Abstract
Background
A universal goniometer is commonly used to measure the elbow’s ROM and carrying angle; however, some authors question its poor intertester reliability.
Questions/purposes
We (1) assessed the validity of goniometric measurements as compared with radiographic measurements in the evaluation of ROM of the elbow and (2) determined the reliability of both.
Methods
The ROM and carrying angle of 51 healthy subjects (102 elbows) were measured using two methods: with a universal goniometer by one observer three times and on radiographs by two independent examiners. Paired t-test and Pearson’s correlation were used to compare and detect the relationship between mean ROM. The maximal error was calculated according to the Bland and Altman method.
Results
The intraclass correlation coefficients (ICC) ranged from 0.945 to 0.973 for the goniometric measurements and from 0.980 to 0.991 for the radiographic measurements. The two methods correlated when measuring the total ROM in flexion and extension. The maximal errors of the goniometric measurement were 10.3° for extension, 7.0° for flexion, and 6.5° for carrying angle 95% of the time. We observed differences for maximum flexion, maximal extension, and carrying angle between the methods.
Conclusion
Both measurement methods differ but they correlate. When measured with a goniometer, the elbow ROM shows a maximal error of approximately 10°.
Clinical Relevance
The goniometer is a reasonable and simple clinical tool, but for research protocols, we suggest using the radiographic method because of the higher level of precision required.
Introduction
The elbow is a trochoginglymoid joint that articulates the distal humerus with the proximal radius and ulna, allowing flexion/extension movements [30]. With the humeral trochlea’s 300° arc of cartilage and the 190° arc of the ulna’s sigmoid notch, the elbow’s normal total ROM averages 145° (range, 140°–150°) [5, 12, 21, 29] in flexion/extension.
The ROM is a primary measure for assessing the elbow’s integrity and evaluating impairment. It is unlikely that a patient who can fully extend and lock his or her elbow will show radiographic evidence of injury [6, 16]. ROM also can be used as an investigative tool to verify disease progression or treatment effectiveness. The average values reported for extension and flexion are, 0° and 150°, respectively [21], with some authors differing slightly, with values between 5° and 140° [12]. The carrying angle (valgus) is defined as being the ulna’s lateral deflection from the shaft of the humerus when the elbow is fully extended and supinated. It is measured clinically in the evaluation of elbow fractures. Reported mean valgus ranges from 10° to 15° [21, 22, 34].
Healthcare professionals commonly use a goniometer to measure the ROM and carrying angle. The universal goniometer (UG) is a simple, easy-to-use instrument but its reliability and accuracy have been questioned [26], and, to date, no consensus has been reached [33]. However, the majority of studies agree that the UG has fair intraexaminer reliability but poor intertester reliability [1, 24, 33]. Intertester ICCs range from 0.26 to 0.99 [8, 26]. Some studies have poor methodologic quality [33]. In others the experimental protocol does not reflect day-to-day use of the UG [7, 11, 28]. Some authors also omit detailing the population, instruments, measurement methods, or protocol when reporting UG use, making it harder to assess reliability of the UG [1, 12]. The main sources of errors in goniometric measurements are positioning of the patient and instrument, ie, the variability in locating anatomic landmarks used to align the UG [1, 7]. These markers, including the lateral epicondyle of the humerus and the tip of the acromion, are potential sources of error because they do not represent the center of rotation or the long axis of the humerus [1, 5, 31].
We therefore (1) assessed validity of goniometric measurements by comparing goniometric values with radiographic ROM values measured from the humeral and ulnar axes and (2) determined the reliability of both methods.
Materials and Methods
We recruited 51 volunteers among healthcare workers of a hospital. Participants were enrolled by advertising within the hospital. There were 31 females and 20 males with a mean age of 31.7 ± 9.3 years (range, 19–50 years). All were informed of the protocol and signed a consent form if they fulfilled the inclusion criteria. Volunteers had to be between 18 and 50 years old with no history of arthritis or osteoarthritis, musculoskeletal or neurologic diseases, or past trauma affecting the upper limb. We excluded pregnant women or those we suspected might be pregnant.
