Abstract
Background and Purpose
Does progression of MRI-defined vascular disease predict subsequent vascular events in the elderly?
Methods
The Cardiovascular Health Study, a longitudinal cohort study of vascular disease in the elderly, allows the question to be answered because its participants had two MRI scans about five years apart and have been followed for about 9 years since the follow-up scan for incident vascular events.
Results
Both MRI-defined incident infarcts and worsened white matter grade (WMG) were significantly associated with heart failure (HF), stroke and death but not transient ischemic attacks, angina, or myocardial infarction. Strongest associations occurred when both incident infarcts and worsened WMG were present: for HF, hazard ratio 1.79 (95% confidence interval 1.18–2.73); for stroke, 2.58 (1.53–4.36); for death, 1.69 (1.28–2.24); and for cardiovascular death 1.97 (1.24–3.14).
Conclusions
Progression of MRI-defined vascular disease identifies elderly people at increased risk of subsequent HF, stroke, and death. Whether aggressive risk factor management would reduce risk is unknown.
Keywords: MRI, brain infarction, leukoaraiosis, stroke, death
The Cardiovascular Health Study (CHS) recruited 5,888 participants from four US sites and followed them for occurrence of vascular events. In participants without a history of transient ischemic attack or stroke, findings on the initial MRI scan predicted subsequent vascular events, including death.1–4 Incident brain infarcts and worsened white matter grade (WMG) between an initial and follow up MRI scan about five years later have also been characterized in CHS.5,6 Whether progression of these covert MRI findings predicts subsequent overt vascular events has not been addressed and may suggest a role for prevention.
Methods
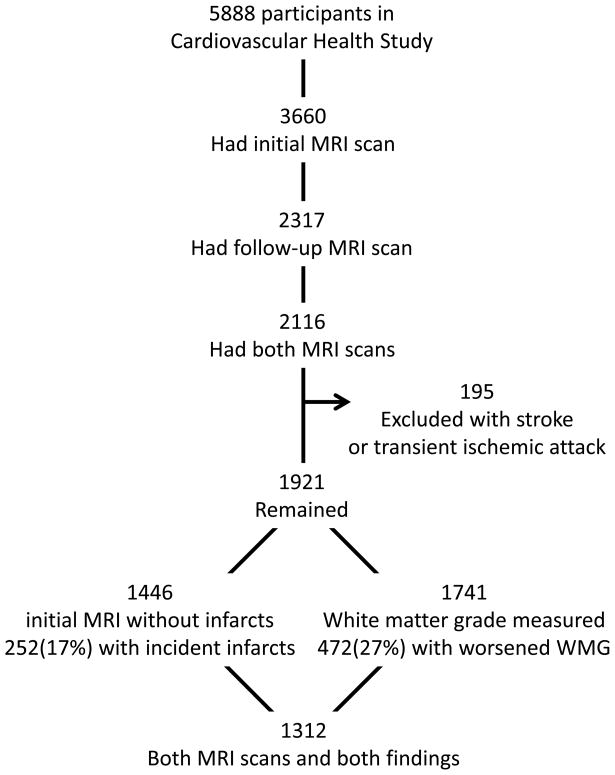
Participants with an initial and follow-up MRI scan and without an adjudicated stroke or transient ischemic attack before their follow-up scan were eligible for these analyses (Figure). All participants provided informed consent. As detailed previously5,6 (also please see http://stroke.ahajournals.org), progression was defined by incident infarcts, worsened WMG, or both on follow-up scans. Incident infarcts meant the initial scan showed no infarcts and the follow-up scan showed one or more infarcts.5 Worsened WMG meant the 10-point semi-quantitative measure of white matter hyperintensities worsened by one or more grades between initial and follow-up scan.6 All vascular events and death between completing follow-up MRI scans in 1997 to 1999 and 2008 June 30 were adjudicated, as detailed previously.7 Median follow-up after follow-up scans was 9.6 years (inter-quartile range=5.9–10.3). Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI), controlling for age, sex, time between scans, current smoking, weight, histories of coronary artery disease, heart failure (HF), claudication, hypertension and diabetes, all at the time of the follow-up scan, unless part of the outcome measure. Numbers in each analysis varied because participants who had events of interest prior to follow-up scans were excluded.
Figure.
Study flowchart.
Results
Incident infarct occurred in 252 (17%) of 1,446 participants, and worsened WMG, in 472 (27%) of 1,741 participants. Both assessments were available in 1,312 participants without an infarct on the initial scan. Associations for transient ischemic attack, angina, and myocardial infarction were not significant (data not shown). Table 1 shows events for incident infarcts, and Table 2, for worsened WMG. These findings were significantly associated with incident HF, stroke and death. Adding WMG on the initial scan to models for worsened WMG removed significance for stroke (HR=1.35, 95% CI 1.00–1.77, p=0.054), but significance was retained for HF and death. The strongest associations were when both incident infarcts and worsened WMG were present (please see http://stroke.ahajournals.org): for HF, hazard ratio (HR) 1.79 (95% CI 1.18–2.73); for stroke, 2.58 (1.53–4.36); for death, 1.69 (1.28–2.24); and for cardiovascular death 1.97 (1.24–3.14).
Table 1.
Incident rates per 1,000 person-years after follow-up MRI scan by incident infarct.
| Incident | # of Events / # at Risk, rate (95% CI) | Hazard Ratio* (95% CI) | |
|---|---|---|---|
| Event | Infarct absent | Infarct present | p-value |
| Heart failure | 216/1132 | 58/226 | 1.41 (1.05–1.89) |
| 24.2 (21.2–27.7) | 35.9 (27.8–46.5) | 0.021 | |
| Stroke | 105/1194 | 43/252 | 2.11 (1.48–3.02) |
| 10.9 (9.00–13.2) | 23.7 (17.6–32.0) | <0.001 | |
| Death | 535/1194 | 146/252 | 1.35 (1.12–1.62) |
| 53.7 (49.3–58.4) | 75.4 (64.1–88.7) | 0.002 | |
Abbreviations: CI, confidence interval.
