Abstract
Background
Stimulating growth in the shorter limb in patients with a lower limb length discrepancy (LLD) theoretically is a better alternative than retarding growth in the longer limb since it would not lead to loss of height. Periosteal stripping and/or division (PSPD) have been studied in animal models and in humans with encouraging results. We combined these procedures and used it to equalize lower limb length.
Surgical Technique
The procedure consists of total circumferential stripping followed by transverse division of the periosteum at the proximal, middle, and distal shafts of the femur, tibia, and fibula of the shorter limb.
Patients and Methods
We retrospectively reviewed 11 children with LLD who underwent PSPD. The average LLD was 6 ± 3.8 cm (range, 3–13 cm). The average age of the patients was 9 ± 2.5 years (range, 7–13 years). Orthoroentgenograms were obtained every 6 to 12 months after the surgery. The minimum followup was 24 months (mean, 52 months; range, 24–108 months).
Results
Limb length equalization (LLE) was achieved in eight of 11 patients in an average of 25 ± 17.2 months (range, 12–60 months) and was maintained throughout the followup. LLE was not achieved in three children whose discrepancy was greater than 10 cm, however, PSPD helped decrease the amount of the discrepancy in all three patients. No major complications were observed in any patients.
Conclusion
PSPD stimulates limb length and LLE is achieved in approximately 2 years after the procedure in the majority of the patients. We believe PSPD should be considered as a surgical option for a LLD up to 6 cm.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
LLD reportedly causes undesirable consequences including osteoarthritis of the hip [8], lower back pain [17], and gait asymmetry [12]. Several nonoperative and operative approaches are used to correct LLD including shoe lifts [15], retarding growth of the longer leg (ie, epiphyseal stapling) [1] or epiphysiodesis [9], and increasing the length of the shorter leg (ie, periosteal stimulation procedure) [2, 4, 11, 25] or distraction osteogenesis [5, 13]. Shortening procedures reduce overall height [1, 9] whereas lengthening procedures require extensive stretching with reported complications [16].
Stimulating growth of the shorter limb before reaching skeletal maturation is one alternative [2, 4, 11, 25] since it would not reduce height as would retarding growth of a longer limb (which is usually otherwise normal). Based on the report by Taylor et al., bone growth stimulation by periosteal stripping dates to the late 19th century [23]. The observations subsequently were reproduced in various animal models including chickens [3], dogs [22], lambs [19], monkeys [22], rabbits [6, 10], and rats [14], although the precise mechanisms which regulated the growth stimulation phenomenon are not completely understood [26]. Several hypotheses have been proposed to explain the growth stimulation including hypervascularization or release of the mechanical restraint after the periosteal stripping [2, 3]. In a chicken radius, a transverse periosteal resection has a similar growth-stimulating effect compared with the transverse osteotomy [3]. Several groups of investigators suggested releasing the mechanical restraint caused by the periosteal sleeve across the growth plate was the responsible mechanism [3, 23, 24].
Clinically, several studies have reported a modest improvement of LLD by using various surgical techniques [4, 11, 25]. Jenkins et al. [11] reported an improvement of approximately 1 cm after periosteal stripping alone. Wilde and Baker [25] and D’Souza and Shah [4] used the periosteal resection technique for treatment of minor LLD. To enhance the maximum potential for the growth stimulation effect, the combination of periosteal stripping and periosteal division procedures, we thought it was reasonable to combine the two procedures.
In this report we describe the PSPD procedure and our findings on LLE in a small number of patients in comparison to the results from previous clinical reports.
Surgical Technique
We measured lower limb lengths preoperatively by orthoroentgenogram. The indications for this technique were: (1) a LLD greater than 3 cm, and (2) radiographic confirmation of opening physes. The contraindications were: (1) a physeal bar formation, (2) joint contracture, and (3) unfavorable conditions of the soft tissue including extensive scars.