For the goniometric method, we used one 360° scale (1°-increments) plastic UG with two 25-cm arms (3 M© Modular Shoulder System, 3 M©, St Paul, MN, USA).
The bony landmarks used to determine ROM (Fig. 1A–B) were defined as: the goniometer was centered on the lateral epicondyle, the stationary arm was pointing at the tip of the acromion process. There is a consensus for use of those two bony landmarks for elbow ROM measurement as they are easily located on the elbow and shoulder [1, 7, 21, 24]. The wrist landmark toward which the mobile arm of the goniometer is oriented sometimes is the ulnar styloid process but we preferred the middle portion of the wrist as it can be used for pronation, neutral, and supination positions (Fig. 1). A positive value of extension is equivalent to flexion, whereas a below-zero extension value represents hyperextension. For the carrying angle (Fig. 1C), the UG’s arms were oriented in the same way, except that the center of the instrument was positioned on the crossline of the bicep’s tendon and the interepicondyle axis. All volunteers were measured in the same room with the same equipment and by the same examiner (JC). Several studies report intraevaluator correlations of goniometry for various joints between 0.45 and 0.98 [1, 20, 26, 27] and that one examiner is acceptable regardless of his or her experience [1]. The participants were asked to sit on an armless chair and special care was taken to ensure that the arm position of the participants in the examination room was as close as possible to the one in radiology. We measured elbow extension and flexion with the humerus raised (shoulder in anterior flexion) and the wrist in neutral position. Valgus was measured with the arm in full extension and the hand supinated. The examiner took three measurements for each position, for both limbs, taking particular care to remind the volunteers to reach their maximal extension/flexion. Measurements of flexion, extension, and carrying angle were noted in degrees; precision for goniometric measurements is ± 0.5°.
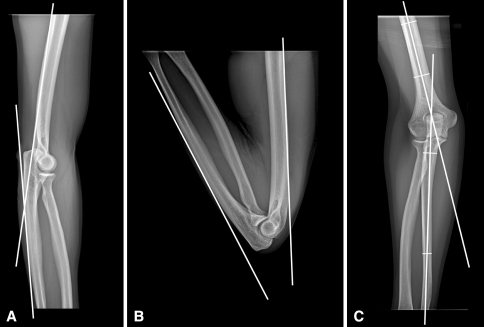
Fig. 1A–C.
The landmarks for (A) extension and (B) flexion are the lateral epicondyle, tip of the acromion, and midline of the wrist. (C) The instrument was centered on the crossline of the biceps tendon and the interepicondyle axis for the carrying angle measurement.
We considered radiographic images as a gold standard for ROM measurements for many reasons. Its computerized measurements are more precise and constant. Where the goniometer has 1°-increments and the examiner reported the measurements with a precision of ± 0.5°, the software used for the radiographic measurements automatically calculated with higher precision: between ± 0.02° and ± 0.1° depending on the dicom resolution (approximately 500–2000 pixels) of the radiograph used. The radiographic method also has the advantage of not being affected by the patient’s morphologic features, eg, the bony landmarks of a patient with long arms or a large amount of soft tissues are not as easily located, thus influencing the accuracy of the goniometric measurements [7, 31].
For radiographic method, a digital radiographic unit (GE Healthcare, Little Chalfont, Buckinghamshire, UK) was used, and subjects were protected with a lead apron. The same examiner (JC) correctly positioned the subjects on the wallstand radiographic table to standardize the radiographs. Three specific elements were considered. First, extension and flexion had to be maximal for all positions. Because the arm must lie on the table for the AP radiograph (carrying angle), we placed a 10-cm cushion under the distal humerus to elevate the forearm off the table. This setup allowed subjects to achieve full ROM. The cushion was removed for lateral extension and flexion positions. Second, we took precautions with the lateral radiographs; the examiner placed and rotated the fully extended elbow to make the capitellum and trochlea appear as concentric circles to achieve a perfect lateral view of the elbow [17]. Third, to maximize the precision of measurements, the radiographs had to include a long enough portion of the humerus and cubitus/radius.
