Abstract
Background
Muscle strains are one of the most common complaints treated by physicians. High-force lengthening contractions can produce very high forces resulting in pain and tissue damage; such strains are the most common cause of muscle injuries. The hamstring muscles are particularly susceptible as they cross two joints and regularly perform lengthening contractions during running. We describe a patient with return to full function after a large hamstring tear.
Case Description
We report the case of a 26-year-old man who presented 1 year after a noncontact, left-sided proximal hamstring tear incurred while sprinting. He received no medical treatment or formal rehabilitation. He was able to return to all sports and activities 1 to 2 months after injury, but noted a persistent deformity of the proximal thigh, which led him to seek evaluation. Physical examination, MRI functional tests, and specific muscle tests 1 year after his injury documented a major hamstring tear at the musculotendinous junction with muscle retraction, but no avulsion of the proximal tendon attachment.
Literature Review
Surgery often is recommended for major proximal hamstring tendon tears, especially when more than one tendon of origin is ruptured from the ischial tuberosity. Myotendinous tears are treated nonoperatively, but may be associated with decreased strength, prolonged recovery, and recurrence.
Purpose and Clinical Relevance
We describe the case of a young man who sustained a hamstring tear, with retraction, at the proximal myotendinous junction, where the biceps femoris and semitendinosus arise from the conjoint tendon. He achieved full functional recovery without medical attention, but had a persistent cosmetic deformity and slight hamstring tightness. This case suggests a benign natural history for this injury and the appropriateness of noninvasive treatment.
Introduction
Force generated during the contraction of skeletal muscle cells, or myofibers, ultimately is transmitted to the tendons at either end of the muscle. Submaximal contractions are used in everyday life, but high-force eccentric (lengthening) contractions, such as in the hamstring muscles during sprinting, are associated with muscle damage and pain [18, 27, 37]. The majority of hamstring musculotendinous injuries occur during maximum sprinting when braking knee extension or at foot strike [7], whereas most proximal hamstring avulsions occur during forced hip flexion and knee extension, such as with a fall during waterskiing [9, 20]. In one kinematic and electromyographic study late swing phase during sprinting correlated with the point of maximum hamstring muscle contraction and lengthening [40, 45].
The force generated during a maximal lengthening contraction is approximately twofold the force developed during a maximal isometric contraction [11]. The increase in force production during eccentric contraction may be sufficient to cause failure of the muscle-tendon complex. Insufficient warmup, lack of flexibility, inadequate muscle strength and endurance, and altered running form have been implicated as predisposing factors to hamstring injury [2]. Proximally, the semitendinosus and biceps are at the highest risk for injury owing to the pennation angle of their myofibers attaching to the common tendon of the hamstring complex [2]. The force generated by muscle is transmitted not only longitudinally along the axis of the muscle, but also radially to nearby muscles [17, 34, 38]. This altered pathway to transmit force to and along nearby muscles could minimize any functional deficits that would be detected if an injured muscle were tested in isolation instead of as part of a functional complex [4, 17, 32, 41].
Nonsurgical management is the standard of care for myotendinous injuries [29], although the required rehabilitation can be protracted from 6 to 50 months [16]. Tests that measure strength, ROM, and pain can provide a reasonable estimate of rehabilitation duration in injuries involving the intramuscular tendon and adjacent muscle fibers [39, 43]. However, for injuries to the proximal free tendon, the amount of impairment identified from these tests does not predict the recovery time needed to return to preinjury level [16].
Tears of the proximal hamstring tendons can be addressed surgically [22]. Surgeons are more likely to recommend repair of proximal hamstring-origin complete avulsions because of the risk for tendon retraction and progressive functional impairment with time [29], whereas the majority of hamstring muscle injuries respond well to nonoperative treatment [5, 36]. In a review of hamstring injuries, Linklater et al. [29] note that “proximal hamstring avulsions are of particular importance because of the substantially improved outcome with early surgical repair”. They also note that, without proper imaging, it can be difficult clinically to distinguish origin avulsions from muscle-tendon junction injury. Certainly hamstring retraction can contribute to sciatic nerve involvement and long-term weakness and make later repair more challenging [5]. The patient in this case report had a major hamstring tear at the musculotendinous junction with muscle retraction, but no avulsion of the proximal tendon attachment.