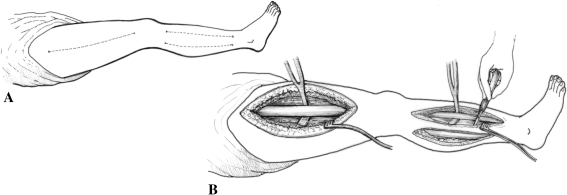
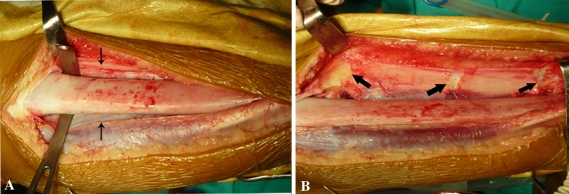
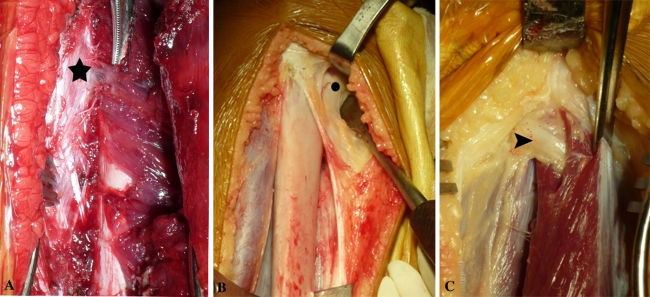
The planned surgical incisions (Fig. 1A) and technique of PSPD (Fig. 1B) are shown. The anterolateral subvastus lateralis approach was used to expose the femoral shaft from the greater trochanteric ridge to the distal femur just above the distal femoral growth plate. The periosteum was incised longitudinally and circumferentially stripped from the shaft completely. The periosteum division then was performed by three transverse cuts at the proximal, middle, and distal parts. An anterior approach was used for the tibia whereas the lateral approach through the peroneal muscles was used for the fibula. The periosteum stripping was completed using the same technique (Fig. 2A), and periosteal division was performed. The divided edges of the periosteum were retracted (Fig. 2B). Perforating branches of the profunda femoris artery were cauterized (Fig. 3A). The periosteum was divided just distal to the insertion of pes anserinus and the insertion should be left intact (Fig. 3B). The common peroneal nerve should be protected during exposure of the proximal fibula (Fig. 3C). The growth plates were left undisturbed. The wound was closed without drains. Each patient had a rigid dressing and long leg cast applied for 2 weeks. Progressive ambulation was restarted when the postoperative pain had diminished. The patients resumed regular activities after cast removal.
Fig. 1A–B.
(A) The broken lines show the skin incision for the PSPD procedures. Separate incisions were used to approach the shafts of the femur, tibia, and fibula. (B) Periosteal stripping was performed using a soft tissue retractor and a periosteal elevator. The periosteum was divided circumferentially using a scalpel.
Fig. 2A–B.
The intraoperative photographs show the PSPD procedures at the tibial shaft. (A) The thin arrows point to the edges of the periosteum after being circumferentially stripped from the tibial shaft. (B) The periosteum was divided transversely at the proximal, middle, and distal sections of the tibial shaft (thick arrows). Periosteal retraction is seen after periosteal division.
Fig. 3A–C.
(A) A perforating branch of the profunda femoris artery at the anterolateral compartment of the thigh can be seen (star). (B) The dot indicates insertion of the pes anserinus at the proximal tibia which is left intact. (C) A common peroneal nerve is shown (arrowhead).
Patients and Methods
We retrospectively reviewed all 11 patients (five females and six males) who underwent PSPD for LLD from January 2000 to December 2005. The average LLD preoperatively was 6 ± 3.8 cm (range, 3–13 cm) or 8% (range, 3%–14%) shorter than the longer limb. The average age of the patients was 9 ± 2.5 years (range, 5–13 years) at the time of the procedure. The underlying cause of LLD included hemihypertrophy (seven patients), posteromedial bowing of the leg (two patients), congenital absence of lateral toes associated with fibular hemimelia (one patient), and LLD secondary to synovial sarcoma resection and radiation at the knee (one patient). Their average followup was 52 ± 23.5 months (range, 24–108 months) and the average age at the final followup was 14 ± 1.67 years (range, 12–16 years) (Table 1). Clinical parameters including ROM and length difference of the lower limb were measured every 6 months during the first year, then every year until the LLE was achieved and/or skeletal maturation was reached. We obtained orthoroentgenograms using the same technique at each followup. One orthopaedic surgeon (NL) measured all the limb lengths on the orthoroentgenograms [18]. No patients were recalled specifically for this study. All data were obtained from medical records and radiographs. No patients were lost during followup and there were no missing radiographs. Complications were divided into major (ie, fracture, deep wound infection) and minor complications (ie, superficial wound infection, hematoma). The study was approved by the Institutional Review Board of our institution.
