICH during the study period or excluding patients with possible underlying lesions did not change the impact of CCI on outcome or study conclusions.
Table 2.
Independent Impact of CCI on 12-month Functional Outcome after ICH
| Predictor | Odds Ratio for 1 point worsening on mRS (95% CI) |
p |
|---|---|---|
| CCI = 1 | 1.78 (0.86-3.70) | 0.123 |
| CCI = 2 | 2.34 (0.98-5.61) | 0.056 |
| CCI ≥ 3 | 3.48 (1.64-7.37) | 0.001 |
| Age (per year) | 1.04 (1.02-1.06) | <0.001 |
| Hematoma Volume (per mL) | 1.02 (1.01-1.04) | 0.003 |
| GCS (per point increase) | 0.73 (0.66-0.81) | <0.001 |
Analysis adjusted for presence of IVH, infratentorial ICH origin, and use of early DNR orders. CCI groups are referenced against the group with CCI score=0. CCI=Charlson Comorbidity Index; mRS= modified Rankin Scale score; CI= confidence interval
DISCUSSION
In this study, the CCI was independently associated with worsened 12-month functional outcome and higher 30-day mortality after adjusting for the components of the ICH score and the use of early care limitations. This supports the use of the CCI as a validated method of accounting for patient comorbidities in ICH studies. The findings of this study are consistent with previous research evaluating the validity of the CCI in assessing comorbidity and functional outcome in ischemic stroke.3
A possible disadvantage to the CCI relates to the method of its determination. The use of ICD-9-CM codes for determining comorbidities is limited by the accuracy of coding and may underestimate the true incidence of comorbidities.8, 9 Even so, a prior systematic review of the CCI found no difference in the adjusted odds ratio for mortality regardless of whether the CCI was derived from administrative data or chart review.9 Two other limitations inherent in the CCI are that not all possible medical comorbidities are represented and that the contribution of individual comorbidities to patient outcome is unable to be assessed due to the sum score nature of the CCI. There are several limitations of this current study including the relatively small number of patients (n=243) and the fact that the CCI was determined retrospectively. Strengths were the ability to adjust for known ICH outcome predictors and the availability of prospectively acquired long-term functional outcome data. Also, the prospective nature of this study allowed the contribution of prior stroke and hemiplegia to be included.
Supplementary Material
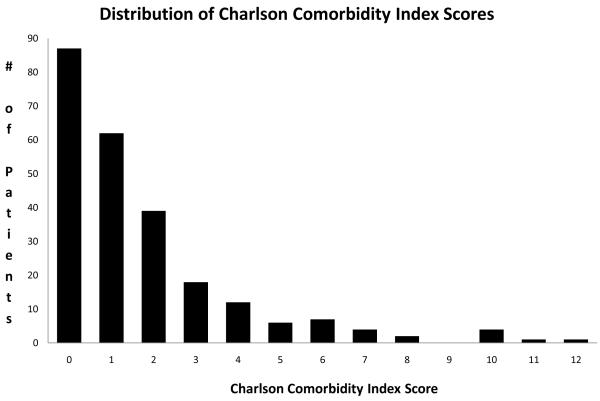
figure 1.
Distribution of Charlson Comorbidity Index sum scores across the entire ICH cohort (n=243)
Acknowledgments
Sources of Funding This work was funded in part by NIH/NINDS grant K23 NS41240 (JCH) and an unrestricted research grant from Novo Nordisk. This publication was supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130. Dr. Hemphill is also funded by NIH/NINDS grant U10 NS058931.
Footnotes
Disclosures Dr. Bar: none
Dr. Hemphill has received > $10,000 in research support from Novo Nordisk, the last having been received four years ago. He has received <$5000 for review of medical records of legal cases in the last two years related to intracerebral hemorrhage, but has not provided testimony in deposition or trial.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Andaluz N, Zuccarello M. Recent trends in the treatment of spontaneous intracerebral hemorrhage: Analysis of a nationwide inpatient database. J Neurosurg. 2009;110:403–410. doi: 10.3171/2008.5.17559. [DOI] [PubMed] [Google Scholar]
- 2.Rost NS, Smith EE, Chang Y, Snider RW, Chanderraj R, Schwab K, et al. Prediction of functional outcome in patients with primary intracerebral hemorrhage: The func score. Stroke. 2008;39:2304–2309. doi: 10.1161/STROKEAHA.107.512202. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke. 2004;35:1941–1945. doi: 10.1161/01.STR.0000135225.80898.1c. [DOI] [PubMed] [Google Scholar]
- 4.Zahuranec DB, Brown DL, Lisabeth LD, Gonzales NR, Longwell PJ, Smith MA, et al. Ethnic differences in do-not-resuscitate orders after intracerebral hemorrhage. Crit Care Med. 2009;37:2807–2811. doi: 10.1097/CCM.0b013e3181a56755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hemphill JC, 3rd, Farrant M, Neill TA., Jr. Prospective validation of the ich score for 12-month functional outcome. Neurology. 2009;73:1088–1094. doi: 10.1212/WNL.0b013e3181b8b332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with icd-9-cm administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 7.Becker KJ, Baxter AB, Cohen WA, Bybee HM, Tirschwell DL, Newell DW, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56:766–772. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- 8.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of icd-9-cm codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 9.Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the charlson comorbidity index using canadian administrative databases: A perspective on risk adjustment in critical care research. Crit Care. 2005;20:12–19. doi: 10.1016/j.jcrc.2004.09.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.