The ROM and carrying angle were measured on the radiographs with SliceOmatic software (TomoVision, Magog, Quebec, Canada) by two of the coauthors (JC, FC). The examiners agreed on the bony landmarks that best represent the ROM and valgus (Fig. 2). They independently measured extension (Fig. 2A), flexion (Fig. 2B), and carrying angle (Fig. 2C) of all elbows on the radiographic images with a precision of ± 0.1°.
Fig. 2A–C.
Landmarks are the same for (A) extension and (B) flexion. The average humeral diaphysis axis and dorsal midthird edge of the ulna defines the angle of flexion. Measurement of the (C) carrying angle is complicated by the S shape of the ulna. The reference portions were the ulnar segment between the radial head and radial tuberosity and the farthest distal diaphysis segment on the radiograph.
We used the Kolmogorov-Smirnov test with a 95% CI to assess the normality of data distribution; we found values from 0.220 to 0.923 for goniometric ROM and from 0.746 to 0.990 for radiographic ROM, confirming the normality of distribution of these two parameters. The ICCs were used to test the reliability of the goniometric and radiographic measurements. Paired Student’s t-tests were used to compare mean flexion, extension, ROM, and carrying angle values between goniometric and radiographic values. Pearson’s correlation coefficient then was calculated to evaluate the relationships between the UG and radiographic measurements. Finally, we made a plot of the difference between UG and radiographic measurements, against the mean, to illustrate and interpret the range of differences, as recommended by Bland and Altman [3, 4] and Lee et al. [15]. The Bland-Altman method analyzes the agreement between two measurement methods. It focuses on the difference obtained in each pair of data and calculates the maximal error expected from the two methods. In our study, we used the Bland-Altman method to analyze the difference between the goniometer and the gold standard radiographs for each pair of 102 elbow measurements. We performed all statistical analyses with PASW Statistics 18.0 software (SPSS Inc, Chicago, IL, USA).
Results
In our sample, the goniometric elbow measurement values were different from those from the gold standard radiographs. When compared with ROM and carrying angle goniometric measurements (UG), the mean radiographic values were lower (Table 1). The largest differences observed were 153.5° ± 3.5° with UG measurement versus 150.9° ± 4.5° with radiographic measurement for flexion and 13.0° ± 3.0° with UG measurement versus 10.1° ± 4.5° with radiographic measurement for the carrying angle. The latter represents a 30% difference between the two methods. The results were closer for the elbow extension measurements with 13.0° ± 6.5° with UG measurement and 11.9° ± 6.7° with radiographic measurement. A larger difference was expected between the two ROM measurements because it includes extension and flexion. However, the goniometric arc of the ROM extension (140.5° ± 8.0°) was closer to the radiographic mean (139.0° ± 7.8°) compared with flexion. Overall, a difference between the two methods was observed for all four measurements. We observed a correlation (0.648–0.728) between the goniometric and radiographic measurements. For the Bland-Altman analysis of difference, the CI reached ± 10.3° for the extension measurements (Fig. 3A); 95% of the goniometric extension measurements were less than 10.3° different from the radiographic gold standard value (Table 2). For the flexion measurements, the 95% CI was ± 7.0° (Fig. 3B). The CI reached ± 11.5° for measurements of ROM (Fig. 3C). The carrying angle measurements had the smallest CI of ± 6.5° (Fig. 3D).
Table 1.