Table 1.
Preoperative and postoperative patient data
| Patient | Gender | Age at PSPD (years) | Preoperative LLD | Time to obtain LLE (months) | Latest followup | ||||
|---|---|---|---|---|---|---|---|---|---|
| Centimeters | % | Age (years) | Months | Centimeters | % | ||||
| 1 | Male | 11 | 3.7 | 2.7 | 24 | 12.5 | 30 | 0.6 | 0.5 |
| 2 | Male | 9 | 7.8 | 5.5 | 24 | 15 | 60 | 0.4 | 0.7 |
| 3 | Female | 10 | 3.5 | 4.9 | 36 | 14 | 48 | 1.8 | 2.2 |
| 4 | Female | 12.5 | 13.5 | 19.7 | No | 15.5 | 36 | 10.8 | 15.2 |
| 5 | Male | 8 | 3.5 | 5.7 | 12 | 13.5 | 66 | + 2.6 | + 3.2 |
| 6 | Female | 10 | 10.5 | 14.4 | No | 12 | 24 | 6.3 | 7.9 |
| 7 | Male | 7 | 3.5 | 6.2 | 12 | 12 | 66 | + 3 | + 3.7 |
| 8 | Female | 8 | 4 | 7.7 | 36 | 13 | 60 | + 0.2 | + 0.3 |
| 9 | Female | 7 | 6.3 | 9.4 | No | 11.5 | 42 | 4 | 5.5 |
| 10 | Male | 13 | 3.5 | 4.4 | 12 | 15 | 36 | 0.3 | 0.35 |
| 11 | Male | 5 | 3 | 5.0 | 6 | 16 | 108 | + 0.7 | + 0.8 |
PSPD = periosteal stripping and periosteal division; LLD = limb length discrepancy; LLE = limb length equalization; + indicates the surgically treated side is longer.
Results
LLE defined as less than 2 cm of LLD [15] was achieved in eight of the 11 patients after an average followup of 25 ± 17.2 months (range, 12–36 months) (Table 2). The LLE was maintained during the followup period in six patients. Two patients (Patients 5 and 7) experienced overstimulation of the surgically treated limb. For three patients (Patients 4, 6, and 9) whose preoperative LLD was greater than 6 cm (average, 10 cm), LLE was not achieved, however, all patients achieved a decrease in LLD before the discrepancy increased again during followup. The length gained from the PSPD was 2.7 cm for Patient 4, 4.2 cm for Patient 6, and 2.3 cm for Patient 9, respectively. Patients 4 and 6 reached skeletal maturity and subsequently underwent distraction osteogenesis. Patient 4 achieved correction of 10.8 cm of the LLD and Patient 6 achieved correction of 6.3 cm. Patient 9 was scheduled for a repeat PSPD.
Table 2.
LLD at each point of measurement
| Patient | LLD (centimeters) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Followup (months) | ||||||||||||
| 6 | 12 | 18 | 24 | 30 | 36 | 42 | 48 | 54 | 60 | 66 | 108 | ||
| 1 | 3.7 | 0.8 | 0.6 | ||||||||||
| 2 | 7.8 | 3.1 | 2.4 | 2.1 | 1 | 0.4 | |||||||
| 3 | 3.5 | 2.2 | 2.1 | 2.7 | 2.5 | 1.5 | 1.8 | ||||||
| 4 | 13.5 | 11.5 | 3.5 | 10.8 | |||||||||
| 5 | 3.5 | 2.2 | 1.1 | 0.7 | 0 | 1 | + 2 | + 2.6 | |||||
| 6 | 10.5 | 10.7 | 8.3 | 11 | 6.3 | ||||||||
| 7 | 3.5 | 0.2 | + 1.4 | + 2.8 | + 3.2 | + 3 | |||||||
| 8 | 4 | 3.1 | 2.7 | 3.2 | 2 | + 0.5 | + 0.2 | ||||||
| 9 | 6.3 | 5.8 | 5.8 | 5.1 | 3 | 4 | |||||||
| 10 | 3.5 | 2 | 1.3 | 0.3 | |||||||||
| 11 | 3 | 1.1 | 0.1 | 0.7 | + 0.7 | ||||||||
LLD = limb length discrepancy; + indicates the surgically treated side is longer.