Case Report
A 26-year-old man complained of a visible and palpable defect in his left posterior thigh. He reported suffering a “pulled hamstring” 1 year previously during a touch football game. He removed himself from the game and treated himself with rest (approximately 1 week) and only occasional, low-dose NSAIDs before making a gradual return to sports. He had an antalgic gait for approximately 3 weeks after the injury. He had no medical evaluation at the time and no formal treatment or rehabilitation. By 1 to 2 months postinjury, he was able to return to all leisure activities and competitive sports that he participated in before his injury. He had occasional soreness after vigorous activity that lasted several hours, which was slightly greater than the soreness experienced in the contralateral extremity after these activities. The patient denied paresthesia, radiating pain, or any difficulty with gait. His medical history and review of systems were negative. There is no history of prior lower extremity injury.
The patient had a normal gait. There was a visible defect in the left proximal hamstring approximately 10 cm in length and 4 to 5 cm in width, and visible ‘balling’ of the proximal muscle tissue and depression inferior to the ischial tuberosity with active knee flexion (Fig. 1). No point tenderness was identified and no weakness was detected with manual muscle tests, which included handheld dynamometry to test hip and knee actions. The patient had full ROM in the spine and at the hips and knees. Height of the straight leg raise was equal bilaterally and did not induce complaint. Although the straight leg raise can be used to measure hamstring length, some have suggested that the passive knee extension method (popliteal angle) of measurement is more accurate [33]. With the hip held at 90° flexion, the popliteal angle was measured with a goniometer to gauge hamstring muscle tightness [44]. The popliteal angle was 23° on the involved side and 5° on the opposite extremity, consistent with slight hamstring tightness on the involved side. The Thomas Test was positive for iliopsoas tightness on the left, but the Ober test was negative bilaterally. The patient was able to perform deep squats and heel/toe raises without difficulty or discomfort. Single-leg stance was equal bilaterally for stability/time.
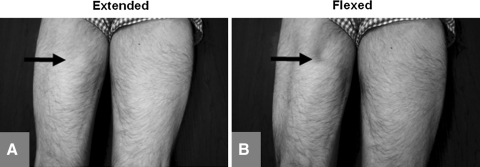
Fig. 1A–B.
The photographs show a posterior view of the thighs with the patient in the prone position. (A) When the patient was examined in the prone or standing position with the knee extended, the left hamstrings had a normal appearance compared to the opposite side. For orientation, the arrow corresponds to the area of the defect in the next image. (B) When the patient was examined in the prone or standing position with the knee flexed, the defect was clearly visible (arrow), but only with active, not passive, flexion.
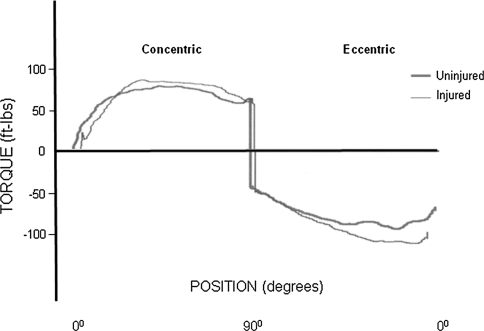
A Biodex dynamometer (Biodex Medical Systems Inc, Shirley, NY, USA) is a reliable tool to measure force [12, 35]. This instrument was used to record right and left knee extension and flexion torque during maximal voluntary shortening and lengthening contractions. After appropriate warmup and acclimatization to the isokinetic testing equipment, the subject performed two sets of 10 maximal repetitions for testing. The recorded measurements were highly reliable and there were no differences in peak torque, rise time (time to peak torque), or total work between the right and left quadriceps and hamstring muscles (Fig. 2). The only loss in maximal torque was at approximately 30° for concentric (shortening) and eccentric (lengthening) contractions (12% and 16%, respectively). Although we did not specifically measure fatigue, there were no differences from right to left in the amount of total work performed by the quadriceps during the course of testing.