Comparison of the difference and correlation between goniometric and radiographic measurements
| Range of motion | Goniometry, mean ± SD (range) |
Radiography, mean ± SD (range) |
Paired Student’s t-test* t score; 95% CI (p value) |
PCC between both methods† (p value) |
|---|---|---|---|---|
| Flexion | 153.5° ± 3.5 | 150.9° ± 4.5 | 6.96; 1.73–3.11 | 0.648 |
| (143.5–160.5) | (140.4–159.8) | (p ≤ 0.001) | (p ≤ 0.001) | |
| Extension | 13.0° ± 6.5 | 11.9° ± 6.7 | 2.22; 0.18–2.14 | 0.688 |
| (−2.5–31.0) | (−3.5–28.4) | (p = 0.029) | (p ≤ 0.001) | |
| Total ROM (flexion-extension) | 140.5° ± 8.0 | 139.0° ± 7.8 | 2.28; 0.17–2.42 | 0.728 |
| (116.0–159.5) | (116.0–155.2) | (p = 0.025) | (p ≤ 0.001) | |
| Carrying angle | 13.0° ± 3.0 | 10.1° ± 4.5 | 9.35; 2.35–3.61 | 0.705 |
| (3.5–19.5) | (0.9–17.9) | (p ≤ 0.001) | (p ≤ 0.001) |
* Paired Student’s t-test assesses difference between means of both methods of measurement; †PCC evaluates correlation between goniometric and radiographic measurement; CI = confidence interval; PCC = Pearson correlation coefficient.
Fig. 3A–D.
In each diagram, the points (n = 102, both elbows of the 51 participants) represent the difference between both measurement methods (radiographs or goniometer) against the mean values in degrees. The middle line represents the mean difference, whereas the upper and lower lines indicate the 95% CI. For (A) extension, 95% of UG measurements were ± 10.3° from radiographic values. Similarly, the UG maximal error was (B) ± 7.0° for flexion, (C) ± 11.5° for total ROM, and (D) ± 6.5° for carrying angle. RX = radiographic; UG = universal goniometer.
Table 2.
Bland-Altman analysis of difference between radiographic and goniometric values*
| Range of motion | Mean ± SD of difference | Upper 95% CI limit (mean + 2 SD) | Lower 95% CI limit (mean – 2 SD) | Absolute maximal error (± 2 SD) |
|---|---|---|---|---|
| Flexion | −2.4° ± 3.5 | 4.6° | −9.5° | ± 7.0° |
| Extension | −1.1° ± 5.1 | 9.2° | −11.4° | ± 10.3° |
| Total ROM (flexion-extension) | −1.3° ± 5.7 | 10.2° | −12.8° | ± 11.5° |
| Carrying angle | −3.0° ± 3.2 | 3.5° | −9.5° | ± 6.5° |
* The difference was calculated with goniometric value subtracted from radiographic value; CI = confidence interval.
Reliability of both measurement methods was confirmed through ICCs. The ICCs for intrarater reliability of the goniometric measurement ranged from 0.945 to 0.973 (Table 3), whereas the interobserver ICC for the four radiographic measurements ranged from 0.980 to 0.991 (Table 4).
Table 3.
Intratester ICCs for goniometric measurements
| Range of motion | Mean ICC (n = 3)* | SD | 95% CI |
|---|---|---|---|
| Flexion | 0.945 | ± 0.016 | 0.905–0.985 |
| Extension | 0.973 | ± 0.007 | 0.956–0.990 |
| Carrying angle | 0.965 | ± 0.003 | 0.958–0.973 |
* One examiner measured 102 elbows three times; ICC = intraclass correlation coefficient; CI = confidence interval.
Table 4.
Intertester ICCs for radiologic measurements
| Range of motion | Right side ICC (n = 2)* | Left side ICC (n = 2) |
|---|---|---|
| Flexion | 0.980 | 0.985 |
| Extension | 0.991 | 0.991 |
| Carrying angle | 0.989 | 0.992 |
* Two examiners measured 102 elbows once; ICC = intraclass correlation coefficient.
Discussion
Previous studies confirmed the role of ROM as an indicator of the elbow’s integrity [6, 16, 18]. The UG is a common clinical tool for evaluations of the elbow and other major joints. However, the reliability of this instrument is still debated and some studies have investigated its intratester or intertester ICC, and/or compared it with new devices [1, 11, 20, 24, 33]. We therefore investigated the goniometer’s validity by comparing its measurements with the gold standard radiographic measurement of ROM of the elbow. The reliability of both instruments then was evaluated.