One superficial wound infection occurred. Rather than thinning of the cortex, cortical hypertrophy of the diaphysis on the surgical limb was observed on the postoperative orthoroentgenogram of every patient (Fig. 4).
Fig. 4.

Cortical thickening (curved arrows) at the tibial and fibular diaphysis is seen after PSPD.
Discussion
Stimulating growth of a shorter leg is a more appealing option than retarding growth of a longer leg if skeletal maturation has not been reached. In clinical studies investigating the utility of either periosteal stripping alone or periosteal division at the growth plate, only modest improvements in LLD were observed [4, 11, 25]. We therefore developed an approach using a combination of periosteal stripping and division and describe our findings.
Our study has a few limitations. First, although the growth stimulation by our technique is anticipated in all cases, the number of patients is small. We have encountered relatively few patients in whom we believed the procedure was indicated. Second, the findings are reported in some patients before their skeletal maturity.
Several periosteal intervention techniques have been explored in animal models and resulted in an increase in bone length (Table 3). In one report the effects of periosteal intervention were the greatest when the periosteum was divided in a circular fashion in addition to periosteal stripping [24]. The authors suggested vascular and/or mechanical effects explained the growth stimulation phenomenon after periosteal interventions [24]. The vascular theory is consistent with the well-established phenomenon of bone overgrowth observed in children after femoral shaft fractures [20]. The regional blood supply to the femoral shaft must be diverted from other sources in addition to that from the periosteum, leading to hyperemia associated with an increase in the bone growth rate [14, 21, 22]. However, the vascular theory alone cannot entirely explain the growth stimulation phenomenon: Crilly [3] found that the longitudinal incision of the periosteum, which disturbed its blood supply, caused few effects on bone growth whereas the transverse section of the periosteum did. Mechanical restraint of the growth plate also could explain the retardation of growth. Several authors have suggested release of the periosteal restraining effect was responsible for an increase in the bone growth rate [3, 23, 24]. We observed immediate retraction of the periosteum after it was divided indicating that the periosteum was constantly under tension (Fig. 2B). The molecular regulation of bone growth stimulation by periosteal stripping is not completely understood. The proliferation rate of the chondrocytes in the proliferative zone and the rate of ossification at the epiphysiometaphyseal junction increase after periosteal stripping, whereas the height of the hypertrophic zone remains constant [23]. However, Sansone et al. [19] reported that the chondrocytes in the hypertrophic zone elongate in an axial manner and have a net effect of growth acceleration owing to reduction of axial compression at the growth plate.
Table 3.
Types of periosteal intervention and results in animal studies
| Study | Animal | Bones | Number of subjects | Periosteal interventions | Locations | Measurement | Duration | Results | Remarks |
|---|---|---|---|---|---|---|---|---|---|
| Sola et al. [22] | Dog | Thigh and leg | 15 | One circumferential stripping | Whole shaft of bone | Difference in growth compared with the other side | 12 months | 0.16 ± 0.03 cm | |
| 22 | Two circumferential strippings at 1–2-months interval | 0.61 ± 0.15 cm | Fracture after second procedure | ||||||
| Monkey | Thigh and leg | 10 | Two circumferential strippings at 2-months interval | 0.17 ± 0.03 cm | |||||
| Crilly [3] | Chicken | Radius | 24 | Transverse section of the periosteum | Distal end—16 Proximal end—8 | Percentage of overgrowth | 120 days | 5.7% | Overgrowth similar to that of fracture of the chicken radius |
| 23 | Longitudinal incision of the periosteum | Distal end—15 Proximal end—8 | 0% | ||||||
| Houghton & Rooker [10] | Rabbit | Tibia | 24 | Hemicircumferential division of the periosteum | Medial upper tibia | Proximal growth plate and tibia shaft angle | 8 weeks | Increase in valgus angulation | |
| Warrell & Taylor [24] | Rat | Tibia | 10 | Circular division | Distal tibia | Difference in growth compared with the other side | 34 days | 0.41 mm | |