Fig. 2.
A representative trace recording of maximal hamstring shortening (concentric) and lengthening (eccentric) contraction through a 90° arc of motion is shown. The thicker line represents the uninvolved extremity (right leg) and the thinner line represents the involved side (left leg). The strength for the injured hamstrings was relatively normal (quadriceps trace recording not shown as no differences were found).
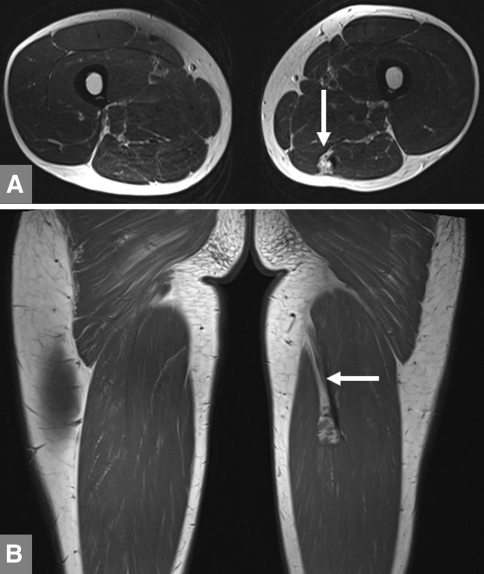
T2-weighted rapid acquisition relaxation-enhanced (RARE) MR images were acquired using a 3-Tesla magnetic resonance system (Magnetom Trio, Siemens Medical Solutions, Erlangen, Germany). The parameters were: FOV = 380 mm, TR = 600 ms, TE = 20 ms, voxel size = 0.9375 × 0.9375 × 3.0 mm, matrix size = 256 × 256. MRI revealed a large tear in the hamstrings (Fig. 3), specifically a 2-cm by 8-cm tear where the biceps femoris and semitendinosus muscles originate from the conjoint tendon.
Fig. 3A–B.
(A) A T1-weighted MR image in the transverse (axial) plane shows a clearly visible tear where the biceps femoris and semitendinosus muscles originate from the conjoint tendon (arrow). (B) In this frontal (coronal) MRI slice through the thigh, the injury is clearly visible (arrow).
Discussion
Muscle strains are one of the most common complaints treated by physicians [13, 21] and account for the majority of all sports-related injuries [8]. Except for complete ruptures of muscles, displaced avulsions, and recalcitrant symptoms from myositis ossificans, almost all muscle injuries are treated uniformly with nonoperative therapy [13, 19, 28, 31]. Standard nonoperative therapy for acute muscle injuries usually involves rest, ice, compression, and elevation (RICE). Although experimental therapies such as platelet-rich plasma [15], suramin [6], and other such agents [14, 30, 42] are being tested, there is no clear consensus on nonoperative treatment of muscle injuries beyond the principle of short-term rest and ice.
Muscle injury can be established from the history and physical examination. The amount of impairment in strength measurement, ROM, and the level of pain reportedly predict the approximate duration of rehabilitation [43]. To a certain extent, muscle has the ability to regenerate and repair itself, most muscle injuries are self-limiting, and recovery occurs spontaneously.
Hamstring strains are one of the most common muscle injuries and the majority are treated nonoperatively [9]. It is not known why some people sustain hamstring injuries while others performing the same activity do not. Previously injured players have more than twice as great a risk of sustaining a new hamstring injury [10]. Almost 1/3 of these injuries recur within the first year after a return to sports, with subsequent injuries being more severe than the original injury [16]. Our patient at 1 year after injury had no recurrence despite participating at the same level of sport. The natural history of large untreated myotendinous tears is not well documented in the literature. Nonoperative treatment usually results in preinjury long-term function, with a higher risk of subsequent injury [1, 43]. In contrast to the literature on surgical treatment of hamstring avulsions, we found no clinical studies or reports regarding surgical treatment of hamstring myotendinous injuries.