There are limitations to our study. First, there is a potential selection bias because only health workers were recruited; therefore, it is possible that this group of healthy adults has a better understanding of the examiner’s oral indications and that their collaboration improved our results. Patients, with traditional boundaries like pain, language, or cognitive difficulties, could prove less collaborative and thus lower correlation between both methods. This limitation does not compromise our conclusions because the subject-dependant boundaries apply equally to both measurement methods and the examiner (JC) provided the same indications of position. Second, the three repeated goniometric measurements were taken during the same day, to accommodate the volunteer participants of our study. This is not representative of the clinical situation in which such measurements are taken at intervals of weeks or months. However, we can compare our reliability results with those in the literature as few authors measured the elbows at weekly intervals or more [10, 11]. Third, the UG in this study was being used in a clinical way, ie, with no calibration or instrument choice; therefore, there is a potential source of systematic errors from the instrument. However, this corresponds to the goniometric measurement performed in a clinic or hospital setting. Moreover, the goniometric average results of ROM and carrying angle correspond to those in the literature [21, 22, 34], especially for the valgus (13.0°) and flexion (153.5°) angles.
We evaluated the validity of the goniometer in comparison to the computerized radiographs. While measurements from the two methods correlated, we observed systematic differences. We also concluded that the extension angle, measured with a UG, would have a maximal error of ± 10.3°, 95% of the time (Table 2). This represents the worst case scenario, because the difference with the flexion angle was ± 7.0° and ± 6.5° for the carrying angle 95% of the time. The maximal error was higher for the total ROM (± 11.5°) because it involved two measurements (extension and flexion). Regarding the means for goniometric measurement and radiographs, as the middle portion of the wrist was our landmark instead of the ulnar styloid process, the extension values differ from zero. The augmented flexion mean with the goniometer cancels the diminished extension, resulting in similar ROM means (Table 1). When reviewing the literature, there are numerous methods for measuring ROM: visual estimation [2, 13, 32, 33], photographic [7], fluid-based [10, 24] or electrogoniometer [10, 11, 34]. Results regarding the validity of the goniometer are ambivalent. In the same way, when comparing the goniometer with radiographs, Jaeger et al. [14] validated the goniometric measurement in cats. However, Piqué-Vidal et al. [25] recommended computerized radiographs for hallux valgus assessment. We still recommend using a UG in a clinical setting where therapists or physicians commonly deal with 30° to 40° loss of ROM in pathologic situations rather than 5° to 10°. However, the radiographic method is a valuable tool for randomized controlled trials or other research studies with ROM as a primary or secondary outcome, such as studies designed to evaluate the impact of different demographic or extrinsic factors on ROM [9, 12, 18, 19, 22, 23]. When the ROM or carrying angle is required for research purposes, the 10°-difference between the goniometric and radiographic methods becomes important, leading to an increase in the cohort needed to find expected results, and one must keep in mind that any measurement performed with the goniometer has a potential (maximal) error of 10°.
Reliability of both methods was assessed through ICCs. For flexion/extension, using a standard 25-cm plastic goniometer, the ICC for the intraexaminer ranged from 0.945 to 0.973, whereas reported ranges are from 0.45 to 0.98 (Table 5) [1, 20, 26]. The interobserver reliability is important in a clinical setting and proper training may be required for all who use the goniometer to standardize the measurements. In daily patient care, ROM might not be measured by the same examiner and weeks or even months could separate measurements (eg, a followup on postsurgical rehabilitation among the orthopaedist, resident, occupational therapist, etc). We observed intertester ICCs ranging from 0.980 to 0.991 with the radiographic method.
Table 5.
Comparison of intrarater ICCs for goniometric measurement of the elbow
| Study | Healthy subjects? (Yes/No) | Number of subjects | Number of repetitions | Flexion ICC | Extension ICC |
|---|---|---|---|---|---|
| Rothstein et al. [27] | No | 24 | 2 | 0.97 | 0.96 |
| Greene & Wolfe [11] | Yes | 20 | 9 | 0.94 | 0.95 |
| Goodwin et al. [10] | Yes | 23 | 2 | 0.87 | 0.87 |
| Armstrong et al. [1] | No | 38 | 2 | 0.55 to 0.98 | 0.45 to 0.98 |
| Current study | Yes | 51 | 3 | 0.95 | 0.97 |
ICC = Intraclass correlation coefficient.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Hôpital du Sacré-Cœur de Montreal, Quebec, Canada.