Adjusted for age, sex, time between scans, and vascular risk factors, as detailed in Methods.
Table 2.
Incident rates per 1,000 person-years after follow-up MRI scan by worsened white matter grade.
| Incident | # of Events / # at Risk, rate (95% CI) | Hazard Ratio (95% CI) | |
|---|---|---|---|
| Event | Worsening absent | Worsening present | p-value |
| Heart failure | 250/1176 | 115/441 | 1.34 (1.07–1.67) |
| 27.5 (24.3–31.2) | 37.7 (31.4–45.3) | 0.010 | |
| Stroke | 135/1269 | 63/472 | 1.39 (1.02–1.88) |
| 13.5 (11.4–15.6) | 19.0 (14.8–24.3) | 0.035 | |
| Death | 582/1269 | 288/472 | 1.46 (1.26–1.68) |
| 55.8 (51.4–60.5) | 82.0 (73.1–92.1) | <0.001 | |
Footnotes as in Table 1.
Discussion
In CHS participants without adjudicated stroke or transient ischemic attacks, progression of covert MRI-defined brain vascular disease with incident infarcts, worsened WMG, or both predicted subsequent incident HF, stroke, and death. Risk of stroke more than doubled in those with incident infarcts. Although WMG on the initial scan appears to be more important than worsened WMG for the outcome of stroke, worsened WMG was significantly related to HF and death regardless of initial WMG.
That progression of covert brain vascular disease would increase the risk of subsequent overt brain vascular disease seems logical, but why it would increase the risk of HF and death is less clear. Perhaps these associations reflect shared risk factors that were not considered or not well-measured since including risk factor measures in multivariable models did not eliminate these significant associations.
Although the study has strength in its large longitudinal cohort design, MRI scans were performed at a time when quantitative assessment of white matter progression on serial scans was not available. In addition, careful assessment of MRI-defined brain infarcts in participants with transient ischemic attacks or strokes to know which ones were covert and overt was not performed. Such information would be important in determining more precisely the added value of serial MRI scans over a single scan. Finally, not all CHS participants underwent both MRI scans (Figure), and those who did were healthier in general than those who did not,5,6 suggesting that these results may underestimate the risk of these outcomes in the entire cohort.
Progression of covert MRI-defined brain vascular disease is associated with subsequent HF, stroke, and death. Interventions aimed to slow, halt, or reverse this progression may be worth exploring. The goal would be to reduce the risk of these outcomes.
Supplementary Material
Acknowledgments
Funding
This research was supported by National Heart Lung and Blood Institute Grant/Contract numbers N01-HC-85239, N01-HC-85079 through N01-HC-85086; N01-HC-35129, N01 HC-15103, N01 HC-55222, N01-HC-75150, N01-HC-45133; HL080295, HL-075366; National Institute of Aging Grant/Contract numbers AG-023269, AG-15928, AG-20098, and AG-027058; University of Pittsburgh Claude D. Pepper Older Americans Independence Center grant number P30-AG-024827; with additional contribution from National Institute of Neurological Disorders and Stroke. See also http://www.chs-nhlbi.org/pi.htm.
Footnotes
Disclosures
None.
References
- 1.Bernick C, Kuller L, Dulberg C, Longstreth WT, Jr, Manolio T, Beauchamp N, et al. Silent MRI infarcts and the risk of future stroke: the Cardiovascular Health Study. Neurology. 2001;57:1222–1229. doi: 10.1212/wnl.57.7.1222. [DOI] [PubMed] [Google Scholar]
- 2.Kuller LH, Longstreth WT, Jr, Arnold AM, Bernick C, Bryan RN, Beauchamp NJ., Jr White matter hyperintensity on cranial magnetic resonance imaging: a predictor of stroke. Stroke. 2004;35:1821–1825. doi: 10.1161/01.STR.0000132193.35955.69. [DOI] [PubMed] [Google Scholar]
- 3.Longstreth WT, Jr, Diehr P, Beauchamp NJ, Manolio TA. Patterns on cranial magnetic resonance imaging in elderly people and vascular disease outcomes. Arch Neurol. 2001;58:2074. doi: 10.1001/archneur.58.12.2074. [DOI] [PubMed] [Google Scholar]
- 4.Kuller LH, Arnold AM, Longstreth WT, Jr, Manolio TA, O'Leary DH, Burke GL, et al. White matter grade and ventricular volume on brain MRI as markers of longevity in the Cardiovascular Health Study. Neurobiol Aging. 2007;28:1307–1315. doi: 10.1016/j.neurobiolaging.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Longstreth WT, Jr, Dulberg C, Manolio TA, Lewis MR, Beauchamp NJ, Jr, O'Leary D, et al. Incidence, manifestations, and predictors of brain infarcts defined by serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2002;33:2376–2382. doi: 10.1161/01.str.0000032241.58727.49. [DOI] [PubMed] [Google Scholar]
- 6.Longstreth WT, Jr, Arnold AM, Beauchamp NJ, Jr, Manolio TA, Lefkowitz D, Jungreis C, et al. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2005;36:56–61. doi: 10.1161/01.STR.0000149625.99732.69. [DOI] [PubMed] [Google Scholar]
- 7.Longstreth WT, Jr, Bernick C, Fitzpatrick A, Cushman M, Knepper L, Lima J, et al. Frequency and predictors of stroke death in 5,888 participants in the Cardiovascular Health Study. Neurology. 2001;56:368–375. doi: 10.1212/wnl.56.3.368. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.