Aside from the visible deformity and slight hamstring tightness, our patient had no major complaints or measurable functional deficits. It may be that, given the size of the hamstring muscle group, even large tears can be compensated for by the remaining hamstring complex without substantial strength deficit or functional limitation. In this case, isokinetic testing revealed virtually no difference in strength in this patient and functional testing was negative. The hamstring tear appears to have involved muscle attachments at the conjoint tendon, where injury is more likely owing to the pennation angle of the muscle fiber attachment. The remaining muscles of the hamstring complex have remained intact. This case report may show that the hamstrings function as a complex, and loss of one component of that complex does not preclude long-term recovery and return to athletic activity.
MRI has high sensitivity to detect the hemorrhage and edema that follow muscle injuries. This, together with the capability to evaluate multiple anatomic planes, make it the most suitable technique to evaluate muscle injures [23–26]. Most muscle injuries might not require imaging, but as this noninvasive technology continues to improve and becomes even more commonplace, it can play a role in rehabilitation planning and prognosis [3]. Muscle strains are revealed best by T2-weighted images, which optimize contrast between injured muscles with edema (increased signal intensity) and normal uninjured muscles.
Hamstring muscle strains, particularly musculotendinous injuries, are quite common and often are treated with nonoperative care and rehabilitation. We conclude that the resulting deformity that led our patient to present is purely cosmetic, as it has had no apparent functional consequence. This patient returned to full activities without the need for protracted rehabilitation that sometimes is necessary.
Acknowledgments
This work was supported by grants to RML from the National Institutes of Health (K01AR053235 and 1R01AR059179).
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40:40–44. doi: 10.1136/bjsm.2005.018879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bencardino JT, Mellado JM. Hamstring injuries of the hip. Magn Reson Imaging Clin N Am. 2005;13:677–690, vi. [DOI] [PubMed]
- 3.Blankenbaker DG, Smet AA. MR imaging of muscle injuries. Appl Radiol. 2004;33:14–26. [Google Scholar]
- 4.Bloch RJ, Gonzalez-Serratos H. Lateral force transmission across costameres in skeletal muscle. Exerc Sport Sci Rev. 2003;31:73–78. doi: 10.1097/00003677-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Carmichael J, Packham I, Trikha SP, Wood DG. Avulsion of the proximal hamstring origin: surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2):249–256. doi: 10.2106/JBJS.I.00382. [DOI] [PubMed] [Google Scholar]
- 6.Chan YS, Li Y, Foster W, Fu FH, Huard J. The use of suramin, an antifibrotic agent, to improve muscle recovery after strain injury. Am J Sports Med. 2005;33:43–51. doi: 10.1177/0363546504265190. [DOI] [PubMed] [Google Scholar]
- 7.Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Med Sci Sports Exerc. 2011;43:525–532. doi: 10.1249/MSS.0b013e3181f23fe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ciullo JV, Zarins B. Biomechanics of the musculotendinous unit: relation to athletic performance and injury. Clin Sports Med. 1983;2:71–86. [PubMed] [Google Scholar]
- 9.Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–355. doi: 10.5435/00124635-200706000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38:1147–1153. doi: 10.1177/0363546509358381. [DOI] [PubMed] [Google Scholar]