References
- 1.Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7:573–580. doi: 10.1016/S1058-2746(98)90003-9. [DOI] [PubMed] [Google Scholar]
- 2.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83:1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 3.Bland JM, Altman DG. A note on the use of the intraclass correlation coefficient in the evaluation of agreement between two methods of measurement. Comput Biol Med. 1990;20:337–340. doi: 10.1016/0010-4825(90)90013-F. [DOI] [PubMed] [Google Scholar]
- 4.Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93. doi: 10.1002/uog.122. [DOI] [PubMed] [Google Scholar]
- 5.Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756–759. [PubMed] [Google Scholar]
- 6.Docherty MA, Schwab RA, Ma OJ. Can elbow extension be used as a test of clinically significant injury? South Med J. 2002;95:539–541. [PubMed] [Google Scholar]
- 7.Fish DR, Wingate L. Sources of goniometric error at the elbow. Phys Ther. 1985;65:1666–1670. doi: 10.1093/ptj/65.11.1666. [DOI] [PubMed] [Google Scholar]
- 8.Glasgow C, Wilton J, Tooth L. Optimal daily total end range time for contracture: resolution in hand splinting. J Hand Ther. 2003;16:207–218. doi: 10.1016/S0894-1130(03)00036-X. [DOI] [PubMed] [Google Scholar]
- 9.Golden DW, Wojcicki JM, Jhee JT, Gilpin SL, Sawyer JR, Heyman MB. Body mass index and elbow range of motion in a healthy pediatric population: a possible mechanism of overweight in children. J Pediatr Gastroenterol Nutr. 2008;46:196–201. doi: 10.1097/MPG.0b013e31812f568b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodwin J, Clark C, Deakes J, Burdon D, Lawrence C. Clinical methods of goniometry: a comparative study. Disabil Rehabil. 1992;14:10–15. doi: 10.3109/09638289209166420. [DOI] [PubMed] [Google Scholar]
- 11.Greene BL, Wolf SL. Upper extremity joint movement: comparison of two measurement devices. Arch Phys Med Rehabil. 1989;70:288–290. [PubMed] [Google Scholar]
- 12.Gunal I, Kose N, Erdogan O, Gokturk E, Seber S. Normal range of motion of the joints of the upper extremity in male subjects, with special reference to side. J Bone Joint Surg Am. 1996;78:1401–1404. doi: 10.2106/00004623-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289–294. doi: 10.1016/s0004-9514(14)60274-9. [DOI] [PubMed] [Google Scholar]
- 14.Jaeger GH, Marcellin-Little DJ, Depuy V, Lascelles BD. Validity of goniometric joint measurements in cats. Am J Vet Res. 2007;68:822–826. doi: 10.2460/ajvr.68.8.822. [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Koh D, Ong CN. Statistical evaluation of agreement between two methods for measuring a quantitative variable. Comput Biol Med. 1989;19:61–70. doi: 10.1016/0010-4825(89)90036-X. [DOI] [PubMed] [Google Scholar]
- 16.Lennon RI, Riyat MS, Hilliam R, Anathkrishnan G, Alderson G. Can a normal range of elbow movement predict a normal elbow x ray? Emerg Med J. 2007;24:86–88. doi: 10.1136/emj.2006.039792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.London JT. Kinematics of the elbow. J Bone Joint Surg Am. 1981;63:529–535. [PubMed] [Google Scholar]
- 18.Macedo LG, Magee DJ. Differences in range of motion between dominant and nondominant sides of upper and lower extremities. J Manipulative Physiol Ther. 2008;31:577–582. doi: 10.1016/j.jmpt.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Macedo LG, Magee DJ. Effects of age on passive range of motion of selected peripheral joints in healthy adult females. Physiother Theory Pract. 2009;25:145–164. doi: 10.1080/09593980802686870. [DOI] [PubMed] [Google Scholar]