| 10 | Circular division plus periosteal stripping | 0.69 mm | Greatest difference in this study | ||||||
| 10 | Vertical periosteal division | 0.03 mm | |||||||
| 10 | Vertical periosteal division plus periosteal stripping | 0.45 mm | |||||||
| Taylor et al. [23] | Rat | Tibia | 16 | Circumferential incision and stripping | Distal tibia | Difference in growth compared with the other side | 35 days | 0.38 mm (1%) | |
| Histologic measurement | Increase labelling index for nucleated cell in the proliferative zone and number of hypertrophic cells | ||||||||
| Lynch et al. [14] | Rat | Tibia | 10 | Circumferential division | Proximal tibia | Difference in growth at the proximal tibia compared with the other side | 21 days | 0.70 mm (23%) | |
| 10 | Distal tibia | 0.22 mm (7%) | |||||||
| 10 | Stripping of periosteum | Whole shaft of bone | 0.5 mm (15%) |
Several clinical reports (Table 4) support the use of periosteal intervention involving either periosteal stripping from the whole shaft [2, 11] or circumferential excision of a cuff of periosteum adjacent to the growth plate [7, 25]. The average preoperative LLD was 3 to 4 cm in these patient cohorts. To maximize the bone growth stimulation effect, we suggest that the periosteum should be stripped circumferentially from the whole diaphysis and divided transversely at the proximal, middle, and distal parts of the femur, tibia, and fibula to diminish the tethering effect of the periosteum on the growth plate. We were able to equalize the lower limb length in patients with as much as 6 cm of LLD.
Table 4.
Comparison of results between periosteal intervention techniques
| Study | Number of patients | Age Mean/ (range) | Underlying conditions of LLD | Periosteal intervention | Measurement | Preoperative LLD mean (range) | Results mean (range) | Duration of followup mean (range) | Complications | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| Chan et al. [2] | 45 | 5–12 years | Poliomyelitis | Complete stripping of the periosteum from the whole shaft of the femur and tibia | Amount of overgrowth | 3.3 (1.1–9.5) cm | 1.3 (0.6–4.4) cm overgrowth—31 patients | 1 ± 3 years (3 months to 7 years) | Superficial wound infection—1 Chilblains—3 | 1) 8 years old is the best age for surgery |
| Within ± 0.4 cm— 9 patients | ||||||||||
| Not improved—5 patients | ||||||||||
| Jenkins et al. [11] | 30 | 6–15 years | Poliomyelitis | Similar to that of Chan et al. [2] | Increase in length relative to the other side | 3.2 (1.0–9.1) cm | 1.3 (0.3–4.2) cm— 17 femurs | 5 years | Superficial wound infection—1 | 1) No result regarding the patient who achieved limb equalization |
| Not improved—11 femurs | 2) Ankle valgus in 18/26 patients. (The procedure was not performed on the fibula.) | |||||||||
| 1.14 (0.2–5.1) cm—17 tibias | ||||||||||
| Not improved—9 tibias | ||||||||||
| Wilde et al. [25] | 38 | 15 months – 13.5 years | Fibular hypoplasia—15 Whole body asymmetry—5 Femoral hypoplasia—3 Osteomyelitis—3 PFFD—3 CDH with upper femoral growth arrest—2 Multiple hemangiomas—1 Unknown—6 | Excise a 0.5-cm cuff of periosteum circumferentially at the distal femoral, tibial, and fibular metaphyses | Mean difference in leg length | 3.8 (1.8–9.2) cm (7.24%) | 5.45% | 32 months | Superficial wound infection—1 Small hematoma—1 | No result regarding the patient who achieved limb equalization |
| Edwards et al. [7] | 10 | 4 years | Achondroplasia | Circumferential division and 2 cm stripping of the periosteum at the distal femur and proximal tibia | Increase in length | N/A | 4.9 ± 1.7 mm (2%) | 2 years | None | |
| D’Souza et al. [4] | 23 | 8.5 (6–12) years | Poliomyelitis | Excise a 1-cm cuff of periosteum circumferentially at the distal femoral, tibial and fibular metaphysis | Percentage of length discrepancy | 3.5 (2.5–8.7) cm (6.53 ± 2.43%) | 1.2 ± 0.9% | 2 years | None | 13 patients reached skeletal maturity with a mean of 0.3 (0.2–0.7) cm of LLD |
| Limb length gain | 4.33 cm | 1 year | ||||||||
| Current study | 11 | 9 (7–13) years | Hemihypertrophy—7 Posteromedial bowing of tibia—2 Congenital absence of lateral toe—1 Secondary to synovial sarcoma treatment—1 | Total periosteal stripping of the periosteum and periosteal division at 3 sites of the femur, tibia and fibula | Amount of leg length different | 3–13 (6) cm | 8 patients achieved LLE within 2 cm range | 52 (24–108) months | Overstimulation-2 |
LLD = limb-length discrepancy; PFFD = proximal femoral focal deficiency; CDH = congenital dislocation of the hip; N/A = not available.