- 11.Faulkner JA, Brooks SV, Opiteck JA. Injury to skeletal muscle fibers during contractions: conditions of occurrence and prevention. Phys Ther. 1993;73:911–921. doi: 10.1093/ptj/73.12.911. [DOI] [PubMed] [Google Scholar]
- 12.Feiring DC, Ellenbecker TS, Derscheid GL. Test-retest reliability of the biodex isokinetic dynamometer. J Orthop Sports Phys Ther. 1990;11:298–300. doi: 10.2519/jospt.1990.11.7.298. [DOI] [PubMed] [Google Scholar]
- 13.Garrett WE., Jr Muscle strain injuries. Am J Sports Med. 1996;24(6 suppl):S2–S8. [PubMed] [Google Scholar]
- 14.Gauldie J, Bonniaud P, Sime P, Ask K, Kolb M. TGF-beta, Smad3 and the process of progressive fibrosis. Biochem Soc Trans. 2007;35:661–664. doi: 10.1042/BST0350661. [DOI] [PubMed] [Google Scholar]
- 15.Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37:1135–1142. doi: 10.1177/0363546508330974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40:67–81. doi: 10.2519/jospt.2010.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huijing PA, Baan GC. Myofascial force transmission causes interaction between adjacent muscles and connective tissue: effects of blunt dissection and compartmental fasciotomy on length force characteristics of rat extensor digitorum longus muscle. Arch Physiol Biochem. 2001;109:97–109. doi: 10.1076/apab.109.2.97.4269. [DOI] [PubMed] [Google Scholar]
- 18.Hunter KD, Faulkner JA. Pliometric contraction-induced injury of mouse skeletal muscle: effect of initial length. J Appl Physiol. 1997;82:278–283. doi: 10.1152/jappl.1997.82.1.278. [DOI] [PubMed] [Google Scholar]
- 19.Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33:745–764. doi: 10.1177/0363546505274714. [DOI] [PubMed] [Google Scholar]
- 20.Jonhagen S, Ericson MO, Nemeth G, Eriksson E. Amplitude and timing of electromyographic activity during sprinting. Scand J Med Sci Sports. 1996;6:15–21. doi: 10.1111/j.1600-0838.1996.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 21.Kirkendall DT, Garrett WE., Jr Clinical perspectives regarding eccentric muscle injury. Clin Orthop Relat Res. 2002;403(suppl):S81–S89. doi: 10.1097/00003086-200210001-00010. [DOI] [PubMed] [Google Scholar]
- 22.Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34:119–123. doi: 10.1007/s00264-009-0739-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–589. doi: 10.1007/s00256-003-0674-5. [DOI] [PubMed] [Google Scholar]
- 24.Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005;25:571–586. doi: 10.1148/rg.253045711. [DOI] [PubMed] [Google Scholar]
- 25.Koulouris G, Connell D. Imaging of hamstring injuries: therapeutic implications. Eur Radiol. 2006;16:1478–1487. doi: 10.1007/s00330-005-0075-3. [DOI] [PubMed] [Google Scholar]
- 26.Koulouris G, Connell DA, Brukner P, Schneider-Kolsky M. Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med. 2007;35:1500–1506. doi: 10.1177/0363546507301258. [DOI] [PubMed] [Google Scholar]
- 27.LaStayo PC, Woolf JM, Lewek MD, Snyder-Mackler L, Reich T, Lindstedt SL. Eccentric muscle contractions: their contribution to injury, prevention, rehabilitation, and sport. J Orthop Sports Phys Ther. 2003;33:557–571. doi: 10.1016/S8756-3282(03)00249-7. [DOI] [PubMed] [Google Scholar]
- 28.Lehto MU, Jarvinen MJ. Muscle injuries, their healing process and treatment. Ann Chir Gynaecol. 1991;80:102–108. [PubMed] [Google Scholar]
- 29.Linklater JM, Hamilton B, Carmichael J, Orchard J, Wood DG. Hamstring injuries: anatomy, imaging, and intervention. Semin Musculoskelet Radiol. 2010;14:131–161. doi: 10.1055/s-0030-1253157. [DOI] [PubMed] [Google Scholar]