- 20.Mayerson NH, Milano RA. Goniometric measurement reliability in physical medicine. Arch Phys Med Rehabil. 1984;65:92–94. [PubMed] [Google Scholar]
- 21.Morrey BF, Sanchez-Sotelo J. The Elbow and its Disorders. 4. Philadelphia, PA: Saunders Elsevier; 2008. [Google Scholar]
- 22.Paraskevas G, Papadopoulos A, Papaziogas B, Spanidou S, Argiriadou H, Gigis J. Study of the carrying angle of the human elbow joint in full extension: a morphometric analysis. Surg Radiol Anat. 2004;26:19–23. doi: 10.1007/s00276-003-0185-z. [DOI] [PubMed] [Google Scholar]
- 23.Park W, Ramachandran J, Weisman P, Jung ES. Obesity effect on male active joint range of motion. Ergonomics. 2010;53:102–108. doi: 10.1080/00140130903311617. [DOI] [PubMed] [Google Scholar]
- 24.Petherick M, Rheault W, Kimble S, Lechner C, Senear V. Concurrent validity and intertester reliability of universal and fluid-based goniometers for active elbow range of motion. Phys Ther. 1988;68:966–969. doi: 10.1093/ptj/68.6.966. [DOI] [PubMed] [Google Scholar]
- 25.Pique-Vidal C, Maled-Garcia I, Arabi-Moreno J, Vila J. Radiographic angles in hallux valgus: differences between measurements made manually and with a computerized program. Foot Ankle Int. 2006;27:175–180. doi: 10.1177/107110070602700304. [DOI] [PubMed] [Google Scholar]
- 26.Riddle DL, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting: shoulder measurements. Phys Ther. 1987;67:668–673. doi: 10.1093/ptj/67.5.668. [DOI] [PubMed] [Google Scholar]
- 27.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting: elbow and knee measurements. Phys Ther. 1983;63:1611–1615. doi: 10.1093/ptj/63.10.1611. [DOI] [PubMed] [Google Scholar]
- 28.Shaaban H, Pereira C, Williams R, Lees VC. The effect of elbow position on the range of supination and pronation of the forearm. J Hand Surg Eur Vol. 2008;33:3–8. doi: 10.1177/1753193407087862. [DOI] [PubMed] [Google Scholar]
- 29.Shiba R, Sorbie C, Siu DW, Bryant JT, Cooke TD, Wevers HW. Geometry of the humeroulnar joint. J Orthop Res. 1988;6:897–906. doi: 10.1002/jor.1100060614. [DOI] [PubMed] [Google Scholar]
- 30.Steindler A. Kinesiology of the Human Body Under Normal and Pathological Conditions. Ed 5. Springfield, IL: Charles C. Thomas; 1977. [Google Scholar]
- 31.Szulc P, Lewandowski J. Verification of selected anatomical landmarks used as reference points for universal goniometer positioning during elbow joint mobility range measurements. Folia Morphol (Warsz) 2003;62:353–355. [PubMed] [Google Scholar]
- 32.Terwee CB, Winter AF, Scholten RJ, Jans MP, Deville W, Schaardenburg D, Bouter LM. Interobserver reproducibility of the visual estimation of range of motion of the shoulder. Arch Phys Med Rehabil. 2005;86:1356–1361. doi: 10.1016/j.apmr.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 33.Pol RJ, Trijffel E, Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother. 2010;56:7–17. doi: 10.1016/S1836-9553(10)70049-7. [DOI] [PubMed] [Google Scholar]
- 34.Zampagni ML, Casino D, Zaffagnini S, Visani AA, Marcacci M. Estimating the elbow carrying angle with an electrogoniometer: acquisition of data and reliability of measurements. Orthopedics. 2008;31:370. doi: 10.3928/01477447-20080401-39. [DOI] [PubMed] [Google Scholar]