D’Souza and Shah suggested the most appropriate age for patients to undergo PSPD was at the beginning of puberty to allow for enough remaining time for the discrepancy to be corrected [4]. This could be determined by the chronologic age [2]. We found bone growth stimulation by PSPD lasted 3 to 5 years, which is similar to times reported in several studies [4, 11, 25].
The complication rates associated with the procedure are low [2, 4, 22]. A pathologic fracture after periosteal intervention was reported in an animal model [21, 22]. However, none of our patients experienced a fracture. We observed cortical hypertrophy of the diaphysis on the orthoroentgenogram as a result of subperiosteal new bone formation [26]. This shows that the vascular supply to the bone essentially is preserved [2, 21]. Another complication was bone overgrowth when the surgically treated limb became longer than the contralateral limb by greater than 2 cm. The predictability of this procedure and characteristics of the patients undergoing bone growth stimulation need further investigation. Although only partial correction of LLD could be achieved when PSPD was performed when the degree of the LLD was greater than 10 cm or around the time of skeletal maturation, we still considered PSPD the preferred treatment. The second stripping procedure could be performed 3 to 5 years after the first operation [25] or at the beginning of the secondary growth spurt [4], although the incidence of pathologic fractures might be increased [22]. The second lengthening procedure performed at the time of skeletal maturation is relatively less extensive. No adverse effects on subsequent distraction osteogenesis were seen in our two patients [13, 21].
We believe PSPD is a practical method for correcting LLD, with few complications. The technique requires simple surgical skills and equipment. The majority of our patients achieved LLE, and evidence of bone growth stimulation was observed in every patient. The patients required a short hospitalization and they resumed normal activities on discharge. PSPD did not interfere with possible subsequent operations.
Acknowledgment
We thank Matthew B. Dobbs MD for his contributions to this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling: a preliminary report. J Bone Joint Surg Am. 1949;31:464–478. [PubMed] [Google Scholar]
- 2.Chan KP, Hodgson AR. Physiologic leg lengthening: a preliminary report. Clin Orthop Relat Res. 1970;68:55–62. doi: 10.1097/00003086-197001000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Crilly RG. Longitudinal overgrowth of chicken radius. J Anat. 1972;112:11–18. [PMC free article] [PubMed] [Google Scholar]
- 4.D’Souza H, Shah NM. Circumferential periosteal sleeve resection: results in limb-length discrepancy secondary to poliomyelitis. J Pediatr Orthop. 1999;19:215–221. doi: 10.1097/00004694-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis) J Pediatr Orthop. 1987;7:129–134. doi: 10.1097/01241398-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Dimitriou CG, Kapetanos GA, Symeonides PP. The effect of partial periosteal division on growth of the long bones: an experimental study in rabbits. Clin Orthop Relat Res. 1988;236:265–269. [PubMed] [Google Scholar]
- 7.Edwards DJ, Bickerstaff DB, Bell MJ. Periosteal stripping in achondroplastic children: little effect on limb length in 10 cases. Acta Orthop Scand. 1994;65:333–334. doi: 10.3109/17453679408995464. [DOI] [PubMed] [Google Scholar]
- 8.Gofton JP, Trueman GE. Studies in osteoarthritis of the hip: II. Osteoarthritis of the hip and leg-length disparity. Can Med Assoc J. 1971;104:791–799. [PMC free article] [PubMed] [Google Scholar]