- 30.Menetrey J, Kasemkijwattana C, Day CS, Bosch P, Vogt M, Fu FH, Moreland MS, Huard J. Growth factors improve muscle healing in vivo. J Bone Joint Surg Br. 2000;82:131–137. doi: 10.1302/0301-620X.82B1.8954. [DOI] [PubMed] [Google Scholar]
- 31.Noonan TJ, Garrett WE., Jr Muscle strain injury: diagnosis and treatment. J Am Acad Orthop Surg. 1999;7:262–269. doi: 10.5435/00124635-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Patel TJ, Lieber RL. Force transmission in skeletal muscle: from actomyosin to external tendons. Exerc Sport Sci Rev. 1997;25:321–363. doi: 10.1249/00003677-199700250-00014. [DOI] [PubMed] [Google Scholar]
- 33.Rakos DM, Shaw KA, Fedor RL, Lamanna M, Yocum CC, Lawrence KJ. Interrater reliability of the active-knee-extension test for hamstring length in school-aged children. Pediatr Phys Ther. 2001;13:37–41. doi: 10.1097/00001577-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Ramaswamy KS, Palmer ML, Meulen JH, Renoux A, Kostrominova TY, Michele DE, Faulkner JA. Lateral transmission of force is impaired in skeletal muscles of dystrophic mice and very old rats. J Physiol. 2011;589:1195–1208. doi: 10.1113/jphysiol.2010.201921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saenz A, Avellanet M, Hijos E, Chaler J, Garreta R, Pujol E, Sandoval B, Buen C, Farreny A. Knee isokinetic test-retest: a multicentre knee isokinetic test-retest study of a fatigue protocol. Eur J Phys Rehabil Med. 2010;46:81–88. [PubMed] [Google Scholar]
- 36.Sallay PI, Ballard G, Hamersly S, Schrader M. Subjective and functional outcomes following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31:1092. doi: 10.3928/01477447-20081101-26. [DOI] [PubMed] [Google Scholar]
- 37.Schneider-Kolsky ME, Hoving JL, Warren P, Connell DA. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med. 2006;34:1008–1015. doi: 10.1177/0363546505283835. [DOI] [PubMed] [Google Scholar]
- 38.Street SF. Lateral transmission of tension in frog myofibers: a myofibrillar network and transverse cytoskeletal connections are possible transmitters. J Cell Physiol. 1983;114:346–364. doi: 10.1002/jcp.1041140314. [DOI] [PubMed] [Google Scholar]
- 39.Swanson SC, Caldwell GE. An integrated biomechanical analysis of high speed incline and level treadmill running. Med Sci Sports Exerc. 2000;32:1146–1155. doi: 10.1097/00005768-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 40.Thelen DG, Chumanov ES, Best TM, Swanson SC, Heiderscheit BC. Simulation of biceps femoris musculotendon mechanics during the swing phase of sprinting. Med Sci Sports Exerc. 2005;37:1931–1938. doi: 10.1249/01.mss.0000176674.42929.de. [DOI] [PubMed] [Google Scholar]
- 41.Tidball JG. Force transmission across muscle cell membranes. J Biomech. 1991;24(suppl 1):43–52. doi: 10.1016/0021-9290(91)90376-X. [DOI] [PubMed] [Google Scholar]
- 42.Wang ZM, Messi ML, Delbono O. Sustained overexpression of IGF-1 prevents age-dependent decrease in charge movement and intracellular Ca(2+) in mouse skeletal muscle. Biophys J. 2002;82:1338–1344. doi: 10.1016/S0006-3495(02)75489-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Warren P, Gabbe BJ, Schneider-Kolsky M, Bennell KL. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med. 2010;44:415–419. doi: 10.1136/bjsm.2008.048181. [DOI] [PubMed] [Google Scholar]
- 44.White LC, Dolphin P, Dixon J. Hamstring length in patellofemoral pain syndrome. Physiotherap. 2009;95:24–28. doi: 10.1016/j.physio.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 45.Yu B, Queen RM, Abbey AN, Liu Y, Moorman CT, Garrett WE. Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41:3121–3126. doi: 10.1016/j.jbiomech.2008.09.005. [DOI] [PubMed] [Google Scholar]