- 9.Green WT, Anderson M. Experiences with epiphyseal arrest in correcting discrepancies in length of the lower extremities in infantile paralysis: a method of predicting the effect. J Bone Joint Surg Am. 1947;29:659–675. [PubMed] [Google Scholar]
- 10.Houghton GR, Rooker GD. The role of the periosteum in the growth of long bones: an experimental study in the rabbit. J Bone Joint Surg Br. 1979;61:218–220. doi: 10.1302/0301-620X.61B2.438275. [DOI] [PubMed] [Google Scholar]
- 11.Jenkins DH, Cheng DH, Hodgson AR. Stimulation of bone growth by periosteal stripping: a clinical study. J Bone Joint Surg Br. 1975;57:482–484. [PubMed] [Google Scholar]
- 12.Kaufman KR, Miller LS, Sutherland DH. Gait asymmetry in patients with limb-length inequality. J Pediatr Orthop. 1996;16:144–150. doi: 10.1097/01241398-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Kawamura B, Hosono S, Takahashi T, Yano T, Kobayashi Y, Shibata N, Shinoda Y. Limb lengthening by means of subcutaneous osteotomy: experimental and clinical studies. J Bone Joint Surg Am. 1968;50:851–878. [PubMed] [Google Scholar]
- 14.Lynch MC, Taylor JF. Periosteal division and longitudinal growth in the tibia of the rat. J Bone Joint Surg Br. 1987;69:812–816. doi: 10.1302/0301-620X.69B5.3680349. [DOI] [PubMed] [Google Scholar]
- 15.Moseley C. Leg-length discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics. Ed 6. Philadelphia, PA: Lippincott William & Wilkins; 2005:1213–1256.
- 16.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 17.Rush WA, Steiner HA. A study of lower extremity length inequality. Am J Roentgenol Radius Ther. 1946;56:616–623. [PubMed] [Google Scholar]
- 18.Sabharwal S, Zhao C, McKeon J, Melaghari T, Blacksin M, Wenekor C. Reliability analysis for radiographic measurement of limb length discrepancy: full-length standing anteroposterior radiograph versus scanogram. J Pediatr Orthop. 2007;27:46–50. doi: 10.1097/01.bpo.0000242444.26929.9f. [DOI] [PubMed] [Google Scholar]
- 19.Sansone JM, Wilsman NJ, Leiferman EM, Noonan KJ. The effect of periosteal resection on tibial growth velocity measured by microtransducer technology in lambs. J Pediatr Orthop. 2009;29:61–67. doi: 10.1097/BPO.0b013e3181929c71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shapiro F. Fractures of the femoral shaft in children: the overgrowth phenomenon. Acta Orthop Scand. 1981;52:649–655. doi: 10.3109/17453678108992162. [DOI] [PubMed] [Google Scholar]
- 21.Silberman FS, Sola CK, Cabrini RL. A study of the vascular distribution after periosteal stripping of the long bones. Surg Gynecol Obstet. 1967;125:1311–1315. [PubMed] [Google Scholar]
- 22.Sola CK, Silberman FS, Cabrini RL. Stimulation of the longitudinal growth of long bones by periosteal stripping: an experimental study on dogs and monkeys. J Bone Joint Surg Am. 1963;45:1679–1684. [PubMed] [Google Scholar]
- 23.Taylor JF, Warrell E, Evans RA. The response of the rat tibial growth plates to distal periosteal division. J Anat. 1987;151:221–231. [PMC free article] [PubMed] [Google Scholar]
- 24.Warrell E, Taylor JF. The role of periosteal tension in the growth of long bones. J Anat. 1979;128:179–184. [PMC free article] [PubMed] [Google Scholar]
- 25.Wilde GP, Baker GC. Circumferential periosteal release in the treatment of children with leg-length inequality. J Bone Joint Surg Br. 1987;69:817–821. doi: 10.1302/0301-620X.69B5.3680350. [DOI] [PubMed] [Google Scholar]
- 26.Wu YK, Miltner LJ. A procedure for stimulation of longitudinal growth of bone: an experimental study. J Bone Joint Surg Am. 1937;19:909–921. [Google Scholar]